Abstract
Cancer patients show a hypercoagulable state with a high risk for thrombosis and pulmonary embolism, due to the malignancy itself as well as various therapies used. Real-world data suggest that the necessary thromboprophylaxis is still underused. In the palliative care setting, patients seem willing to accept the use of subcutaneous low-molecular-weight heparin (LMWH) injections as compared to compression stockings because of the greater efficacy. However, the advent of “direct” or “new” oral anticoagulants (direct oral anticoagulants [DOACs], novel oral anticoagulants, or non-vitamin K oral coagulants [NOACs]) is likely to change the landscape of anticoagulation in cancer patients if the current efficacy and toxicity data are confirmed.
The provident and structured use of blood products in patients undergoing anticancer therapy reduces the need for them including their sequelae. This also reduces the economic strain on this part of the healthcare system. Bleeding complications in cancer patients undergoing surgery are relatively frequent, and novel strategies for perioperative risk stratification and correspondent therapies in cancer patients have been developed. More clinical research is needed to improve our understanding of thrombosis and bleeding in cancer patients.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The writings of Virchow in 1856 were the first descriptions on the way to the understanding of the pathogenesis of thrombosis [1]. Hypercoagulability is a frequent phenomenon in cancer patients. Published knowledge dates back to Armand Trousseau, who described a tendency to “spontaneous coagulation” in two patients with phlegmasia alba dolens and gastric cancer [2]. Since these observations, much progress has been made; it has become clear that activation of blood coagulation not only is a result of the presence of malignant cells; rather, it makes part of the malignant process [3]. Recent years have shown that the pathophysiology is likely to be different in different types of cancer [3, 4]; for example, specific genetic alterations associated with increased thrombogenicity in myeloproliferative diseases, different from solid tumors, have been identified [5]. In general, however, cancer patients display a procoagulant phenotype [6]. But cancer patients are also prone to bleeding due to the properties of the tumor, during interventions or when a disseminated intravascular coagulation [DIC] occurs [7, 8]. This chapter will review the important issues of thrombosis and bleeding in cancer patients from a practical point of view.
Epidemiology of Hypercoagulability in Cancer Patients
There is ample evidence that cancer patients frequently show increased biochemical markers of plasmatic and platelet coagulation activation (increased prothrombin fragment 1 + 2 and thrombin-antithrombin complex), generation of soluble fibrin (increased fibrinopeptide A and B), fibrin generation and degradation (increased fibrin degradation products, D-dimer), and surrogates of continued platelet activation [9,10,11]. Such markers of overall coagulation activation prove the procoagulant phenotype [12, 13] in cancer patients. Besides, some of these markers such as fibrin monomer or D-dimer have been shown to be associated with tumor spread [14] as well as progression, response to therapy, and survival [15,16,17]. In addition, certain genotypes of coagulation proteins seem associated with survival and response to therapy (e.g., PAI-1 in testicular cancer [18] and TFPI in breast cancer [19]), although this is, for now, not part of a management algorithm.
Depending on the type of cancer and the state of the disease, increased surrogate markers of coagulation activation can be found in up to 90% of patients. However, one has to recognize that coagulation proteins and markers of coagulation activation make part of a dynamic phenomenon: even largely increased markers of coagulation activation are not predictive of the occurrence of a thromboembolic event in the single patient, although the relative risk is increasing with increasing activation marker concentrations [10, 16, 20,21,22]. On the other hand, it is well documented that cancer patients have a high prevalence of clinically silent thrombi, as shown by the fact that cancer patients have a high prevalence of thrombi that are detected at autopsy only [23,24,25].
Venous thromboembolism (VTE) that is cancer associated can precede cancer diagnosis. The highest risks for VTE before a cancer diagnosis is made are found in acute myelogenous leukemia (AML), non-Hodgkin lymphoma (NHL), and renal, ovarian, and pancreatic cancer (approximately three- to fourfold increased risk); the overall risk in cancer patients to develop a VTE as a sign of (the still undetected) cancer is approximately 1.3 [26]. In the first 2 years after a VTE diagnosis is made, the greatest risks for being diagnosed with cancer are found for lymphoma (approximately fivefold) and ovarian cancer (approximately sevenfold) [27]. Prospective studies have also confirmed the association between overt malignancy and VTE. A prospective case-control study of 3220 patients with VTE revealed an overall sevenfold increased risk in patients with cancers. Hematologic malignancies had the highest risk (OR 28), whereas solid tumors had ORs from 2 to >20 [28]. Comparable results for VTE in lymphoma, leukemia, and plasma cell dyscrasias were described in other studies [29]. Besides, various additional comorbidities, including various forms of cancer, are associated with an increased risk of dying in patients admitted to the hospital for VTE [30].
The tumor itself is able to induce (mainly) procoagulant changes, but such changes are also found in relationship to cancer treatment. In a US study, 8% of 66,000 (neutropenic) cancer patients hospitalized were found to develop thromboembolic events (5% venous, 15% arterial events during first hospital admission) [31]. The highest incidence for VTE was found in leukemias and lymphomas and pancreatic, brain, endometrial, or cervical cancer; on the other hand, arterial thrombosis was most commonly seen in hematological malignancies and prostate, lung, and bladder cancer [32]. Immunomodulatory therapy in multiple myeloma is associated with an increased risk for VTE [33]. These observations are well in line with those in other patient cohorts of chemotherapy in solid cancer with an incidence of VTE of 7% within 3 months after chemotherapy and an annual incidence of 11% [34].
Besides its overall predictive properties in hospitalized patients [30], VTE is a significant predictor of a 2-year mortality in breast cancer patients with the greatest effect in patients with local- or regional-stage (hazard ratio 3.5–5) breast cancer [35]. These and similar observations [26] suggest that survival is worse the closer VTE and cancer diagnosis come together. This might be due to a more advanced cancer stage in such situations.
Pathogenesis of Thromboembolism in Cancer Patients
According to Virchow, the main reasons for the occurrence of a thrombosis are changes in blood flow, vessel integrity, and composition of the blood [1]. Aberrant blood flow is frequently observed in situations associated with hyperviscosity, which can derive from both fluid and cellular blood components. As perfusion problems due to hyperviscosity frequently occur in small vessels first, it is easy to understand from a mechanistic point of view that the brain, the heart, the lungs, and the kidneys are frequently affected, with the resulting clinical manifestations [36]. Laboratory tests for hyperviscosity are infrequently performed. Therefore, the recognition of hyperviscosity usually depends on clinical suspicion and supporting laboratory data, e.g., increased monoclonal proteins in multiple myeloma [37]. These can affect flow characteristics via several mechanisms [38]; as hyperviscosity is also a function of the size of the molecules involved, it is most common with IgM paraproteins [39]. Other (rare) reasons for hyperviscosity can be light chain disease as well as cryofibrinogenemia and cryoglobulinemia [40]. Fibrinogen , which significantly influences blood viscosity and is frequently increased in cancer patients [41], is, as are other hemostatic markers, dependent on the course of the malignant disease [16].
Further important reasons for hyperviscosity are massively increased cell counts [42]. A high hematocrit can convey hyperviscosity , as can be deduced from the thromboembolic risk that is well documented for polycythemia vera (P. vera) patients; thromboembolism is the most frequent cause of death in P. vera [43]. Other factors seem to play important roles, too, such as platelet activation (increased thromboxane formation) [44]) and JAK-2 mutations, shown to be involved in the development of myeloproliferative diseases; specifically, the incidence of thromboembolism seems to depend on the number of alleles affected, but the exact mechanism remains to be elucidated [4, 45,46,47].
Leukostasis can occur within the microcirculation of the central nervous and respiratory system when hyperleukocytosis is present. It can occur in chronic leukemias, especially chronic myeloid leukemia, but it is rather seen in AML variants with increased blast adhesiveness [48]. Leukostasis is much less frequently seen in lymphoid leukemias: lymphocytes are smaller and seem to have a lower adherence to vasculature, specifically in chronic lymphocytic leukemia (CLL) [49]. Different from myeloid leukemias, leukostasis in lymphoid leukemia might need additional risk factors such as a concurrent infection to upregulate adhesive cell surface molecules in order to precipitate clinical symptoms.
Thrombocytosis is associated with an increased risk for VTE in cancer patients as well: patients with a platelet count of >350 G/l have a significantly increased risk [50, 51]. Also, there is evidence that physical properties such as mean platelet volume (MPV) [52] as well as the degree of platelet activation [21] are associated with the risk for thrombosis in cancer patients.
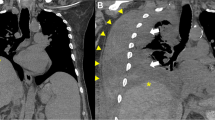
As most solid tumors or affected lymph nodes grow expansively at some point in time, vessel compression is a further potential reason for the occurrence of VTE in cancer patients. However, the classical example for this situation, the superior vena cava syndrome (SVCS) , is probably much rarer than perceived. In a large retrospective cohort of more than 34,000 patients, only 6 had SVCS thrombosis and most had to be attributed to central lines [53]. Any vein might be subject to external compression, thus a reason for VTE [54]. Cancer patients are often immobilized or have to undergo surgery; both situations result in impairment of regular circulation, inducing an additional risk factor (besides the cancer itself). That this risk is severe can be deduced from a prospective cohort in which up to 50% of the deaths early after cancer surgery were due to VTE [55].
