Abstract
With the introduction of modern equipment, imaging, and surgical techniques, many surgeons now treat Zenker diverticula via endoscopic approaches. Newer equipment and imaging systems have allowed adequate exposure of the esophagodiverticular wall which contains the cricopharyngeal muscle enabling its division by various means. This chapter addresses these methods, including laser-assisted diverticulotomy, stapler-assisted diverticulotomy, harmonic scalpel-assisted diverticulotomy, and bipolar diathermic electrocoagulation division of the party wall. Perioperative treatment is directed at avoiding mediastinitis in all of the endoscopic approaches. Treatment outcomes for endoscopic approaches to Zenker diverticula have consistently been excellent with first-treatment success and low complication rates. Zenker diverticula can be safely and effectively managed with endoscopic techniques for the majority of patients. Large Zenker diverticula should be treated with stapler-assisted technique. Treatment of smaller Zenker diverticula or difficult-to-expose diverticula should be attempted with laser-assisted diverticulotomy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The treatment of dysphagia associated with Zenker diverticula (ZD) has evolved since its description by Zenker and Ziemssen [1]. While initial attempts were made to manage these transorally, these efforts were largely abandoned because of limitations in exposure and concerns for patient safety. For many years through the early 1900s, surgeons approached Zenker diverticula through a transcervical approach in order to control the alimentary tract and drain expected fistulae. As recovery was protracted and complications such as fibrosis, fistula formation, and recurrent laryngeal nerve injury continued to occur, a less invasive—yet efficacious—method of surgical correction was sought through the latter half of the twentieth century. As a result of modifications in technique, equipment, and imaging, most surgeons now choose to manage ZD through endoscopic means, with open techniques reserved for ever fewer challenging cases.
Historical Considerations
Early attempts at diverticulotomy by an endoscopic approach were initiated in the early twentieth century. Jackson was the first to report his experience with esophagoscope-assisted diverticulectomy in 1915 [2]. This first attempt was a combined endoscopic and transcervical procedure, using a standard esophagoscope to remove retained debris from within the diverticulum, present and transilluminate the diverticulum through the external wound, and maintain the esophageal lumen during esophageal closure. Though the diverticulum was still excised in a transcervical fashion, this represented the first effort to use endoscopic techniques during diverticulectomy. Two years later, Mosher was the first to attempt an entirely endoscopic approach. During this procedure, the esophagoscope was used to visualize the diverticulum, and a surgical knife was used to cut the cricopharyngeal bar through the esophagoscope [3]. As visualization of the cricopharyngeal bar was limited during these procedures, the subsequent risk of mediastinitis was high. Indeed, the seventh patient that underwent this procedure developed mediastinitis and died. Thus, Mosher and other surgeons abandoned this technique in favor of transcervical approaches that could control leaks from the hypopharynx. Based on the high rate of morbidity and mortality seen in this limited experience in endoscopic management, open diverticulectomy remained the gold standard for the decades to follow. However, with advances in imaging, antibiotic therapy, optics, diverticuloscopes, and endoscopic tools, surgeons continued to seek safe and efficacious endoscopic approaches to treat ZD.
The first of these advances came in the form of exposure. By the late 1950s, Dohlman developed a modified esophagoscope, which displayed two “lips” (one placed into the esophagus and one placed into the diverticulum) allowing for exposure of the common diverticular and esophageal wall and the ability to place it on tension for more controlled surgical division. By utilizing this modified esophagoscope, diathermic coagulation (similar in many ways to monopolar electrocautery) could be utilized to divide the cricopharyngeus [4]. In Dohlman’s experience of nearly 100 cases, there were no cases of severe complications (including death or mediastinitis), and a recurrence rate of 7% was reported. This published experience gave more surgeons the confidence that endoscopic diverticulotomy could be safe and efficacious and laid the foundation for further development and experimentation.
With improved exposure of the cricopharyngeal bar , further modifications to Dohlman’s technique sought to allow even more controlled division of the cricopharyngeal muscle and overlying mucosa with the operating microscope [5] and surgical lasers (both carbon dioxide [5] and potassium titanyl phosphate [6]). While technically feasible and likely superior to electrosurgical endoscopic approaches, the use of the surgical microscope and laser was not commonly available and still required a great deal of skill. Surgeons continued to seek a simpler solution to the problem of controlled cricopharyngeal bar division. The answer came in 1993, when both Collard and Martin-Hirsch independently published reports of performing a stapled diverticulotomy with an endoscopic gastrointestinal anastomosis stapler (Multifire Endo GIA 30, Medtronic, Minneapolis, MN) [7, 8]. Both reports demonstrated the safety of these instruments when applied to ZD, and surgeons rapidly embraced this technique. By the mid-1990s, endoscopic stapler-assisted diverticulotomy became the procedure of choice by most surgeons for the treatment of ZD.
