Abstract
In severely injured trauma patients the hemorrhage control should occur as soon as possible, with a time-consciousness multidisciplinary protocol to reduce coagulopathies and secondary compartment syndrome risks. The damage control interventional radiology (DCIR) is an aggressive and time-conscious algorithm that prioritizes lifesaving maneuvers. As in damage control surgery, the DCIR could be a multistep strategy to maintain the patient alive, sometimes controlling but not definitively repairing the injury. It’s a teamwork effort in a very time-restricted procedure, and it’s crucial that all decisions should be shared with the trauma team. The choice of materials, embolic agent, and the operator expertise are critical to ultimate success. When severely injured patients are hemodynamically unstable, the DCIR suggest abandoning any time-consuming procedure in favor of another to save the patients’ life. The use of a hybrid trauma room containing an angiography suite/operating room is paramount for DCIR.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
Interventional radiology in damage control setting of the hemodynamically unstable trauma patients is an aggressive and time-restrained algorithm prioritizing saving life of the exsanguinating trauma patient.
-
DCIR aims to control hemorrhage by any possible means to save life in an extremely time-conscious, aggressive and minimally invasive manner.
-
The hybrid trauma room containing an angiography suite/operating room is a developing program around the world in the attempt to build new facilities to best hemorrhage control of DCIR treatment in severely injured trauma patients.
-
The choice of materials, embolic agent, and the operator expertise are critical to the success of DCIR.
-
DCIR belongs to a teamwork effort to maintain the patient alive in a very time-conscious procedure, and all decisions should be shared with the trauma team.
1 Introduction
The improvement of the acute trauma care workflow performed by a trained multidisciplinary team [1] and the increasing role of interventional radiology (IR) have been changing the management of severely injured patients [2]. Hemorrhage control is time critical, and delaying the operative intervention increases the mortality risks [3]. The hemorrhage control should occur as soon as possible [4], in a time-consciousness protocol to reduce coagulopathies and secondary compartment syndromes’ risk [4,5,6].
Damage control interventional radiology (DCIR) is an aggressive and time-restrained algorithm that prioritizes saving life of the severely traumatized patient with ongoing hemorrhage [1] focusing on hemodynamically unstable patients. Different from DCIR, conventional emergency interventional radiology (CEIR) focuses on hemodynamically stable patients; however, both groups require distinct approaches, methods, and strategies.
The prompt and rapid endovascular strategies in trauma occasions (PRESTO) algorithm addresses and manages the trauma of severe acute hemorrhaging patient from the moment of arrival to the trauma bay until initial completion of hemostasis [1]. This algorithm is based on the motto “Start soon and finish sooner” and aims to shorten the timing of interventional radiology (IR) activation when compared to CEIR. It also relies on the rapid completion of hemostasis in hemodynamically unstable patients, specifically tailoring the damage control. The PRESTO/DCIR algorithm can successfully manage severely injured patients and can increase survival rates [2].
The term “damage control” is derived from the US Navy and describes the capacity of a ship to absorb damage and maintain mission integrity [7]. The concept of “damage control surgery” was developed in the early 1980s to reduce mortality in exsanguinating patients with coagulopathy [8]. In the management of traumatic hemorrhage, the risk of death is increased by a vicious cycle of hypothermia, coagulopathy, and metabolic acidosis known as the triad of death. The “damage control” approach reduces the mortality rate in severely injured patients [9,10,11,12,13]. It is a multistep strategy that aims to restore normal physiology over restoring normal anatomy in hemodynamically unstable patients, controlling but not definitively repairing the injury. Definitive surgery would only occur once all physiological parameters were corrected and normalized [14].
DCIR focuses on hemodynamically unstable patients and aims to control hemorrhage by any possible means to save life in an extremely time-conscious, aggressive, and minimally invasive manner. According to PRESTO/DCIR [1], all procedures from catheterization to the final visual confirmation of embolization are to be completed within a 10-min window for each targeted vessel. The goal of DCIR is not to reach a perfect distal embolization but rather to contain the ongoing bleeding in the fastest way to maintain or re-establish normal hemodynamic values.
The DCIR also develops a crucial role in the presence of arterial hemorrhage after damage control laparotomy. Sometimes the arterial hemorrhage could not be controlled by correction of coagulopathy, and it requires an adjunctive endovascular intervention procedure such as transarterial embolization [15,16,17,18].
2 Principles, Tools, and Techniques of IR in the Setting of Trauma
It’s important to record that DCIR belongs to a teamwork effort to maintain the patient alive in a very time-conscious procedure and all decision should be shared with the trauma team group. As in damage control surgery, the DCIR could be a multistep strategy that aims to maintain the patient alive over restoring normal anatomy, sometimes controlling but not definitively repairing the injury.
The choice of materials, embolic agent, and the operator expertise are critical to ultimate success. Smaller blood vessels typically require femoral access with a 5F sheath, distal catheterization with microcatheters, followed by deployment of microcoils, gel-foam slurry, beads, and glue, based on operator familiarity. In hemodynamically unstable trauma patients, the entity of trauma is usually bigger, and the IR must be more aggressive to save the life of the patient by rapidly controlling exsanguinating hemorrhage. An organ may be sacrificed as life matters most [1], and a balance needs to be struck between precision and suboptimal embolization [19,20,21,22]. As the procedure should be done in the shortest time possible, the expertise of IR and the ability with material play a crucial role.
Larger vessels (such as proximal internal iliac and splenic arteries) typically require femoral access with 5F or 6F sheaths followed by deployment of larger coils or Amplatzer plugs [23, 24]. For other arterial injuries, the placement of covered stent grafts is a valid option and usually requires sheath access that can be obtained, depending on the location of the injury, from either the femoral or brachial artery. Usually, femoral access is preferable because stent grafts require sheaths up to 7F or 8F and should be placed over the stiffest wire possible to allow for better support during deployment. The choice of self or balloon-expandible stent grafts depends on the type and the localization of the vascular lesion. Self-expandible stent grafts are more flexible and can be tracked easily through tortuous anatomy; they can conform to different diameters of a single vessel and should be oversized to reach an outward radial force for good vessel wall apposition. They also have higher resistance to crushing or deformation in mobile areas of the body and are produced in a greater range of diameters and lengths; for these reasons, they are more frequently used. Balloon-expandable stent grafts are ideal for immobile and well-protected areas of the body, such as renal, mesenteric, common iliac, and subclavian arteries, as well as ostial lesions. In addition, these stent grafts have higher precision in deployment compared to self-expanding stent grafts [23, 24].
When severely injured patients are hemodynamically unstable, the DCIR suggest abandoning any time-consuming procedure in favor of another for the sake of patient survival. Placing a temporary balloon catheter will maintain sufficient blood flow and pressure, whereby providing the physician enough time to assess and consult with trauma team whether to continue the IR procedure or not. It’s important to remember that for an aortic balloon occlusion, it’s necessary vascular access with sheaths up to 12Fr. During DCIR procedure, the operator is expected to reassess each maneuver every 5 min. In this setting, failing or time-consuming procedures (>5 min) should be discontinued and replaced by alternative procedures [1].
The use of a hybrid trauma room containing an angiography suite/operating room is the future trend to better DCIR treatment. A time rigorous and specifically designed protocol for hemodynamically unstable patients is crucial to successfully control time and consequently increase survival rates.
Case 1. Mediastinal Hematoma
Male 77 years old hemodynamically unstable with mediastinal hematoma with arterial blushing from the right bronchial artery. The mass effect of the hematoma determined atrial compression and atrial fibrillation (Figs. 57.1 and 57.2).
The right bronchial artery was super-selectively entered, and the embolization was performed with Glubran (Figs. 57.3 and 57.4).
Case 2. Axillary Injury
Male 48 years old, hemodynamically unstable trauma with pneumothorax and axillary artery injury.


