Abstract
Processes within the IVF laboratory are critical in achieving high success rates from assisted reproduction. These various processes make up the “culture system,” and optimizing each of these variables is crucial. Importantly, within the context of the entire culture system, “optimal” conditions may vary slightly from laboratory to laboratory. However, initial gamete quality aside and accounting for laboratory-specific considerations, there are critical components of the culture system that are important to maximizing resulting embryo development. Items such as incubator type and management, strict monitoring, and control of environmental variables like use of low oxygen, temperature, pH, and osmolality are of paramount importance. Careful screening and use of culture media, protein, and oil are all required to avoid potentially harmful conditions for embryo development.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Multiple factors influence the success of an IVF program. Obtaining good quality gametes and ensuring appropriate uterine receptivity are paramount. However, despite the often large variability in these clinical aspects or the inherent properties of patients themselves, immense focus and critique are often placed in the processes that occur within the confines of the IVF laboratory. It is often viewed that much of what drives IVF success, or failure, is a result of what occurs during the time that the gametes and embryos reside within the laboratory. The IVF laboratory takes extreme measures to ensure consistency and repeatability: tracking inventory, monitoring equipment function, and assessing technician efficacy on a regular basis. This attention to detail and quantification of quality data may explain why such credit, and blame, is often assigned to the laboratory.
Certainly, when embryo development is poor or outcomes are low, one of the first suspected culprits is a suboptimal culture system. Indeed, laboratory conditions are one key component than can impact embryo quality. As a result, immense amounts of time and resources are devoted to identifying the “optimal” system to culture embryos. The key word here, however, is “system,” as culturing embryos consists of several variables. Importantly, within the context of the entire culture system and interactions between variables, “optimal” conditions may vary slightly from laboratory to laboratory.
2 Gamete Processing
Quality of preimplantation embryos is dependent upon quality of the gametes used to create the embryo. Unfortunately, a significant component of gamete quality is inherent and beyond influence of laboratory conditions. Thus, it should be mentioned, that if gamete quality is poor, even an “optimal” culture system is likely unable to overcome inherent abnormalities. That being said, sperm and oocytes are processed and cultured briefly within the laboratory, and these brief periods can impact quality. A detailed discussion regarding the processing of oocytes and sperm is beyond the scope of this review. However, some key factors should be considered. Care should be taken to ensure appropriate environmental conditions, including temperature and pH stability, during handling and manipulation of oocytes and sperm. This includes use of appropriate media formulated for the respective gametes. Precautions should also be taken to avoid excessive physical stress during manipulations occurring during procedures like sperm isolation/centrifugation and oocyte denuding.
Laboratories should permit adequate oocyte maturation prior to insemination/ICSI, often 2–4 h post-retrieval. It has been shown that completion of nuclear maturation does not occur until ~1 h following polar body extrusion and injection of oocytes prior to 2–4 h after retrieval yielded lower fertilization rates [1]. The culture of cumulus intact oocytes for 3–6 h prior to injection yielded superior fertilization and cleavage embryo development compared to those cultured <3 h [2]. Similarly, using patient randomization in a prospective trial, waiting for 4 h to inject cumulus intact oocytes following retrieval, yielded superior fertilization and blastocyst development compared to injection immediately after retrieval [3]. It should be noted that these timings are likely dependent upon the type of stimulation and trigger used and timing between the trigger and oocyte retrieval.
It is known that separation and processing techniques can impact sperm quality and DNA integrity and likely resulting embryo quality [4, 5]. Various studies exist comparing common sperm isolation practices such as density gradient separation, swim-up and also newer technological approaches [6,7,8,9]. A clear consensus as to the superior approach is not apparent from the literature and conflicting results may stem from subtle variations in techniques, such as gradient used, centrifugation speed and time of centrifugation, number of washes, media used, swim-up technique and other variables [10]. Appropriate sperm concentrations should be used for standard insemination cases, with 50,000–100,000 motile sperm/mL as standard accepted concentrations. Brief co-incubation of sperm with eggs has been shown to be sufficient and may avoid possible negative impacts of extended sperm exposure [11,12,13]. Elevated sperm concentrations and/or extended exposure could be detrimental to oocyte quality and embryo development due to increased ROS, lowered pH, or other media alterations. With regard to ICSI , at a minimum, normal morphology sperm should be utilized for injection with sperm assessment at 400×. Use of higher magnification approaches, such as IMSI, does not appear overly beneficial, though this may depend on patient population and what magnification is normally used for ICSI [14,15,16,17]. Emerging sperm selection approaches, such as PICSI , may also be useful [18], though this likely depends on the patient population and semen characteristics [19].
