Abstract
Chronic deciduitis is characterized by the presence of lymphoplasmacytic inflammation or, in the absence of plasma cells, diffuse and intense (>50/HPF) non-perivascular lymphocytes in the decidua. Chronic deciduitis is one of a group of chronic placental inflammatory lesions, which include VUE and chronic chorioamnionitis. While the exact cause is not known, it is suggested that immune mechanisms related to maternal anti-fetal rejection, or alternatively, chronic microbial infection, may be involved in causation. Chronic deciduitis is an association with preterm labour. Chronic deciduitis is more frequent in chromosomally normal and abnormal spontaneous miscarriage, when compared to elective terminations, suggesting a role in first trimester pregnancy loss.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Chronic deciduitis is one of the chronic inflammatory lesions of the placenta, the involved placental compartment being the decidua [1]. It is diagnosed in the presence of plasma cells and lymphocytes, or in the absence of plasma cells, diffuse and intense non-perivascular lymphocytes [1]. Chronic deciduitis is frequently seen in association with chronic chorioamnionitis and VUE [2]. The association of chronic deciduitis with other placental chronic inflammatory lesions supports it being a histologic manifestation of maternal anti-fetal rejection; however, the possibility of microbial infection of the endometrium must also be considered as a cause [3]. The association of chronic deciduitis with higher rates of IgG class I and IgG class II HLA panel antibodies [4] and placental C4d deposition [5] when compared to controls supports the association of chronic deciduitis with maternal immune response to fetal antigens, rather than to infection. Chronic deciduitis is more frequent in placentas resulting from egg donor pregnancies (immunogenetically unrelated to the mother) when compared to non-egg donor pregnancies (semi-allografts) [6, 7] also supporting an immune mechanism. Chronic deciduitis is an association with preterm labour [8].
2 Definition
Chronic deciduitis is diagnosed in the presence of lymphoplasmacytic inflammation in the decidua or, in the absence of plasma cells, the presence of diffuse and intense (>50/HPF) non-perivascular lymphocytic inflammation.
3 Synonyms
Lymphoplasmacytic deciduitis , Chronic lymphoplasmacytic deciduitis , Chronic deciduitis with plasma cells, Chronic plasma cell deciduitis , Chronic lymphocytic deciduitis .
4 Epidemiology
Chronic deciduitis is a commonly diagnosed lesion. It is more frequent in preterm compared to term placentas, having been reported in 8–25% of preterm compared to 2–13% of term placentas [2, 9]. Chronic deciduitis is frequently seen with chronic chorioamnionitis [2] and VUE, particularly basal chronic villitis [2, 10]; however, it is not uncommon to see chronic deciduitis in isolation [2]. Chronic deciduitis is also frequently seen in decidualized endometrium from first trimester spontaneous miscarriage, having been reported in 9–20% of chromosomally normal and 4–30% of chromosomally abnormal spontaneous miscarriage [5, 11]. It is particularly common in recurrent chromosomally normal spontaneous miscarriage [11]. In comparison, it has been reported in 0% of elective abortions [5].
5 Gross Findings
Chronic deciduitis is not associated with any gross morphologic changes in the basal plate or the placental disc.
6 Histopathology
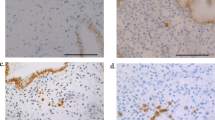
Chronic deciduitis is diagnosed when plasma cells and lymphocytes are identified in the decidua (Figs. 33.1 and 33.2) or there is diffuse and intense lymphocytic infiltration (>50/HPF) [1]. Plasma cells are frequently present in small scattered clusters admixed with the lymphocytes, although they can be sparse. There are no current data to correlate the numbers of lymphocytes or plasma cells with clinical outcomes; however, this quantification of lymphocytes represents an agreed-upon definition by the authors allowing for reproducibility and future research. The lymphocytes should be non-perivascular, as lymphocytes in a perivascular location may be seen with maternal vasculopathy, and therefore may have a different connotation. As chronic deciduitis is associated with other chronic inflammatory lesions, especially basal chronic villitis [2, 10], the presence of basal chronic villitis should prompt a search for chronic deciduitis.
7 Immunohistochemistry
Immunohistochemical stains for CD138 will highlight plasma cells but are not necessary to confirm the diagnosis (Fig. 33.3).
