Abstract
Rapidly growing mycobacteria (RGM) are divided into six major groups including the two clinically most important groups, M. chelonae/M. abscessus complex and Mycobacterium fortuitum group. This chapter discusses infections associated with these groups with an emphasis on pulmonary disease. Phenotypic and molecular laboratory identification methods are reviewed as accurate organism identification is necessary for optimal RGM lung disease patient management. Antimicrobial susceptibility patterns for the most common pathogenic RGM species are discussed with an emphasis on the impact of inducible macrolide resistance found in many RGM species and subspecies. Because of antibiotic resistance, the RGM are frequently difficult to treat successfully. Current therapeutic approaches are reviewed with an emphasis on antibiotic options in the context of both innate and acquired antibiotic resistance.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Taxonomy
Historical Background and Current RGM Classification
The term rapidly growing mycobacteria (RGM) was originally used to describe mycobacterial organisms with growth on subculture in less than 7 days. The first rapidly growing mycobacterium was described in the early twentieth century when Mycobacterium chelonae was recovered from the lungs of sea turtles [1]. Mycobacterium fortuitum was originally recovered from frogs in 1905 and dubbed Mycobacterium ranae later to become M. fortuitum at the suggestion of Ernest Runyon [2]. In 1953 Mycobacterium abscessus was first reported as a cause of human skin and soft tissue infection in a patient with multiple soft tissue abscesses [3].
There are now more than 75 recognized RGM species, representing approximately 50% of all mycobacterial species. (Table 1) [4,5,6,7,8,9,10,11]. The three most clinically important pathogenic species that represent more than 80% of clinical RGM isolates are M. fortuitum, M. chelonae, and M. abscessus. Mycobacterium abscessus was separated from M. chelonae more than 20 years ago, but some mycobacterial laboratories still utilize anachronistic nomenclature labeling M. abscessus isolates with a group label, “M. chelonae/abscessus complex,” rather than species or subspecies identification. This approach is not adequate or acceptable for contemporary RGM disease management.
Unfortunately, even the advent of molecular organism identification methods has not eliminated nomenclature confusion as illustrated by the recent controversies surrounding M. abscessus species and subspecies taxonomic designations. Mycobacterium bolletii and M massiliense were originally described as unique species distinct from M abscessus in 2004 and 2006, respectively, but were subsequently found to be indistinguishable based on 16S rRNA sequence analysis [5, 12,13,14,15]. This latter finding suggested that the putatively unique species were in fact the same species [12,13,14,15]. In 2011, a proposal was made that the two organisms should be combined as one species and reclassified as M. bolletii [14]. Subsequently, with multigene and whole genome sequencing , it became apparent that the two organisms are in fact distinct species with an extremely important genetic difference [15, 16]. One organism has an active erythromycin ribosomal resistance methylase (erm) gene and one does not. The erm gene results in methylation of the 23S rRNA macrolide binding site and inducible loss of macrolide activity/function, discussed in detail below.
Adoption of the 2011 proposal would have created significant confusion because the taxonomic designation M. massiliense had already been widely accepted in the medical literature to describe the “M. abscessus” organism without an active erm gene, while the term M. bolletii was used to describe the other similar organism with an active erm gene. There was a clear need to standardize the nomenclature for the three closely related M. abscessus organisms, two with active erm genes and one with an inactive erm gene.
In an effort to clarify this situation, Tortoli et al. recently proposed that the three organisms in the M. abscessus complex should be emended to three subspecies: M. abscessus subsp. abscessus and M. abscessus subsp. bolletii with active erm genes and M. abscessus subsp. massiliense with an inactive erm gene [16, 17]. The Tortoli proposal is not without controversy as universally accepted criteria for species and subspecies designations does not exist. A counter proposal has recently been advocated to grant species designations for the three M. abscessus organisms [18]. It should be emphasized that the M abscessus subsp. massiliense, or M. massiliense as sometimes cited, remains the generally accepted name for the M. abscessus organism with an inactive erm gene which remains the most clinically important aspect of the taxonomy debate [16, 17, 19, 20]. From a nihilistic standpoint, the clinician may not care what an organism is named but absolutely must know the status of the erm gene and in vitro macrolide susceptibility of the organism.
For this chapter we have adopted the M abscessus nomenclature suggested by Tortoli et al. with M. abscessus subspecies designations [16]. Where possible, an M. abscessus subspecies is identified in the text. When the term M. abscessus without a subspecies designation is used, it was not possible to tease out a particular subspecies designation. The term M. abscessus without a subspecies designation is not, therefore, synonymous with M. abscessus subspecies abscessus but indicates a lack of subspecies differentiation in the cited references.
Identifying RGM
Laboratory techniques for identifying RGM are briefly summarized here. A detailed discussion is beyond the scope of this chapter. For a more in-depth discussion, please see chapter “Laboratory Diagnosis and Antimicrobial Susceptibility Testing of Nontuberculous Mycobacteria”.
Phenotypic laboratory identification of RGM was previously based on growth in subculture in less than 7 days, colony morphology, and biochemical growth requirements. While the group of organisms categorized as RGM can be identified in this manner, definitive RGM identification is not possible. High-performance liquid chromatography (HPLC) of mycolic acids can identify only a few RGM species. HPLC may be useful for separating organisms into complexes or groups but lacks the specificity needed for full species-level identification [11, 21].
Lipid and ribosomal protein analyses by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) is a method currently being used to identify the NTM including RGM [21,22,23]. Although MALDI-TOF MS has been successful in the identification of many species of NTM, several clinically significant species and subspecies of RGM, including M. abscessus subsp. abscessus, M. abscessus subsp. massiliense, and M. abscessus subsp. bolletii, have been difficult to differentiate by MALDI-TOF.
Currently, the only nucleic acid probe available for identification of the RGM is the INNO-LiPA multiplex probe assay (Innogenetics, Ghent, Belgium). The major advantage is that a large variety of species can be identified by a single probe without necessitating the selection of a specific probe for each species. Disadvantages include cross-reactivity among closely related M. fortuitum groups and the inability to differentiate isolates of M. chelonae from M. abscessus [24, 25].
The primary gene target of molecular taxonomic studies has been the 16S rRNA gene which is a highly conserved gene within mycobacterial species [26]. Differentiation of M. chelonae and M. abscessus and some species within the M. fortuitum group requires complete 16S rRNA sequence analysis for species identification unless other gene targets are sequenced. The limitations of complete 16S rRNA sequencing for RGM species and subspecies differentiation were exposed by the recent M. abscessus subspecies controversy described above.
The 65-kDa heat shock protein gene (hsp65) is also useful for species-level RGM isolates such as M. abscessus and M. chelonae and for most of the common RGM species [27, 28]. Some RGM species, including M. fortuitum, are more readily discriminated with the hsp65 gene analysis than by 16S rRNA gene analysis [29]. The rpoβ gene has been used recently in the identification of RGM, including the identification of several new species [5, 12, 30,31,32,33].
Multiple different erm genes have been recognized in RGM species, including erm (M. fortuitum) and erm (M. abscessus subsp. abscessus). Some RGM species such as M. chelonae have no detectable erm gene which allows reliable identification of this organism.
Whole genome sequencing (WGS) and phylogenomic analysis are the most recently utilized methods for studying genetic variations and population studies in mycobacteria. Whole genome sequencing enables the study of multiple genetic regions which may be associated with pathogenicity, antibiotic resistance, virulence, and/or host relationships to the NTM. [34,35,36,37,38]. As previously noted, there are no universally accepted WGS criteria for defining NTM species and subspecies. Recent publications in cystic fibrosis literature have revealed M. abscessus subsp. massiliense isolates from patients in different countries including the United Kingdom, Brazil, and the United States, to have high levels of genetic relatedness by WGS and thus provided the first suggestion of possible person-to-person RGM transmission [17, 39, 40]. The future of NTM identification and epidemiological studies will likely be based upon WGS findings.
Clinicians must be familiar with the laboratory methods used for RGM identification including the limitations of the specific methods available to them. Clinicians should clearly communicate to laboratorians that optimal management of RGM disease patients requires timely and accurate organism identification. Clinicians face many challenges impeding successful treatment of these patients, and the laboratory should not be one of them.
Clinical Disease
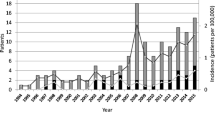
The RGM are frequently isolated in the environment and have been found in 30% to 78% of soil samples from various geographical regions in the United States [11, 41, 42]. Although it is a much less common occurrence than with Mycobacterium avium complex (MAC), M. abscessus has also been isolated from municipal water [43]. Until recently, the majority of reported cases were from the United States, with a strong disease geographic localization in the southern United States [11, 44]. Human infections have now been reported from most areas of the developed world (see chapters “Epidemiology of Nontuberculous Mycobacterial Pulmonary Disease (NTM PD) in the USA” and “Global Epidemiology of NTM Disease (Except Northern America)”). The route of organism acquisition for RGM pulmonary disease is presumably inhalation of contaminated aerosols, similar to MAC [44]. Community-acquired localized skin, soft tissue, and/or bone disease usually follows a traumatic injury with potential soil contamination . Nosocomial infections are strongly associated with tap water exposure or contamination.
Chronic Pulmonary Infections
Chronic RGM pulmonary infections are most often associated with M. abscessus subspecies [11, 42, 44] (Tables 2 and 3). The majority are due to either M. abscessus subsp. abscessus or M. abscessus subsp. massiliense. These infections are typically found in postmenopausal nonsmoking females who present with chronic cough, weight loss, fatigue, and sometimes hemoptysis. By high-resolution computerized tomography (HRCT) of the chest, most patients have patchy cylindrical bronchiectasis and small nodules involving the right middle lobe and lingua (Fig. 1a, b). This radiographic pattern is referred to as nodular bronchiectatic (NB) disease and is also typical of patients with Mycobacterium avium complex (MAC) lung disease. Chronic NB lung disease caused by MAC and M. abscessus are radiographically and clinically indistinguishable. RGM lung disease tends to be slowly progressive, with indolent symptomatic and radiographic progression [42, 44].