As mentioned, direct tumor-associated vessel impairment increases the risk for VTE. Besides outside vessel compression, direct tumor cell invasion of the vessel wall might result in increased risk for VTE; also, the tumor induces tissue factor (TF)-dependent angiogenesis, thereby increasing the exposition of the blood volume to tumor-derived procoagulants [56]. The tumor itself might present as an intravascular mass that induces additional adjacent accumulation of blood cells and fibrin. Emboli directly deriving from tumors are rare but do occur, most frequently in gastrointestinal cancers [57]. This phenomenon might, for example, explain the reduced survival in hepatocellular carcinoma with portal vein tumor thrombi (3-year survival 20% with vs. 56% without [58]), with the extent of the portal vein thrombus likely also being important [59]. Other tumor entities have been found to show similar phenomena.
It is well known that the procoagulant phenotype in cancer is at least partially related to cytokine trafficking from cancer cells, endothelial cells, and peripheral blood cells [60, 61]. This can lead to tissue factor (TF) (over-) expression (e.g., on monocytes), upregulation of procoagulants, downregulation of anticoagulants, platelet activation [62], or neovascularization through proangiogenic signaling [63]. Neutrophils can activate platelets via cathepsins, can produce elastase to degrade the endothelium, can expose thrombogenic subendothelium [64], and can bind to platelets via various mechanisms [65]. It was recently shown that generation of neutrophil extracellular traps (NETs) in malignancy links the neutrophils to the generation of a prothrombotic state [66], while neutrophilia is associated with an increased risk of VTE in cancer patients with chemotherapy [67].
Tumor cells produce several factors that induce the prothrombotic state in cancer. TF is increased in cancer patients [68] with DVT [69], especially in leukemia and lymphoma [70]. On the other hand, increased profibrinolytic activity might also be encountered in leukemia patients [71] as well as patients with solid tumors [8].
PAI-1 levels are frequently increased in cancer patients, which is associated with an increased risk for VTE in both cancer and non-cancer patients [72]. Whether the 4G/4G polymorphism has direct or indirect (through VTE) influence on the outcome remains to be elucidated [18].
Apoptosis of (tumor) cells results in a prothrombotic state as observed with different malignant and benign cell lines; thrombin generation seems to parallel the degree of apoptosis [73], resulting in increased prothrombotic risk. This offers a mechanistic explanation for the hypercoagulablity observed in tumor lysis syndrome as well as the increased risk of VTE during tumor therapy [74].
Very small membrane fragments are known as microparticles (MP) ; they derive from normal cells (platelets, blood cells, or endothelial cells) but can also be derived from malignant cells. Microparticles carry TF and may—through the provision of phospholipids—be involved in facilitation of complex formation and thus increased thrombin generation. Recent clinical studies have shown MP to be increased in cancer patients with different tumors [74, 75]. Procoagulant microparticles devoid of TF activity have also been described ([76] see also below).
Cancer patients can acquire a resistance against activated protein C (APC resistance) [29, 77,78,79,80], but the exact contribution of this potentially prothrombotic mechanism to the VTE phenotype is difficult to define, given the other prothrombotic mechanisms present in cancer patients.
The antiphospholipid syndrome (APS) is characterized by thromboembolism and the presence of antiphospholipid antibodies (APA, by definition against cardiolipin or β-2 glycoprotein I or a lupus anticogulant; to fulfill the diagnostic criteria for APS, the antibodies have to be found in two separate investigations at least 12 weeks apart). In lymphoma patients, APA seems not infrequent (up to 27%, with an annual rate of thrombosis of 5.1% in patients with APA and 0.75% in those without [81]), well in line with other findings [82]. As in non-cancer patients, the presence of antiphospholipid antibodies in cancer patients seems to be associated with an increased risk of thromboembolism [83, 84]. Although overall causality of the malignant process for the presence of APA seems unlikely [85, 86], some data suggest that antiphospholipid antibody-associated VTE might be the first manifestation of malignancy [84, 87]; whether or not chemotherapy modulates the VTE risk associated with APA is unclear.
Factor V Leiden is the most frequent inherited thrombophilia, also in cancer patients [88]. It confers an approximately 7-fold increased risk for DVT in heterozygotes and an 80-fold increase risk in individuals being homozygous. Overall, its presence seems to add an additional risk factor for VTE in cancer patients besides the cancer itself [89]. The prothrombin 20210A mutation causes increased prothrombin levels and is associated with a relative thrombotic risk of three in heterozygotes. It seems possible, however, that the VTE risk mediated through these most frequent congenital thrombophilias is different in different cancer patient populations [88, 90,91,92].
Iatrogenic Factors
Chemotherapies and tumor surgery frequently induce a hypercoagulable state [93, 94]. Therefore, cancer patients (and specifically those undergoing chemotherapy) have a high risk of developing thromboembolic events [95]. A special situation is encountered with the use of asparaginase in lymphoproliferative diseases; the initial phase with early reduction in protein synthesis is followed by a phase of hypercoagulability as procoagulants recover earlier than anticoagulants (mainly antithrombin); this is associated with an increased thrombin generation throughout therapy [96]. Corticosteroids , often used in conjunction, also might increase the prothrombotic risk [97]. Other chemotherapeutic regimens with procoagulant effects include cisplatin, which seems able to induce a TF-independent procoagulant response mediated through generation of (TF free) microparticles from endothelial cells [76]. Thalidomide and analogues such as lenalidomide are also prothrombotic. When used for single-agent therapy in myeloma, less than 2% of patients will develop thromboembolism [98]. In combination with steroids (dexamethasone), however, the rate increases markedly [99] [100]. Cohort studies suggest, however, that prophylaxis with low-molecular-weight heparin (LMWH) can significantly reduce the VTE risk in these patients [101].
Central venous catheters (CVC) are frequently used in order to provide a secure and reliable way for repeated access to the venous system during IV-based therapies. CVCs are believed to be thrombogenic due to the vessel injury to begin with but also because of changes in blood flow as well as provision of an artificial surface in the setting of hypercoagulability from the underlying cancer [102]. Underlying congenital thrombophilia might be an aggravating factor [103], and prevalence might differ with different access sites [104]; prospective data are missing, however. Also, data on the frequency of CVC-related venous thrombosis are not homogeneous [105,106,107,108]. In a registry of 2945 cancer patients, deep venous thrombosis (DVT) in the upper extremities overall occured in 6.7%; association with a CVC occured in 3.5% [109]. Other trials suggested ovarian cancer to induce a specific risk for CVC-related DVT [108] and thrombocytopenia to be somewhat protective in this setting.
Management of Hypercoagulable States
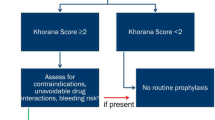
As mentioned above, VTE is frequent in cancer patients [6, 110] (with an estimated prevalence of 4–20%) and is the second greatest cause of mortality in cancer. In the past, a prospective randomized clinical landmark trial has clearly demonstrated that long-term use of daily subcutaneous LMWH is more efficient than vitamin K antagonists to prevent recurrent VTE in cancer patients [111], but a recent trial failed to confirm this [112]; a potential explanation for this outcome, besides other things, might be that cancer therapy has considerably changed over the decade that has elapsed between these trials. Various national and international guidelines [113,114,115,116] recommend the use of LMWH for 3–6 months for treatment and secondary prophylaxis of VTE in cancer patients. Despite convincing data that effective pharmacological antithrombotic prophylaxis is relevant, many caregivers still seem not to have yet modified their clinical practice [117]. This problem is of significance [118], as there is evidence that up to 40% of patients that developed VTE did not receive the thromboprophylaxis necessary [95, 118]. And this is despite the fact that LMWH long-term use appears well tolerated and may, in some instances, positively influence overall response to therapy [119]. Palliative care patients might be preferring LMWH injections over warfarin or compression stockings, but physicians’ preferences also seem to have an important influence on the respective decisions [120,121,122,123,124].
The exact rate of VTE or arterial thromboses [125] with the use of thalidomide and its analogues probably depends on the therapeutic regimens chosen (especially in combination with dexamethasone, see above) and therefore still remains some matter of debate [33, 126], but the frequency of VTE is high enough to suggest that pharmacological thromboprophylaxis, probably preferably with low-molecular-weight heparin, should be used [127, 128].
Pneumatic compression stockings seem to work well for thromboprophylaxis in cancer patients, but randomized controlled studies on their use, specifically in comparison to other pharmacological antithrombotic therapies, are rare [117, 129,130,131].
At the time being, there is still no unequivocal evidence that antithrombotic prophylaxis will prevent catheter-associated thrombosis in cancer patients, but available data strongly suggest a rational for the use of antithrombotics [106, 132, 133].