3 Embryo Culture
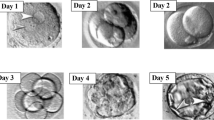
Once a sperm has been successfully joined with an egg, formation of a zygote occurs. Continued development of the resulting preimplantation embryo in vitro, often to the blastocyst stage, is a requirement for a successful IVF program. Therefore, the culture conditions used in the laboratory must support this development. However, numerous variables are present in the embryo culture system. Thus, it is extremely difficult to do a properly controlled comparison of culture systems, considering the number of variables involved. Without an exhaustive comparison within the same laboratory, identification of an “optimal” system is practically unattainable.
That being said, there are key components of the culture system that have been found to be superior to alternative approaches and that are viewed as “best practices.” Some of these key components, as well as other relevant variables, will be discussed.
3.1 Incubators
Minimizing environmentally induced stress within the IVF laboratory is crucial in creating a culture system optimized for embryo development and to achieve maximal assisted reproductive outcomes. Key environmental variables to consider include temperature, humidity and atmospheric/gas stability. These can subsequently impact properties of embryo culture media, such as pH and osmolality. Importantly, all of these potential stressors are regulated or impacted by the laboratory incubator. As a result, the incubator is arguably the most important piece of equipment in the embryo culture system.
Multiple culture incubator types exist with varying capabilities and differing methods of regulating their internal environment. Box-type incubators, initially developed to hold multiple flasks of somatic cells, have been long used for clinical IVF. These were later adapted to smaller box-type incubators, with lower volume and faster gas/atmosphere recovery following openings/closings. Most recently, a plethora of embryo-specific benchtop incubators have been development. These newer incubators tend to have several small chambers for individual patients to reduce the number of openings/closing and to speed gas recovery. They tend to also include direct heat for faster temperature recovery and various accessories, such as air filtration and other technologies aimed at improving environmental stability. As a result, selection of an appropriate culture incubator for the IVF laboratory has become a complex process. To date, there is no clear consensus as to a superior incubator type, as exhaustive controlled comparisons have not been done, and as efficacy and environmental stability rely heavily on incubator management [20] (Table 9.1).
For any incubator, optimal function requires proper use and daily quality control (gas and temperature measurements/validation). An appropriate number of units is required to avoid overcrowding with patient samples and prevent excessive openings/closings. Reduced incubator openings appears to benefit mouse embryo development [21, 22], as well as improving human blastocyst development [23]. Importantly, it should be noted that while single-step culture media (discussed later) and new time-lapse incubator technology permit uninterrupted culture of embryos with no disturbance over 5/6 days of development, no clear benefit of this approach has been shown, indicating that other variables in the culture system must also be considered [24,25,26]. A mix of incubator types within an individual laboratory permits a wide variety of uses to accommodate different dish or test-tube types, as well as implementation of emerging culture technology.
3.2 Atmosphere
Today’s optimal culture system requires the use of low oxygen within the incubator. Culturing embryos in reduced oxygen concentrations (~5%), compared to atmospheric concentrations of ~21%, have been long recognized as superior in various animal IVF systems [27,28,29,30,31,32,33]. This makes sense when one considers the female reproductive tract appears to have oxygen levels between 2 and 8% (see reviews [31]). Numerous studies have also demonstrated improved human embryo development, implantation, and pregnancy rates when using reduced oxygen concentrations [34,35,36,37,38,39,40,41,42,43,44,45,46]. Importantly, use of low oxygen throughout the entire culture period through day 5/6 appears to be required to see the most benefit [34, 36, 46]. While 5% is often the standard concentration used for low oxygen culture, it is currently unknown if even lower oxygen concentrations or differential oxygen concentrations during embryo development may yield superior outcomes [47, 48].