Patients undergoing therapy for MAC lung disease sometimes have co-isolation of M. abscessus from respiratory specimens. The clinical significance of these isolates is variable and must be determined with longitudinal evaluation [45]. In one recent series of MAC patients with co-isolation of M. abscessus, most M. abscessus isolates did not appear to be clinically significant when they occurred only once or twice without clinical and radiographic impact [45]. For some patients, however, M. abscessus was isolated from multiple specimens over time and was associated with radiographic progression, especially new or expanding lung cavitation. In these patients M. abscessus appeared to be a significant pathogen requiring therapeutic intervention. This latter consideration is not inconsequential as there are few antibiotic agents with activity against both MAC and M. abscessus subspecies with an active erm gene and therefore little overlap in treatment regimens for M. abscessus and MAC.
Cavitary lung disease that occurs with M. abscessus subspecies is a more aggressive disease than the NB form. Patients with long-standing NB RGM lung disease, either untreated or refractory to treatment, can evolve from NB lung disease to a mixed NB and cavitary lung disease (Fig. 2). Patients with primary cavitary disease are similar clinically to cavitary MAC lung disease patients, usually male with a history of cigarette smoking and COPD. Mycobacterium abscessus infection is also sometimes associated with other lung diseases and infections that leave residual areas of bronchiectasis and scarring such as tuberculosis.
Pulmonary infections with the M. fortuitum group are rare and most often seen in patients with achalasia, chronic vomiting, and other forms of gastrointestinal disturbances associated with chronic aspiration [42]. Mycobacterium fortuitum is a relatively non-virulent pathogen and a rare cause of lung disease outside of these conditions [42, 46]. Mycobacterium mucogenicum is sometimes a significant pathogen in the setting of chronic obstructive lung disease but overall is rarely associated with progressive chronic pulmonary infection [42]. Mycobacterium fortuitum and M. mucogenicum are examples of the poor specificity of the current NTM diagnostic guidelines in that patients with multiple sputum AFB cultures positive for M. fortuitum or M. mucogenicum are unlikely to develop progressive disease and require therapy. In the absence of a specific predisposition, such as chronic aspiration, clinicians are urged to use more rigorous diagnostic criteria for M. fortuitum and M. mucogenicum isolates than for other more common NTM respiratory pathogens.
Chronic pulmonary infections with M. abscessus also are seen in patients with cystic fibrosis (CF) (chapter “Non-tuberculous Mycobacteria in Cystic Fibrosis”) [47,48,49]. Patients with CF have aggressive and rapidly progressive bronchiectasis in addition to chronic recurrent airway and parenchymal infections due to Pseudomonas aeruginosa and other bacterial pathogens [48, 49]. Nontuberculous mycobacteria were previously thought not transmissible between humans. Recently, however, geographically widely dispersed cases associated with M. abscessus subsp. massiliense isolates that are indistinguishable by DNA analysis have been identified, suggesting direct or indirect spread of identical infections that can occur at least in this highly vulnerable population [17, 50].
The most common pathogens associated with CF lung disease in some series have been members of the M. abscessus group. One-half of 104 NTM isolates recovered in a multicenter study involving 1582 CF patients in France were M. abscessus [51]. A 3-year longitudinal clinical study from Brazil recovered NTM from 8% of 129 children with the majority of RGM isolates M. abscessus [52]. An early large study from US CF centers found that M. abscessus isolates were second in prevalence to those of the MAC [49]. Although some patients appear to have transient carriage, other patients remain culture positive, with significant symptoms and high morbidity and mortality [49].
The difficulty effectively treating M. abscessus lung infections in CF patients adds an additional layer of complexity to their management. Because of resistance to antibiotic therapy and the specter of postoperative infections with poor wound healing, isolation of M. abscessus can preclude lung transplant for CF patients in some centers.
Localized Posttraumatic Wound Infections
Wound infections are typically associated with accidental penetrating trauma with soft tissue infection sometimes followed by osteomyelitis [11] (Fig. 3). Patients with this type of infection are usually healthy without systemic immune suppression. After an incubation period of 3–6 weeks, local redness and swelling with spontaneous drainage typically occurs. Systemic symptoms such as fever, chills, malaise, and fatigue are infrequent. The drainage is usually thin and clear but occasionally can be thick and purulent. Sinus tract formations with intermittent drainage are common.
The most common pathogens in these settings are the M. fortuitum group including M. fortuitum, M. porcinum, and M. houstonense, but almost any of the pathogenic RGM species can cause disease in patients with infected open fractures [4, 8, 11]. Furthermore, these infections may be polymicrobial, reflecting environmental contamination with more than one species of mycobacteria or a combination of bacteria and mycobacteria. Timely diagnosis requires clinical suspicion in a patient who is not responding to or improving with standard antibacterial antibiotics.
Surgical Wound Infections
Most outbreaks of healthcare-associated RGM infections or pseudo-infections have been associated epidemiologically with various water sources, including water-based solutions, distilled water, tap water, ice, and ice water [11, 52, 53]. The utilization of pulsed-field gel electrophoresis and randomly amplified polymorphic DNA PCR methods for analyzing genomic DNA has improved the investigation of nosocomial outbreaks [11, 54, 55]. DNA fingerprinting for some of these outbreaks has confirmed molecular identity between water and human isolates. One study of hemodialysis centers in the United States showed that 55% of incoming city water contained mycobacteria, of which RGM species were the most common [56]. Biofilms, which are the lipid-rich layers that form at water-solid interfaces, are present in most water transport pipes. Up to 90% of these from community-piped water systems contain mycobacteria [57]. Compared with free-living mycobacteria, mycobacteria associated with biofilms are more resistant to water treatment [58].
Surgical wound infections , including cataract excision, corneal graft, laser surgery, extremity amputations, dacryocystorhinostomy, plastic surgery of the face, prosthetic hip or knee insertions, coronary artery bypass, excision of basal cell carcinoma, augmentation mammaplasty, and cosmetic surgeries including liposuction and liposculpture, clinically present in a similar fashion to accidental trauma [11, 59,60,61,62,63,64]. After an incubation period of 2–8 weeks, the healing wound will develop serous drainage and redness. Localized nodular areas adjacent to the incision may develop which are often painful and may require incision and drainage. Isolates of the M. fortuitum group are most commonly recovered in these settings, but other species may also be involved [11, 64]. Rare cases of M. wolinskyi infection have been reported, mainly skin and soft tissue infection following surgery including cosmetic procedures [65,66,67,68]. Additionally, pseudo-outbreaks of M. abscessus or M. immunogenum related to contaminated automated bronchoscope disinfection machines, contaminated gastric endoscopes, and laboratory contamination have been described [11, 69, 70].
A recent large nosocomial outbreak of M. abscessus subspecies in lung transplant patients was associated with positive cultures for M. abscessus from patients, biofilms, and water sources obtained from hospital water outlets [71]. Using pulsed-field gel electrophoresis (PFGE), 4 of 10 patients and 8 of 12 environmental cultures showed the same strain of M. abscessus. Multiple interventions were made, and the incidence rate of M. abscessus decreased from 3.9 cases/month during the outbreak period to 1 case/month during the intervention period. This decrease in incidence showed that the outbreak of clonally related pulmonary M. abscessus was epidemiologically linked to the water sources and amenable to targeted infection control efforts [71]. Please see chapter “Environmental Niches for NTM and Their Impact on NTM Disease” for a more extensive discussion of nosocomial RGM disease.
Catheter-Related Infections
The most common healthcare-associated NTM disease since the 1990s has been central venous catheter infections . These may manifest as occult bacteremia, granulomatous hepatitis, septic lung infiltrates, tunnel infections, or exit site infections [11]. The timing of these infections usually involves catheters that have been in place at least several months. The most frequent etiologic agent is M. fortuitum, although pigmented species such as M. neoaurum and M. bacteremicum have also been associated with catheter sepsis [72,73,74,75]. Other long-term catheters, including chronic peritoneal dialysis catheters, hemodialysis catheters, nasolacrimal duct catheters, and ventriculoperitoneal shunts also have been associated with RGM infection [4, 76, 77]. Removal of catheters is necessary for successful treatment.
Disseminated Cutaneous Infections
One type of RGM skin involvement occurs in patients who require chronic steroid therapy and is characterized by the presence of multiple noncontiguous nodules with spontaneous drainage on one or more extremities. These multiple skin lesions develop without life-threatening sequelae and almost always involve the lower extremity and are typically due to M. chelonae [11]. Steroid doses may be as low as 5–10 mg of prednisone daily. The most common underlying disease is rheumatoid arthritis but may also include organ transplants and chronic autoimmune disorders [11]. The patients are frequently asymptomatic except for the local discomfort of the lesions.
A second type of disseminated skin disease is seen in immune-compromised patients, some with rapidly fatal disorders such as poorly controlled hematologic malignancies [11, 77, 78]. This type of infection is usually systemic, with positive cultures of the blood and bone marrow. A portal of entry for the organism is rarely identified, although central catheters may be involved. It is usually caused by M. abscessus and, combined with the underlying disease, was often fatal in the era before current antimicrobial therapy was available. Interestingly, members of the M. fortuitum and M. mucogenicum groups are rarely associated with either type of disseminated disease [11, 79]. As with most infections associated with immune suppression, reversal of the immune suppression is necessary for adequate treatment response for the RGM pathogen.
Ophthalmic Infections
A recent study of 100 patients with nontuberculous mycobacterial ophthalmic infections showed that 95% of the infections were due to RGM, commonly M. chelonae and M. abscessus [80]. Ophthalmic infections due to RGM are often associated with poor visual outcomes despite aggressive treatment [81,82,83].
Nail Salon/Footbath-Associated Folliculitis
RGM lower extremity skin infections involving M. fortuitum, M. mageritense, and a newly described species, M. cosmeticum, is associated with the use of contaminated nail salon whirlpool footbaths [81,82,83]. Patients were salon customers with persistent skin infections below the knee [83]. Most often the infections involved a furunculosis of the lower leg hair follicles [82]. The disease pathogenesis likely results from microtrauma caused by shaving the legs prior to pedicures and footbath water that is heavily contaminated with RGM due to failure to routinely clear the footbath filters [82,83,84].