The potential use of direct oral anticoagulants (DOACs , also still referred to as NOAC for “new oral anticoagulants” or “non-VKA oral anticoagulants”) in cancer patients is of utmost interest and seems in a transition phase at the time being. The phase III studies for VTE therapy and secondary prophylaxis for dabigatran, rivaroxaban, apixaban, and edoxaban all included patients with VTEs that were later on found to be related to a malignancy. Such patients within these trials (subgroup analyses) as well as “real-world patients” (cohort studies) were separately evaluated; no sign was found that the use of DOACs showed evidence for decreased efficacy or increased toxicity as compared to non-DOAC, standard anticoagulant therapy in the setting of cancer-associated thomboembolism [134,135,136,137,138,139,140,141,142]. However, as patients with active cancer were excluded from the respective phase III studies, a formal evaluation of the use of DOACs in cancer patients is needed [143]. Such studies are underway. Meanwhile, in VTE found to be cancer associated, our approach is to continue DOACs in patients that were started on it if therapy has been effective and well tolerated. If a malignacy is already known when VTE occurs, we currently still suggest to start therapy with LMWH according to the current guidelines. But as mentioned before, a transition phase is taking place. Should the formal studies confirm the positive initial clinical experience with DOACs in cancer patients, these substances will be an important addition to the current selection of antithrombotic therapies in patients with cancer. Specifically, these substances will likely reduce the need for the subcutaneous application of antithrombotics in many, if not most, cancer patients and thus also increase their quality of life.
Despite being frequently used, aspirin cannot be generally considered as an adequate prophylaxis for primary or secondary prophylaxis of venous thromboembolism in cancer patients [144]. However, in situations where plasmatic antithrombotics are contraindicated and aspirin is not, its use might be considered rather than completely withholding antithrombotic therapy [115].
In hypercoagulable states due to acquired anticoagulant deficiency such as antithrombin deficiency with asparaginase therapy, replacement therapy should be taken into consideration although randomized controlled trials are needed to clarify this question [145, 146].
In patients with hyperviscosity due to paraproteins [37, 80], plasma exchange or plasmapheresis might be the most appropriate way to treat, at least for the short-term benefit. High protein concentrations, however, tend to “rebound” due to the high protein concentrations present in the extravascular space (especially with IgG) [147]. Other reasons for hyperviscosity in cancer patients might exist and thus necessitate different and/or continued therapeutic prophylactic approaches [41]. Recently, this was recognized specifically for JAK-2-positive hematological diseases [148, 149].
Vena cava filters might be an option for the prevention of thromboembolism in patients with manifest thrombosis or very high risk for thromboembolism and bleeding risk with antithrombotic therapy (such as chemotherapy-induced thrombocytopenia) or contraindication to anticoagulation [115], but the consideration itself is a sign of poor prognosis [150]. CVC filters may be associated with device-related thromboembolic complications in nearly 10% of patients [151]; however, in the absence of randomized trials, results from different reports are difficult to compare as survival times of the patients might greatly differ [152]. From a hemostaseological point of view, IVC filters are almost never needed and frequently create more problems than they solve [153].
Pathogenesis of Bleeding
Besides thromboembolic events, cancer patients show also evidence of a bleeding tendency. This can be related to various, seemingly separate pathologies; however, recent research suggests that bleeding might occur, in fact, as the result of an interplay of various different pathologies [154,155,156].
Thrombocytopenia
Drug-induced thrombocytopenia is a frequent finding in cancer patients undergoing chemotherapy [157]. It is common knowledge that thrombocytopenia increases the risk of bleeding, both in cancer and non-cancer patients [158]. In thrombocytopenic patients, additional risk factors for bleeding are infection, antithrombotic therapy, signs of renal dysfunction, and anemia [159]. In acute leukemia, the degree of thrombocytopenia correlates well with the risk and degree of bleeding. Fever and infection not only increase the bleeding risk but also reduce the response to platelet transfusion [160]. There is some well-based evidence that platelet substitution in AML induction chemotherapy can be lowered to trigger levels of 10 or 20 G/l [161]; the same group performed a randomized clinical trial indicating that a non-prophylactic approach outside induction or reinduction therapy for acute leukemia might be reasonable if the staff involved is sufficiently experienced [162].
Although bleeding does occur during treatment for solid cancers such as lung cancer, it seems that thrombocytopenic bleeding in solid cancer patients is rather rare [163]. Defining the exact need for platelet transfusion seems relevant as treating patients in this setting consumes considerable resources, with approximately half of the therapy courses inducing the additional financial burden [164]. It is important to preemptively consider the need for platelet support in advanced cancer patients on a case-by-case basis; this should allow to provide the therapy necessary and, at the same time, to reduce the strain on the resources available [165, 166].
Platelet Dysfunction
The potential reasons for platelet dysfunction are manifold; most frequently, platelet dysfunction is drug induced [167], including anticancer drugs such as tyrosine kinase inhibitors [168]. Unexplained GI bleeding is frequently associated with nonsteroidal anti-inflammatory drugs (NSAIDs) or anticoagulants [169]; NSAIDs impair mucosal healing or directly induce mucosal toxicity, both properties that will increase the risk for bleeding, e.g., in the gastrointestinal tract [170]. In that respect, COX-2 inhibition could be an attractive target in cancer patients with pain [171]; however, as COX-2 inhibitors may be associated with increased cardiovascular risk [172], the decision to use them should be carefully evaluated and be taken on a case-by-case basis.
Tumor Infiltration
Bleeding in cancer patients might be due to direct infiltration of the respective vessel, as it can be encountered, for example, in gastric lymphoma; here, therapy has shifted away from primary surgery. But if bleeding occurs, early surgical intervention needs to be considered [173]. Radiation therapy might be an appropriate approach to control bleeding that comes from direct tumor infiltration [174]; rarely, however, radiotherapy can aggravate or induce bleeding in sensitive tumors, especially when applied in combination with chemotherapy [175].
Fibrinolysis
Many malignancies might be associated with an increased fibrinolytic activity [8, 176]. Along with elevated levels of plasminogen activators in many hematological malignancies, excessive fibrinolysis can increase the risk of bleeding [177]. In DIC (with increased fibrinolysis), the extent of bleeding correlates with fibrinolytic activity [178], as is probably the case in acute promyelocytic leukemia [71]. The increased fibrinolytic response in APL might have to do with the increased expression of uPA [179] and Annexin II [180], a receptor for tPA and plasminogen. Annexin II has been found to be highly expressed in in cerebral endothelial cells [181], which may explain why intracranial hemorrhage in APL seems frequent and provides a rational for the prophylactic use of antifibrinolytics. Annexin II might also contribute to bleeding in other acute leukemias [180]. The standard use of antifibrinolytics seems helpful to reduce bleeding and thus the use of blood products [182], but requires careful consideration of the concurrent thrombembolic risk.
Rarely, coagulation factor inhibitors are found in cancer patients; in this situation, bleeding complications can be severe [183] (see also “Paraproteins” below).
Perioperative Bleeding Problems in Cancer Patients
Perioperative coagulopathies continue to be a diagnostic and therapeutic dilemma, especially in cancer patients. The pathophysiology behind unexplained intraoperative coagulopathies is of great variety and complexity as all aforementioned mechanisms can occur [154, 184,185,186,187]. If the pathophysiology is known, therapy should be directed accordingly. We showed in prospective studies that patients with “unexplained” intraoperative coagulopathy have significantly less factor XIII per unit thrombin available at any point in time [188], resulting in the loss of clot firmness and increased intraoperative blood loss. These patients have less cross-linking capacity to begin with, explaining their preoperatively increased fibrin monomer concentration, which can be used for preemptive risk stratification [189]. Importantly, the relative (compared to the amount of thrombin generated) acquired FXIII deficiency shows clinical relevance with surgical stress even if deficiency is moderate, which differs from the experiences in patients with inborn FXIII deficiency. There is proof of principle that the use of FXIII in high-risk patients (high preoperative fibrin monomer) leads to maintenance (vs. loss) of clot firmness and significant reduction in blood loss [190].
Adverse Effects of Therapies
Drugs used for oncologic therapies frequently induce myelosuppression , which can cause thrombocytopenia and thus induce bleeding [191]. In addition, other mechanisms might include direct or indirect influences on platelets (such as tyrosine kinase inhibition [168], see above) and coagulation factors: L-asparaginase, used for the treatment of acute lymphocytic leukemia, induces a depletion in L-asparagine, leading to an impaired protein synthesis that also extends to procoagulants, anticoagulants, and fibrinolytic proteins. The lowering of various procoagulants induces a transient hypocoagulable state that is at least partially balanced due to the parallel decrease of anticoagulants [96, 192]; however, replacement of coagulation factors in high-risk situations might be appropriate and needs to be decided on a case-by-case basis.
Paraproteins
High levels of paraproteins can interfere with hemostasis in various ways: they can inhibit polymerization of fibrin monomers, interfere with platelet aggregation, or inhibit clotting factor activity [193, 194]. As already described for hyperviscosity, bleeding problems in such patients might improve with plasmapheresis (but also might rebound with redistribution). Although this can be a clinically important in single patients, it is a rare problem.