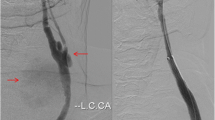
The angiography confirms the left axillary injury. A cover stent was placed to correct the axillary lesion.
Case 3. Pelvic Fracture with Arterial Bleeding from Left Hypogastric Artery
Female 68 years old with a pelvic and femoral fracture. CT after pelvic packing shows arterial blushing. The angiography confirms blushing from left obturator artery, super-selective catheterization was quickly performed, and the pseudoaneurysm was occluded with Glubran.


Case 4. Pelvic Fracture with Arterial Bleeding from Hypogastric Artery
Female 38 years old with pelvic fracture. The angiography shows blushing from right obturator artery; quick embolization was performed with Glubran.


Case 5. Hepatic Injury
Male 50 years old, hemodynamically unstable after motorcycle polytrauma. The axial CT scan shows arterial blushing in the S7 hepatic segment. The angiography confirms the right hepatic blushing. Quick embolization was performed with Glubran. The patient developed a hepatic abscess that was drained; no hepatic dysfunction was observed later.


Case 6. Splenic Embolization
Male 66 years old, hemodynamically unstable polytrauma, after falling from the second floor. Axial CT scan shows a grade IV spleen lesion. The angiography confirms CT found. Quick embolization was performed with proximal splenic artery plug.


Case 7. Extremity Vascular Injuries
Male 30 years old, hemodynamically unstable polytrauma after a free fall. The angiography confirms the arterial blushing from deep femoral arterial with arteriovenous fistula. The branch was embolized with Glubran. The X-ray shows the Glubran occluding the vessel.


Case 8. Blunt Traumatic Thoracic Aortic Injury
Blunt thoracic aortic injury after a car accident in a hemodynamically unstable patient. Thoracic endovascular aortic repair (TEVAR) was performed.