Anti-TNF-α Therapy-Associated Infections
NTM infections associated with the use of biologic therapies that inhibit tumor necrosis factor alpha (TNF-α) have been reported and are discussed in detail in chapters “Vulnerability to Nontuberculous Mycobacterial Lung Disease or Systemic Infection Due to Genetic/Heritable Disorders and Immune Dysfunction and Nontuberculous Mycobacterial Disease”. Patients receiving anti-TNF-α therapy are at high risk for activation of tuberculosis and appear to have some increase in disease risk or difference in clinical manifestation for NTM as well [85]. A recent review of the US Food and Drug Administration MedWatch database reports identified 239 possible cases of NTM disease associated with TNF-α inhibitor use from 1999 to 2006 of which 105 cases (44%) met NTM disease criteria. NTM infections were associated with immunosuppressive therapies including infliximab, etanercept, and adalimumab, while 65% and 55% of patients were also taking prednisone and methotrexate, respectively. Infections with MAC were most commonly reported, while 20/105 cases (20%) involved RGM species including M. abscessus, M. chelonae, and M. fortuitum [85].
Interferon-Gamma/Interleukin 12 (IFN- γ/IL-12)-Associated Infections
IFN-γ/IL12 is an immunological pathway designed for intracellular killing of mycobacteria and is discussed in more detail in chapter “Vulnerability to Nontuberculous Mycobacterial Lung Disease or Systemic Infection Due to Genetic/Heritable Disorders”. An apparently acquired autoantibody-mediated immunodeficiency was recently described and found to be almost exclusively among Asian-born women [86, 87]. Most cases related to NTM were associated with MAC; however, recent reports suggest that approximately 45% of the NTM cases are due to RGM including M. abscessus (32%) and M. fortuitum (12%). Infections were typically multifocal affecting lymph nodes, osteoarticular tissue, lungs, skin, and/or soft tissues. IFN-γ autoantibodies should be considered in cases of unexplained disseminated NTM infection , especially in the Asian-born population. [86, 87].
Drug Therapy/Drug Resistance
Antimicrobial Susceptibility
Antimicrobial regimens for disease caused by the RGM are usually based upon their in vitro susceptibility patterns. While this approach is appealing from a traditional infectious diseases perspective, it is frequently frustrating with limited practical applicability [11, 42, 88,89,90,91,92,93,94]. Recognizing those limitations is a prerequisite for successful RGM patient treatment. RGM isolates are not susceptible to the first-line antituberculous drugs and require in vitro susceptibility testing in specialized laboratories that are experienced in processing RGM. The current drugs that should be tested for susceptibility include amikacin, cefoxitin, imipenem, moxifloxacin, meropenem, sulfamethoxazole or trimethoprim-sulfamethoxazole, clarithromycin, ciprofloxacin, doxycycline/minocycline, linezolid, and tobramycin (the latter only for isolates of M. chelonae) [90]. Tigecycline is frequently included in routine testing, but no minimum inhibitory concentration (MIC) breakpoints have been determined [88, 89].
Clarithromycin inhibits all RGM isolates with no functional erm gene, including M. chelonae and M. abscessus subsp. massiliense at a concentration of 4 μg/ml at 3 days [90]. The MICs for several species, including M. abscessus subsp. abscessus, M abscessus subsp. bolletii, and M. fortuitum may be in the susceptible range with only 3 days of incubation but due to the presence of the erm gene become resistant with a 14-day macrolide incubation. Most RGM species that have late intrinsic resistance to clarithromycin contain an inducible erm gene [91,92,93,94]. The finding of the erm gene in the RGM helps explain the lack of effectiveness for macrolide therapy despite ostensibly “susceptible” routine in vitro MICs with standard (3 days) incubation times.
It cannot be overemphasized that routine in vitro macrolide susceptibility testing that does not include macrolide preincubation of the RGM isolate for 14 days is not reliable and cannot be used for basing treatment decisions [92]. In 2011, the Clinical and Laboratory Standards Institute (CLSI) recommended the final reading of the clarithromycin MICs for RGM at 14 days, to detect inducible resistance [88]. Alternatively, the need for extended incubation could be eliminated for isolates where erm gene functionality has been molecularly determined by erm gene sequencing [89].
Multiple studies have shown that patients with RGM lung disease due to an erm gene inactive isolate respond significantly more favorably to therapy than patients with an erm gene active RGM [95, 96]. Because of the impact on treatment response, determining the erm gene functionality of clinically significant RGM isolates is absolutely essential, either with preincubation of the RGM isolate in the presence of macrolide or by molecular methods. Clinicians can also be confident that RGM isolates accurately identified as M. chelonae or M. abscessus subsp. massiliense do not have an active erm gene and will respond to macrolide-containing regimens.
For antibiotics other than the macrolides, the terms “susceptible” and “resistant” have limited meaning as treatment regimens based on these designations are not predictably effective. In general, isolates of M. abscessus (all subspecies) and M. chelonae are more resistant to antibiotics than other RGM species and are usually susceptible or intermediate only to amikacin, imipenem, and clarithromycin, in the absence of an active erm gene [11]. Isolates of M. abscessus (all subspecies) are moderately susceptible (intermediate) to cefoxitin (MIC ≤64 μg/mL), whereas isolates of M. chelonae are highly resistant (MIC ≥256 μg/mL). Additionally, MICs of tobramycin for M. chelonae are lower than those of amikacin, so that M. chelonae is the only species of RGM for which amikacin is not the preferred aminoglycoside. Approximately 20% of the strains of M. chelonae are also susceptible to achievable serum levels of ciprofloxacin and/or doxycycline or minocycline [11, 97] (Table 4).
Amikacin is an important antibiotic in RGM treatment regimens. An amikacin resistance breakpoint MIC of >64 μg/mL (compared to ≥64 μg/mL for IV amikacin) has been proposed to the CLSI for inhaled amikacin and has been correlated with the finding of a mutation in the 23S rRNA gene [89, 98]. A recent randomized placebo controlled trial of inhaled liposomal amikacin in patients with MAC and M. abscessus lung disease demonstrated the efficacy of inhaled amikacin in Mycobacterium avium complex (MAC), but only a small number of conversions occurred in patients with M. abscessus [99].
Among the oxazolidinones, linezolid has in vitro activity against the M. fortuitum group and M. chelonae [100]. Linezolid has been used subsequently in the treatment of infections due to RGM, including disseminated M. chelonae with acquired mutational resistance to clarithromycin [101]. Isolates of M. abscessus have variable susceptibility to linezolid. Recently a new oxazolidinone, tedizolid, has shown early in vitro activity among isolates of RGM [102]. No clinical experience in the treatment of RGM disease has been reported so far with this antibiotic.
Tigecycline , a glycylcycline derivative of minocycline, has shown excellent in vitro activity against all species of RGM, including M. chelonae, M. abscessus, and M. fortuitum group with MICs of <1 μg/mL [97]. A clinical trial of patients treated with tigecycline showed limited efficacy of the drug for salvage therapy of patients with respiratory M. abscessus infections [103]. However, MIC breakpoints for this agent with the RGM have not been established so that tigecycline MICs are reported without interpretation [89].
Clofazimine , a riminophenazine antibiotic, has been used in the treatment of M. leprae and multidrug-resistant (MDR) M. tuberculosis. Recently there has been a revival of interest in its efficacy against RGM, especially M. chelonae and M. abscessus. Synergism between clofazimine and amikacin against M. abscessus was demonstrated in vitro [104, 105]. Clofazimine may also act to increase exposure to other important antimicrobials including macrolides. There are no CLSI breakpoints available yet for the interpretation of clofazimine MICs, and large prospective clinical studies have not been done. A recent retrospective study of 42 patients treated with clofazimine as part of multidrug treatment regimens for M. abscessus subsp. abscessus found a 24% sputum conversion rate and 81% treatment response rate based on symptoms with 31% radiographic response [106]. Although clofazimine MICs are frequently reported and the drug appears to be widely used, the clinical efficacy of clofazimine for treating M. abscessus subsp. abscessus remains unclear and its role in this context not yet established. As with most aspects of this difficult process, further studies are necessary.
The new diarylquinolone antibiotic, bedaquiline , was recently approved by the FDA to treat multidrug-resistant (MDR) tuberculosis. It causes disruption of ATP synthesis and has impressive in vitro activity against isolates of NTM including M. abscessus subspecies. In a study of four patients with M. abscessus lung infection, two patients had microbiologic improvement (i.e., decrease in semiquantitative colony counts), and all but one patient showed symptomatic improvement [107]. Large clinical studies along with in vitro susceptibility studies, however, remain to be performed.
A 2014 in vitro study showed the lack of bactericidal antibiotics , including amikacin, in the currently recommended treatment regimens for M. abscessus [108]. This finding was hypothesized to be due to the presence of functional aminoglycoside-modifying enzymes encoded by specific genes in the M. abscessus chromosome [108]. In vitro studies, such as this, emphasize the need for novel antibiotics and/or therapeutic options to improve the therapeutic outcome of patients with RGM, especially M. abscessus [108, 109].
Isolates of the M. fortuitum group, M. smegmatis group, and M. mucogenicum group are generally the most susceptible of the commonly encountered RGM species [6, 11]. In vitro, they are usually susceptible or intermediate to amikacin, cefoxitin, imipenem, ciprofloxacin, sulfonamides, and moxifloxacin, with about 50% of the isolates of M. fortuitum susceptible to doxycycline (Table 4). Both minocycline and doxycycline are preferred over tetracycline because of greater in vitro activity of the former two antimicrobials in previous studies of the RGM [97].
Treatment of RGM Disease
Therapy for most RGM infections has not been established from clinical trials. Current recommendations are generally based on uncontrolled case series and clinical experience. There is a clear dichotomy in the anticipated response of RGM pathogens to therapy. Infections caused by M. fortuitum group pathogens are usually responsive to antibiotic therapy, while infections due to M. abscessus subsp. are usually less responsive to antibiotic therapy.