The widespread application of the endoscopic stapler was made possible through contemporaneous refinements to Dohlman’s original modified esophagoscope. Further evolution occurred with the development of the Weerda diverticuloscope (Karl Storz Endoscopy, Tuttlingen, Germany). Developed in Germany, this was the first scope to utilize a bivalved design, in which both the proximal and distal openings could be widened or collapsed (Fig. 7.1). This esophagoscope design provided markedly improved visualization of the common wall. This visualization was essential for application of the endoscopic stapler in many cases and allowed the diverticulum wall to be placed under greater tension for division with a laser.
The Weerda diverticuloscope (Karl Storz Endoscopy, Tuttlingen, Germany). For reference, see Lang et al. [45]
Despite the simplicity of the laparoscopic stapler to perform diverticulotomy and cricopharyngeal myotomy and its widespread application, surgeons recognized that this treatment was not universally effective. Difficulties in exposure and the presence of small diverticula that did not allow complete division of the cricopharyngeus muscle limited the use of the endoscopic stapler to a subset of intermediate-sized diverticula that could be suitably exposed for the 12-mm-diameter stapler. While some surgeons continued to use carbon dioxide lasers to address these smaller lesions, others sought innovative solutions to this problem. Scher and his colleagues used a laparoscopic suture applier to encircle the cricopharyngeus muscle on either side of the diverticulotomy [9]. Traction could be applied to these sutures to pull the cricopharyngeus muscle into the stapler for more complete division. Other innovative endoscopic techniques in the twenty-first century have been reported, including the use of ultrasonic high-frequency transduction (Harmonic scalpel, Ethicon Inc., Somerville, NJ) [10] or bipolar diathermy (LigaSure, Medtronic, Minneapolis, MN) [11]. The Harmonic scalpel was felt to “seal” the diverticulum mucosa and submucosa thus providing a safer means to divide smaller diverticula than the carbon dioxide laser. While reports of this technique are limited to relatively small cohorts of patients, the most recent evaluation of this approach suggests an unacceptably high complication rate to merit widespread application [12].
Outcomes for treatment of ZD via transoral means remain excellent with high first-treatment success and low complication rates. A large retrospective study by van Overbeek et al. of 545 patients treated endoscopically by a variety of techniques (including diathermic electrocoagulation and carbon dioxide laser) showed that 91% of patients reported “high satisfaction” with the procedure [13]. A large meta-review published in 2004 shows a satisfactory outcome in 96% of patients treated endoscopically, with a 6% persistence/recurrence rate and a 3% rate of major morbidity (including a 2.6% rate of esophageal perforation or leak) [14]. A recent retrospective review by Barton of 106 consecutive patients undergoing either laser-assisted or stapler-assisted endoscopic Zenker diverticulotomy demonstrated an overall satisfaction rating of 8.2 on a 10-point scale with no major complications [15].
Modern Endoscopic Approaches
Modern endoscopic techniques for safe and successful management of ZD require careful consideration of patient factors. Successful intervention mandates adequate exposure of the diverticulum and esophagodiverticular, or “party,” wall containing the cricopharyngeus muscle. Once exposed, a variety of techniques can be used to intervene upon the diverticulum in an effective manner. Following the procedure, cautious advancement of oral intake may be initiated, or imaging should be obtained to ensure the absence of an esophageal leak or perforation.
Preoperative Considerations
A comprehensive preoperative work-up is imperative for appropriate patient selection prior to endoscopic procedures for ZD. All patients should undergo radiographic imaging with either an esophagram or modified barium swallow study (MBSS) to evaluate the size and location of the pouch. MBSS with esophageal follow-through, a functional study, is the preferred imaging modality, which allows for assessment of comorbid pharyngoesophageal conditions. Diverticula that are longer than 2 cm and adequate to expose may be considered for stapler-assisted ZD, while others may be treated with the laser [15]. Furthermore, an assessment of anatomic factors that may limit exposure of the diverticulum from an endoscopic approach should be pursued. Patients who may be at risk for unsuccessful endoscopic exposure of the diverticular sac include those with small ZD (<2 cm), retrognathic mandibles, large tongues, kyphosis, or decreased neck mobility [16].
Exposure
Rigid diverticuloscopy is performed under general anesthesia with neuromuscular blockade. Once general anesthesia is obtained and the patient is intubated, the patient is typically rotated 90° or 180° away from the anesthesia team. The patient is then placed into the “sniffing position,” with extension of the neck and slight flexion of the atlanto-occipital joint. The dentition or maxilla is protected in all cases with either a durable pre-molded dental guard or thermoplastic sheeting (Aquaplast, Allied Medical Products, Tarzana, CA) molded to the patient’s dentition. Such protection is essential as the forces on the maxillary dentition can be substantial during rigid diverticuloscopy . Unlike direct laryngoscopy, the surgeon should also be careful to observe the mandibular dentition during exposure and suspension, as the distending diverticuloscopes can apply pressure to these teeth in many cases. If the patient is edentulous, a moist gauze may be used to protect the maxillary mucosa.