References
Matsumoto J, Lohmana BD, Morimotob K, Ichinoseb Y, Hattoric T, Taira Y. Damage control interventional radiology (DCIR) in prompt and rapid endovascular strategies in trauma occasions (PRESTO): a new paradigm. Diagn Interv Imaging. 2015;96:687–91.
Kinoshita T, Yamakawa K, Matsuda H, Yoshikawa Y, Wada D, Hamasaki T, Ono K, Nakamori Y, Fujimi S. The survival benefit of a novel trauma workflow that includes immediate whole-body computed tomography, surgery, and interventional radiology, all in one trauma resuscitation room: a retrospective historical control study. Ann Surg. 2017.
Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 min. J Trauma. 2002;52:420–5.
Kirkpatrick AW, Vis C, Dubé M, Biesbroek S, Ball CG, Laberge J, Shultz J, Rea K, Sadler D, Holcomb JB, Kortbeek J. The evolution of a purpose designed hybrid trauma operating room from the trauma service perspective: the RAPTOR (resuscitation with angiography percutaneous treatments and operative resuscitations). Injury. 2014;45(9):1413–21.
Kirkpatrick AW, Balogh Z, Ball CG, Ahmed N, Chun R, McBeth P, et al. The secondary abdominal compartment syndrome: iatrogenic or unavoidable? J Am Coll Surg. 2006;202(4):668–79.
Tremblay LN, Feliciano DV, Rozycki GS. Secondary extremity compartment syndrome. J Trauma. 2002;53:833–7.
Department of Defense. Surface ship survivability. Washington, DC: US Government Printing Office; 1996. Naval War Publication 3e20.31.
Stone HH, Strom PR, Mullins RJ. Management of the major coagulopathy with onset during laparotomy. Ann Surg. 1983;197(5):532–5.
Loveland JA, Boffard KA. Damage control in the abdomen and beyond. Br J Surg. 2004;91:1095–101.
Moore EE, Burch JM, Franciose RJ, et al. Staged physiologic restoration and damage control surgery. World J Surg. 1998;22:1184–90.
Pachter HL, Spencer FC, Hofstetter SR, et al. Significant trends in the treatment of hepatic trauma: experience with 411 injuries. Ann Surg. 1992;215:492–500.
Rotondo MF, Schwab CW, McGonigal MD, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35:375–82.
Rotondo MF, Zonies DH. The damage control sequence and underlying logic. Surg Clin N Am. 1997;7:761–77.
Jaunoo SS, Harji DP. Damage control surgery. Int J Surg. 2009;7(2):110–3.
Lin BC, Wong YC, Lim KE, Fang JF, Hsu YP, Kang SC. Management of ongoing arterial haemorrhage after damage control laparotomy: optimal timing and efficacy of transarterial embolization. Injury. 2010;41(1):44–9.
Davis KA, Fabian TC, Croce MA, et al. Improved success in nonoperative management of blunt splenic injuries: embolization of splenic artery pseu-doaneurysm. J Trauma. 1998;44:1008–113.
Gorich J, Rilinger N, Brado M, et al. Non-operativemanagementofarterialliver hemorrhages. Eur Radiol. 1999;9:60–7.
Sclafani SJ, Shaftan GW, Scalea TM, et al. Non-operative salvage of computed tomography-diagnosed splenic injuries: utilization of angiography for triage and embolization for hemostasis. J Trauma. 1995;39:818–25, discussion 826–7.
Singh A, Kumar A, Kumar P, Kumar S, Gamanagatti S. “Beyond saving lives”: current perspectives of interventional radiology in trauma. World J Radiol. 2017;9(4):155–77.
Wallis A, Kelly MD, Jones L. Angiography and embolization for solid abdominal organ injury in adults - a current perspective. World J Emerg Surg. 2010;5:18.
Lopera JE. Embolization in trauma: principles and techniques. Semin Intervent Radiol. 2010;27:14–28.
Bauer JR, Ray CE. Transcatheter arterial embolization in the trauma patient: a review. Semin Intervent Radiol. 2004;21:11–22.
Zhu X, Tam MD, Pierce G, McLennan G, Sands MJ, Wang W. Utility of the Amplatzer Vascular Plug in splenic artery embolization: a comparison study with conventional coil technique. Cardiovasc Intervent Radiol. 2011;34(3):522–31.
Kalish J. Selective use of endovascular techniques in the management of vascular trauma. Semin Vasc Surg. 2010;23(4):243–8.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Barbosa, F., Vercelli, R., Solcia, M., Migliorisi, C., Rampoldi, A. (2019). Selective Use of Endovascular Techniques in the Damage Control Setting. In: Aseni, P., De Carlis, L., Mazzola, A., Grande, A.M. (eds) Operative Techniques and Recent Advances in Acute Care and Emergency Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-95114-0_57
Download citation
DOI: https://doi.org/10.1007/978-3-319-95114-0_57
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95113-3
Online ISBN: 978-3-319-95114-0
eBook Packages: MedicineMedicine (R0)