Abstract
Spinal arteriovenous malformation is a rare, congenital disease (excluding dural arteriovenous fistula, which is thought to be acquired). Once symptoms arise, the pathology is usually progressive, and spontaneous remission seldom occurs, leading to bedridden status. The technique of surgical intervention for pathological arteriovenous shunt is discussed in this chapter.
Both authors belonged to the Department of Neurosurgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan. And both presented cases were treated in here.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Purpose
Spinal arteriovenous malformation (sAVM) is a rare, congenital disease (excluding dural arteriovenous fistula (dAVF), which is thought to be acquired). Once symptoms arise, the pathology is usually progressive, and spontaneous remission seldom occurs, leading to bedridden status. Surgical intervention for arteriovenous shunt (AVS) disease is discussed in this chapter.
Prerequisites
The therapy for sAVM is interruption of the AVS, with preservation of draining veins that contribute to normal circulation. For this purpose, accurate diagnosis of AV shunt based on the classification of sAVM is necessary. While some controversy remains, sAVM is generally classified as sAVM (also called glomerular AVM or nidus-type AVM) with an intramedullary AV shunt; fistulous AVM (perimedullary AVF), showing an AV shunt on the surface of the spinal cord; spinal dural arteriovenous fistula (sdAVF), with shunt in the dura mater draining into the spinal cord; and epidural AVF, with AV shunt on the outer surface of the dura and drain into the extradural space. On T2-weighted magnetic resonance imaging (MRI), intramedullary hyperintensity and flow void in the subarachnoid space are suggestive of sAVM. Accurate determination of the shunt point by selective angiography is mandatory for treatment.
Planning and Diagnostics
The symptoms of sAVM include radiculopathy, localized complaints such as neck pain, and myelopathies such as paresis, sensory disturbance, and bowel and/or bladder dysfunction. The pathophysiologies of developing symptoms include hemorrhage, congestion due to venous hypertension, arterial steal and mass effects resulting from dilated and serpentine vessels. Sudden symptoms are caused by hemorrhage, either in the subarachnoid space or intramedullary. Symptoms depend on the site of hemorrhage. Subarachnoid hemorrhage causes meningeal signs such as headache and vomiting, while intramedullary hematoma causes neurological deficits. Other mechanisms cause progressive myelopathy and/or radiculopathy. Symptoms and speed of progression are influenced by the disease location and degree of shunting.
Diagnosis is usually first made from MRI. T1- and T2-weighted signal voids due to dilated, serpentine vessels are recognized, although T2-weighted signal voids are more easily identified. Intramedullary signal voids are seen with nidus-type AVM. Intramedullary signal hyperintensity is frequently found on T2-weighted imaging. In cases with signal voids on the surface of the spinal cord without intramedullary hyperintensity on T2-weighted imaging, the possibility of sAVM can largely be ruled out. Conversely, the possibility of microshunt cannot be excluded in cases of intramedullary signal hyperintensity without signal void on T2-weighted imaging. Dilated veins and intramedullary swelling are enhanced by Gd-DTPA. MRI cannot distinguish the type of sAVM, but MR angiography with Gd-DTPA can show the approximate location of the shunt, helping to minimize the amount of contrast medium needed in selective spinal angiography.
Types of sAVM are diagnosed using spinal angiography. Locations of feeding arteries, nidi, shunts, and draining veins should be determined. With the exception of sdAVF, multiple feeding arteries, shunt points, and draining veins are usually present, and all suspected vessels should be examined.
A serpiginous defect in myelography is a characteristic finding, but this modality is no longer a necessary investigation since the advent of MRI.
Symptomatic sAVM should be treated, since spontaneous remission cannot be expected. Treatment methods include transarterial embolization (TAE) and surgical interruption. Preoperative planning should clarify the degree to which shunt flow can be expected to decrease following TAE and/or surgical interruption. A single shunt is usually seen in sdAVF, so the goal of treatment is complete shunt obstruction. With TAE, glue should fill from the feeding artery to the draining vein through the shunt point. Particulate agents such as Avitene and polyvinyl alcohol (PVA) are unsuitable, since these result in early recanalization. If a risk of unintended embolization of an important artery such as the vertebral artery is present, TAE is contraindicated. In cases without indications for TAE or that are treated with TAE unsuccessfully, the draining vein should be surgically interrupted at the point at which it arises from the dura mater. In other types of sAVM, multiple shunts are common, and complete interruption is difficult. However, any reduction in shunt flow contributes to improvement of symptoms and can be considered beneficial, differing from the situation with cerebral AVM. Pre- or perioperatively, the goals of TAE should be examined, and plans for any subsequent surgical interruption should be evaluated. Coiling at the surgical level can contribute to determination of the surgical level during direct surgery.