Rigid exposure for direct transoral endoscopic intervention is performed using a diverticuloscope to expose the cricopharyngeus (CP) muscle. As previously stated, the Weerda endoscope is preferred once the patient is correctly positioned, and the diverticuloscope is then placed gently into the oral cavity and advanced past the base of the tongue and epiglottis and through the oropharynx to the postcricoid hypopharynx. It is important to remember to insert and advance the scope with the distal and proximal openings in a collapsed or closed position. Surgical lubricant may facilitate advancing the scope and minimize mucosal injury. The scope is then advanced until the flanges of the scope expose the CP muscle, with the posterior flange proximal to the diverticulum and the anterior flange proximal to the esophagus. When using an articulating diverticuloscope, the proximal and distal openings are then widened to place the diverticuloesophageal wall containing the cricopharyngeus muscle wall on stretch. The diverticuloscope is then suspended using a suspension arm (Karl Storz Endoscopy, Tuttlingen, Germany) and a mustard table (Medtronic, Dublin, Ireland), allowing for adequate visualization of the CP muscle (Fig. 7.2) [15, 17]. At this point, correct placement of the diverticuloscope may be confirmed by using a nasogastric tube or bougie stylet to palpate the diverticular pouch and esophagus.
If entry into the cervical esophagus is challenging because of hypertonicity or fibrosis of the cricopharyngeus muscle , careful dilation of the esophagus may be performed. This can be performed under direct visualization either with the use of Savary-Gilliard dilators (over a guidewire), serial dilations of the upper esophageal sphincter from 21 to 42 Fr [20], or a controlled radial expansion (CRE) balloon catheter [17]. The authors prefer to pass a bougie into the cervical esophageal introitus and follow this with the anterior flange of the diverticuloscope. This is effective in almost all cases and does not cause significant trauma in our experience.
Once adequate exposure of the diverticular wall is achieved, the diverticulopharyngeal wall can then be divided by a variety of techniques. Endoscopic staplers, laser, cold instruments, bipolar diathermy, and harmonic scalpel have all been used recently for this technique. The endoscopic staple approach will be covered in a separate chapter.
Laser-Assisted Diverticulotomy
Endoscopic stapler-assisted Zenker diverticulotomy may not be adequately or easily performed secondary to small pouch size or patient anatomical factors resulting in limited exposure. In these cases, an endoscopic laser-assisted diverticulotomy should be considered. In general, laser techniques can be performed on diverticula smaller than 2 cm since the laser is able to divide the diverticulopharyngeal wall more completely than the stapler [18]. Additionally, endoscopic laser diverticulotomy may require less exposure when compared to endoscopic stapler-assisted procedures and may allow the endoscopic procedure to be completed in cases which previously would have been aborted [15]. Historically, endoscopic laser cricopharyngeal myotomy has been performed using both the potassium-titanyl-phosphate (KTP) laser [6, 19] and carbon dioxide (CO2) laser [5]. The CO2 laser is likely superior for this procedure as it is easier to control on a micromanipulator attached to the microscope and better at cutting tissue with less thermal artifact and char than the KTP laser.
Technique
As with any procedure involving laser use, a laser safety checklist should be performed prior to using a laser device, ensuring the use of eye protection by the patient and staff and determining that laser settings are correct and the laser has been test fired, irrigation is available on the surgical field, and all staff are aware of fire extinguisher locations. Following adequate exposure of the ZD wall, a CO2 or KTP laser is then used with a micromanipulator attached to the operating microscope to divide the CP muscle until the muscular fibers are completely transected and the diverticular pouch is flushed with the esophagus [17] (Figs. 7.3 and 7.4). Cervical esophageal fibers that contribute to the upper esophageal sphincter can also be divided for 5–10 mm inferiorly just under the esophageal submucosa. The laser should be used to cautiously divide all of the cricopharyngeal muscle fibers layer by layer to ensure a complete myotomy without inadvertent injury to the buccopharyngeal fascia that invests the entire pharyngoesophageal segment. Hemostasis is generally easy to achieve with the laser and topical 1:10,000 epinephrine on cotton pledgets. In rare cases, more troublesome bleeding may be treated with judicious monopolar cautery, thrombin, or microfibrillar collagen hemostat application (Avitene, Davol, subsidiary of CR Bard, Warwick, RI). A laser-shielded or metal endotracheal tube should be used and communication with the anesthesiologist that a laser is about to be used should be undertaken to assure that the end tidal oxygen level is brought to its lowest allowable concentration. The authors prefer to use room air for ventilation whenever possible to minimize the risk of a laser airway fire.
