Abstract
Atherosclerosis is a localized disease. It develops near bifurcations and areas where shear stress, the frictional force that the blood flow exerts on the intimal surface, is low (shear stress less than 4 dynes/cm2). A classic example is the carotid sinus, where flow separation takes place in some periods of the cardiac cycle leading to low and oscillatory shear stress. Low shear results in lesions and vulnerable plaque, while in areas with vortices and variable shear more stable plaques develop, composition of these plaques also differs. Wall shear stress not only plays a role in atherosclerosis, but is also a major determinant of graft failure and intima hyperplasia following angioplasty and stenting.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords

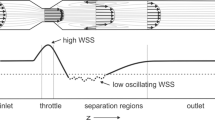
Atherosclerosis is a localized disease. It develops near bifurcations and areas where shear stress, the frictional force that the blood flow exerts on the intimal surface, is low (shear stress less than 4 dynes/cm2). A classic example is the carotid sinus , where flow separation takes place in some periods of the cardiac cycle leading to low and oscillatory shear stress. Flow patterns and location of plaques are schematically shown in the left panel. Areas of normal shear stress (>10 dynes/cm2) or areas subjected to high shear, are plaque-free, adapted from Ref. [1], used by permission. The right panel shows that low shear results in larger lesions and vulnerable plaque, while in areas with vortices and variable shear more stable plaques develop, composition of these plaques also differs, adapted from Ref. [2], by permission. Wall shear stress not only plays a role in atherosclerosis, but is also a major determinant of graft failure and intima hyperplasia following angioplasty and stenting.
1 Description
Hemodynamic forces not only regulate blood vessel geometry and structure, i.e., remodeling, but they can be considered also as main factors influencing the development of different forms of vascular disease, such as atherosclerosis and aneurysms. Of particular importance is the role of shear stress, the minute force resulting from the friction that the flowing blood exerts on the luminal surface, on the localization and development of atherosclerosis.
Atherosclerosis is associated with genetic predisposition and systemic factors such as hypertension, hyperlipidemia, smoking, etc. However, the localized nature of the disease, which occurs principally in areas of disturbed flow such as near bifurcations and curvatures, cannot be explained by systemic factors that apply equally throughout the vasculature. It is recognized today that atherosclerosis develops in areas where shear stress is low, typically less than 4 dyn/cm2, or 0.4 Pa, and changes direction during the cardiac cycle. An example is the wall of the carotid sinus , where local shear is low and flow separates during the decelerating phase of the heart cycle, leading to flow separation and thus flow reversal and change in shear stress direction (left panel of Figure in the Box). Other areas where low shear stress co-localizes with atherosclerosis are the coronaries, the infrarenal aorta and the femoral artery.
1.1 Shear Stress and Endothelial Function
Apart from its non-thrombogenic protective role, the endothelial layer constitutes the mechano-sensing element, which senses the local flow conditions and produces autocrine and paracrine factors for the functional regulation of the arterial wall. Studies of endothelial cells in vitro and in vivo have revealed the deleterious effect of low and oscillatory, vortex-related, shear stress on endothelial function. Under physiological shear (σ > 10 dyn/cm2) endothelial cells align in the direction of flow whereas they do not when exposed to low shear (σ < 4 dyn/cm2). Low and oscillatory shear stress lead to inhibition of NO-synthase, greater endothelial cell cycling and increase in apoptosis. Low and oscillatory shear also contribute to local endothelial dysfunction, which may lead to enhanced monocyte adhesion, increased platelet activation, increased vasoconstriction, increased smooth muscle cell proliferation, and increased oxidant activity, thus constituting a likely model for atherogenesis. It has been shown that low shear stress in combination with flow patterns such as vortices determine the type of plaque, both in composition and vulnerability (right panel of Figure in the Box). Low shear results in vulnerable plaque while vortex-based shear results in more stable plaque [2]. High shear stress induces an atheroprotective endothelial phenotype, increases NO production, and decreases the expression of vasoconstrictors, inflammatory response mediators, adhesion molecules and oxidants.
Detailed discussion on the relation between shear stress and endothelial function can be found in the review articles by Davies et al. [3] and Malek et al. [1].
2 Physiological and Clinical Relevance
2.1 Assessing Risk for Atherosclerosis
Ultrasound measurements in the carotid artery of healthy young adults aged 28–38 years revealed a significant inverse relation between the measured intima-media thickness and local shear stress. This suggests that there is a prognostic value in the assessment of local wall shear levels using noninvasive techniques, such as ultrasound Doppler or MRI.