Effective therapy for many RGM, especially M. abscessus subsp. abscessus, is thwarted by two major mechanisms of drug resistance. The first is innate or natural drug resistance best illustrated by the erm gene whereby initial, routine, MICs for macrolides appear susceptible, but subsequent MICs after macrolide exposure show resistance consistent with the activation of the inducible macrolide resistance gene [91,92,93,94, 109]. While the description of the erm gene has opened windows into the perplexing and complicated realm of innate antibiotic resistance, it is by no means the end of the story. M. abscessus subsp. abscessus possesses multiple innate drug resistance mechanisms that frustrate antibiotic therapy [109].
Patients infected with M. abscessus with a nonfunctional erm(41) gene, primarily those due to M. abscessus subsp. massiliense, have the best prognosis as they are macrolide susceptible [96, 109]. The prognostic difference between an RGM pathogen with an active versus an inactive erm gene is so critical that it necessitates a pause at this point in the narrative to explicitly emphasize this concept. When a clinician is faced with an RGM infection, especially one due to an organism identified as “M. abscessus,” the clinician must know the functional status of the erm gene from that organism. The erm gene status can usually be deduced from the identification of the organism but must be corroborated after incubation of the organism in the presence of macrolide for 14 days. Identification of an organism as M. abscessus subsp. massiliense will inevitably mean the organism does not have an active erm gene. Identification of an organism as M. abscessus subsp. abscessus does not inevitably mean that the organism will have an active erm gene as approximately 20% of these isolates will have an erm gene mutation that renders it nonfunctional [110]. The clinician must have both taxonomic and erm gene functional status for all clinically significant RGM isolates. It is imperative that the clinician is familiar with the method used to determine in vitro macrolide susceptibility.
The second mechanism of resistance is through acquired mutational drug resistance in isolates that do not have an active erm gene such as Mycobacterium abscessus subsp. massiliense, M. chelonae, and approximately 20% of M. abscessus subsp. abscessus isolates [109]. Mutational drug resistance can develop on therapy and is a concern for ribosomal active drugs, such as clarithromycin (23S rRNA gene) and amikacin (16S rRNA gene). The mechanism of acquired mutational resistance for these organisms is the same as for all mycobacteria, inadequate companion medications to prevent the emergence of isolates with naturally occurring ribosomal gene mutations. The recognition that clinically significant RGM isolates without erm gene activity can subsequently develop acquired mutational macrolide resistance dictates that these isolates must be treated with adequate companion medications for macrolide to prevent the emergence of acquired mutational macrolide resistance .
The difference in clinical response for M. abscessus subspecies with and without active erm genes is profound [95, 111,112,113,114]. It would be extraordinarily disappointing for a patient with M. abscessus subsp. abscessus disease who was fortunate enough to have an inactive erm gene to become macrolide resistant because of inappropriate therapy resulting in acquired mutational macrolide resistance. Protection against the emergence of acquired mutational amikacin resistance is equally as important. Physicians must treat these patients with adequate aggressiveness to prevent acquired mutational resistance. This is, yet again, another reminder that there are no shortcuts in the management of these infections.
Mutational resistance is also a concern for the quinolones. Hence, therapy with these agents for organisms such as M. chelonae and M. fortuitum should include combination therapy, especially for extensive disease with large numbers of organisms. Acquired mutational resistance with the tetracyclines and sulfonamide monotherapy has not been described.
Treatment of M. abscessus lung disease is impeded not only by the antibiotic resistance of the organisms but by the complexity, expense, and toxicity of the required antibiotics [42]. See Tables 4 and 5 for a summary of drugs and suggested therapeutic approaches.
A critical evaluation, comparison, and summary of the literature reporting treatment outcomes for “M. abscessus” are impossible for studies done prior to knowledge and demonstration of erm gene activity . Prior to erm gene analysis, published M. abscessus case series included variable numbers of patients with erm gene active (M. abscessus subsp. abscessus) and erm gene inactive (M abscessus subsp. massiliense) patients which explains the wide variability in reported treatment responses. For instance, in one study from the United States, 69 M. abscessus lung disease patients without subspecies identification or reported erm gene activity were aggressively treated for 52 antibiotic months, including 6 months parenteral antibiotic therapy and surgery in 33% of cases [115]. Forty-eight percent of patients were AFB culture negative by the end of the study including 57% of the patients who had surgery [115]. In a retrospective study from the Republic of Korea, 65 patients with M. abscessus lung disease were treated with 1 month parenteral and oral antibiotics followed by 24 months oral antibiotics usually including a macrolide [116]. Sputum conversion and maintenance of negative sputum cultures for ≥12 months were achieved in 58%. In another study from the Republic of Korea 41 patients, 41% received macrolide and one parenteral agent while 59% received a macrolide and 2 parenteral agents [117]. Sputum conversion was achieved in 81% of patients without a difference between the two groups. It is clear that the improved outcomes in the Korean studies cited above were due to a much higher prevalence of M. abscessus subsp. massiliense patients in the study cohorts compared to the US cohorts.
In a subsequent study from the Republic of South Korea with subspecies organism identification, sputum conversion and maintenance of culture negativity occurred in 88% of 33 patients with M. massiliense lung disease compared with only 25% of 24 patients with M. abscessus subsp. abscessus infection [95]. Similar results were reported in a Japanese study that evaluated 62 patients and found higher sputum conversion rates (50% vs 31%) and lower relapse rates (30% vs 65%) in patients with M. abscessus subsp. massiliense lung disease compared with M. abscessus subsp. abscessus lung disease [118]. In a prospective cohort of 16 M. abscessus subsp. massiliense and 27 M. abscessus subsp. abscessus lung infection cases with CF, clarithromycin-based combination therapies led to mycobacterial eradication in 100% of M. massiliense cases but only in 27% of M. abscessus cases [119].
The preponderance of patients with erm gene inactive M. abscessus subsp. massiliense not only explains the improved treatment outcomes reported in the Republic of Korea compared with the United States but also the success of less aggressive treatment regimens with only brief exposure to parenteral medications and long-term oral antibiotic therapy including macrolide monotherapy [120]. While attractive from the standpoint of patient convenience and avoidance of drug toxicity, this approach has been reported to result in acquired macrolide resistance and is not recommended [95, 111,112,113,114].
It cannot be emphasized too strongly that patients with macrolide susceptible M. abscessus subsp. abscessus isolates because of an inactive erm gene are vulnerable to acquired mutational macrolide resistance due to mutations in the 23S rRNA gene. These mutations emerge during therapy with inadequate companion medications for the macrolides. This development is especially pernicious because it signals a significant decline in the chances for successful therapy of the patient [95, 111,112,113,114]. We are concerned by the recommendations for oral drugs of uncertain, even dubious, activity as companions for macrolides against M. abscessus isolates that do not have an active erm gene, and we strongly disagree with this approach [121]. It perhaps doesn’t matter what oral drugs are used with erm gene active M. abscessus subsp. abscessus, but the creation of acquired mutational macrolide resistance for these difficult to treat organisms is an incalculable disservice to the patient. Expert consultation for management of RGM lung disease patients should occur prior to the advent of acquired mutational macrolide resistance.
So far, there is no consensus on the optimal composition of multidrug therapy for M. abscessus subsp. abscessus with the exception of the necessity for including a macrolide for patients with an inactive erm gene. The therapy of the patient is directed by the erm gene activity analysis and in vitro macrolide susceptibility status. Patients who are macrolide susceptible unquestionably have a much greater chance of completing successful therapy than those patients with macrolide-resistant isolates. For erm gene active isolates, there is also consensus that amikacin is an important element in the therapeutic regimen.
Our approach to patients with RGM diseases including lung disease is to treat with the intent to eradicate the infection (Fig. 4a–d). We recognize that this approach is not universally accepted due to extensive RBM drug resistance and the need for potentially toxic parenteral medications in a prolonged multidrug treatment regimen. We also do not promote the concept of “induction” and “maintenance” therapy for RGM in general and M. abscessus subsp. abscessus in particular. First, those concepts make pathophysiologic sense for tuberculosis, but we are not aware of information that supports similar pathophysiology for RGM lung disease. Second, also in contrast to TB, there are not a plethora of oral medications with activity against M. abscessus subsp. abscessus to choose from which brings into play the possibility that an erm gene inactive macrolide susceptible M. abscessus subsp. abscessus isolate might undergo macrolide therapy with oral drugs of questionable activity resulting in acquired mutational macrolide resistance.
(a) Chest CT cut from 71-year-old man with M. abscessus subsp. abscessus lung disease and right apical cavitation. (b) Chest CT cut from the same patient showing extensive right upper lobe inflammatory density. (c) Chest CT cut at same level as Fig. 4a showing improvement in cavitary lesions after extended therapy with tigecycline, tedizolid switched to linezolid, and amikacin switched to imipenem for a duration including 12 months sputum culture negativity. (d) Chest CT cut a same level as Fig. 4b showing improvement in extensive inflammatory densities after therapy. (e) Chest CT cut from 62-year-old patient with M. abscessus subsp. abscessus lung disease. Her M. abscessus subsp. abscessus isolate was macrolide susceptible in vitro because the isolate had an erm gene mutation rendering it inactive. (f) Chest CT cut from the same patient at the same level showing closure of the cavity associated with 12 months sputum culture negativity while on therapy. Her treatment consisted of 6 months oral azithromycin and linezolid with intravenous amikacin followed by 8 months oral azithromycin and linezolid with inhaled amikacin
We are also aware that some clinicians, as a result of multiple obstacles, toxicity, and complexities presented by parenteral medication administration, choose to treat patients with relatively short and intermittent regimens. Given the lack of a predictably favorable response to current antibiotic choices, it is hard to argue vehemently against this approach which should be left to the discretion of the patient and treating physician.
We base initial therapy on in vitro susceptibility results, which is clearly not optimal but is the best default approach available in our view. Obviously, an inactive erm gene isolate should be treated with a macrolide (Fig. 4e, f). For M. abscessus subsp. abscessus and M. massiliense, we would then choose at least one parenteral agent, usually amikacin. The next choice would depend on disease severity. For cavitary disease we would choose a second parenteral agent, such as tigecycline, imipenem, or cefoxitin. If the isolate was susceptible in vitro to linezolid, that would be a reasonable third drug choice as well. Some experts would use clofazimine in this situation. As noted, our goal initially is eradication of the organism. We do not a priori assume that any patient is untreatable, although regrettably, a significant proportion of these patients will turn out to be refractory to even aggressive therapeutic efforts (Fig. 5a–d). Our recommendation for a specific treatment strategy is outlined in Table 5.