Conclusions
Hypercoagulability in cancer patients not only is an attendant phenomenon but in fact is part of the problem. Therefore, the stringent evaluation of the need for thromboprophylaxis or continued use of anticoagulant therapy in every cancer patient is a must, especially as recent data suggest that the use of low-molecular-weight heparin might improve clinical outcome, whereas at the same time, not all patients in need of thromboprophylaxis will receive it.
On the other hand, our knowledge of the use of blood products in cancer patients has evolved (e.g., platelet transfusion in leukemia patients) and should thus allow us to make better use of the available resources, avoiding unnecessary burden and risk to the patient and economic strain to the healthcare system.
Studies in recent years have advanced our understanding of thromboembolism and bleeding complications in cancer patients. The next important step to come will be to define the adequate use of direct (or “novel”) oral anticoagulants in cancer patients. Other issues such as specific problems and therapies with disease-specific approaches (e.g., JAK-2-positive diseases) are on the horizon, indicating that we will need to continue prospective controlled trials to generate further evidence-based knowledge.
References
Virchow R. Phlogose und Thrombose im Gefässsystem. In: Müller C, editor. Gesammelte Abhandlungen zur Wissenschaftlichen Medicin. Zweite unveränderte Auflage ed. Hamm: G. Grot'sche Buchhandlung; 1862. p. 458–732.
Trousseau A. Phlegmasia alba dolens. Clinique medicale de l'Hotel-Dien de Paris 1865;3.
Schaffner F, Ruf W. Tissue factor and PAR2 signaling in the tumor microenvironment. Arterioscler Thromb Vasc Biol. 2009;29(12):1999–2004.
Lussana F, Caberlon S, Pagani C, Kamphuisen PW, Buller HR, Cattaneo M. Association of V617F Jak2 mutation with the risk of thrombosis among patients with essential thrombocythaemia or idiopathic myelofibrosis: a systematic review. Thromb Res. 2009;124(4):409–17.
Sozer S, Fiel MI, Schiano T, Xu M, Mascarenhas J, Hoffman R. The presence of JAK2V617F mutation in the liver endothelial cells of patients with Budd-Chiari syndrome. Blood. 2009;113(21):5246–9.
Donnellan E, Kevane B, Bird BR, Ainle FN. Cancer and venous thromboembolic disease: from molecular mechanisms to clinical management. Curr Oncol. 2014;21(3):134–43.
Hreinsson JP, Jonasson JG, Bjornsson ES. Bleeding-related symptoms in colorectal cancer: a 4-year nationwide population-based study. Aliment Pharmacol Ther. 2014;39(1):77–84.
Palma Anselmo M, Nobre de Jesus G, Lopes JM, Victorino RM, Meneses Santos J. Massive bleeding as the first clinical manifestation of metastatic prostate cancer due to disseminated intravascular coagulation with enhanced fibrinolysis. Case Reports Hematol. 2016;2016:7217915.
Korte W. Changes of the coagulation and fibrinolysis system in malignancy: their possible impact on future diagnostic and therapeutic procedures. Clin Chem Lab Med. 2000;38(8):679–92.
Ay C, Pabinger I. Predictive potential of haemostatic biomarkers for venous thromboembolism in cancer patients. Thromb Res. 2012;129(Suppl 1):S6–9.
Riedl J, Kaider A, Marosi C, Prager GW, Eichelberger B, Assinger A, et al. Decreased platelet reactivity in patients with cancer is associated with high risk of venous thromboembolism and poor prognosis. Thromb Haemost. 2016;20:117(1).
Ay C, Simanek R, Vormittag R, Dunkler D, Alguel G, Koder S, et al. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: results from the Vienna Cancer and Thrombosis Study (CATS). Blood. 2008;112(7):2703–8.
Ay C, Vormittag R, Dunkler D, Simanek R, Chiriac AL, Drach J, et al. D-dimer and prothrombin fragment 1 + 2 predict venous thromboembolism in patients with cancer: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol. 2009;27(25):4124–9.
Seitz R, Rappe N, Kraus M, Immel A, Wolf M, Maasberg M, et al. Activation of coagulation and fibrinolysis in patients with lung cancer: relation to tumour stage and prognosis. Blood Coagul Fibrinolysis. 1993;4(2):249–54.
Antoniou D, Pavlakou G, Stathopoulos GP, Karydis I, Chondrou E, Papageorgiou C, et al. Predictive value of D-dimer plasma levels in response and progressive disease in patients with lung cancer. Lung Cancer. 2006;53(2):205–10.
Reitter EM, Kaider A, Ay C, Quehenberger P, Marosi C, Zielinski C, et al. Longitudinal analysis of hemostasis biomarkers in cancer patients during antitumor treatment. J Thromb Haemost. 2016;14(2):294–305.
Kanda M, Tanaka C, Kobayashi D, Mizuno A, Tanaka Y, Takami H, et al. Proposal of the coagulation score as a predictor for short-term and long-term outcomes of patients with Resectable gastric cancer. Ann Surg Oncol. 2017;24(2):502–9.
de Haas EC, Zwart N, Meijer C, Suurmeijer AJ, Meijer K, Guchelaar HJ, et al. Association of PAI-1 gene polymorphism with survival and chemotherapy-related vascular toxicity in testicular cancer. Cancer. 2010;116(24):5628–36.
Tinholt M, Vollan HK, Sahlberg KK, Jernstrom S, Kaveh F, Lingjaerde OC, et al. Tumor expression, plasma levels and genetic polymorphisms of the coagulation inhibitor TFPI are associated with clinicopathological parameters and survival in breast cancer, in contrast to the coagulation initiator TF. Breast Cancer Res. 2015;17:44.
Wada H, Mori Y, Okabayashi K, Gabazza EC, Kushiya F, Watanabe M, et al. High plasma fibrinogen level is associated with poor clinical outcome in DIC patients. Am J Hematol. 2003;72(1):1–7.
Riedl J, Hell L, Kaider A, Koder S, Marosi C, Zielinski C, et al. Association of platelet activation markers with cancer-associated venous thromboembolism. Platelets. 2016;27(1):80–5.
Pabinger I, Thaler J, Ay C. Biomarkers for prediction of venous thromboembolism in cancer. Blood. 2013;122(12):2011–8.
Rickles FR, Levine MN. Epidemiology of thrombosis in cancer. Acta Haematol. 2001;106(1–2):6–12.
Veress B, Alafuzoff I. A retrospective analysis of clinical diagnoses and autopsy findings in 3,042 cases during two different time periods. Hum Pathol. 1994;25(2):140–5.
Ogren M, Bergqvist D, Wahlander K, Eriksson H, Sternby NH. Trousseau's syndrome - what is the evidence? A population-based autopsy study. Thromb Haemost. 2006;95(3):541–5.
White RH, Chew HK, Zhou H, Parikh-Patel A, Harris D, Harvey D, et al. Incidence of venous thromboembolism in the year before the diagnosis of cancer in 528,693 adults. Arch Int Med. 2005;165(15):1782–7.
Murchison JT, Wylie L, Stockton DL. Excess risk of cancer in patients with primary venous thromboembolism: a national, population-based cohort study. Br J Cancer. 2004;91(1):92–5.
Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293(6):715–22.
Jimenez-Zepeda VH, Dominguez-Martinez VJ. Acquired activated protein C resistance and thrombosis in multiple myeloma patients. Thromb J. 2006;4:11.
Tsai J, Abe K, Boulet SL, Beckman MG, Hooper WC, Grant AM. Predictive accuracy of 29-comorbidity index for in-hospital deaths in US adult hospitalizations with a diagnosis of venous thromboembolism. PLoS One. 2013;8(7):e70061.
Khorana AA, Francis CW, Culakova E, Fisher RI, Kuderer NM, Lyman GH. Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol. 2006;24(3):484–90.
Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007;110(10):2339–46.
Musallam KM, Dahdaleh FS, Shamseddine AI, Taher AT. Incidence and prophylaxis of venous thromboembolic events in multiple myeloma patients receiving immunomodulatory therapy. Thromb Res. 2009;123(5):679–86.
Otten HM, Mathijssen J, ten Cate H, Soesan M, Inghels M, Richel DJ, et al. Symptomatic venous thromboembolism in cancer patients treated with chemotherapy: an underestimated phenomenon. Arch Intern Med. 2004;164(2):190–4.
Chew HK, Wun T, Harvey DJ, Zhou H, White RH. Incidence of venous thromboembolism and the impact on survival in breast cancer patients. J Clin Oncol. 2007;25(1):70–6.
von Tempelhoff GF, Heilmann L, Hommel G, Pollow K. Impact of rheological variables in cancer. Semin Thromb Hemost. 2003;29(5):499–513.
Mehta J, Singhal S. Hyperviscosity syndrome in plasma cell dyscrasias. Semin Thromb Hemost. 2003;29(5):467–71.
Linenberger ML, Wittkowsky AK. Thromboembolic complications of malignancy. Part 1: risks. Oncology. 2005;19(7):853–61.
Zgouras D, Engels K, Lindhoff-Last E. Lymphoplasmacytic lymphoma with Waldenstrom's macroglobulinemia as a reason for peripheral arterial perfusion disorders. Vasa. 2009;38(2):193–6.