There is no consensus as to the superior method of achieving low oxygen conditions. Nitrogen gas is used to depress oxygen concentration down from atmospheric levels of 21%. Nitrogen gas can be supplied via a nitrogen generator, nitrogen gas siphoned from a high-pressure liquid nitrogen tank, or compressed cylinders of nitrogen or premixed cylinders of gas.
The exact mechanism of the benefit of low oxygen use for embryo culture is unknown. Use of low oxygen may be superior due to improved embryo metabolism, reduced ROS, or perhaps even improved air quality (reduced levels of VOCs).
Maintenance of an appropriate and stable CO2 concentration by the laboratory incubator is also required to ensure a highly effective embryo culture system. The carbon from CO2 can be utilized by developing embryos for biosynthetic processes [49,50,51]. Additionally, the CO2 concentration inside the incubator is important in establishing the pH of the embryo culture media [52,53,54]. The CO2 gas dissolves in the media and reaches equilibrium with the sodium bicarbonate concentrations to establish a set point. As CO2 is increased, pH decreases and vice versa. This is important because the pH of culture media can impact embryo development. No clear consensus exits as to the optimal pH requirement of embryo culture media to optimize development. This may vary between media, due to the impact of ingredients, such as lactate [54], and may vary between embryo developmental stages [54, 55]. The value usually falls between 7.2–7.4 and may change if using a sequential cutlure medium. The amount of CO2 required to achieve the desired pH will vary between labs based on lab elevation, type of culture media, and other variables (protein concentrations, etc.). Rapid and accurate CO2 recovery and maintenance of CO2/pH stability is paramount. Thus establishment of the desired pH range by the laboratory is required, with pH measurement to determine the required CO2 concentration with routine verification.
3.3 Temperature
Temperature is another variable of the culture system that may impact efficacy. It is well known that temperature can impact various aspects of gamete and embryo function, most notably, meiotic spindle stability [56,57,58] and possibly embryo metabolism [59]. Studies have reported that maintaining a warm temperature around 35–37 °C compared to 25–30 °C during retrieval is beneficial for bovine embryo development and mouse embryo gene expression [60, 61]. Maintaining temperature stability around 37 °C during human oocyte injection also improved fertilization rates and embryo development [57]. However the optimal temperature at which to culture embryos remains unknown.
Commonly, 37 °C is used to culture embryos and is based on the estimate of human core body temperature. Importantly, body temperature varies and is likely not exactly 37 °C. Temperature can vary based on time of day, between the sexes and between individuals. Furthermore, temperature of the female reproductive tract may actually be slightly less than the core body temperature. The temperature of the human follicle is ~2.3 °C cooler than surrounding stroma, and the fallopian tube from animal models carries a temperature gradient ~1.5 °C cooler [62,63,64,65,66,67]. As a result, the question has been poised “whether human IVF and related procedures should be carried out, at, say, 35.5–36°C rather than at 37°C” [59]. Use of a 1.5 °C lower temperature would presumably lower the metabolic rate of the embryo ~15%, which may result in a more “quiet” metabolism, thereby possibly benefiting embryo development [59]. However, this hypothesis has not been proven.
Recently, a prospective randomized controlled trial utilized patient embryo splits and examined the effect of culture human embryos at either 37 or 36 °C [68]. Controlling for temperature variations, incubator type, and pH, authors demonstrated that culture of human embryos at 37 °C yields higher average cell numbers at day 3 of development, higher blastocyst formation , and higher useable blastocyst rates compared to 36 °C (Table 9.2). No differences were observed in rates of aneuploidy or implantation. More detailed analysis of the optimal temperature for embryo culture is required, but the best practice at the moment appears to be maintenance of a stable temperature around 37 °C.
There is no clear advantage of one incubator type over another in terms of temperature regulation, though some types may recover temperature faster or maintain temperature better than others under various circumstances [20]. In addition to incubators, temperature stability should be monitored on other lab equipment, such as warm ovens and heating stages. The type of culture dish, as well as other factors that can impact heat exchange, should be considered. Careful monitoring of temperature and proper handling of embryos during use is imperative to ensure the desired conditions are achieved and maintained.