(a) Chest radiograph from 76-year-old patient with M. abscessus subsp. abscessus lung disease showing nonspecific bilateral densities consistent with bronchiectasis and nontuberculous mycobacterial disease. (b) Chest CT cut from the same patient showing bronchiectasis and nodular densities with tree-in-bud pattern. (c) Chest radiograph showing progressive right lower lung field densities associated with persistently positive sputum cultures for M. abscessus subsp. abscessus in spite of treatment with amikacin, imipenem, and tedizolid switched to linezolid and azithromycin. (d) Chest CT cut at same level as Fig. 5b at same time as chest radiograph in Fig. 5c showing bronchiectasis with increased peribronchial inflammation and early cavitation
For erm gene active M. abscessus subsp. abscessus isolates, we recommend at least two parenteral agents including amikacin plus oral linezolid or clofazimine (Table 5). We do not believe that the inclusion of a macrolide favorably influences the outcome of therapy for these organisms, but the macrolide may have a beneficial effect on bronchiectasis as an immune modulating agent. Mycobacterium bolletii isolates would be treated identically to M. abscessus subsp. abscessus isolates, guided by erm gene activity. As with other NTM respiratory pathogens, the target duration of therapy is 12 months of sputum culture negativity while on therapy.
In the (hopefully) rare situation where a clinician is faced with an M. abscessus isolate of unknown erm gene activity, then we believe it would be reasonable to include a macrolide in the regimen on the small chance that the isolate had an inactive erm gene.
Surgery is an important option for selected patients with M. abscessus disease, especially those with macrolide resistance from any mechanism, and is covered in detail in chapter “Surgical Management of NTM Diseases”. For an organism that is so difficult to eradicate with medication alone, surgery is associated with improved clinical outcomes [115] (Fig. 6a, b). While a minority of patients will be appropriate candidates for adjunctive surgery, for various reasons, we feel that the surgical option should be considered for all M. abscessus patients, even if only briefly to confirm a patient’s non-suitability.
(a) Chest CT cut from 64-year-old female with M. abscessus subsp. abscessus lung disease and persistently positive sputum cultures in spite of aggressive therapy including parenteral antibiotics. (b) Chest CT cut from the same patient at a comparable level to Fig. 6b after right middle lobe lobectomy and 12 months sputum culture negativity following surgery and antibiotic therapy including tigecycline and amikacin
Fortunately, M. fortuitum is usually susceptible in vitro to multiple oral antibiotics with the exception of macrolides due to the presence of an active erm gene. We recommend treatment of M. fortuitum disease with at least two agents to which the organism is susceptible in vitro. Parenteral agents may be necessary for severe or refractory disease. Removal of any foreign body is also essential for successful therapy of extrapulmonary or disseminated M. fortuitum infection associated with foreign material.
M. chelonae does not have an active erm gene and is also frequently more susceptible to oral antibiotics than M. abscessus subsp. abscessus, including macrolide, which offers opportunities for therapy without parenteral agents. It must be emphasized again that monotherapy with macrolide can result in acquired macrolide resistance and worse prognosis.
The general recommendation for serious wound infections is combination therapy with initial parenteral therapy for M. chelonae and M. abscessus until clinically improved, followed by oral therapy for a total treatment duration of at least 6 months. Development of new skin lesions on therapy is not necessarily indicative of treatment failure. Cultures should be obtained, and antibiotic therapy should be continued. In most cases, cultures are sterile following approximately 6–8 weeks of proper treatment. The new skin lesions likely represent a paradoxical immunological response rather than microbiological persistence or relapse. New lesions on therapy are not unexpected but should be aggressively evaluated including new AFB cultures. As long as cultures of these new lesions remain negative, treatment should be continued for a minimum of 4 months for less serious infections and 6 months for more serious infections. Abscess drainage and surgical debridement are essential. Surgical debridement may be necessary more than once. Cultures for AFB must be sent with each biopsy and debridement procedure. Sadly, this simple requirement is not always met.
In summary, the management of RGM infections in general and M. abscessus infections, specifically, remains challenging. There are many confounding aspects to RGM disease from nomenclature to drug resistance mechanisms that confuse or intimidate clinicians caring for these patients. Given those unfavorable circumstances, there is no other group of NTM organism that require as much knowledge by the clinician for optimal patient management. The clinician must have accurate organism identification and must know the significance of in vitro susceptibility results. With that knowledge, the clinician must craft drug treatment regimens that, at a minimum, do not make the patient’s status worse. There is simply no substitute for an in-depth understanding by the clinician of the nuances and idiosyncrasies of RGM disease and no short cuts in the management of these patients (Table 6).
References
Cobbett L. An acid-fast bacillus obtained from a pustular eruption. Br Med J. 1918;2:158.
Runyon H. Conservation of the specific epithet fortuitum in the name of the organism known as Mycobacterium fortuitum da Costa Cruz. Int J Syst Bacteriol. 1972;22:50–1.
Moore M, Frerichs JB. An unusual acid fast infection of the knee with subcutaneous, abscess-like lesions of the gluteal region: report of a case study with a study of the organism, Mycobacterium abscessus. J Investig Dermatol. 1953;20:133–69.
Schinsky MF, Morey RE, Steigerwalt AG, Douglas MP, Wilson RW, Floyd MM, Butler WR, Daneshvar MI, Brown-Elliott BA, Wallace RJ Jr, McNeil MM, Brenner DJ, Brown JM. Taxonomic variation in the Mycobacterium fortuitum third-biovariant complex: description of Mycobacterium boenickei sp. nov., Mycobacterium houstonense sp. nov., Mycobacterium neworleansense sp. nov., Mycobacterium brisbanense sp. nov., and recognition of Mycobacterium porcinum from human clinical isolates. Int J Syst Evol Microbiol. 2004;54:1653–67.
Adékambi T, Berger P, Raoult D, Drancourt M. rpoB gene sequence-based characterization of emerging non-tuberculous mycobacteria with descriptions of Mycobacterium bolletii sp. nov., M. phocaicum sp. nov. and Mycobacterium aubagnense sp. nov. Int J Syst Evol Microbiol. 2006;56:133–43.
Brown-Elliott BA, Wallace RJ Jr. Mycobacterium: clinical and laboratory characteristics of rapidly growing mycobacteria. In: Manual of clinical microbiology, vol. 1. 11th ed. Washington, D.C: ASM Press; 2015.
Brown BA, Springer B, Steingrube VA, Wilson RW, Pfyffer GE, Garcia MJ, Menendez MC, Rodriguez-Salgado B, Jost KC Jr, Chiu SH, Onyi GO, Bottger EC, Wallace RJ Jr. Mycobacterium wolinskyi sp. nov. and Mycobacterium goodii sp. nov., two new rapidly growing species related to Mycobacterium smegmatis and associated with human wound infections: a cooperative study from the international working group on mycobacterial taxonomy. Int J Syst Bacteriol. 1999;49:1493–511.
Wallace RJ Jr, Brown-Elliott BA, Wilson RW, Mann L, Hall L, Zhang Y, Jost KC Jr, Brown JM, Kabani A, Schinsky MF, Steigerwalt AG, Crist CJ, Roberts GD, Blacklock Z, Tsukamura M, Silcox V, Turenne C. Clinical and laboratory features of Mycobacterium porcinum. J Clin Microbiol. 2004;42:5689–97.
Jiménez MS, Campos-Herrero MI, García D, Luquin M, Herrera L, García MJ. Mycobacterium canariasense sp. nov. Int J Syst Evol Microbiol. 2004;54:1729–34.
Whipps CM, Butler WR, Pourahmad F, Watral VG, Kent ML. Molecular systematics support the revival of Mycobacterium salmoniphilum (ex Ross 1960) sp. nov., nom. Rev., a species closely related to Mycobacterium chelonae. Int J Syst Evol Microbiol. 2007;57:2525–31.
Brown-Elliott BA, Wallace RJ Jr. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev. 2002;15:716–46.
Adékambi T, Drancourt M. Dissection of phylogenetic relationships among nineteen rapidly growing mycobacterium species by 16S r-RNA, hsp65, sodA, recA, and rpoB gene sequencing. Int J Syst Evol Microbiol. 2004;54:2095–105.
Leao SC, Tortoli E, Viana-Niero C, Ueki SYM, Batista Lima KV, Lopes ML, Yubero J, Menendez MC, Garcia MJ. Characterization of mycobacteria from a major Brazilian outbreak suggests a revision of the taxonomic status of members of the Mycobacterium chelonae-abscessus group. J Clin Microbiol. 2009;47:2691–8.
Leao SC, Tortoli E, Euzeby JP, Garcia MJ. Proposal that Mycobacterium massiliense and Mycobacterium bolletii be united and reclassified as Mycobacterium abscessus subsp. bolletii comb. nov., designation of Mycobacterium abscessus subsp. abscessus subsp. nov. an amended description of Mycobacterium abscessus. Int J Syst Evol Microbiol. 2011;61:2311–3.
Zelazny AM, Root JM, Shea YR, Colombo RE, Shamputa IC, Stock F, Conlan SS, McNulty S, Brown-Elliott BA, Wallace RJ Jr, Olivier KN, Holland SM, Sampaio EP. Cohort study of molecular identification and typing of Mycobacterium abscessus, Mycobacterium massiliense and Mycobacterium bolletii. J Clin Microbiol. 2009;47:1985–95.
Tortoli E, Kohl TA, Trovato A, Garcia MJ, Leao SC, Baldan R, Campana S, Cariani L, Colombo C, Costa D, Pizzamiglio G, Rancoita PM, Russo MC, Simonetti TM, Sottotetti S, Taccetti G, Teri A, Niemann S, Cirillo DM, Brown-Elliott BA, Wallace Jr. RJ. Emended description of Mycobacterium abscessus, Mycobacterium abscessus subsp. abscessus, Mycobacterium abscessus subsp. bolletii and designation of Mycobacterium abscessus subsp. massiliense subsp. nov. Int J Syst Evol Microbiol. 2016; In press.