Patient Positioning
In cases of other types of sdAVF in which shunt points exist dorsal to the spinal cord, the lesions are approached with the patient in a prone position. The head is fixed using pins, such as with a Mayfield clamp. If intraoperative digital subtraction angiography (DSA) is applied, a radiolucent clamp made of carbon is useful. The head is slightly elevated to avoid increasing venous pressure. The neck is slightly, but not excessively, flexed, as excessive flexion leads to venous congestion. At least two fingerwidths should be kept between the chin and chest. The patient’s body should be fixed to the surgical table for intraoperative tilting. If shunt points exist on the anterior surface of the spinal cord, such as related anterior spinal arteries, an anterior approach is useful for cervical lesions.
Surgical Technique
Representative Case 1: sdAVF
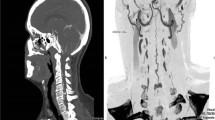
This case involved sdAVF at the craniovertebral junction. Enlarged and serpiginous anterior spinal veins were seen in the arterial phase from the point at which the vertebral artery penetrates the dura mater. The feeding artery was the vertebral artery (Fig. 92.1).
Case Example 1 DSA of right vertebral artery of case1, a case of dural AVF. (a) AP view, (b) lateral view. Enlarged and serpiginous anterior spinal veins were seen in the arterial phase from the point at which the vertebral artery penetrates the dura mater (arrow). The feeding artery was the vertebral artery
Approach
The lesion was approached from posteriorly. As mentioned above, the head was fixed with a Mayfield head clamp. The neck was slightly flexed, and the operative field was positioned higher than the heart. Preoperative evaluation should clarify from which side, ipsi- or contralateral, is better to observe the shunt point, and the operator is positioned accordingly. The lamina was approached with a midline linear skin incision and midline dissection of the muscle layers. Laminectomy is performed at the shunt point, and the lamina is not necessarily exposed bilaterally. The shunt point was located at the lateral margin of the dural sac, and laminectomy was performed sufficiently laterally to observe the lateral margin of the dural sac. Although excess removal of facets leads to instability and should be avoided, removal to the extent that the lateral border of the dural sac may be observed is allowable. Usually, one cranial and one caudal laminectomy is enough. In this case, the operator stood on the left of the patient, contralateral to the lesion. Only the right-sided C1 and C2 laminae were exposed and removed.
Dural Incision
The dura was incised in the middle part of the operative field, maintaining a margin for suturing. At the start of the dural incision, the arachnoid membrane was preserved. After making a small dural incision sufficient to allow the use of forceps, the dura was opened craniocaudally by drawing bilaterally with forceps. The draining vein arising from the dura can sometimes be surgically interrupted in the subdural epiarachnoid space, so an arachnoidal incision is not always necessary. This is important, because preservation of the arachnoid membrane contributes to preventing postoperative leakage of cerebrospinal fluid.
Interruption of the Shunt Point
Treatment of sdAVF involved interruption at the point where the draining vein arises from the dura. The dura was retracted laterally with a filament suture at the edge of the incision. An enlarged, serpiginous draining vein was found arising from the internal surface of the dura (Fig. 92. 2). To confirm the draining vein, detection of flow direction with Doppler echography was useful. Contrary to normal circulation, in which flow direction in the vein is efferent (from spinal cord to nerve root), flow is afferent in sdAVF. This draining vein is interrupted with a clip or coagulated and cut at the point of arising from the dura (Fig. 92.3). The draining vein itself functions as normal circulation, and coagulation or removal of the draining vein on the surface of the spinal cord is unnecessary. If the feeding artery is a radiculomeningeal artery, it can be interrupted. In this case, the feeding artery was the vertebral artery and could not be interrupted.
Intraoperative view of case 1, after dural and arachnoidal opening. Upper is right inner surface of dura; left is cranial. Right vertebral artery is penetrating the dura at this point. Just caudal to this point, draining vein is arising from the dura. Spinal cord and accessory nerve are also observed
Closure
The dura was sutured in a watertight manner. If the arachnoid membrane had been opened, it would have been sutured simultaneously. The seam is sealed with fibrin glue and reinforced with polyglycolic acid (PGA) sheet if available. Structures, like the nuchal ligament, superficial fascia, subcutaneous tissue, and skin, should be reconstructed layer by layer, in a watertight manner to prevent CSF leakage.
Case 2: Fistulous AVM (Perimedullary AVF, Intradural AVF)
In this case of fistulous AVM, the feeding artery was the anterior spinal artery (Fig. 92.4). The shunt point existed on the anterior surface of the spinal cord. The lesion was approached from anteriorly with corpectomy, and the shunt point was interrupted.