Demonstration of the buccopharyngeal fascia and cervical esophagus within the diverticulopharyngeal party wall after the use of the CO2 laser for diverticulotomy and cricopharyngeal myotomy. This fascia prevents leakage from the alimentary tract into the prevertebral space. Note that the cricopharyngeus muscle is completely divided and retracts laterally deep under the mucosa when under tension
Careful attention and operator experience are required to safely complete the myotomy without creating an esophageal perforation. The myotomy should only be performed when the CP muscle can be adequately visualized, and dissection should stop once the deepest muscle fiber is divided and the buccopharyngeal fascia is visualized. Aside from utilizing extreme caution, several techniques have been described to prevent esophageal perforation. Primary mucosal closure with Vicryl suture has been described [20]. Alternatively, some authors recommend avoiding division of the soft tissue all the way down to the buccopharyngeal fascia and instead use a CRE balloon to dilate the cricopharyngeal area to 18–20 mm after a laser-assisted partial myotomy is performed [17]. These techniques are not routinely performed—nor are they required in the authors’ opinion—and their usage largely depends on the operator’s preference and comfort level.
Outcomes
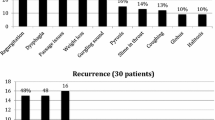
Patients undergoing endoscopic laser treatment of ZD report overall satisfaction with the procedure. In an early series of ten patients treated with KTP laser diverticulotomy, all were either “very satisfied” or “satisfied” with their results, and none of the patients required further treatment after diverticulotomy [6]. Four of these patients had evidence of a residual pouch on postoperative MBSS, of which two patients experienced mild persistent pill dysphagia. In a study of 37 patients undergoing laser-assisted diverticulotomy, a 92% long-term satisfaction rate was noted, with 70% complete resolution and 22% partial resolution of symptoms [21]. A large patient satisfaction study, evaluating 507 patients treated endoscopically with carbon dioxide laser-assisted myotomy (with or without diathermy for hemostasis) showed a 99% satisfaction rate [22]. Additionally, the majority of patients experience a significant reduction in their symptoms, including a subjective reduction in dysphagia and regurgitation in 91% [23], reduction in functional outcome swallowing scale (FOSS) scores by 1.4 of 6 points [17], and significant reduction in EAT-10 scores by 11.2 points [15]. These improvements seemed durable in the vast majority of these patients with an average follow-up of over 4 years.
Complications
Potential complications of endoscopic laser-assisted diverticulotomy are similar to that of stapler-assisted procedures and include esophageal perforation, which may require external drainage, mediastinitis, dental injury, subcutaneous emphysema, bleeding, temporary regurgitation of liquids, and throat pain [15, 24]. In the aforementioned patient satisfaction study, an 8% complication rate was identified, including 2% rate of mediastinitis [22]. In Kuhn’s series evaluating KTP laser diverticulotomy of ten patients, 10% had subcutaneous emphysema, and 20% had postoperative fever (over 101.5 °F), though there were no major complications [6].
Endoscopic Stapler-Assisted Versus Laser-Assisted Diverticulotomy
Both stapler-assisted and laser-assisted techniques can be successfully used to manage patients with ZD and provide myriad benefits over the traditional open approach. Endoscopic techniques lead to similar or better outcomes and have fewer complications. When compared to an open approach, laser techniques offer an improved postoperative course, shorter operative time, and potentially shorter hospital course [25]. Stapler-assisted techniques offer shorter operative time, reduced hospital stay, earlier initiation of oral intake, and lower overall complication rates [26,27,28,29,30,31,32].
Outcomes
Both endoscopic laser-assisted and stapler-assisted Zenker diverticulotomy offer symptom relief and a high degree of patient satisfaction [21, 32]. Postoperative outcomes with regard to swallowing are similar despite method of endoscopic management. In the 2016 study by Barton et al., an improvement in postoperative dysphagia scores on the EAT-10 improved by an average of 8.0 points out of 40, with no statistically significant difference in improvement based on endoscopic technique [15]. It is important to note that this study was not a head-to-head comparison of techniques, rather an analysis of safety and efficacy of endoscopic treatment using both stapler- and laser-assisted techniques to resolve symptoms by transoral means. Secondary outcomes, such as length of hospitalization or length of time to initiation of oral intake, can be difficult to compare between the two techniques since most centers use different postoperative protocols for each procedure. Regardless, Chang et al. performed a review of the literature as it pertains to the endoscopic surgical treatment for ZD and found that those treated with laser-assisted diverticulotomy experience an average of 2.2 days to initiation of oral intake and mean hospital stay of 6.5 days, compared to an average of 1.0 day to initiation of oral intake and a mean hospital stay of 1.8 days in the stapler-assisted group [25]. Therefore, postoperative outcomes favoring stapler-assisted technique include a shorter duration of nil per os (NPO) status [26, 40] and a decreased length of hospitalization [16, 18, 33]. Additionally, a lower incidence of postoperative fevers [18] and abnormal chest X-rays are seen following stapler-assisted Zenker diverticulotomy [33]. On the contrary, though patients undergoing either laser- and stapler-assisted endoscopic diverticulotomy experience significant improvement in both dysphagia and regurgitation [15, 16, 34], a greater improvement in these outcomes has been shown in those patients who underwent laser-assisted procedures in some studies [15, 33, 34].