Tettelin H, Davidson RM, Agrawal S, Aitken ML, Shallom S, Hasan NA, Strong M, de Moura VCN, De Groote MA, Duarte RS, Hine E, Parankush S, Su Q, Daugherty SC, Fraser CM, Brown-Elliott BA, Wallace RJ Jr, Holland SM, Sampaio EP, Olivier KN, Jackson M, Zelazny AM. High-level relatedness among Mycobacterium abscessus subsp. massiliense strains from widely separated outbreaks. Emerg Infect Dis. 2014;20:364–71.
Adekambi T, Sassi M, van Ingen J, Drancourt M. Reinstating Mycobacterium massiliense and Mycobacterium bolletii as species of the Mycobacterium abscessus complex. Int J Syst Evol Microbiol. 2017;67(8):2726–30.
Kim K, Hong S-H, Kim B-J, Kim B-R, Lee S-Y, Kim G-N, Shim TS, Kook Y-H, Kim B-J. Separation of Mycobacterium abscessus into subspecies or genotype level by direct application of peptide nucleic acid multi-probe-real-time PCR method into sputa samples. BMC Infect Dis. 2015;15:325–31.
Tan JL, Ngeow YF, Choo SW. Support from phylogenomic networks and subspecies signatures for separation of Mycobacterium massiliense from Mycobacterium bolletii. J Clin Microbiol. 2015;53:3042–6.
Tortoli E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev. 2014;27:727–52.
Buckwalter SP, Olson SL, Connelly BJ, Lucas BC, Rodning AA, Walchak RC, Deml SM, Wohlfiel SL, Wengenack NL. Evaluation of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of Mycobacterium species, Nocardia species, and other aerobic actinomycetes. J Clin Microbiol. 2016;54:376–84.
Saleeb PG, Drake SK, Murray PR, Zelazny AM. Identification of mycobacteria in solid-culture media by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2011;49:1790–4.
Tortoli E, Nanetti A, Piersimoni C, Cichero P, Farina C, Mucignat G, Scarparo C, Bartolini L, Valentini R, Nista D, Gesu G, Passerini Tosi C, Crovatto M, Brusarosco G. Performance assessment of new multiplex probe assay for identification of mycobacteria. J Clin Microbiol. 2001;39:1079–84.
Tortoli E, Pecorari M, Fabio G, Messinò M, Fabio A. Commercial DNA probes for mycobacteria incorrectly identify a number of less frequently encountered species. J Clin Microbiol. 2010;48:307–10.
Tortoli E. Impact of genotypic studies on mycobacterial taxonomy: the new mycobacteria of the 1990s. Clin Microbiol Rev. 2003;16:319–54.
Steingrube VA, Gibson JL, Brown BA, Zhang Y, Wilson RW, Rajagopalan M, Wallace RJ Jr. PCR amplification and restriction endonuclease analysis of a 65-kilodalton heat shock protein gene sequence for taxonomic separation of rapidly growing mycobacteria [ERRATUM 1995;33:1686]. J Clin Microbiol. 1995;33:149–53.
Telenti A, Marchesi F, Balz M, Bally F, Böttger EC, Bodmer T. Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol. 1993;31:175–8.
McNabb A, Eisler D, Adie K, Amos M, Rodrigues M, Stephens G, Black WA, Isaac-Renton J. Assessment of partial sequencing of the 65-kilodalton heat shock protein gene (hsp65) for routine identification of Mycobacterium species isolated from clinical sources. J Clin Microbiol. 2004;42:3000–11.
Adékambi T, Reynaud-Gaubert M, Greub G, Gevaudan MJ, La Scola B, Raoult D, Drancourt M. Amoebal coculture of “Mycobacterium massiliense” sp. nov. from the sputum of a patient with hemoptoic pneumonia. J Clin Microbiol. 2004;42:5493–501.
Adékambi T, Colson P, Drancourt M. rpo B-based identification of nonpigmented and late pigmented rapidly growing mycobacteria. J Clin Microbiol. 2003;41:5699–708.
Kim H-Y, Kook Y, Yun Y-J, Park CG, Lee NY, Shim TS, Kim B-J, Kook Y-H. Proportion of Mycobacterium massiliense and Mycobacterium bolletii in strains among Korean Mycobacterium chelonae-Mycobacterium abscessus group isolates. J Clin Microbiol. 2008;46:3384–90.
Forbes BA, Banaiee N, Beavis KG, Brown-Elliott BA, Della Latta P, Elliott LB, Hall GS, Hanna B, Perkins MD, Siddiqi SH, Wallace Jr. RJ, Warren NG. Laboratory detection and identification of mycobacteria; approved guideline. CLSI document M48-A. 2008.
Ngeow YF, Wee WY, Wong YL, Tan JL, Ongi CS, Ng KP, Choo SW. Genomic analysis of Mycobacterium abscessus strain M139, which has an ambiguous subspecies taxonomic position. J Bacteriol. 2012;194:6002–3.
Ngeow YF, Wong YL, Lokanathan N, Wong GJ, Ong CS, Ng KP, Choo SW. Genomic analysis of Mycobacterium massiliense strain M115, an isolate from human sputum. J Bacteriol. 2012;194:4786.
Ngeow YF, Wong YL, Tan JL, Arumugam R, Wong GJ, Ong CS, Ng KP, Choo SW. Genome sequence of Mycobacterium massiliense M18, isolated from a lymph node biopsy specimen. J Bacteriol. 2012;194:4125.
Tettelin H, Sampaio EP, Daugherty SC, Hine E, Riley DR, Sadzewicz L, Sengamalay N, Shefchek K, Su Q, Tallon LJ, Conville P, Olivier KN, Holland SM, Fraser CM, Zelazny AM. Genomic insights into the emerging human pathogen Mycobacterium massiliense. J Bacteriol. 2012;194:5450.
Chan J, Halachev M, Yates E, Smith G, Pallen M. Whole-genome sequence of the emerging pathogen Mycobacterium abscessus strain 47J26. J Bacteriol. 2012;194:549.
Bryant JM, Grogono DM, Greaves D, Foweraker J, Roddick I, Inns T, Reacher M, Haworth CS, Curran MD, Harris SR, Peacock SJ, Parkhill J, Floto RA. Whole-genome sequencing to identify transmission of Mycobacterium abscessus between patients with cystic fibrosis: a retrospective cohort study. Lancet. 2013;381:1551–60.
Davidson RM, Hasan N, Reynolds PR, Totten S, Garcia B, Levin A, Ramamoorthy P, Heifets L, Daley CL, Strong M. Genome sequencing of Mycobacterium abscessus isolates from patients in the United States and comparisons to globally diverse clinical strains. J Clin Microbiol. 2014;52:3573–82.
Wolinsky E. State of the art: nontuberculous mycobacterial and associated disease. Am Rev Respir Dis. 1979;119:107–59.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K. An official ATS/IDSA statement: diagnosis, treatment and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416.
Thomson R, Tolson C, Sidjabat H, Huygens F, Hargreaves M. Mycobacterium abscessus isolated from municipal water - a potential source of human infection. BMC Infect Dis. 2013;13:241.
Falkinham JO. The changing pattern of nontuberculous mycobacterial disease. Can. J Infect Dis. 2003;14:281–6.
Griffith DE, Philley JV, Brown-Elliott BA, Benwill JL, Shepherd S, York D, Wallace RJ Jr. The significance of Mycobacterium abscessus subspecies abscessus isolation during Mycobacterium avium complex lung disease therapy. Chest. 2015;147(5):1369–75.
Jun HJ, Jeon K, Um SW, Kwon OJ, Lee NY, Koh WJ. Nontuberculous mycobacteria isolated during the treatment of pulmonary tuberculosis. Respir Med. 2009;103(12):1936–40.
Cullen AR, Cannon CL, Mark EJ, Colin AA. Mycobacterium abscessus infection in cystic fibrosis. Am J Respir Crit Care Med. 2000;161:641–5.
Fauroux B, Delaisi B, Clément A, Saizou C, Moissenet D, Truffot-Pernot C, Tournier G, Vu Thien H. Mycobacterial lung disease in cystic fibrosis: a prospective study. Pediatr Infect Dis J. 1997;16:354–8.
Olivier KN, Weber DJ, Wallace RJ Jr, Faiz AR, Lee J-H, Zhang Y, Brown-Elliott BA, Handler A, Wilson RW, Schechter MS, Edwards LJ, Chakraborti S, Knowles MR, Group ftNMiCFS. Nontuberculous mycobacteria. I. Multicenter prevalence study in cystic fibrosis. Am J Respir Crit Care Med. 2003;167:828–34.
Aitken ML, Limaye A, Pottinger P, Whimbey E, Goss GH, Tonelli MR, Cangelosi GA, Ashworth M, Olivier KN, Brown-Elliott BA, Wallace RJ Jr. Respiratory outbreak of Mycobacterium abscessus subspecies massiliense in a lung transplant and cystic fibrosis center. Letter to the Editor Am J Respir Crit Care Med. 2012;185:231–3.
Roux A-L, Catherinot E, Ripoll F, Soismier N, Macheras E, Ravilly S, Bellis G, Vibet M-A, Le Roux E, Lemonnier L, Gutierrez C, Vincent V, Fauroux B, Rottman M, Guillemot D, Gaillard J-L, Herrman J-L, Group. ftO. Multicenter study of prevalence of nontuberculous mycobacteria in patients with cystic fibrosis in France. J Clin Microbiol. 2009;47:4124–8.
Cândido PHC, De Souza Nunes L, Marques EA, Folescu TW, Coelho FS, Nogueira de Moura VC, da Silva MG, Gomes KM, da Silva Lourenço MC, Aguiar FS, Chitolina F, Armstrong DT, Leão SC, Neves FPG, de Queiroz Mello FC, Duarte RS. 2014. Multidrug-resistant nontuberculous mycobacteria isolated from cystic fibrosis patients. J Clin Microbiol 58:2990–2997 [52] Gubler JGH, Salfinger M, von Graevenitz A. 1992. Pseudoepidemic of nontuberculous mycobacteria due to a contaminated bronchoscope cleaning machine: report of an outbreak and review of the literature. Chest. 101:1245–1249.
