Abstract
The concept of acquired short esophagus is possibly one of the most controversial aspects in surgery for benign esophageal disease with esophageal lengthening procedures being useful techniques in the armamentarium of an upper GI surgeon. Esophageal lengthening procedures are required when there is a less than 2.5 cm of intra-abdominal esophagus. Conditions often associated with this include chronic GERD, giant hernia, and presence of a stricture; however, ultimately the need for a Collis gastroplasty can only be determined intraoperatively. Type II mobilization of the esophagus is critical to gaining length in addition to careful determination of the gastroesophageal junction. The modified Collis gastroplasty holds the potential to decrease recurrence and wrap failure in the properly selected patient population. It is associated with minimal morbidity with most studies demonstrating equivalent quality of life outcomes in comparison with fundoplication-only cohorts.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Short esophagus
- Collis gastroplasty
- Paraesophageal hernia
- Intrathoracic stomach
- Fundoplication
- Stapled gastroplasty
- Recurrence paraesophageal hernia
- Esophageal lengthening
The concept of acquired short esophagus is possibly one of the most controversial aspects in surgery for benign esophageal disease. Many experienced surgeons challenge the existence of this condition [1, 2], whereas others attest to the importance of its recognition and treatment to optimize surgical outcomes. Regardless, esophageal lengthening procedures are useful techniques in the armamentarium of an upper GI surgeon and are the focus of this chapter.
Incidence and Pathophysiology
The incidence of shortened esophagus is challenging to ascertain due to a lack of uniform definition with a wide variation in the surgical literature. Recent studies at high-volume centers identify rates between 0% and 18% [3,4,5] depending on the need for extensive mediastinal dissection and Collis gastroplasty. Pathophysiology of a foreshortened esophagus is multifactorial and attributed to chronic inflammation in the setting of GERD. A lax lower esophageal sphincter results in refluxed gastric juices with edema and inflammation seeping from the mucosa into the esophageal wall. Chronicity of this insult causes transmural inflammation and longitudinal fibrosis and is presumed to be the cause of a shorter esophagus [6, 7].
Treating a short esophagus or intra-abdominal esophageal length of <2.5 cm is imperative to ensure decreased tension of the wrap, prevent wrap failure, and avoid recurrence. Of particular importance is the higher failure rates noted for giant paraesophageal hernias where a lengthening procedure will be of benefit [8].
Preoperative Prediction of the Short Esophagus
No single preoperative test is adequate to predict the need for esophageal lengthening maneuvers, although a patient with a giant paraesophageal hernia that has been present for more than 30 years with severe reflux is certainly a warning sign. The usual battery of preoperative tests for GERD patients includes upper endoscopy, pH study, manometry, and an upper GI contrast esophagogram (Fig. 21.1). Some studies suggested that presence of long segment (>5 cm) nonreducible type I hernia or a type III hernia on esophagogram were predictive of a short esophagus [9]; however other investigations have yielded a positive predictive value of only 50% for barium esophagograms [6]. Esophageal length on manometry is useful if found to be below the 5th percentile, but absolute values are difficult to interpret due to variation according to body habitus [10].
Endoscopic measurements of esophageal length, when corrected for height, have been used for prediction. The esophageal length index (ELI) is the ratio of esophageal length (cm) to the patient’s height (meters) with an ELI of 19.5 or less having a positive predictive value of 81% and a negative predictive value of 83% [11]. The use of information from all tests conducted preoperatively will aid in prognostication of a lengthening procedure; however definite assessment takes place intraoperatively (Table 21.1).