Revision Rate
In most studies, a lower revision rate has been reported in those undergoing endoscopic laser Zenker diverticulotomy as compared to endoscopic staple-assisted diverticulotomy [33,34,35]. Other reports have demonstrated no significant difference in revision rate when comparing endoscopic stapler-assisted and laser-assisted techniques [15, 18, 33]. If reoperation is required, however, the length of time to reoperation has been shown to be significantly shorter in the stapler-assisted group [18]. Because a more complete and precise diverticulotomy can be performed with the laser, this may contribute to the lower revision rate seen compared to stapler-assisted procedures [15, 34].
Complications
Complications in both procedures are typically uncommon and relatively minor, and mortality after both procedures has rarely been reported [34, 35]. The most common operative complication of either endoscopic technique was dental trauma [34], which may be prevented by the judicious use of dental protection and careful insertion and suspension of the diverticuloscope. An increased risk of non-dental complications is seen with the CO2 laser technique; however, no statistically significant difference in overall complications, dental complications, or major complications is reported in most studies [33]. The Barton et al. study demonstrated an overall complication rate of 8% when evaluating all methods of endoscopic diverticulotomy, though all of the complications were noted in patients undergoing a laser-assisted procedure [15]. All complications were minor, including transient subcutaneous emphysema (5%), dental injury (2%), esophageal perforation (1%), and temporary regurgitation of liquids (1%). In Chang et al.’s literature review, patients undergoing endoscopic laser-assisted Zenker diverticulotomy experienced a complication rate of 7.4%, compared to a complication rate of 2.6% in stapler-assisted diverticulotomy [26]. Other studies have shown overall higher complication rates: 31% in laser procedures and 11% in stapler-assisted procedures [16]. Cervical subcutaneous emphysema or the presence of extra-esophageal air on lateral neck X-ray has been reported to occur more frequently in those patients undergoing laser diverticulotomy. When this occurs, it frequently resolves within 24 h without further complication (such as radiographic evidence of perforation) but must be followed until resolution [16, 18, 34].
Alternative Methods of Endoscopic Diverticulotomy
In recent decades, additional methods of endoscopic diverticulotomy have been explored. These techniques utilize alternative means for dividing the tissue within the common wall and performing the cricopharyngeal myotomy.
In 2009, Fama et al. was the first to describe the use of the Harmonic scalpel to perform the endoscopic diverticulotomy [10]. The Harmonic scalpel (Ethicon Inc., Somerville, NJ) is an ultrasonic transduction device, by which high-frequency vibrations in the transducer tip, creating mechanical energy, divide and coagulate tissue. This high-frequency disruption of tissues results in low-temperature coagulation and is commonly utilized in other head and neck procedures, including neck dissection and thyroidectomy. In this initial report, 25 patients were treated with the Harmonic scalpel, and complication rates were similar to other endoscopic techniques (8% postoperative chest pain, 4% postoperative cardiac event, 4% aspiration pneumonia, 4% transient cervical emphysema). Several additional smaller case series [36,37,38] showed similar rates of persistent symptoms and complications when comparing Harmonic scalpel-assisted and traditional endoscopic techniques. One study even reported the safe and efficacious use of a Harmonic scalpel through a flexible endoscope [39]. However, a more recent and larger series showed an increased rate of complications in Harmonic scalpel-assisted procedures (25%) compared to stapler-assisted procedures (5%) [12].
Another method recently introduced in the literature is endoscopic diverticulotomy with bipolar diathermic electrocoagulation (LigaSure, Medtronic, Minneapolis, MN) [11]. This electrosurgical device uses bipolar cautery to effect rapid coagulation and division of tissue. While similar to ultrasonic electrosurgery, this method may create similar tissue coagulum with less thermal injury and reduce the risk of fibrosis and stenosis at the surgical site. First described by Nielsen et al. in 2010 for the treatment of ZD in 15 patients, 80% of patients treated with bipolar electrocautery had resolution of symptoms in the long term, although 1 patient (7%) had an esophageal perforation requiring treatment with long-term antibiotics [11]. Several small case studies show promising efficacy and complication rates, which are similar to standard endoscopic techniques [40,41,42,43]. However, given the lack of large patient studies with long-term results, further study is needed to determine whether these alternative methods may replace more widely accepted techniques.