3.4 Group Culture
It is known that embryos can modify their surrounding microenvironments during culture though secretion or depletion of various proteins. Indeed, examination of the embryo secretome through analysis of spent culture media has become an active area of research [69,70,71,72,73,74,75,76,77,78]. Modification of their own microenvironment may impact embryo development during the culture period. It is therefore perhaps not surprising that group embryo culture has been shown to be beneficial over individual embryo culture for animal embryos, from both mono- and polyovulatory species. Various studies have shown a benefit of group culture of embryos from the rodent [79,80,81,82,83] as well as domestic species like the cow, sheep, and pig [84,85,86,87,88,89,90,91].
Similarly, studies exist that indicate human embryos may also benefit from group embryo culture [92]. Grouping of human embryos significantly enhanced cleavage rates but not morphology grade as compared with embryos grown individually [93]. Group embryo culture resulted in significantly improved pregnancy rates, with embryos grown in groups producing a 43% pregnancy rate per transfer, compared to a 24% pregnancy rate for embryos that were cultured individually [94]. A retrospective analysis of patients who had embryos cultured from day 1 to day 3, either individually or in groups of three to five embryos, had no differences in pregnancy or implantation rates, but those cultured in groups did result in more usable blastocysts [95]. This is similar to a prior prospective report that indicated no benefit of group culture of human embryos prior to day 2 or day 3 transfer [96], suggesting extended culture may be required to observe the full benefits of group embryo culture. Finally, prospective trial patients had their embryos split between three treatment groups using sibling embryos [9]. Embryos were cultured individually or in groups where embryos were physically separated but able to exchange media, or in groups without physical separation. Importantly, all treatments were included within the same culture dish to help control for variables. Group culture of embryos without physical separation resulted in greater rates of compaction on day 4 and blastocyst formation on day 5 compared to group culture with physical separation and embryos cultured individually. Group culture yielded a trend toward higher live birth rate compared to individual culture. This indicates that extended group culture of embryos may be beneficial for human preimplantation embryo development and that physical contact or proximity of embryos seems to be an important factor.
3.5 Culture Dishes
Various factors involved in group embryo culture can impact results, including volume of media and shape/size of the culture area. These factors can impact the ratio of media volume used to the number of embryos (embryo density) and embryo spacing. Importantly, these factors may be influenced by the type of culture dish utilized. The type of culture dish may impact heat exchange during embryo manipulations due to surface contact with the bottom of the dish. The type of culture dish may also be dictated by the type of incubator. Notably, new time-lapse incubator systems have proprietary culture dishes, many of which promote single embryo culture or that are aimed at trying to utilize a beneficial microenvironment created by the culture area. The type of culture dish could therefore have an impact on embryo quality and outcomes [97,98,99]. Currently, there is no consensus as to a superior type of culture dish or volume of media used for embryo culture.
Directly related to optimizing the culture system is an assurance that the culture dish, as well as other contact materials, is nontoxic. Contact material testing is one of the most important aspects of laboratory QC/QA and is paramount for improving embryo development. It is well documented that not all products, despite being packaged or sold as sterile, are inert in terms of the impact on embryo development [100, 101]. Thus, verification of material safety is required prior to clinical use. This is usually performed using a relevant bioassay, such as the mouse embryo assay (MEA) or the human sperm survival assay (HSSA) , also known as the human sperm motility assay (HSMA) . Comparisons and the merits of these two assays have been discussed elsewhere [102,103,104,105,106,107,108], and each can be useful in their own respect, with factors such as cost and availability warranting attention. Perhaps more importantly, the sensitivity of the bioassay is important, and approaches can be modified to increase this sensitivity to ensure that subtle material toxicity can be detected. Examples of approaches used to increase sensitivity are use of the one-cell vs. the two-cell MEA, outbred vs. inbred vs. hybrid mouse strains, blastocyst cell counts vs. simple blastocyst formation, exclusion of protein from media vs. protein inclusion, and use of a simple media vs. a more robust complex media [109,110,111]. Importantly, thresholds must be set for an assay to “pass,” and these thresholds should be set to ensure rigorous criteria. Each laboratory can determine which assay and threshold suits their needs regarding sensitivity and cost. A commonly used and often recommended sensitive assay includes using the one-cell MEA, noting time-appropriate embryo development with the rate of expanded or hatching blastocyst >70% at 96 h (4 days) of culture. Real-time assessment of morphokinetics may also be useful in helping improve sensitivity of the MEA [112].