Tiwari TSP, Ray B, Jost KC Jr, Rathod MK, Zhang Y, Brown-Elliott BA, Hendricks K, Wallace RJ Jr. Forty years of disinfectant failure: outbreak of postinjection Mycobacterium abscessus infection caused by contamination of benzalkonium chloride. Clin Infect Dis. 2003;36:954–62.
Hector JSR, Pang Y, Mazurek GH, Zhang Y, Brown BA, Wallace RJ Jr. Large restriction fragment patterns of genomic Mycobacterium fortuitum DNA as strain-specific markers and their use in epidemiologic investigation of four nosocomial outbreaks. J Clin Microbiol. 1992;30:1250–5.
Zhang Y, Rajagopalan M, Brown BA, Wallace RJ Jr. Randomly amplified polymorphic DNA PCR for comparison of Mycobacterium abscessus strains from nosocomial outbreaks. J Clin Microbiol. 1997;35:3132–9.
Carson LA, Bland LA, Cusick LB, Favero MS, Bolan GA, Reingold AL, Good RC. Prevalence of nontuberculous mycobacteria in water supplies of hemodialysis centers. App Environ Microbiol. 1988;54:3122–5.
Schulze-Röbbecke R, Janning B, Fischeder R. Occurrence of mycobacteria in biofilm samples. Tuberc Lung Dis. 1992;73:141–4.
Galassi L, Donato R, Tortoli E, Burrini D, Santianni D, Dei R. Nontuberculous mycobacteria in hospital water systems: application of HPLC for identification of environmental mycobacteria. J Water Health. 2003;1:133–9.
Sudesh S, Cohen EJ, Schwartz LW, Myers JS. Mycobacterium chelonae infection in a corneal graft. Arch Ophthalmol. 2000;118:294–5.
Reviglio V, Rodriguez ML, Picotti GS, Paradello M, Luna JD, Juárez CP. Mycobacterium chelonae keratitis following laser in situ keratomileusis. J Refract Surg. 1998;14:357–60.
Saluja A, Peters NT, Lowe L, Johnson TM. A surgical wound infection due to Mycobacterium chelonae successfully treated with clarithromycin. Dermatol Surg. 1997;23:539–43.
Friedman ND, Sexton DJ. Bursitis due to Mycobacterium goodii, a recently described, rapidly growing mycobacterium. J Clin Microbiol. 2001;39:404–5.
Meyers H, Brown-Elliott BA, Moore D, Curry J, Truong C, Zhang Y, Wallace RJ Jr. An outbreak of Mycobacterium chelonae infection following liposuction. Clin Infect Dis. 2002;34:1500–7.
Centers for Disease Control and Prevention. Rapidly growing mycobacterial infection following liposuction and liposculpture—Caracas, Venezuela, 1996-1998. Morb Mortal Wkly Rep. 1998;47:1065.
Nagpal A, Wentink JE, Berbari EF, Aronhalt KC, Wright AJ, Krageschmidt DA, Wengenack NL, Thompson RI, Tosh PK. A cluster of Mycobacterium wolinskyi surgical site infection at an academic medical center. Infect Control Hosp Epidemiol. 2014;35:1169–75.
Dupont C, Terru D, Aguilhon S, Frapier J-M, Paquis M-P, Morquin D, Lamy B, Godreuil S, Parer S, Lotthé A, Jumas-Bilak E, Romano-Bertrand S. Source-case investigation of Mycobacterium wolinskyi cardiac surgical site infection. J Hosp Infect. 2016; In press.
Ariza-Heredia EJ, Databneh AS, Wilhelm MP, Wengenack NL, Razonable RR, Wilson JW. Mycobacterium wolinskyi: a case series and review of the literature. Diagn Microbiol Infect Dis. 2011;71:421–7.
Bossart S, Schnell B, Kerl K, Urosevic-Maiwald M. Ulcers as a sign of skin infection with Mycobacterium wolinskyi: report of a case and review of the literature. Case Rep Dermatol. 2016;8:151–5.
Lai KK, Brown BA, Westerling JA, Fontecchio SA, Zhang Y, Wallace RJ Jr. Long-term laboratory contamination by Mycobacterium abscessus resulting in two pseudo-outbreaks: recognition with use of random amplified polymorphic DNA (RAPD) polymerase chain reaction. Clin Infect Dis. 1998;27:169–75.
Wilson RW, Steingrube VA, Böttger EC, Springer B, Brown-Elliott BA, Vincent V, Jost KC Jr, Zhang Y, Garcia MJ, Chiu SH, Onyi GO, Rossmoore H, Nash DR, Wallace RJ Jr. Mycobacterium immunogenum sp. nov., a novel species related to Mycobacterium abscessus and associated with clinical disease, pseudo-outbreaks, and contaminated metalworking fluids: an international cooperative study on mycobacterial taxonomy. Int J Syst Evol Microbiol. 2001;51:1751–64.
Baker AW, Lewis SS, Alexander BD, Chen LF, Wall S, Wallace RJ Jr, Brown-Elliott BA, Isaacs PJ, Pickett LC, Patel CB, Smith PK, Reynolds JM, Engel J, Wolfe CR, Milano CA, Schroder JN, Davis RD, Hartwig MG, Stout JE, Strittholt N, Maziarz EK, Saullo JH, Hazen KC, Walczak RJ Jr, Vasireddy R, Vasireddy S, CM MK, Anderson DJ, Sexton DJ. A cluster of Mycobacterium abscessus among lung transplant patients: investigation and mitigation. Clin Infect Dis. 2017;64(7):902–11.
Brown-Elliott BA, Wallace RJ Jr, Petti CA, Mann LB, McGlasson M, Chihara S, Smith GL, Painter P, Hail D, Wilson R, Simmon KE. Mycobacterium neoaurum and Mycobacterium bacteremicum sp. nov. as causes of bacteremia. J Clin Microbiol. 2010;48:4377–85.
Raad II, Vartivarian S, Khan A, Bodey GP. Catheter-related infections caused by the Mycobacterium fortuitum complex: 15 cases and review. Rev Infect Dis. 1991;13:1120–5.
Washer LL, Riddell IVJ, Rider J, Chenoweth CE. Mycobacterium neoaurum bloodstream infection: report of 4 cases and review of the literature. Clin Infect Dis. 2007;45:e10–3.
Martínez López AB, Álvarez Blanco O, Ruíz Serrano MJ, Morales San-José MD, Luque de Pablos A. Mycobacterium fortuitum as a cause of peritoneal dialysis catheter port infection. A clinical case and a review of the literature. Nefrologia. 2015;35:584–6.
Al Shaalan M, Law BJ, Israels SJ, Pianosi P, Lacson AG, Higgins R. Mycobacterium fortuitum interstitial pneumonia with vasculitis in a child with Wilms tumor. Pediatr Infect Dis J. 1997;16:996–1000.
Levendoglu-Tugal O, Munoz J, Brudnicki A, Ozkaynak MF, Sandoval C, Jayabose S. Infections due to nontuberculous mycobacteria in children with leukemia. Clin Infect Dis. 1998;27:1227–30.
Tahara M, Yatera K, Yamasaki K, Orihashi T, Hirosawa M, Ogoshi T, Noguchi S, Nishida C, Ishimoto H, Yonezawa A, Tsukada J, Mukae H. Disseminated Mycobacterium abscessus complex infection manifesting as multiple areas of lymphadenitis and skin abscess in the preclinical stage of acute lymphocytic leukemia. Intern Med. 2016;55:1787–91.
Chetchotisakd P, Mootsikapun P, Anunnatsiri S, Jirarattanapochai K, Choonhakarn C, Chaiprasert A, Ubol PN, Wheat LJ, Davis TE. Disseminated infection due to rapidly growing mycobacteria in immunocompetent hosts presenting with chronic lymphadenopathy: a previously unrecognized clinical entity. Clin Infect Dis. 2000;32:29–34.
Brown-Elliott BA, Mann LB, Hail D, Whitney C, Wallace RJ Jr. Antimicrobial susceptibility of nontuberculous mycobacteria from eye infections. Cornea. 2012;31:900–6.
Cooksey RC, de Waard JH, Yakrus MA, Rivera I, Chopite M, Toney SR, Morlock GP, Butler WR. Mycobacterium cosmeticum sp. nov., a novel rapidly growing species isolated from a cosmetic infection and from a nail salon. Int J Syst Evol Microbiol. 2004;54:2385–91.
Gira AK, Reisenauer H, Hammock L, Nadiminti U, Macy JT, Reeves A, Burnett C, Yakrus MA, Toney S, Jensen BJ, Blumberg HM, Caughman SW, Nolte FS. Furunculosis due to Mycobacterium mageritense associated with footbaths at a nail salon. J Clin Microbiol. 2004;42:1813–7.
Winthrop KL, Albridge K, South D, Albrecht P, Abrams M, Samuel MC, Leonard W, Wagner J, Vugia DJ. The clinical management and outcome of nail salon-acquired Mycobacterium fortuitum skin infection. Clin Infect Dis. 2004;38:38–44.
Vugia DJ, Jang Y, Zizek C, Ely J, Winthrop KL, Desmond E. Mycobacteria in nail salon whirlpool footbaths. California Emerg Infect Dis. 2005;11:616–8.
Winthrop KL, Chang E, Yamashita S, Iademarco MF, LoBue PA. Nontuberculous mycobacteria infections and anti-tumor necrosis factor-alpha therapy. Emerg Infect Dis. 2009;15:1556–61.
Czaja CA, Merkel PA, Chan ED, Lenz LL, Wolf ML, Alam R, Franke SK, Fischer A, Gogate S, Perez-Velez CM, Knight V. Rituximab as successful adjunct treatment in a patient with disseminated nontuberculous mycobacterial infection due to acquired anti-interferon-γ autoantibody. Clin. Infect. Dis. In: 58:e-115-118; 2014.
Valour F, Perpoint T, Sénéchal A, Kong X-F, Bustamante J, Ferry T, Chidiac C, Ader A, group obotLTs. Interferon-γ autoantibodies as predisposing factor for nontuberculous mycobacterial infection. Emerg. Infect. Dis. 2016;22:1124–6.
Clinical and Laboratory Standards Institute. Susceptibility testing of mycobacteria, nocardiae, and other aerobic actinomycetes: approved standard—second edition. CLSI document M24-A2. 2011.