Postoperative Management
The management of patients undergoing endoscopic Zenker diverticulotomy in the immediate postoperative period is crucial to a safe and efficacious outcome. Although postoperative management protocols differ based on institution and surgeon preference, general guidelines and principles should be followed. Management also differs by type of endoscopic procedure performed. For example, since endoscopic laser diverticulotomy places patients at higher risk for esophageal perforation, they should be observed more closely or kept NPO longer than those undergoing a stapler-assisted procedure. The focus of postoperative management should be to reduce the risk of mediastinitis and infection. Signs and symptoms of mediastinitis include tachycardia, fever, chest pain, EKG changes, diaphoresis, and a general sense of unexplained discomfort and require immediate evaluation and intervention.
Postoperative management protocols following endoscopic cricopharyngeal myotomy vary in the literature and among practitioners, without a standard algorithm or process by which to follow. One published protocol immediately advances patients to a clear liquid diet on postoperative day 0 and to a soft diet on postoperative day 1 with discharge once diet is tolerated [17]. Another protocol maintains NPO until postoperative day 1, at which time they are initiated on a clear liquid diet and advanced to a soft mechanical diet prior to discharge home [16]. In a more conservative approach, patients are kept NPO until postoperative day 3, when they are advanced to a clear liquid diet and then to a full liquid diet prior to discharge, with advancement to a mechanical soft and regular diet as an outpatient [34].
In general, patients undergoing stapler-assisted endoscopic diverticulotomy are at lowest risk for esophageal perforation; this is due to the staple lines sealing the mucosal incisions along the diverticulopharyngeal wall and creating a water-tight seal of the tissue edges. Therefore, the postoperative management protocol tends to be more liberal than with other procedures. In the absence of concerning symptoms or findings in recovery, patients may be discharged home the same day and initiate a clear liquid diet on postoperative day 0. Indeed, a study by Gross et al. demonstrated the safety of discharge home from the recovery room on a liquid and soft food diet in uncomplicated cases if the patients could swallow adequately before discharge [44]. It is important to note that patients should be counseled extensively regarding symptoms concerning for mediastinitis and advised to present immediately to an emergency department should they develop concern for these. If the patient tolerates the clear liquid diet, they may be advanced to a soft mechanical diet and maintained on this until they are seen in follow-up several weeks later.
Patients undergoing laser-assisted endoscopic diverticulotomy are likely safest if observed until at least postoperative day 1. As the mucosal incisions are not routinely closed in these procedures, the risk for esophageal perforation is significant. Overnight observation allows the patient to be monitored for signs of mediastinitis , allowing for prompt diagnosis and management. Subcutaneous emphysema may be seen occasionally and, although worrisome, does not necessarily herald the development of mediastinitis. Though not all practitioners will obtain routine postoperative imaging, an esophagram obtained prior to initiation of oral intake can rule out a significant esophageal perforation. The absence of concerning findings on imaging can allow the practitioner to feel confident initiating oral intake trials if there is no evidence of leak [15, 18]. The patient is then advanced to a diet of all liquids and soft foods and discharged home. In our experience, patients may advance their own diet after 2 weeks to an unrestricted diet and be seen at approximately 4 weeks to assess response to surgery.
Some authors do not advocate for routine standard imaging unless there is clinical concern postoperatively. In those patients who demonstrate clinical concern for a postoperative complication, a lateral neck X-ray or CT neck and chest should be considered. If this demonstrates free air within the neck, the patient should be maintained NPO, and serial daily imaging examinations should be obtained until resolution is evident. If clinical decompensation or failure of resolution is apparent, a radiographic swallow study should be obtained to assess for a leak [17]. If at any point an esophageal perforation is identified, a nasogastric feeding tube should be placed under fluoroscopic guidance, and the patient maintained NPO for at least 1 week. Such placement may be challenging, and, as such, the authors (and others) choose to place a 10–12 Fr. nasogastric tube in all patients who undergo laser-assisted diverticulotomy or have anything to suggest concern during stapler-assisted diverticulotomy [15, 18].
The algorithms for postoperative diet advancement described above are not necessarily applicable to patients who were fed preoperatively via a gastrostomy tube or are at high risk of aspiration; instead, these patients require additional assessment and consideration prior to initiation of an oral diet.
Conclusion
ZD can be safely and effectively managed with endoscopic techniques. Through technological and procedural advancements, the vast majority of patients can be treated endoscopically. Patients with large ZD and favorable anatomy should be treated with stapler-assisted endoscopic diverticulotomy. However, patients with more difficult diverticular exposure, recurrent diverticula, or smaller diverticula may require a laser-assisted endoscopic approach. Although these approaches are preferred, other minimally invasive techniques, such as septotomy via flexible esophagoscopy, remain available as alternatives. With careful patient selection, precise surgical technique, and conservative postoperative practices, patients with ZD treated endoscopically have minimal risk of complications and excellent functional results.
References
Zenker FA, Zeimssen H. Dilatations of the esophagus. Cyclopedia Pract Med. 1878;3:46–8.