3.6 Culture Media
In trying to discern key components of the “optimal” embryo culture system, focus often immediately turns to culture media. Unquestionably, culture media plays a significant role in embryo development and quality and therefore, clinical outcomes. However, in terms of identifying or selecting the single “optimal” medium for use within IVF laboratories, this is likely a futile endeavor. As mentioned, numerous variables are present within the laboratory and can impact culture media performance [113]. Thus, the same medium can perform differently between laboratories. The inability to identity a single optimum media is reflected by examining the numerous studies in the literature comparing one medium against another [114]. Indeed, when examining prospective trials using sibling oocytes splits or patient randomization, comparison of different sequential media [115,116,117,118,119,120,121], as well as comparisons between single-step culture media and sequential media [122,123,124,125,126,127], many studies fail to identify a clearly superior approach or product. No trial exists comparing every available media against each other in a controlled fashion, which would be required to identify the superior medium. It is also unclear whether changing media at 48 or 72 h intervals or utilizing uninterrupted culture yields superior results with modern media formulations. Individual laboratories should perform their own trials/splits to determine which product and methodology performs most successfully under their specific conditions. (see Table 9.3).
Modern human embryo culture media must contain some assortment of amino acids. Amino acids support numerous cellular processes, including acting as metabolites, osmolytes, antioxidants and buffers, and likely help alleviate stress in the embryo culture system [136]. Brief period of culture with no amino acids present can impair mouse embryo development [21]. While animal studies have given some insight [128, 129, 137], it is likely impossible to determine the optimal mixture and concentrations of specific amino acids for human embryo culture. Studies have identified glycine, taurine, and glutamine as important amino acids for human embryos [131,132,133]. If glutamine is present, modern embryo culture media should include the dipeptide form of the amino acid. Use of the stable dipeptide-glutamine helps avoid ammonium accumulation and the associated detrimental effects on human embryo development and appears superior to glutamine [130, 134, 135, 138]. No clear consensus exists regarding whether glycyl-glutamine or alanyl-glutamine is the superior dipeptide for human embryo culture. Whether use of other dipeptide amino acids may be beneficial is unknown.
The pH of culture media should be monitored and used adhering to manufacturers recommendations. As mentioned, CO2 concentrations should be adjusted to achieve the desired/recommended pH. No clear consensus exists as to the ideal pH for embryo culture, whether this be a single pH set point throughout culture or whether pH should change during embryo development.
3.7 Protein
Protein supplementation to culture media can have a dramatic impact on embryo development and resulting outcomes. The macromolecule supplementation can act as a surfactant, nitrogen source to stabilize membranes, modulate physical microenvironment, act as a carrier molecule for other compounds, or even bind trace elements/toxins. A recent report even indicates that protein in culture media can impact human birth weight [139], though results of the study should be interpreted with caution due to lack of control over other system variables. Regardless, it is irrefutable that protein supplements are the ones least defined components of the culture system and thus are a large source of potential variation. For example, stabilizers/preservatives, such as octanoic acid, used when making protein solutions, may be embryotoxic [140]. Additionally, as mentioned, other proteins, growth factors, and hormone “contaminants” may be present at varying levels in protein preparation [141,142,143]. Some clinical IVF media currently include growth factors, though limited data exists to support their purposeful use [144,145,146], and this remains a controversial topic [147]. Thus, to optimize performance of the culture system, specific lot numbers of protein should be screened for efficacy prior to clinical implementation.
Primary protein supplements used in clinical embryo culture media include human serum albumin (HSA), as well as complex protein supplements containing HSA and a combination of alpha and beta globulins [148, 149]. Recombinant albumin is also available, as well as a dextran-based macromolecular supplement. Data suggest that a complex protein supplement with globulins is superior to HSA for animal embryos [148, 150], human embryo development [151, 152], and even live birth [153]. This may be due to growth hormones and other components in the complex protein products [142]. Recombinant albumin gave comparable embryo development to HSA in a prospective randomized trial and may reduce variability in the culture system [154]. Optimal concentrations of protein are unknown, though 5% of albumin or 10% of complex protein products are commonly used and higher concentrations of up to 20% of a globulin supplement may be beneficial in certain circumstances [155].