Michaud M, Moulis G, Puissant B, Cougoul P, Sailler L. Cryofibrinogenemia and risk of cancer in cryoglobulinemic patients without vasculitis criteria. Eur J Intern Med. 2016;28:e10–2.
von Tempelhoff GF, Heilmann L, Hommel G, Schneider D, Niemann F, Zoller H. Hyperviscosity syndrome in patients with ovarian carcinoma. Cancer. 1998;82(6):1104–11.
Sharma K, Puniyani RR, Bhat SV, Advani SH, Hegde U, Rao S. Blood viscosity parameter correlation with types of leukemia. Physiol Chem Phys Med NMR. 1992;24(2):159–64.
Finazzi G. A prospective analysis of thrombotic events in the European collaboration study on low-dose aspirin in polycythemia (ECLAP). Pathol Biol. 2004;52(5):285–8.
Landolfi R, Ciabattoni G, Patrignani P, Castellana MA, Pogliani E, Bizzi B, et al. Increased thromboxane biosynthesis in patients with polycythemia vera: evidence for aspirin-suppressible platelet activation in vivo. Blood. 1992;80(8):1965–71.
De Stefano V, Za T, Rossi E, Fiorini A, Ciminello A, Luzzi C, et al. Influence of the JAK2 V617F mutation and inherited thrombophilia on the thrombotic risk among patients with essential thrombocythemia. Haematologica. 2009;94(5):733–7.
Borowczyk M, Wojtaszewska M, Lewandowski K, Gil L, Lewandowska M, Lehmann-Kopydlowska A, et al. The JAK2 V617F mutational status and allele burden may be related with the risk of venous thromboembolic events in patients with Philadelphia-negative myeloproliferative neoplasms. Thromb Res. 2015;135(2):272–80.
Arellano-Rodrigo E, Alvarez-Larran A, Reverter JC, Colomer D, Villamor N, Bellosillo B, et al. Platelet turnover, coagulation factors, and soluble markers of platelet and endothelial activation in essential thrombocythemia: relationship with thrombosis occurrence and JAK2 V617F allele burden. Am J Hematol. 2009;84(2):102–8.
Ventura GJ, Hester JP, Smith TL, Keating MJ. Acute myeloblastic leukemia with hyperleukocytosis: risk factors for early mortality in induction. Am J Hematol. 1988;27(1):34–7.
Ostergren J, Fagrell B, Bjorkholm M. Hyperleukocytic effects on skin capillary circulation in patients with leukaemia. J Intern Med. 1992;231(1):19–23.
Khorana AA, Francis CW, Culakova E, Lyman GH. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer. 2005;104(12):2822–9.
Simanek R, Vormittag R, Ay C, Alguel G, Dunkler D, Schwarzinger I, et al. High platelet count associated with venous thromboembolism in cancer patients: results from the Vienna Cancer and Thrombosis Study (CATS). J Thromb Haemost. 2010;8(1):114–20.
Riedl J, Kaider A, Reitter EM, Marosi C, Jager U, Schwarzinger I, et al. Association of mean platelet volume with risk of venous thromboembolism and mortality in patients with cancer. Results from the Vienna Cancer and Thrombosis Study (CATS). Thromb Haemost. 2014;111(4):670–8.
Otten TR, Stein PD, Patel KC, Mustafa S, Silbergleit A. Thromboembolic disease involving the superior vena cava and brachiocephalic veins. Chest. 2003;123(3):809–12.
Hiraiwa K, Morozumi K, Miyazaki H, Sotome K, Furukawa A, Nakamaru M, et al. Isolated splenic vein thrombosis secondary to splenic metastasis: a case report. World J Gastroenterol. 2006;12(40):6561–3.
Bergqvist D. Venous thromboembolism: a review of risk and prevention in colorectal surgery patients. Dis Colon Rectum. 2006;49(10):1620–8.
Fernandez PM, Patierno SR, Rickles FR. Tissue factor and fibrin in tumor angiogenesis. Semin Thromb Hemost. 2004;30(1):31–44.
Sakuma M, Fukui S, Nakamura M, Takahashi T, Kitamukai O, Yazu T, et al. Cancer and pulmonary embolism: thrombotic embolism, tumor embolism, and tumor invasion into a large vein. Circ J. 2006;70(6):744–9.
Le Treut YP, Hardwigsen J, Ananian P, Saisse J, Gregoire E, Richa H, et al. Resection of hepatocellular carcinoma with tumor thrombus in the major vasculature. A European case-control series. J Gastrointest Surg. 2006;10(6):855–62.
Chen XP, Qiu FZ, Wu ZD, Zhang ZW, Huang ZY, Chen YF, et al. Effects of location and extension of portal vein tumor thrombus on long-term outcomes of surgical treatment for hepatocellular carcinoma. Ann Surg Oncol. 2006;13(7):940–6.
Rickles FR, Falanga A. Molecular basis for the relationship between thrombosis and cancer. Thromb Res. 2001;102(6):V215–24.
Reitter EM, Ay C, Kaider A, Pirker R, Zielinski C, Zlabinger G, et al. Interleukin levels and their potential association with venous thromboembolism and survival in cancer patients. Clin Exp Immunol. 2014;177(1):253–60.
Franco AT, Corken A, Ware J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood. 2015;126(5):582–8.
Marchetti M, Vignoli A, Russo L, Balducci D, Pagnoncelli M, Barbui T, et al. Endothelial capillary tube formation and cell proliferation induced by tumor cells are affected by low molecular weight heparins and unfractionated heparin. Thromb Res. 2008;121(5):637–45.
Leone G, Sica S, Chiusolo P, Teofili L, De Stefano V. Blood cells diseases and thrombosis. Haematologica. 2001;86(12):1236–44.
de Gaetano G, Cerletti C, Evangelista V. Recent advances in platelet-polymorphonuclear leukocyte interaction. Haemostasis. 1999;29(1):41–9.
Demers M, Krause DS, Schatzberg D, Martinod K, Voorhees JR, Fuchs TA, et al. Cancers predispose neutrophils to release extracellular DNA traps that contribute to cancer-associated thrombosis. Proc Natl Acad Sci U S A. 2012;109(32):13076–81.
Connolly GC, Khorana AA, Kuderer NM, Culakova E, Francis CW, Lyman GH. Leukocytosis, thrombosis and early mortality in cancer patients initiating chemotherapy. Thromb Res. 2010;126(2):113–8.
Thaler J, Koder S, Kornek G, Pabinger I, Ay C. Microparticle-associated tissue factor activity in patients with metastatic pancreatic cancer and its effect on fibrin clot formation. Transl Res. 2014;163(2):145–50.
Kamikura Y, Wada H, Nobori T, Kobayashi T, Sase T, Nishikawa M, et al. Elevated levels of leukocyte tissue factor mRNA in patients with venous thromboembolism. Thromb Res. 2005;116(4):307–12.
Sase T, Wada H, Yamaguchi M, Ogawa S, Kamikura Y, Nishikawa M, et al. Haemostatic abnormalities and thrombotic disorders in malignant lymphoma. Thromb Haemost. 2005;93(1):153–9.
Stein E, McMahon B, Kwaan H, Altman JK, Frankfurt O, Tallman MS. The coagulopathy of acute promyelocytic leukaemia revisited. Best Pract Res. 2009;22(1):153–63.
Lisman T, de Groot PG, Meijers JC, Rosendaal FR. Reduced plasma fibrinolytic potential is a risk factor for venous thrombosis. Blood. 2005;105(3):1102–5.
Wang J, Weiss I, Svoboda K, Kwaan HC. Thrombogenic role of cells undergoing apoptosis. Br J Haematol. 2001;115(2):382–91.
Date K, Hall J, Greenman J, Maraveyas A, Madden LA. Tumour and microparticle tissue factor expression and cancer thrombosis. Thromb Res. 2013;131(2):109–15.
Davila M, Amirkhosravi A, Coll E, Desai H, Robles L, Colon J, et al. Tissue factor-bearing microparticles derived from tumor cells: impact on coagulation activation. J Thromb Haemost. 2008;6(9):1517–24.
Lechner D, Kollars M, Gleiss A, Kyrle PA, Weltermann A. Chemotherapy-induced thrombin generation via procoagulant endothelial microparticles is independent of tissue factor activity. J Thromb Haemost. 2007;5(12):2445–52.
Nijziel MR, van Oerle R, Christella M, Thomassen LG, van Pampus EC, Hamulyak K, et al. Acquired resistance to activated protein C in breast cancer patients. Br J Haematol. 2003;120(1):117–22.
De Lucia D, De Vita F, Orditura M, Renis V, Belli A, Conte M, et al. Hypercoagulable state in patients with advanced gastrointestinal cancer: evidence for an acquired resistance to activated protein C. Tumori. 1997;83(6):948–52.
Elice F, Fink L, Tricot G, Barlogie B, Zangari M. Acquired resistance to activated protein C (aAPCR) in multiple myeloma is a transitory abnormality associated with an increased risk of venous thromboembolism. Br J Haematol. 2006;134(4):399–405.