8 Genetic Susceptibility
Currently, there is no known genetic susceptibility to develop chronic deciduitis.
9 Prognosis and Predictive Factors
Chronic deciduitis is an association with preterm labour [2, 8]. It is also an association with chromosomally normal and abnormal spontaneous miscarriage [5, 11], being particularly frequent in recurrent spontaneous miscarriage [11], supporting a role for maternal anti-fetal rejection in early fetal loss. Chronic deciduitis is frequently associated with C4d deposition in the placenta in spontaneous miscarriage, a feature of classical complement pathway activation, and it has been proposed that this might be a mechanism of placental and fetal injury [5]. A recent study has shown an association of basal chronic deciduitis with morbidly adherent placenta; however, the role of chronic inflammation in the pathogenesis of abnormal placental adherence is unclear [12]. As with other chronic inflammatory lesions of the placenta, the antigenic stimulation eliciting the inflammation is not known. The association of chronic deciduitis with preterm labour and spontaneous miscarriage requires further investigation. Most studies have required the presence of plasma cells for the diagnosis of chronic deciduitis, and the significance of chronic deciduitis with plasma cells may be different from that without plasma cells.
References
Khong TY, Bendon RW, Qureshi F, Redline RW, Gould S, Stallmach T, et al. Chronic deciduitis in the placental basal plate: definition and interobserver reliability. Hum Pathol. 2000;31:292–5.
Kim CJ, Romero R, Kusanovic JP, Yoo W, Dong Z, Topping V, et al. The frequency, clinical significance, and pathological features of chronic chorioamnionitis: a lesion associated with spontaneous preterm birth. Mod Pathol. 2010;23:1000–11.
Kim CJ, Romero R, Chaemsaithong P, Kim J-S. Chronic inflammation of the placenta: definition, classification, pathogenesis, and clinical significance. Am J Obstet Gynecol. 2015;213:S53–69.
Lee JH, Romero R, Xu Y, Kim J-S, Park JY, Kusanovic JP, et al. Maternal HLA panel-reactive antibodies in early gestation positively correlate with chronic chorioamnionitis: evidence in support of the chronic nature of maternal anti-fetal rejection. Am J Reprod Immunol. 2011;66:510–26.
Lee JY, Hong J-S, Kim EN, Ahn S, Choe J, Hwang D, et al. Placental C4d is a common feature of chromosomally normal and abnormal miscarriages. Virchows Arch. 2014;464:613–20.
Perni SC, Predanik M, Cho JE, Baergen RN. Placental pathology and pregnancy outcomes in donor and non-donor oocyte in vitro fertilization pregnancies. J Perinat Med. 2005;33:27–32.
Gundogan F, Bianchi DW, Scherjon SA, Roberts DJ. Placental pathology in egg donor pregnancies. Fertil Steril. 2010;93:397–404.
Edmondson N, Bocking A, Machin G, Rizek R, Watson C, Keating S. The prevalence of chronic deciduitis in cases of preterm labor without clinical chorioamnionitis. Pediatr Dev Pathol. 2009;12:16–21.
Kraus FT, Redline RW, Gersell DJ, Nelson DM, Dicke DK. Inflammation and infection. Placental pathology: atlas of non-tumor pathology (first series, fascicle 3). Washington (DC): American Registry of Pathology; 2004. p. 75–115.
Redline RW. Villitis of unknown etiology: noninfectious chronic villitis in the placenta. Hum Pathol. 2007;38:1439–46.
Redline R, Zaragoza M, Hassold T. Prevalence of developmental and inflammatory lesions in nonmolar first-trimester abortions. Hum Pathol. 1999;30:93–100.
Ernst LM, Linn RL, Mintern L, Miller ES. Pathologic associations with morbidly adherent placenta: potential insights into pathogenesis. Pediatr Devel Pathol. 2017;20:387–96.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jacques, S.M., Qureshi, F., Ernst, L.M. (2019). Chronic Deciduitis. In: Khong, T., Mooney, E., Nikkels, P., Morgan, T., Gordijn, S. (eds) Pathology of the Placenta. Springer, Cham. https://doi.org/10.1007/978-3-319-97214-5_33
Download citation
DOI: https://doi.org/10.1007/978-3-319-97214-5_33
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97213-8
Online ISBN: 978-3-319-97214-5
eBook Packages: MedicineMedicine (R0)