Care should be taken to ensure pH of the culture media is still within expected ranges after adding protein, as supplementation can cause pH to shift and may require adjustment of incubator CO2 levels.
3.8 Oil
Oil overlay is commonly used during embryo culture to prevent media evaporation, which can result in media osmolality increase and compromised embryo development. Oil is required when using modern benchtop incubators with no humidification. However, open culture, or culture without oil overlay, may also be used if humidification is present and sufficient volume of media is used. Similar to protein, despite improvements in refinement and testing, oil overlay products can differ significantly due to contaminants and are a large source of variation within the culture system. Washing of oil with either water or culture media can help alleviate some toxicity concerns [156] and a good practice to ensure that all oil is washed. Additionally, proper storage is required to avoid peroxidation of oil, which can lead to embryo toxicity [156,157,158,159]. Recommendations often include keeping oil out of direct light and storing at 4 °C.
There are several oil products for embryo culture including paraffin oil and light mineral oil. Products are sold in plastic or glass bottles. There is no clear consensus on a superior oil type or packaging method. Regardless of the oil, testing using an approved bioassay is recommended prior to use.
4 Conclusions
It is evident that there are numerous variables to consider when attempting to optimize an embryo culture system. Interactions between variables can impact outcomes. Thus, an “optimum” system may vary slightly from laboratory to laboratory. Key variables that appear consistent between high-performing culture systems include use of low-oxygen, proper incubator management to yield stable CO2/pH and temperature and proper quality control. Of course, even if a culture system is optimized, embryo selection remains a critically important factor to maximize outcomes. In fact, if a system is optimized to maximize embryo development, then selection of embryos becomes even more difficult, as there are more “good quality” embryos to choose from. Embryo assessment, noting key morphological features or morphokinetic timings/selection algorithms, or use of embryo biopsy/CCS become very important.
With advances in technology, culture “systems” have been introduced which consist of advanced incubator systems with imaging technology, proprietary customized cultureware, and embryo selection algorithms. Even if selecting one of these systems, differing culture media and other variables, such as protein and oil, often vary. This is likely at least one reason why there appears to be difficulty in identifying a single embryo selection algorithm that is applicable between laboratories. Regardless, existing data does not demonstrate that any of these emerging commercial systems is superior to another or to more traditional methods of culturing embryos to the blastocyst stage [160,161,162,163,164].
References
Hyun CS, Cha JH, Son WY, Yoon SH, Kim KA, Lim JH. Optimal ICSI timing after the first polar body extrusion in in vitro matured human oocytes. Hum Reprod. 2007;22(7):1991–5. https://doi.org/10.1093/humrep/dem124; [pii]: dem124.
Rienzi L, Ubaldi F, Anniballo R, Cerulo G, Greco E. Preincubation of human oocytes may improve fertilization and embryo quality after intracytoplasmic sperm injection. Hum Reprod. 1998;13(4):1014–9.
Hassan HA. Cumulus cell contribution to cytoplasmic maturation and oocyte developmental competence in vitro. J Assist Reprod Genet. 2001;18(10):539–43.
Sakkas D. Novel technologies for selecting the best sperm for in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril. 2013;99(4):1023–9. https://doi.org/10.1016/j.fertnstert.2012.12.025.
Said TM, Land JA. Effects of advanced selection methods on sperm quality and ART outcome: a systematic review. Hum Reprod Update. 2011;17(6):719–33. https://doi.org/10.1093/humupd/dmr032.
Simon L, Murphy K, Aston KI, Emery BR, Hotaling JM, Carrell DT. Optimization of microelectrophoresis to select highly negatively charged sperm. J Assist Reprod Genet. 2016;33(6):679–88. https://doi.org/10.1007/s10815-016-0700-x.
Smith GD, Takayama S. Application of microfluidic technologies to human assisted reproduction. Mol Hum Reprod. 2017;23(4):257–68. https://doi.org/10.1093/molehr/gaw076.