Gaub OJ, Jackson C. Pulsion diverticulum of the esophagus: a new operation for its cure. Surg Gynecol Obstet. 1915;21:52.
Mosher HP. Webs and pouches of the oesophagus, their diagnosis and treatment. Surg Gynecol Obstet. 1917;25:175–87.
Dohlman G, Mattsson O. The endoscopic operation for hypopharyngeal diverticula: a roentgencinematographic study. AMA Arch Otolaryngol. 1960;71:744–52.
van Overbeek JJ, Hoeksema PE, Edens ET. Microendoscopic surgery of the hypopharyngeal diverticulum using electrocoagulation or carbon dioxide laser. Ann Otol Rhinol Laryngol. 1984;93(1 Pt 1):34–6.
Kuhn FA, Bent JP III. Zenker’s diverticulotomy using the KTP/532 laser. Laryngoscope. 1992;102(8):946–50.
Collard JM, Otte JB, Kestens PJ. Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Ann Thorac Surg. 1993;56(3):573–6.
Martin-Hirsch DP, Newbegin CJ. Autosuture GIA gun: a new application in the treatment of hypopharyngeal diverticula. J Laryngol Otol. 1993;107(8):723–5.
Scher RL, Richtsmeier WJ. Endoscopic staple-assisted esophagodiverticulostomy for Zenker’s diverticulum. Laryngoscope. 1996;106(8):951–6.
Fama AF, Moore EJ, Kasperbauer JL. Harmonic scalpel in the treatment of Zenker’s diverticulum. Laryngoscope. 2009;119(7):1265–9.
Nielsen HU, Trolle W, Rubek N, Homoe P. New technique using LigaSure for endoscopic mucomyotomy of Zenker’s diverticulum: diverticulotomy made easier. Laryngoscope. 2014;124(9):2039–42.
Whited C, Lee WT, Scher R. Evaluation of endoscopic harmonic diverticulostomy. Laryngoscope. 2012;122(6):1297–300.
van Overbeek JJ. Meditation on the pathogenesis of hypopharyngeal (Zenker’s) diverticulum and a report of endoscopic treatment in 545 patients. Ann Otol Rhinol Laryngol. 1994;103(3):178–85.
Aly A, Devitt PG, Jamieson GG. Evolution of surgical treatment for pharyngeal pouch. Br J Surg. 2004;91(6):657–64.
Barton MD, Detwiller KY, Palmer AD, Schindler JS. The safety and efficacy of endoscopic Zenker’s diverticulotomy: a cohort study. Laryngoscope. 2016;126(12):2705–10.
Miller FR, Bartley J, Otto RA. The endoscopic management of Zenker diverticulum: CO2 laser versus endoscopic stapling. Laryngoscope. 2006;116(9):1608–11.
Bergeron JL, Chhetri DK. Indications and outcomes of endoscopic CO2 laser cricopharyngeal myotomy. Laryngoscope. 2014;124(4):950–4.
Verhaegen VJ, Feuth T, van den Hoogen FJ, Marres HA, Takes RP. Endoscopic carbon dioxide laser diverticulostomy versus endoscopic staple-assisted diverticulostomy to treat Zenker’s diverticulum. Head Neck. 2011;33(2):154–9.
Halvorson DJ, Kuhn FA. Transmucosal cricopharyngeal myotomy with the potassium-titanyl-phosphate laser in the treatment of cricopharyngeal dysmotility. Ann Otol Rhinol Laryngol. 1994;103(3):173–7.
Ho AS, Morzaria S, Damrose EJ. Carbon dioxide laser-assisted endoscopic cricopharyngeal myotomy with primary mucosal closure. Ann Otol Rhinol Laryngol. 2011;120(1):33–9.
Nyrop M, Svendstrup F, Jorgensen KE. Endoscopic CO2 laser therapy of Zenker’s diverticulum--experience from 61 patients. Acta Otolaryngol Suppl. 2000;543:232–4.
Wouters B, van Overbeek JJ. Endoscopic treatment of the hypopharyngeal (Zenker’s) diverticulum. Hepatogastroenterology. 1992;39(2):105–8.
Anagiotos A, Feyka M, Eslick GD, Lichtenstein T, Henning TD, Guntinas-Lichius O, et al. Long-term symptom control after endoscopic laser-assisted diverticulotomy of Zenker’s diverticulum. Auris Nasus Larynx. 2014;41(6):568–71.
Lim RY. Endoscopic CO2 laser cricopharyngeal myotomy. J Clin Laser Med Surg. 1995;13(4):241–7.
Chang CW, Burkey BB, Netterville JL, Courey MS, Garrett CG, Bayles SW. Carbon dioxide laser endoscopic diverticulotomy versus open diverticulectomy for Zenker’s diverticulum. Laryngoscope. 2004;114(3):519–27.