Intraoperative Evaluation for Conducting a Lengthening Procedure
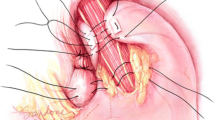
Prior to determining esophageal length , any intrathoracic stomach must be completely reduced along with removal of the hernia sac. Classification of circumferential mediastinal mobilization of the esophagus is labeled as type I if the length is less than 5 cm and type II when it is between 5 and 10 cm [6]. The vagus nerves must be identified and preserved during this mobilization in order to prevent delayed gastric emptying postoperatively. After a type I mobilization is completed, the gastroesophageal fat pad is dissected medially, and any tubes in the esophagus are withdrawn. Starting from the left side of the patient, the gastroesophageal fat pad is removed sparing the vagus to reveal the esophagogastric junction. The very best way to identify this is in conjunction with intraoperative endoscopy and transillumination of the esophagogastric junction (top of the rugal folds). One must be aware not to merely identify the squamocolumnar junction, as many of these patients may have Barrett’s esophagus, and this line may be falsely high above the esophagogastric junction. Intra-abdominal esophageal length can be estimated by measuring the distance from the hiatus to the gastroesophageal junction without utilizing any instruments to pull down on the esophagus during the measurement with an aim of 2.5 cm to ensure minimal tension on the fundoplication. If the intra-abdominal length is suboptimal, further mediastinal dissection of up to 10 cm (type II mobilization) should be completed for mobilization. Some authors have identified the carina [12] or the inferior pulmonary veins [13] as their upper limit. Extensive mediastinal dissection generally yields an adequate intra-abdominal length [14]; however, if this is still insufficient, modified Collis gastroplasty techniques will be required to decrease tension (Fig. 21.2) and reduce recurrence.
Techniques for Esophageal Lengthening
The original Collis gastroplasty described in 1957 was performed through a thoracoabdominal incision [15]. With the progress of minimally invasive techniques, currently the modified Collis wedge gastroplasty is completed laparoscopically, often using the same port placement required for the fundoplication. Our standard port placement is a 5 mm epigastric port for a Nathanson liver retractor , two surgeon ports in the right midclavicular (5 mm) and left subcostal (10 mm) region, a supraumbilical camera port (10 mm), and a midaxillary assistant port (5 mm).
The left subcostal operator port is upsized to a 12 mm port and a 50F bougie is inserted. The surgeon retracts the stomach just beyond the angle of His using the right operator port, and the assistant applies downward traction near the first short gastric artery in order to fan out the stomach in preparation for a wedge gastroplasty. A reticulating endoscopic stapler is introduced through the left subcostal port and fired at a 45-degree angle aiming for 3 cm below the GEJ and abutting the bougie. Usually two to three firings of the linear stapler may be required (Fig. 21.3). Then, a vertical firing of the staple parallel to the bougie results in completion of the wedge. A fundoplication can be completed in the usual manner for a wrap fashioned around this neo-esophagus with the bougie still in place. The wrap should ideally cover the staple line, and it is not typically necessary to oversew the staple line. Of note, performing a lengthening procedure on a stomach with ischemic changes such as patients with volvulus is highly discouraged due to increased risk of leak.
Important aspects to consider when performing the wedge gastroplasty include avoiding a 90-degree angle with the stapler which inadvertently removes a larger portion of the fundus, leaving the same length gained on the esophagus but a smaller portion of fundus to perform the wrap. The use of a bougie is imperative to avoid stenosis of the neo-esophagus.
A modified Collis gastroplasty can be performed with a Nissen and Toupet [16] and less often with a Dor [17] fundoplication. Type of fundoplication will be dictated by the preoperative esophageal motility studies and factors including scleroderma, diffuse esophageal spasm, and achalasia.
Slight variations to the modified Collis gastroplasty are published in the current literature with good outcomes. Wilson and colleagues [18] describe their approach consisting of a single fire of the endoscopic stapler parallel to the bougie through a single left anterior axillary line intercostal space incision after completing all the usual steps laparoscopically. The group describes obviating the need for a wedge fundectomy and crossing staple lines with this technique.
Postoperative Management
A nasogastric tube is inserted intraoperatively, and postoperative nausea is carefully controlled to avoid retching or vomiting which strains the wrap. We selectively perform barium swallow on postoperative day 1, and if no leak is confirmed, the nasogastric tube is removed, and the patient resumes a clear fluid diet. Gradual progression to a soft fundoplication diet is advised and discharged is planned typically on POD 1. Occasionally esophagograms performed after Collis gastroplasty may be misinterpreted as recurrence due to the presence of rugal folds above the wrap, and caution must be exercised when reading these images.