Shirota K, Yotsumoto F, Itoh H, Obama H, Hidaka N, Nakajima K, Miyamoto S. Separation efficiency of a microfluidic sperm sorter to minimize sperm DNA damage. Fertil Steril. 2016;105(2):315–21.e1. https://doi.org/10.1016/j.fertnstert.2015.10.023.
Seiringer M, Maurer M, Shebl O, Dreier K, Tews G, Ziehr S, Schappacher-Tilp G, Petek E, Ebner T. Efficacy of a sperm-selection chamber in terms of morphology, aneuploidy and DNA packaging. Reprod Biomed Online. 2013;27(1):81–8. https://doi.org/10.1016/j.rbmo.2013.03.013.
Jayaraman V, Upadhya D, Narayan PK, Adiga SK. Sperm processing by swim-up and density gradient is effective in elimination of sperm with DNA damage. J Assist Reprod Genet. 2012;29(6):557–63. https://doi.org/10.1007/s10815-012-9742-x.
Lin SP, Lee RK, Su JT, Lin MH, Hwu YM. The effects of brief gamete co-incubation in human in vitro fertilization. J Assist Reprod Genet. 2000;17(6):344–8.
Swenson K, Check JH, Summers-Chase D, Choe JK, Check ML. A randomized study comparing the effect of standard versus short incubation of sperm and oocyte on subsequent pregnancy and implantation rates following in vitro fertilization embryo transfer. Arch Androl. 2000;45(1):73–6.
Le Bras A, Hesters L, Gallot V, Tallet C, Tachdjian G, Frydman N. Shortening gametes co-incubation time improves live birth rate for couples with a history of fragmented embryos. Syst Biol Reprod Med. 2017;63:1–7. https://doi.org/10.1080/19396368.2017.1336581.
Teixeira DM, Barbosa MA, Ferriani RA, Navarro PA, Raine-Fenning N, Nastri CO, Martins WP. Regular (ICSI) versus ultra-high magnification (IMSI) sperm selection for assisted reproduction. Cochrane Database Syst Rev. 2013;(7):CD010167. https://doi.org/10.1002/14651858.CD010167.pub2.
Leandri RD, Gachet A, Pfeffer J, Celebi C, Rives N, Carre-Pigeon F, Kulski O, Mitchell V, Parinaud J. Is intracytoplasmic morphologically selected sperm injection (IMSI) beneficial in the first ART cycle? A multicentric randomized controlled trial. Andrology. 2013;1(5):692–7. https://doi.org/10.1111/j.2047-2927.2013.00104.x.
De Vos A, Van de Velde H, Bocken G, Eylenbosch G, Franceus N, Meersdom G, Tistaert S, Vankelecom A, Tournaye H, Verheyen G. Does intracytoplasmic morphologically selected sperm injection improve embryo development? A randomized sibling-oocyte study. Hum Reprod. 2013;28(3):617–26. https://doi.org/10.1093/humrep/des435.
Delaroche L, Yazbeck C, Gout C, Kahn V, Oger P, Rougier N. Intracytoplasmic morphologically selected sperm injection (IMSI) after repeated IVF or ICSI failures: a prospective comparative study. Eur J Obstet Gynecol Reprod Biol. 2013;167(1):76–80. https://doi.org/10.1016/j.ejogrb.2012.11.011.
Worrilow KC, Eid S, Woodhouse D, Perloe M, Smith S, Witmyer J, Ivani K, Khoury C, Ball GD, Elliot T, Lieberman J. Use of hyaluronan in the selection of sperm for intracytoplasmic sperm injection (ICSI): significant improvement in clinical outcomes—multicenter, double-blinded and randomized controlled trial. Hum Reprod. 2013;28(2):306–14. https://doi.org/10.1093/humrep/des417.
Majumdar G, Majumdar A. A prospective randomized study to evaluate the effect of hyaluronic acid sperm selection on the intracytoplasmic sperm injection outcome of patients with unexplained infertility having normal semen parameters. J Assist Reprod Genet. 2013;30(11):1471–5. https://doi.org/10.1007/s10815-013-0108-9.