Approach
The patient was placed in a supine position, with neck slightly extended and rotated opposite to the approach side. Either side could have been selected, with the right-sided approach preferable for a right-handed surgeon. If intraoperative DSA is applied, a Mayfield head clamp is useful to minimize motions. Corpectomy should be limited to observe and interrupt the shunt point, with no necessity to observe the broad area of the enlarged draining vein. Extensive corpectomy leads to dislocation of grafted bone and decreased range of motion and so should be avoided.
Dural Incision
A dural incision was made in the midline. The shunt point was located on the surface of the spinal cord, so an incision in the arachnoid was made later. Even so, arachnoid membrane was preserved as much as possible to facilitate dural incision. Retracting the incised dura to either side with filament, enlarged serpiginous vessels were observed through the arachnoid membrane. An arachnoidal incision was made and then fixed to the dura with a mini-clip.
Interruption of Shunt Point
A key step in the treatment of fistulous AVM is confirmation of the shunt point. Most of the enlarged serpiginous draining vein functions as normal spinal circulation, so excess coagulation can cause perfusion disorder. Compared to preoperative DSA, the shunt point where the thin feeding artery suddenly changes to a thick draining vein should be detectable (Fig. 92.5). The draining vein should be carefully dissected and exposed, since hemostasis is difficult to provide in the event of accidental injury. Arterial pressure is applied on the thin wall of the draining vein. When the shunt point is found, a temporary clip is applied. If this point is a true shunt point, pressure in the draining vein will decrease, and the color will darken. Doppler echography shows decreased arterial pulsations in the draining vein. If available, intraoperative DSA is useful for confirming interruption. The shunt point is coagulated and cut after confirmation. In fistulous AVM, multiple shunt points are often present. After interruption of the main shunt, any occult shunts will become visible. With reference to preoperative DSA, other shunts should be detected.
Intraoperative view of case 2. After corpectomy and dural incision. The lesion is approached from right anterior, so left of image is cranial, upper is left side. Anterior spinal artery, vein, and enlarged serpiginous draining vein are observed on the anterior surface of the spinal cord. Shunt point, in which thin feeding artery suddenly changes to enlarged vein, is observed
Closure
The dura is sutured with the arachnoid membrane in a watertight manner. With fistulous AVM, recurrence of the AVS is not rare. In surgery for recurrence, adhesions between the dural suture and spinal cord may prove problematic. To avoid such adhesions, Goretex® sheet should be placed under the dura with stay sutures at the opening in the dura. This prevents adhesion between the dura and spinal cord, making any reoperation easier. The dural suture is sealed with fibrin glue and can be reinforced with PGA sheet. If an anterior approach is applied, a watertight seal is especially important (Table 92.1). Compared with the posterior approach, preventing the formation of dead space by suturing the muscle layer is difficult with the anterior approach. Additionally, compression from outside is impossible. Removed sections of the vertebral body should be reconstructed with autografted material and artificial vertebral body.
Summary of Main Surgical Steps
-
1.
Positioning: Operative field is slightly elevated. The head and body are fixed for intraoperative angiography and tilting.
-
2.
Approach: Laminectomy or corpectomy is performed to visualize the lesion.
-
3.
Dural incision: Arachnoid membrane is kept intact if possible.
-
4.
Confirmation of shunt point: It should be confirmed precisely, with intraoperative DSA, if necessary.
-
5.
Interruption of shunt point: Only the point should be interrupted. Enlarged draining vessels function as normal circulation.
-
6.
Closure: Watertight dural closure is essential. Putting Goretex sheet under dura should be considered.
Bibliography
Flores BC, Klinger DR, White JA, et al. Spinal vascular malformations: treatment strategies and outcome. Neurosurg Rev. 2017;40(1):15–28. https://doi.org/10.1007/s10143-016-0713-z.
Jahan R, Vinuela F. Vascular anatomy, pathophysiology, and classification of vascular malformation of the spinal cord. Semin Cerebrovasc Dis Stroke. 2002;2:186–200.
Kikuchi Y, Miyasaka K. Treatment strategy of spinal arteriovenous malformations based on a simple classification. J Clin Neurosci. 1998;5(Suppl 1):16–9.
Krings T. Vascular malformations of the spine and spinal cord*: anatomy, classification, treatment. Clin Neuroradiol. 2010;20(1):5–24. https://doi.org/10.1007/s00062-010-9036-6.
Rodesch G, Lasjaunias P. Spinal cord arteriovenous shunts: from imaging to management. Eur J Radiol. 2003;46(3):221–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Aoyama, T., Hida, K. (2019). Vascular Malformation in the Cervical Spine. In: Koller, H., Robinson, Y. (eds) Cervical Spine Surgery: Standard and Advanced Techniques. Springer, Cham. https://doi.org/10.1007/978-3-319-93432-7_92
Download citation
DOI: https://doi.org/10.1007/978-3-319-93432-7_92
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-93431-0
Online ISBN: 978-3-319-93432-7
eBook Packages: MedicineMedicine (R0)