Review of Outcomes
Prevention of staple line leak is a foremost priority after a modified Collis procedure. In recent series, the incidence for wedge gastroplasty does not demonstrate any significant increased leak risk in comparison with a fundoplication-only cohort [19, 20].
Furthermore, since the neo-esophagus lacks motility, worsened dysphagia is another concern for these patients. Studies have demonstrated a slightly higher rate of dysphagia in comparison with fundoplication-only patients; however these have not been statistically significant. Furthermore, when comparing pre- and postoperative dysphagia symptoms, consistent improvement in the modified Collis cohort has been noted [19].
Due to an aperistaltic segment and wrap around the mucosa that can still produce acid, increased reflux is another postoperative issue to consider. Studies have confirmed a longer acid clearance time in patient with a Collis gastroplasty in comparison with a fundoplication-only group [21]. However, reflux symptoms and use of anti-reflux medication have demonstrated to be comparable in the two groups [19].
Recurrence rates or wrap failure after a Collis gastroplasty ranges between 0% and 18% in a recent review of current literature [22]. It is difficult to compare recurrence rates as patients are not followed routinely with imaging, and the definition of recurrence differs among studies (radiologic vs. clinical). In a few studies, wrap failure and recurrence for giant paraesophageal hernias (where a Collis gastroplasty is now often employed) who received only a fundoplication were between 32% and 42% [23,24,25]. Therefore, this suggests a trend of improved outcomes with the modified Collis procedure.
Summary
A key to the success of the reflux operation and paraesophageal hernia repair is a tension-free intra-abdominal wrap. Esophageal lengthening procedures are required when there is a less than 2.5 cm of intra-abdominal esophagus. Conditions often associated with this include chronic GERD, giant hernia, and presence of a stricture; however, ultimately the need for a Collis gastroplasty can only be determined intraoperatively. Type II mobilization of the esophagus is critical to gaining length in addition to careful determination of the gastroesophageal junction. The modified Collis gastroplasty holds the potential to decrease recurrence and wrap failure in the properly selected patient population. It is associated with minimal morbidity with most studies demonstrating equivalent quality of life outcomes in comparison with fundoplication-only cohorts.
References
Madan AK, Frantzides CT, Patsavas KL. The myth of the short esophagus. Surg Endosc. 2004;18(1):31–4.
Korn O, Csendes A, Burdiles P, Braghetto I, Sagastume H, Biagini L. Length of the esophagus in patients with gastroesophageal reflux disease and Barrett’s esophagus compared to controls. Surgery. 2003;133(4):358–63.
Swanstrom LL, Marcus DR, Galloway GQ. Laparoscopic Collis gastroplasty is the treatment of choice for the shortened esophagus. Am J Surg. 1996;171(5):477–81.
Awad ZT, Mittal SK, Roth TA, Anderson PI, Wilfley WA Jr, Filipi CJ. Esophageal shortening during the era of laparoscopic surgery. World J Surg. 2001;25(5):558–61.
O’Rourke RW, Khajanchee YS, Urbach DR, Lee NN, Lockhart B, Hansen PD, Swanstrom LL. Extended transmediastinal dissection: an alternative to gastroplasty for short esophagus. Arch Surg. 2003;138(7):735–40.
Horvath KD, Swanstrom LL, Jobe BA. The short esophagus: pathophysiology, incidence, presentation, and treatment in the era of laparoscopic antireflux surgery. Ann Surg. 2000;232(5):630–40.
Gozzetti G, Pilotti V, Spangaro M, Bassi F, Grigioni W, Carulli N, Loria P, Felice V, Lerro F, Mattioli S. Pathophysiology and natural history of acquired short esophagus. Surgery. 1987;102(3):507–14.
Terry ML, Vernon A, Hunter JG. Stapled-wedge Collis gastroplasty for the shortened esophagus. Am J Surg. 2004;188(2):195–9.