Zangari M, Berno T, Zhan F, Tricot G, Fink L. Mechanisms of thrombosis in paraproteinemias: the effects of immunomodulatory drugs. Semin Thromb Hemost. 2012;38(8):768–79.
Pusterla S, Previtali S, Marziali S, Cortelazzo S, Rossi A, Barbui T, et al. Antiphospholipid antibodies in lymphoma: prevalence and clinical significance. Hematol J. 2004;5(4):341–6.
Genvresse I, Luftner D, Spath-Schwalbe E, Buttgereit F. Prevalence and clinical significance of anticardiolipin and anti-beta2-glycoprotein-I antibodies in patients with non-Hodgkin’s lymphoma. Eur J Haematol. 2002;68(2):84–90.
Horowitz N, Brenner B. Thrombophilia and cancer. Pathophysiol Haemost Thromb. 2008;36(3–4):131–6.
Salluh JI, Soares M, De Meis E. Antiphospholipid antibodies and multiple organ failure in critically ill cancer patients. Clinics (Sao Paulo). 2009;64(2):79–82.
Font C, Vidal L, Espinosa G, Tassies D, Monteagudo J, Farrus B, et al. Solid cancer, antiphospholipid antibodies, and venous thromboembolism. Autoimmun Rev. 2011;10(4):222–7.
Bazzan M, Montaruli B, Vaccarino A, Fornari G, Saitta M, Prandoni P. Presence of low titre of antiphospholipid antibodies in cancer patients: a prospective study. Intern Emerg Med. 2009;4(6):491–5.
Gomez-Puerta JA, Cervera R, Espinosa G, Aguilo S, Bucciarelli S, Ramos-Casals M, et al. Antiphospholipid antibodies associated with malignancies: clinical and pathological characteristics of 120 patients. Semin Arthritis Rheum. 2006;35(5):322–32.
Decousus H, Moulin N, Quenet S, Bost V, Rivron-Guillot K, Laporte S, et al. Thrombophilia and risk of venous thrombosis in patients with cancer. Thromb Res. 2007;120(Suppl 2):S51–61.
Pabinger I, Ay C, Dunkler D, Thaler J, Reitter EM, Marosi C, et al. Factor V Leiden mutation increases the risk for venous thromboembolism in cancer patients - results from the Vienna Cancer And Thrombosis Study (CATS). J Thromb Haemost. 2015;13(1):17–22.
Abramson N, Costantino JP, Garber JE, Berliner N, Wickerham DL, Wolmark N. Effect of Factor V Leiden and prothrombin G20210–>A mutations on thromboembolic risk in the national surgical adjuvant breast and bowel project breast cancer prevention trial. J Natl Cancer Inst. 2006;98(13):904–10.
Wahba MA, Ismail MA, Saad AA, Habashy DM, Hafeez ZM, Boshnak NH. Impact of thrombophilic genes mutations on thrombosis risk in Egyptian nonmetastatic cancer patients. Blood Coagul Fibrinolysis. 2015;26(3):309–15.
Eroglu A, Ulu A, Cam R, Kurtman C, Akar N. Prevalence of factor V 1691 G-A (Leiden) and prothrombin G20210A polymorphisms and the risk of venous thrombosis among cancer patients. J Thromb Thrombolysis. 2007;23(1):31–4.
Lechner D, Weltermann A. Chemotherapy-induced thrombosis: a role for microparticles and tissue factor? Semin Thromb Hemost. 2008;34(2):199–203.
Samare Fekri M, Khalily Zade M, Fatehi S. The association of deep vein thrombosis with cancer treatment modality: chemotherapy or surgery? Iran Red Crescent Med J. 2014;16(9):e14722.
Kucher N, Spirk D, Baumgartner I, Mazzolai L, Korte W, Nobel D, et al. Lack of prophylaxis before the onset of acute venous thromboembolism among hospitalized cancer patients: the SWIss Venous ThromboEmbolism Registry (SWIVTER). Ann Oncol. 2010;21(5):931–5.
Mitchell LG, Sutor AH, Andrew M. Hemostasis in childhood acute lymphoblastic leukemia: coagulopathy induced by disease and treatment. Semin Thromb Hemost. 1995;21(4):390–401.
Jorgensen KA, Sorensen P, Freund L. Effect of glucocorticosteroids on some coagulation tests. Acta Haematol. 1982;68(1):39–42.
Singhal S, Mehta J. Thalidomide in cancer. Biomed Pharmacother. 2002;56(1):4–12.
Zangari M, Siegel E, Barlogie B, Anaissie E, Saghafifar F, Fassas A, et al. Thrombogenic activity of doxorubicin in myeloma patients receiving thalidomide: implications for therapy. Blood. 2002;100(4):1168–71.
Gieseler F. Pathophysiological considerations to thrombophilia in the treatment of multiple myeloma with thalidomide and derivatives. Thromb Haemost. 2008;99(6):1001–7.
Klein U, Kosely F, Hillengass J, Hundemer M, Schmitt S, Neben K, et al. Effective prophylaxis of thromboembolic complications with low molecular weight heparin in relapsed multiple myeloma patients treated with lenalidomide and dexamethasone. Ann Hematol. 2009;88(1):67–71.
Agnelli G, Verso M. Therapy insight: venous-catheter-related thrombosis in cancer patients. Nat Clin Pract Oncol. 2006;3(4):214–22.
Dentali F, Gianni M, Agnelli G, Ageno W. Association between inherited thrombophilic abnormalities and central venous catheter thrombosis in patients with cancer: a meta-analysis. J Thromb Haemost. 2008;6(1):70–5.
Refaei M, Fernandes B, Brandwein J, Goodyear MD, Pokhrel A, Wu C. Incidence of catheter-related thrombosis in acute leukemia patients: a comparative, retrospective study of the safety of peripherally inserted vs. centrally inserted central venous catheters. Ann Hematol. 2016;95(12):2057–64.
Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003;21(19):3665–75.
Debourdeau P, Farge D, Beckers M, Baglin C, Bauersachs RM, Brenner B, et al. International clinical practice guidelines for the treatment and prophylaxis of thrombosis associated with central venous catheters in patients with cancer. J Thromb Haemost. 2013;11(1):71–80.
Gaitini D, Beck-Razi N, Haim N, Brenner B. Prevalence of upper extremity deep venous thrombosis diagnosed by color Doppler duplex sonography in cancer patients with central venous catheters. J Ultrasound Med. 2006;25(10):1297–303.
Lee AY, Levine MN, Butler G, Webb C, Costantini L, Gu C, et al. Incidence, risk factors, and outcomes of catheter-related thrombosis in adult patients with cancer. J Clin Oncol. 2006;24(9):1404–8.
Monreal M, Munoz FJ, Rosa V, Romero C, Roman P, Di Micco P, et al. Upper extremity DVT in oncological patients: analysis of risk factors. Data from the RIETE registry. Exp Oncol. 2006;28(3):245–7.
Tyritzis SI, Wallerstedt A, Steineck G, Nyberg T, Hugosson J, Bjartell A, et al. Thromboembolic complications in 3,544 patients undergoing radical prostatectomy with or without lymph node dissection. J Urol. 2015;193(1):117–25.
Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146–53.
Lee AY, Kamphuisen PW, Meyer G, Bauersachs R, Janas MS, Jarner MF, et al. Tinzaparin vs warfarin for treatment of acute venous thromboembolism in patients with active cancer: a randomized clinical trial. JAMA. 2015;314(7):677–86.
Lyman GH, Khorana AA, Falanga A, Clarke-Pearson D, Flowers C, Jahanzeb M, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25(34):5490–505.
Debourdeau P, Elalamy I, de Raignac A, Meria P, Gornet JM, Amah Y, et al. Long-term use of daily subcutaneous low molecular weight heparin in cancer patients with venous thromboembolism: why hesitate any longer? Support Care Cancer. 2008;16(12):1333–41.
Farge D, Debourdeau P, Beckers M, Baglin C, Bauersachs RM, Brenner B, et al. International clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. J Thromb Haemost. 2013;11(1):56–70.
Mandala M, Falanga A, Piccioli A, Prandoni P, Pogliani EM, Labianca R, et al. Venous thromboembolism and cancer: guidelines of the Italian Association of Medical Oncology (AIOM). Crit Rev Oncol Hematol. 2006;59(3):194–204.
Martino MA, Williamson E, Rajaram L, Lancaster JM, Hoffman MS, Maxwell GL, et al. Defining practice patterns in gynecologic oncology to prevent pulmonary embolism and deep venous thrombosis. Gynecol Oncol. 2007;106(3):439–45.
Farge-Bancel D, Bounameaux H, Brenner B, Buller HR, Kakkar A, Pabinger I, et al. Implementing thrombosis guidelines in cancer patients: a review. Rambam Maimonides Med J. 2014;5(4):e0041.
Lee AY, Rickles FR, Julian JA, Gent M, Baker RI, Bowden C, et al. Randomized comparison of low molecular weight heparin and coumarin derivatives on the survival of patients with cancer and venous thromboembolism. J Clin Oncol. 2005;23(10):2123–9.