Chang CY, Payyapilli RJ, Scher RL. Endoscopic staple diverticulostomy for Zenker’s diverticulum: review of literature and experience in 159 consecutive cases. Laryngoscope. 2003;113(6):957–65.
Gutschow CA, Hamoir M, Rombaux P, Otte JB, Goncette L, Collard JM. Management of pharyngoesophageal (Zenker’s) diverticulum: which technique? Ann Thorac Surg. 2002;74(5):1677–82, discussion 1682–3.
Philippsen LP, Weisberger EC, Whiteman TS, Schmidt JL. Endoscopic stapled diverticulotomy: treatment of choice for Zenker’s diverticulum. Laryngoscope. 2000;110(8):1283–6.
Raut VV, Primrose WJ. Long-term results of endoscopic stapling diverticulotomy for pharyngeal pouches. Otolaryngol Head Neck Surg. 2002;127(3):225–9.
Scher RL. Endoscopic staple diverticulostomy for recurrent Zenker’s diverticulum. Laryngoscope. 2003;113(1):63–7.
Smith SR, Genden EM, Urken ML. Endoscopic stapling technique for the treatment of Zenker diverticulum vs standard open-neck technique: a direct comparison and charge analysis. Arch Otolaryngol Neck Surg. 2002;128(2):141–4.
van Eeden S, Lloyd RV, Tranter RM. Comparison of the endoscopic stapling technique with more established procedures for pharyngeal pouches: results and patient satisfaction survey. J Laryngol Otol. 1999;113(3):237–40.
Parker NP, Misono S. Carbon dioxide laser versus stapler-assisted endoscopic Zenker’s diverticulotomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2014;150(5):750–3.
Adam SI, Paskhover B, Sasaki CT. Laser versus stapler: outcomes in endoscopic repair of Zenker diverticulum. Laryngoscope. 2012;122(9):1961–6.
Pollei TR, Hinni ML, Hayden RE, Lott DG, Mors MB. Comparison of carbon dioxide laser-assisted versus stapler-assisted endoscopic cricopharyngeal myotomy. Ann Otol Rhinol Laryngol. 2013;122(9):568–74.
Allen J, Belafsky PC. Endoscopic cricopharyngeal myotomy for Zenker diverticulum using the harmonic scalpel. Ear Nose Throat J. 2010;89(5):216–8.
May JT 4th, Padhya TA, McCaffrey TV. Endoscopic repair of Zenker’s diverticulum by harmonic scalpel. Am J Otolaryngol. 2011;32(6):553–6.
Sharp DB, Newman JR, Magnuson JS. Endoscopic management of Zenker’s diverticulum: stapler assisted versus Harmonic Ace. Laryngoscope. 2009;119(10):1906–12.
Hondo FY, Maluf-Filho F, Giordano-Nappi JH, Neves CZ, Cecconello I, Sakai P. Endoscopic treatment of Zenker’s diverticulum by harmonic scalpel. Gastrointest Endosc. 2011;74(3):666–71.
Andersen MF, Trolle W, Anthonsen K, Nielsen HU, Homoe P. Long-term results using LigaSure 5 mm instrument for treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol. 2017;274(4):1939–44.
Gonzalez N, Viola M, Costa X, Gamba A. Endoscopic treatment of Zenker’s diverticulum by LigaSure scalpel. Endoscopy. 2014;46(Suppl 1 UCTN):E229–30.
Moreira da Silva BA, Germade A, Perez Citores L, Maestro Antolin S, Santos F, Sanchez Barranco F, et al. Endoscopic diverticulotomy using Ligasure. Gastroenterol Hepatol. 2017;40(2):80–4.
Noguera-Aguilar J, Dolz-Abadia C, Vilella A, Munoz-Perez JM, Canaval-Zuleta HJ, Salvatierra-Arrieta L. Transoral endoluminal approach to Zenker’s diverticulum using Ligasure. Early clinical experience. Rev Esp Enferm Dig. 2014;106(2):137–41.
Gross ND, Cohen JI, Andersen PE. Outpatient endoscopic Zenker diverticulotomy. Laryngoscope. 2004;114(2):208–11.
Lang RA, Spelsberg FW, Winter H, Jauch KW, Hüttl TP. Transoral diverticulostomy with a modified Endo-Gia stapler: results after 4 years of experience. Surg Endosc. 2007;21(4):532–6. Epub 20 Dec 2006.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Chadwick, K.A., Schindler, J.S., Krane, N.A. (2018). Non-staple Endoscopic Management of Zenker Diverticulum. In: Scher, R., Myssiorek, D. (eds) Management of Zenker and Hypopharyngeal Diverticula. Springer, Cham. https://doi.org/10.1007/978-3-319-92156-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-92156-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92155-6
Online ISBN: 978-3-319-92156-3
eBook Packages: MedicineMedicine (R0)