Bremner RM, Bremner CG, Peters JH. Fundamentals of antireflux surgery. In: Peters JH, DeMeester TR, editors. Minimally invasive surgery of the foregut. 1st ed. St Louis: Quality Medical Publishing; 1994. p. 119–243.
Gastal OL, Hagen JA, Peters JH, Campos GM, Hashemi M, Theisen J, Bremner CG, DeMeester TR. Short esophagus: analysis of predictors and clinical implications. Arch Surg. 1999;134(6):633–6.
Yano F, Stadlhuber RJ, Tsuboi K, Garg N, Filipi CJ, Mittal SK. Preoperative predictability of the short esophagus: endoscopic criteria. Surg Endosc. 2009;23(6):1308–12.
Swanstrom LL, Hansen P. Laparoscopic total esophagectomy. Arch Surg. 1997;132(9):943–7.
DeMeester SR. Laparoscopic paraesophageal hernia repair: critical steps and adjunct techniques to minimize recurrence. Surg Laparosc Endosc Percutan Tech. 2013;23(5):429–35.
Bochkarev V, Lee YK, Vitamvas M, Oleynikov D. Short esophagus: how much length can we get? Surg Endosc. 2008;22(10):2123–7.
Collis JL. An operation for hiatus hernia with short oesophagus. Thorax. 1957;12(3):181–8.
J Z, DeMeester SR, Ayazi S, Kilday P, Alicuben ET, DeMeester TR. Laparoscopic wedge fundectomy for collis gastroplasty creation in patients with a foreshortened esophagus. Ann Surg. 2014;260(6):1030–3.
Latzko M, Borao F, Squillaro A, Mansson J, Barker W, Baker T. Laparoscopic repair of paraesophageal hernias. JSLS. 2014;18(3):e2014.00009.
Wilson JL, Bradley DD, Louie BE, Aye RW, Vallières E, Farivar AS. Laparoscopy with left chest collis gastroplasty: a simplified technique for shortened esophagus. Ann Thorac Surg. 2014;98(5):1860–2.
Nason KS, Luketich JD, Awais O, Abbas G, Pennathur A, Landreneau RJ, Schuchert MJ. Quality of life after collis gastroplasty for short esophagus in patients with paraesophageal hernia. Ann Thorac Surg. 2011;92(5):1854–60.
Houghton SG, Deschamps C, Cassivi SD, Allen MS, Nichols FC 3rd, Barnes SA, Pairolero PC. Combined transabdominal gastroplasty and fundoplication for shortened esophagus: impact on reflux-related and overall quality of life. Ann Thorac Surg. 2008;85(6):1947–52.
Mor A, Lutfi R, Torquati A. Esophageal acid-clearance physiology is altered after Nissen-Collis gastroplasty. Surg Endosc. 2013;27(4):1334–8.
Kunio NR, Dolan JP, Hunter JG. Short esophagus. Surg Clin North Am. 2015;95(3):641–52.
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, Bremner CG. Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg. 2000;190(5):553–60.
Khaitan L, Houston H, Sharp K, Holzman M, Richards W. Laparoscopic paraesophageal hernia repair has an acceptable recurrence rate. Am Surg. 2002;68(6):546–51.
Jobe BA, Aye RW, Deveney CW, Domreis JS, Hill LD. Laparoscopic management of giant type III hiatal hernia and short esophagus. Objective follow-up at three years. J Gastrointest Surg. 2002;6(2):181–8; discussion 188.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 SAGES
About this chapter
Cite this chapter
Sudarshan, M., Blackmon, S.H. (2019). Esophageal Lengthening Procedures. In: Grams, J., Perry, K., Tavakkoli, A. (eds) The SAGES Manual of Foregut Surgery . Springer, Cham. https://doi.org/10.1007/978-3-319-96122-4_21
Download citation
DOI: https://doi.org/10.1007/978-3-319-96122-4_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-96121-7
Online ISBN: 978-3-319-96122-4
eBook Packages: MedicineMedicine (R0)