Since the velocity profile near a bifurcation depends strongly on the geometry, it has been suggested that there exist ‘geometrical risk’ factors for atherosclerosis. Certain branching geometries, i.e., high curvatures and large angles, may predispose to atherosclerosis because they would lead more easily to flow separation and low shear stress regions [4].
2.2 Shear Stress and Intima Hyperplasia in Vein Grafts
Intima hyperplasia in vein grafts is also sensitive to wall shear. Dobrin et al. [5] examined the effect of all mechanical factors (pressure, extension, and shear stress) on intima hyperplasia and medial thickening in autogenous vein grafts in dogs. Autologous vein grafts were used to bypass a segment of the femoral artery. The femoral artery on one side was ligated, so that all femoral blood flow passed through the graft. The femoral artery at the opposite side was left patent, which permitted only part of the flow to pass through the vein graft. A stiff cuff was placed over the middle section of the vein grafts impeding radial expansion. Cross-sectional areas are given in Fig. 30.1. The results show that intima hyperplasia is greater on both sides, in the distended, low shear, regions, than in the regions constrained by the cuffs, thus at high shear. Furthermore, intima hyperplasia was globally lower on the side with high flow, obtained by femoral artery ligation, as compared to the side were femoral artery was left patent, i.e., low flow.
Intimal hyperplasia in vein grafts. (Adapted from Ref. [5], by permission)
2.3 Shear Stress and Intima Hyperplasia in Bypass Grafts
High shear stress inhibits neointima formation in artificial ePTFE grafts. Animal experiments have shown that exposure of implanted grafts to higher shear, by means of distal arterio-venous fistulas, leads to a decrease in the thickness of the already existing neointima hyperplasia.
Low and oscillatory wall shear stress patterns may also be responsible for the failure of bypass grafts. In the vicinity of an end-to-side anastomosis, blood flow is greatly disturbed. This is mainly due to the abrupt change in geometry. For vascular grafts, intima hyperplasia develops preferentially at the ‘toe’ and the ‘heel’ of the anastomosis. These are exactly the locations where flow separation, low wall shear stress and large gradients of wall shear stress take place.
2.4 Intima Hyperplasia Following Angioplasty and Stenting
Restenosis is an undesirable occlusive response to stent implantation after balloon angioplasty. In contrast to balloon angioplasty, where acute or sub-acute recoil represents the major mechanism of restenosis, stent restenosis is exclusively attributed to neointima proliferation, a tissue reaction often termed intima hyperplasia (IH). Morphological studies have demonstrated that neointima is caused by early smooth muscle cell ingrowth, which is then gradually replaced by extracellular matrix.
There is a good deal of scientific evidence that intima hyperplasia is sensitive to flow. Kohler and Jawien [6] studied the effects of flow on intima hyperplasia after balloon injury of the rat common carotid. Flow was increased, by ~35%, by ligation of the opposite common carotid artery or decreased, also by ~35%, by ligation of the ipsilateral internal carotid. Two weeks after the intervention, intima thickness, indicated by the distance between the artery lumen and arrow, was significantly smaller in the high flow group (Fig. 30.2a) as compared with the low-flow group (Fig. 30.2b).
Histological sections of the rat carotid subjected to high flow (a) and low flow (b) indicating the degree of intimal hyperplasia 2 weeks after balloon injury. (Adapted from Ref. [6], by permission)
There appears also to be strong clinical evidence for the relation between post interventional flow and patency of balloon angioplasty. If local flow, and thus wall shear stress, after balloon angioplasty is high, the artery is expected to remain patent. This observation, common to many physicians practicing balloon angioplasty, is substantiated by studies reporting increased long-term patency after angioplasty in lower extremity arteries when flows are high. Direct clinical proof of the inverse relationship between wall shear stress and intima thickness was given by Wentzel et al. [7]. Computational fluid dynamics simulations of the flow field within a stented carotid artery have demonstrated that athero-prone regions co-localize with stent mal-apposition and stent strut interconnections [8].
The restenosis problem following stent placement has been drastically reduced with the use of drug-eluting stents. Drug-eluting stents with the capability to deliver anti-inflammatory or anti-proliferative drugs directly to the adjacent arterial tissue, inhibit neointima hyperplasia and restenosis.