Noble SI, Nelson A, Turner C, Finlay IG. Acceptability of low molecular weight heparin thromboprophylaxis for inpatients receiving palliative care: qualitative study. BMJ. 2006;332(7541):577–80.
Seaman S, Nelson A, Noble S. Cancer-associated thrombosis, low-molecular-weight heparin, and the patient experience: a qualitative study. Patient Prefer Adherence. 2014;8:453–61.
Sheard L, Prout H, Dowding D, Noble S, Watt I, Maraveyas A, et al. The ethical decisions UK doctors make regarding advanced cancer patients at the end of life—the perceived (in) appropriateness of anticoagulation for venous thromboembolism: a qualitative study. BMC Med Ethics. 2012;13:22.
Johnson MJ, Sheard L, Maraveyas A, Noble S, Prout H, Watt I, et al. Diagnosis and management of people with venous thromboembolism and advanced cancer: how do doctors decide? A qualitative study. BMC Med Inform Decis Mak. 2012;12:75.
Gartner V, Kierner KA, Namjesky A, Kum-Taucher B, Hammerl-Ferrari B, Watzke HH, et al. Thromboprophylaxis in patients receiving inpatient palliative care: a survey of present practice in Austria. Support Care Cancer. 2012;20(9):2183–7.
Martin MG, Vij R. Arterial thrombosis with immunomodulatory derivatives in the treatment of multiple myeloma: a single-center case series and review of the literature. Clin Lymphoma Myeloma. 2009;9(4):320–3.
Rajkumar SV, Blood E. Lenalidomide and venous thrombosis in multiple myeloma. N Engl J Med. 2006;354(19):2079–80.
Zangari M, Elice F, Fink L, Tricot G. Thrombosis in multiple myeloma. Expert Rev Anticancer Ther. 2007;7(3):307–15.
Zamagni E, Brioli A, Tacchetti P, Zannetti B, Pantani L, Cavo M. Multiple myeloma, venous thromboembolism, and treatment-related risk of thrombosis. Semin Thromb Hemost. 2011;37(3):209–19.
Maxwell GL, Synan I, Dodge R, Carroll B, Clarke-Pearson DL. Pneumatic compression versus low molecular weight heparin in gynecologic oncology surgery: a randomized trial. Obstet Gynecol. 2001;98(6):989–95.
Patiar S, Kirwan CC, McDowell G, Bundred NJ, McCollum CN, Byrne GJ. Prevention of venous thromboembolism in surgical patients with breast cancer. Br J Surg. 2007;94(4):412–20.
Nagahiro I, Andou A, Aoe M, Sano Y, Date H, Shimizu N. Intermittent pneumatic compression is effective in preventing symptomatic pulmonary embolism after thoracic surgery. Surg Today. 2004;34(1):6–10.
Young AM, Billingham LJ, Begum G, Kerr DJ, Hughes AI, Rea DW, et al. Warfarin thromboprophylaxis in cancer patients with central venous catheters (WARP): an open-label randomised trial. Lancet. 2009;373(9663):567–74.
De Cicco M, Matovic M, Balestreri L, Steffan A, Pacenzia R, Malafronte M, et al. Early and short-term acenocumarine or dalteparin for the prevention of central vein catheter-related thrombosis in cancer patients: a randomized controlled study based on serial venographies. Ann Oncol. 2009;20(12):1936–42.
van Es N, Buller HR. Using direct oral anticoagulants (DOACs) in cancer and other high-risk populations. Hematology Am Soc Hematol Educ Program. 2015;2015:125–31.
Ross JA, Miller M, Hernandez CR. OC-13 - safe and effective use of direct oral anticoagulants (DOAC) versus conventional anticoagulation for the treatment of cancer-related venous thromboembolism. Thromb Res. 2016;140(Suppl 1):S173–4.
Vedovati MC, Germini F, Agnelli G, Becattini C. Direct oral anticoagulants in patients with VTE and cancer: a systematic review and meta-analysis. Chest. 2015;147(2):475–83.
Mancuso A, Vedovati MC, Pierpaoli L, Paliani U, Conti S, Filippucci E, et al. PO-40 - Real-life use of non-vitamin k antagonist oral anticoagulants in patients with cancer associated venous thromboembolism: data from a prospective cohort. Thromb Res. 2016;140(Suppl 1):S191.
Wells PS, Theberge IA, Bowdridge JC, Forgie MA, Carrier M. PO-41 - rivaroxaban is effective therapy for high risk cancer patients with venous thromboembolic disease. Thromb Res. 2016;140(Suppl 1):S191–2.
Mantha S, Laube E, Miao Y, Sarasohn DM, Parameswaran R, Stefanik S, et al. Safe and effective use of rivaroxaban for treatment of cancer-associated venous thromboembolic disease: a prospective cohort study. J Thromb Thrombolysis. 2017;43(2):166–71.
Agnelli G, Buller HR, Cohen A, Gallus AS, Lee TC, Pak R, et al. Oral apixaban for the treatment of venous thromboembolism in cancer patients: results from the AMPLIFY trial. J Thromb Haemost. 2015;13(12):2187–91.
Schulman S, Goldhaber SZ, Kearon C, Kakkar AK, Schellong S, Eriksson H, et al. Treatment with dabigatran or warfarin in patients with venous thromboembolism and cancer. Thromb Haemost. 2015;114(1):150–7.
Raskob GE, van Es N, Segers A, Angchaisuksiri P, Oh D, Boda Z, et al. Edoxaban for venous thromboembolism in patients with cancer: results from a non-inferiority subgroup analysis of the Hokusai-VTE randomised, double-blind, double-dummy trial. Lancet Haematol. 2016;3(8):e379–87.
Prandoni P. The treatment of cancer-associated venous thromboembolism in the era of the novel oral anticoagulants. Expert Opin Pharmacother. 2015;16(16):2391–4.
Kakkar AK, Levine M, Pinedo HM, Wolff R, Wong J. Venous thrombosis in cancer patients: insights from the FRONTLINE survey. Oncologist. 2003;8(4):381–8.
Korte W, Greiner J. PARKAA paves the way. Thromb Haemost. 2003;90(2):163–4.
Mitchell LG, Andrew M, Hanna K, Abshire T, Halton J, Anderson R, et al. A prospective cohort study determining the prevalence of thrombotic events in children with acute lymphoblastic leukemia and a central venous line who are treated with L-asparaginase: results of the Prophylactic Antithrombin Replacement in Kids with Acute Lymphoblastic Leukemia Treated with Asparaginase (PARKAA) Study. Cancer. 2003;97(2):508–16.
Nand S, Molokie R. Therapeutic plasmapheresis and protein A immunoadsorption in malignancy: a brief review. J Clin Apher. 1990;5(4):206–12.
Malecki R, Gacka M, Kuliszkiewicz-Janus M, Jakobsche-Policht U, Kwiatkowski J, Adamiec R, et al. Altered plasma fibrin clot properties in essential thrombocythemia. Platelets. 2016;27(2):110–6.
De Stefano V, Vannucchi AM, Ruggeri M, Cervantes F, Alvarez-Larran A, Iurlo A, et al. Splanchnic vein thrombosis in myeloproliferative neoplasms: risk factors for recurrences in a cohort of 181 patients. Blood Cancer J. 2016;6(11):e493.
Barginear MF, Lesser M, Akerman ML, Strakhan M, Shapira I, Bradley T, et al. Need for inferior vena cava filters in cancer patients: a surrogate marker for poor outcome. Clin Appl Thromb Hemost. 2009;15(3):263–9.
Zerati AE, Wolosker N, Yazbek G, Langer M, Nishinari K. Vena cava filters in cancer patients: experience with 50 patients. Clinics (Sao Paulo). 2005;60(5):361–6.
Usoh F, Hingorani A, Ascher E, Shiferson A, Tran V, Marks N, et al. Long-term follow-up for superior vena cava filter placement. Ann Vasc Surg. 2009;23(3):350–4.
Ingber S, Geerts WH. Vena caval filters: current knowledge, uncertainties and practical approaches. Curr Opin Hematol. 2009;16(5):402–6.
Mita K, Ito H, Murabayashi R, Sueyoshi K, Asakawa H, Nabetani M, et al. Postoperative bleeding complications after gastric cancer surgery in patients receiving anticoagulation and/or antiplatelet agents. Ann Surg Oncol. 2012;19(12):3745–52.
Cihoric N, Crowe S, Eychmuller S, Aebersold DM, Ghadjar P. Clinically significant bleeding in incurable cancer patients: effectiveness of hemostatic radiotherapy. Radiat Oncol. 2012;7:132.
Trujillo-Santos J, Nieto JA, Ruiz-Gamietea A, Lopez-Jimenez L, Garcia-Bragado F, Quintavalla R, et al. Bleeding complications associated with anticoagulant therapy in patients with cancer. Thromb Res. 2010;125(Suppl 2):S58–61.
Bodensteiner DC, Doolittle GC. Adverse haematological complications of anticancer drugs. Clinical presentation, management and avoidance. Drug Saf. 1993;8(3):213–24.