Clinical and Laboratory Standards Institute. Susceptibility testing of mycobacteria, nocardia, and other aerobic actinomycetes. 3rd ed. Wayne, PA: Clinical and Laboratory Standards Institute; 2017. To be submitted
Brown BA, Wallace RJ Jr, Onyi GO, De Rosas V, Wallace RJ III. Activities of four macrolides, including clarithromycin, against Mycobacterium fortuitum, Mycobacterium chelonae, and M. chelonae-like organisms. Antimicrob Agents Chemother. 1992;36:180–4.
Nash KA. Intrinsic macrolide resistance in Mycobacterium smegmatis is conferred by a novel erm gene, erm(38). Antimicrob Agents Chemother. 2003;47:3053–60.
Nash KA, Andini N, Zhang Y, Brown-Elliott BA, Wallace RJ Jr. Intrinsic macrolide resistance in rapidly growing mycobacteria. Antimicrob Agents Chemother. 2006;50:3476–8.
Nash KA, Brown-Elliott BA, Wallace RJ Jr. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob Agents Chemother. 2009;53:1367–76.
Nash KA, Zhang Y, Brown-Elliott BA, Wallace RJ Jr. Molecular basis of intrinsic macrolide resistance in clinical isolates of Mycobacterium fortuitum. J Antimicrob Chemother. 2005;55:170–7.
Koh WJ, Jeon K, Lee NY, Kim B-J, Kook Y-H, Lee S-H, Park Y-K, Kim CK, Shin SJ, Huitt GA, Daley CL, Kwon OJ. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus. Am J Respir Crit Care Med. 2011;183:405–10.
Koh WJ, Stout JE, Yew WW. Advances in the management of pulmonary disease due to Mycobacterium abscessus complex. Int J Tuberc Lung Dis. 2014;18(10):1141–8.
Wallace RJ Jr, Brown-Elliott BA, Crist CJ, Mann L, Wilson RW. Comparison of the in vitro activity of the glycylcycline tigecycline (formerly GAR-936) with those of tetracycline, minocycline, and doxycycline against isolates of nontuberculous mycobacteria. Antimicrob Agents Chemother. 2002;46:3164–7.
Brown-Elliott BA, Iakhiaeva E, Griffith DE, Woods GL, Stout JE, Wolfe CR, Turenne CY, Wallace Jr. RJ. 2013. In vitro activity of amikacin against isolates of Mycobacterium avium complex with proposed MIC breakpoints and finding of a 16S rRNA gene mutation in treated isolates. J Clin Microbiol 51:3389–3394. ERRATUM JCM 2014; 3352:1311.
Olivier KN, Griffith DE, Eagle G, McGinnis II JP, Micioni L, Liu K, Daley CL, Winthrop KL, Ruoss S, Addrizzo-Harris DJ, Flume PA, Dorgan D, Salathe M, Brown-Elliott BA, Gupta R, Wallace Jr. RJ. Randomized trial of liposomal amikacin for inhalation in nontuberculous mycobacterial lung disease. Am J Respir Crit Care Med. 2016; Submitted.
Wallace RJ Jr, Brown-Elliott BA, Ward SC, Crist CJ, Mann LB, Wilson RW. Activities of linezolid against rapidly growing mycobacteria. Antimicrob Agents Chemother. 2001;45:764–7.
Brown-Elliott BA, Wallace RJJ, Blinkhorn R, Crist CJ, Mann LB. Successful treatment of disseminated Mycobacterium chelonae infection with linezolid. Clin Infect Dis. 2001;33:1433–4.
Brown-Elliott BA, Philley JV, Griffith DE, Wallace RJ Jr. Comparison of in vitro susceptibility testing of tedizolid (TZD) and linezolid (LZD) against isolates of nontuberculous mycobacteria (NTM). Boston, MA: General Meeting of the American Society of Microbiology 2016; 2016.
Wallace RJ Jr, Dukart G, Brown-Elliott BA, Griffith DE, Scerpella EG, Marshall B. Clinical experience in 52 patients with tigecycline-containing regimens for salvage treatment of Mycobacterium abscessus and Mycobacterium chelonae infections. J Antimicrob Chemother. 2014;69(7):1945–53.
Shen G-H, Wu B-D, Hu S-T, Lin C-F, Wu K-M, Chen J-H. High efficacy of clofazimine and its synergistic effect with amikacin against rapidly growing mycobacteria. Int J Antimicrob Agents. 2010;35:400–4.
van Ingen J, Totten SE, Helstrom NK, Heifets LB, Boeree MJ, Daley CL. In vitro synergy between clofazimine and amikacin in treatment of nontuberculous mycobacterial disease. Antimicrob Agents Chemother. 2012;56(12):6324–7.
Yang B, Jhun BW, Moon SM, Lee H, Park HY, Jeon K, Kim DH, Kim SY, Shin SJ, Daley CL, Koh WJ. Clofazimine-containing regimen for the treatment of Mycobacterium abscessus lung disease. Antimicrob Agents Chemother. 2017;61(6):e02052–16.
Philley JV, Wallace RJ Jr, Benwill JL, Taskar V, Brown-Elliott BA, Thakkar F, Aksamit TR, Griffith DE. Preliminary results of bedaquiline as salvage therapy for patients with nontuberculous mycobacterial lung disease. Chest. 2015;148:499–506.
Maurer FP, Bruderer VL, Ritter C, Castelberg C, Bloemberg GV, Böttger EC. Lack of antimicrobial bactericidal activity in Mycobacterium abscessus. Antimicrob Agents Chemother. 2014;58:3828–36.
van Ingen J, Boeree MJ, van Soolingen D, Mouton JW. Resistance mechanisms and drug susceptibility testing of nontuberculous mycobacteria. Drug Resist Updat. 2012;15:149–61.
Brown-Elliott BA, Vasireddy S, Vasireddy R, Iakhiaeva E, Howard ST, Nash K, Parodi N, Strong A, Gee M, Smith T, Wallace RJ Jr. Utility of sequencing the erm(41) gene in isolates of Mycobacterium abscessus subsp. abscessus with low and intermediate clarithromycin MICs. J Clin Microbiol. 2015;53(4):1211–5.
Koh WJ, Jeong BH, Jeon K, Kim SY, Park KU, Park HY, Huh HJ, Ki CS, Lee NY, Le SH, Kim CK, Daley CL, Shin SJ, Kim H, Kwon OJ. Oral macrolide therapy following short-term combination antibiotic treatment for Mycobacterium massiliense lung disease. Chest. 2016;150(6):1211–21.
Choi H, Kim S-Y, Kim DH, Huh HJ, Ki C-S, Lee NY, Lee S-H, Shin S, Shin SJ, Daley CL, Koh W-J. Clinical characteristics and treatment outcomes of patients with acquired macrolide-resistant Mycobacterium abscessus lung disease. Antimicrob Agents Chemother. 2017;61:e01146–17, https://doi.org/10.1128/AAC.01146–17.
Choi H, Kim SY, Lee H, Jhun BW, Park HY, Jeon K, Kim DH, Huh HJ, Ki CS, Lee NY, Lee SH, Shin SJ, Daley CL, Clinical Characteristics KWJ. Treatment outcomes of patients with macrolide-resistant Mycobacterium massiliense lung disease. Antimicrob Agents Chemother. 2017;61(2):293–5
Griffith DE, Aksamit TR. Nontuberculous mycobacterial disease therapy: take it to the limit one more time. Chest. 2016;150(6):1177–8.
Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL. Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin Infect Dis. 2011;52(5):565–71.
Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, Park YK, Kim CK, Koh WJ. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009;180(9):896–902.
Lyu J, Jang HJ, Song JW, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Shim TS. Outcomes in patients with Mycobacterium abscessus pulmonary disease treated with long-term injectable drugs. Respir Med. 2011;105(5):781–7.
Harada T, Akiyama Y, Kurashima A, Nagai H, Tsuyuguchi K, Fujii T, Yano S, Shigeto E, Kuraoka T, Kajiki A, Kobashi Y, Kokubu F, Sato A, Yoshida S, Iwamoto T, Saito H. Clinical and microbiological differences between Mycobacterium abscessus and Mycobacterium massiliense lung diseases. J Clin Microbiol. 2012;50(11):3556–61.
Roux AL, Catherinot E, Soismier N, Heym B, Bellis G, Lemonnier L, Chiron R, Fauroux B, Le Bourgeois M, Munck A, Pin I, Sermet I, Gutierrez C, Véziris N, Jarlier V, Cambau E, Herrmann JL, Guillemot D, Gaillard JL, group O. Comparing Mycobacterium massiliense and Mycobacterium abscessus lung infections in cystic fibrosis patients. J Cyst Fibros. 2015;14:63–9.
Lee SH, Yoo HK, Kim SH, Koh WJ, Kim CK, Park YK, Kim HJ. The drug resistance profile of Mycobacterium abscessus group strains from Korea. Ann Lab Med. 2014;34(1):31–7.
Floto RA, Olivier KN, Saiman L, Daley CL, Herrmann JL, Nick JA, Noone PG, Bilton D, Corris P, Gibson RL, Hempstead SE, Koetz K, Sabadosa KA, Ermet-Gaudelus I, Smyth AR, van Ingen J, Wallace RJ, Winthrop KL, Marshall BC, Haworth CS. US Cystic Fibrosis Foundation and European cystic fibrosis society. US Cystic Fibrosis Foundation and European cystic fibrosis society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax. 2016;71(Suppl 1):i1–22.
Acknowledgments
We humbly acknowledge and thank our patients with M. abscessus lung disease whose patience with their physicians, courage and strength are both boundless and inspirational.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Philley, J.V., Griffith, D.E. (2019). Disease Caused by Mycobacterium Abscessus and Other Rapidly Growing Mycobacteria (RGM). In: Griffith, D. (eds) Nontuberculous Mycobacterial Disease. Respiratory Medicine. Humana Press, Cham. https://doi.org/10.1007/978-3-319-93473-0_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-93473-0_13
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-93472-3
Online ISBN: 978-3-319-93473-0
eBook Packages: MedicineMedicine (R0)