2.5 Shear Stress and Aortic Aneurysm
Cerebral aortic aneurysms have a saccular, eccentric shape that can be digitally removed to retrieve the aortic geometry prior to disease. Such artificially generated ‘baseline’ geometries have been used to relate computationally obtained shear stress descriptors with the onset of cerebral aneurysm formation [9]. Long time follow-up of cerebral aneurysms further demonstrated that those areas experiencing lowest time-averaged wall shear stress are also the areas where the aneurysm grows most. Due to the recirculation of blood the dilated zone of the aneurysm experiences locally decreased and oscillatory shear stress that accelerates the local process of inflammation and proteolysis, thus entering into a vicious circle [10]. Abdominal aortic aneurysms on the other hand have a diffuse shape that makes it impossible to retrieve the original, non-diseased geometry. That is why most research on the role of shear stress in aneurysm initiation is performed in mice [11]. Computationally derived wall shear stress patterns have demonstrated a decreased shear stress in patients with spinal cord injury, which may be linked to the higher incidence of aneurysm formation in these patients [12]. Computational models of patient-specific abdominal aortic aneurysms have been used to demonstrate that the deposition of intraluminal thrombus is most likely driven by local hemodynamics [13].
References
Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 1999;282:2035–42.
Cheng C, Tempel D, van Haperen R, van der Baan A, Grosveld F, Daemen MJ, et al. Atherosclerotic lesion size and vulnerability are determined by patterns of fluid shear stress. Circulation. 2006;113:2744–53.
Davies PF, Barbee KA, Lal R, Robotewskyj A, Griem ML. Hemodynamics and atherogenesis. Endothelial surface dynamics in flow signal transduction. Ann N Y Acad Sci. 1995;748:86–102. discussion 102-103
Goubergrits L, Affeld K, Fernandez-Britto J, Falcon L. Atherosclerosis in the human common carotid artery. A morphometric study of 31 specimens. Pathol Res Pract. 2001;197:803–9.
Dobrin PB, Littooy FN, Endean ED. Mechanical factors predisposing to intimal hyperplasia and medial thickening in autogenous vein grafts. Surgery. 1989;105:393–400.
Kohler T, Jawien A. Flow affects development of intimal hyperplasia after arterial injury in rats. Arterioscler Thromb. 1992;12:963–71.
Wentzel JJ, Krams R, Schuurbiers JC, Oomen JA, Kloet J, Van der Giessen WJ, et al. Relationship between neointimal thickness and shear stress after Wallstent implantation in human coronary arteries. Circulation. 2001;103:1740–5.
De Santis G, Conti M, Trachet B, De Schryver T, De Beule M, Degroote J, et al. Impact of stent-vessel (mal) apposition following carotid artery stenting: mind the gaps! Ann Biomed Eng. 2013;16:648–59.
Mantha A, Karmonik C, Benndorf G, Strother C, Metcalfe R. Hemodynamics in a cerebral artery before and after the formation of an aneurysm. AJNR Am J Neuroradiol. 2006;27:1113–8.
Boussel L, Rayz V, McCulloch C, Martin A, Acevedo-Bolton G, Lawton M, et al. Aneurysm growth occurs at region of low wall shear stress: patient-specific correlation of hemodynamics and growth in a longitudinal study. Stroke. 2008;39:2997–3002.
Trachet B, Renard M, De Santis G, Staelens S, De Backer J, Antiga L, et al. An integrated framework to quantitatively link mouse-specific hemodynamics to aneurysm formation in angiotensin II-infused ApoE −/− mice. Ann Biomed Eng. 2011;39:2430–44.
Yeung JJ, Kim HJ, Abbruzzese TA, Vignon-Clementel IE, Draney-Blomme MT, Yeung KK, et al. Aortoiliac hemodynamic and morphologic adaptation to chronic spinal cord injury. J Vasc Surg. 2006;44:1254–65.
Di Achille P, Tellides G, Humphrey JD. Hemodynamics-driven deposition of intraluminal thrombus in abdominal aortic aneurysms. Int J Numer Method Biomed Eng. 2017;33:e2828.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Westerhof, N., Stergiopulos, N., Noble, M.I.M., Westerhof, B.E. (2019). Blood Flow and Arterial Disease. In: Snapshots of Hemodynamics. Springer, Cham. https://doi.org/10.1007/978-3-319-91932-4_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-91932-4_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-91931-7
Online ISBN: 978-3-319-91932-4
eBook Packages: MedicineMedicine (R0)