Avvisati G, Tirindelli MC, Annibali O. Thrombocytopenia and hemorrhagic risk in cancer patients. Crit Rev Oncol Hematol. 2003;48(Suppl):S13–6.
Vinholt PJ, Alnor A, Nybo M, Hvas AM. Prediction of bleeding and prophylactic platelet transfusions in cancer patients with thrombocytopenia. Platelets. 2016;27(6):547–54.
Webert K, Cook RJ, Sigouin CS, Rebulla P, Heddle NM. The risk of bleeding in thrombocytopenic patients with acute myeloid leukemia. Haematologica. 2006;91(11):1530–7.
Wandt H, Frank M, Ehninger G, Schneider C, Brack N, Daoud A, et al. Safety and cost effectiveness of a 10 × 10(9)/L trigger for prophylactic platelet transfusions compared with the traditional 20 × 10(9)/L trigger: a prospective comparative trial in 105 patients with acute myeloid leukemia. Blood. 1998;91(10):3601–6.
Wandt H, Schaefer-Eckart K, Wendelin K, Pilz B, Wilhelm M, Thalheimer M, et al. Therapeutic platelet transfusion versus routine prophylactic transfusion in patients with haematological malignancies: an open-label, multicentre, randomised study. Lancet. 2012;380(9850):1309–16.
Le Maitre A, Ding K, Shepherd FA, Leighl N, Arnold A, Seymour L. Anticoagulation and bleeding: a pooled analysis of lung cancer trials of the NCIC Clinical Trials Group. J Thorac Oncol. 2009;4(5):586–94.
Elting LS, Cantor SB, Martin CG, Hamblin L, Kurtin D, Rivera E, et al. Cost of chemotherapy-induced thrombocytopenia among patients with lymphoma or solid tumors. Cancer. 2003;97(6):1541–50.
Deichmann M, Helmke B, Bock M, Jackel A, Waldmann V, Flechtenmacher C, et al. Massive lethal cerebral bleeding in a patient with melanoma without intracranial metastasis. Clin Oncol. 1998;10(4):272–3.
Wandt H, Schafer-Eckart K, Greinacher A. Platelet transfusion in hematology, oncology and surgery. Deutsch Arztebl Int. 2014;111(48):809–15.
Koscielny J, von Tempelhoff GF, Ziemer S, Radtke H, Schmutzler M, Sinha P, et al. A practical concept for preoperative management of patients with impaired primary hemostasis. Clin Appl Thromb Hemost. 2004;10(2):155–66.
Sabrkhany S, Griffioen AW, Pineda S, Sanders L, Mattheij N, van Geffen JP, et al. Sunitinib uptake inhibits platelet function in cancer patients. Eur J Cancer. 2016;66:47–54.
Hreinsson JP, Bjarnason I, Bjornsson ES. The outcome and role of drugs in patients with unexplained gastrointestinal bleeding. Scand J Gastroenterol. 2015;50(12):1482–9.
Lehmann FS, Beglinger C. Impact of COX-2 inhibitors in common clinical practice a gastroenterologist's perspective. Curr Top Med Chem. 2005;5(5):449–64.
Lee Y, Rodriguez C, Dionne RA. The role of COX-2 in acute pain and the use of selective COX-2 inhibitors for acute pain relief. Curr Pharm Des. 2005;11(14):1737–55.
Salinas G, Rangasetty UC, Uretsky BF, Birnbaum Y. The cyclooxygenase 2 (COX-2) story: it’s time to explain, not inflame. J Cardiovasc Pharmacol Ther. 2007;12(2):98–111.
Spectre G, Libster D, Grisariu S, Da'as N, Yehuda DB, Gimmon Z, et al. Bleeding, obstruction, and perforation in a series of patients with aggressive gastric lymphoma treated with primary chemotherapy. Ann Surg Oncol. 2006;13(11):1372–8.
Kawabata H, Uno K, Yasuda K, Yamashita M. Experience of low-dose, short-course palliative radiotherapy for bleeding from unresectable gastric cancer. J Palliat Med. 2017;20(2):177–80.
Desai SP, Ben-Josef E, Normolle DP, Francis IR, Greenson JK, Simeone DM, et al. Phase I study of oxaliplatin, full-dose gemcitabine, and concurrent radiation therapy in pancreatic cancer. J Clin Oncol. 2007;25(29):4587–92.
Wada Y, Uchiba M, Kawano Y, Kai N, Takahashi W, Honda J, et al. Severe bleeding tendency caused by a rare complication of excessive fibrinolysis with disseminated intravascular coagulation in a 51-year-old Japanese man with prostate cancer: a case report. J Med Case Reports. 2012;6:378.
Rocha E, Paramo JA, Montes R, Panizo C. Acute generalized, widespread bleeding. Diagnosis and management. Haematologica. 1998;83(11):1024–37.
Okajima K, Sakamoto Y, Uchiba M. Heterogeneity in the incidence and clinical manifestations of disseminated intravascular coagulation: a study of 204 cases. Am J Hematol. 2000;65(3):215–22.
Tallman MS, Lefebvre P, Baine RM, Shoji M, Cohen I, Green D, et al. Effects of all-trans retinoic acid or chemotherapy on the molecular regulation of systemic blood coagulation and fibrinolysis in patients with acute promyelocytic leukemia. J Thromb Haemost. 2004;2(8):1341–50.
Menell JS, Cesarman GM, Jacovina AT, McLaughlin MA, Lev EA, Hajjar KA. Annexin II and bleeding in acute promyelocytic leukemia. N Engl J Med. 1999;340(13):994–1004.
Kwaan HC, Wang J, Weiss I. Expression of receptors for plasminogen activators on endothelial cell surface depends on their origin. J Thromb Haemost. 2004;2(2):306–12.
Celebi N, Celebioglu B, Selcuk M, Canbay O, Karagoz AH, Aypar U. The role of antifibrinolytic agents in gynecologic cancer surgery. Saudi Med J. 2006;27(5):637–41.
Sallah S, Wan JY. Inhibitors against factor VIII in patients with cancer. Analysis of 41 patients. Cancer. 2001;91(6):1067–74.
Uramoto H, Shimokawa H, Tanaka F. Postoperative bleeding after surgery in patients with lung cancer. Anticancer Res. 2014;34(2):981–4.
Bonello VA, Bhangu A, Fitzgerald JE, Rasheed S, Tekkis P. Intraoperative bleeding and haemostasis during pelvic surgery for locally advanced or recurrent rectal cancer: a prospective evaluation. Tech Coloproctol. 2014;18(10):887–93.
Yamashita S, Tokuishi K, Moroga T, Abe S, Yamamoto K, Miyahara S, et al. Totally thoracoscopic surgery and troubleshooting for bleeding in non-small cell lung cancer. Ann Thorac Surg. 2013;95(3):994–9.
Campagnutta E, Giorda G, De Piero G, Gallo A, Fantin D, Scarabelli C. Different patterns of postoperative bleeding following cytoreductive surgery for gynecological cancer. Eur J Gynaecol Oncol. 2000;21(1):91–4.
Wettstein P, Haeberli A, Stutz M, Rohner M, Corbetta C, Gabi K, et al. Decreased factor XIII availability for thrombin and early loss of clot firmness in patients with unexplained intraoperative bleeding. Anesth Analg. 2004;99(5):1564–9; table of contents
Korte W, Gabi K, Rohner M, Gahler A, Szadkowski C, Schnider TW, et al. Preoperative fibrin monomer measurement allows risk stratification for high intraoperative blood loss in elective surgery. Thromb Haemost. 2005;94(1):211–5.
Korte WC, Szadkowski C, Gahler A, Gabi K, Kownacki E, Eder M, et al. Factor XIII substitution in surgical cancer patients at high risk for intraoperative bleeding. Anesthesiology. 2009;110(2):239–45.
Hashiguchi Y, Fukuda T, Ichimura T, Matsumoto Y, Yasui T, Sumi T, et al. Chemotherapy-induced thrombocytopenia and clinical bleeding in patients with gynecologic malignancy. Eur J Gynaecol Oncol. 2015;36(2):168–73.
Appel IM, Hop WC, van Kessel-Bakvis C, Stigter R, Pieters R. L-Asparaginase and the effect of age on coagulation and fibrinolysis in childhood acute lymphoblastic leukemia. Thromb Haemost. 2008;100(2):330–7.
Kasturi J, Saraya AK. Platelet functions in dysproteinaemia. Acta Haematol. 1978;59(2):104–13.
Colwell NS, Tollefsen DM, Blinder MA. Identification of a monoclonal thrombin inhibitor associated with multiple myeloma and a severe bleeding disorder. Br J Haematol. 1997;97(1):219–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Korte, W. (2018). Thrombosis and Bleeding in Cancer Patients. In: Olver, I. (eds) The MASCC Textbook of Cancer Supportive Care and Survivorship. Springer, Cham. https://doi.org/10.1007/978-3-319-90990-5_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-90990-5_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-90989-9
Online ISBN: 978-3-319-90990-5
eBook Packages: MedicineMedicine (R0)