Swain JE. Decisions for the IVF laboratory: comparative analysis of embryo culture incubators. Reprod Biomed Online. 2014;28(5):535–47. https://doi.org/10.1016/j.rbmo.2014.01.004.
Gardner DK, Lane M. Alleviation of the ‘2-cell block’ and development to the blastocyst of CF1 mouse embryos: role of amino acids, EDTA and physical parameters. Hum Reprod. 1996;11(12):2703–12.
Hyslop L, Prathalingam N, Nowak L, Fenwick J, Harbottle S, Byerley S, Rhodes J, Watson B, Henderson R, Murdoch A, Herbert M. A novel isolator-based system promotes viability of human embryos during laboratory processing. PLoS One. 2012;7(2):e31010. https://doi.org/10.1371/journal.pone.0031010; [pii]: PONE-D-11-18079.
Zhang JQ, Li XL, Peng Y, Guo X, Heng BC, Tong GQ. Reduction in exposure of human embryos outside the incubator enhances embryo quality and blastulation rate. Reprod Biomed Online. 2010;20(4):510–5. https://doi.org/10.1016/j.rbmo.2009.12.027; [pii]: S1472-6483(09)00340-X.
Park H, Bergh C, Selleskog U, Thurin-Kjellberg A, Lundin K. No benefit of culturing embryos in a closed system compared with a conventional incubator in terms of number of good quality embryos: results from an RCT. Hum Reprod. 2015;30(2):268–75. https://doi.org/10.1093/humrep/deu316.
Kirkegaard K, Hindkjaer JJ, Grondahl ML, Kesmodel US, Ingerslev HJ. A randomized clinical trial comparing embryo culture in a conventional incubator with a time-lapse incubator. J Assist Reprod Genet. 2012;29(6):565–72. https://doi.org/10.1007/s10815-012-9750-x.
Wu YG, Lazzaroni-Tealdi E, Wang Q, Zhang L, Barad DH, Kushnir VA, Darmon SK, Albertini DF, Gleicher N. Different effectiveness of closed embryo culture system with time-lapse imaging (EmbryoScope(TM)) in comparison to standard manual embryology in good and poor prognosis patients: a prospectively randomized pilot study. Reprod Biol Endocrinol. 2016;14(1):49. https://doi.org/10.1186/s12958-016-0181-x.
Lonergan P, Rizos D, Gutierrez-Adan A, Fair T, Boland MP. Oocyte and embryo quality: effect of origin, culture conditions and gene expression patterns. Reprod Domest Anim. 2003;38(4):259–67.
Kelley RL, Gardner DK. Combined effects of individual culture and atmospheric oxygen on preimplantation mouse embryos in vitro. Reprod Biomed Online. 2016;33:537. https://doi.org/10.1016/j.rbmo.2016.08.003.
Preis KA, Seidel GE Jr, Gardner DK. Reduced oxygen concentration improves the developmental competence of mouse oocytes following in vitro maturation. Mol Reprod Dev. 2007;74(7):893–903. https://doi.org/10.1002/mrd.20655.
Thompson JG, Simpson AC, Pugh PA, Donnelly PE, Tervit HR. Effect of oxygen concentration on in-vitro development of preimplantation sheep and cattle embryos. J Reprod Fertil. 1990;89(2):573–8.
Wale PL, Gardner DK. The effects of chemical and physical factors on mammalian embryo culture and their importance for the practice of assisted human reproduction. Hum Reprod Update. 2016;22(1):2–22. https://doi.org/10.1093/humupd/dmv034.
Lonergan P, O’Kearney-Flynn M, Boland MP. Effect of protein supplementation and presence of an antioxidant on the development of bovine zygotes in synthetic oviduct fluid medium under high or low oxygen tension. Theriogenology. 1999;51(8):1565–76.
Tervit HR, Whittingham DG, Rowson LE. Successful culture in vitro of sheep and cattle ova. J Reprod Fertil. 1972;30(3):493–7.
Kovacic B, Vlaisavljevic V. Influence of atmospheric versus reduced oxygen concentration on development of human blastocysts in vitro: a prospective study on sibling oocytes. Reprod Biomed Online. 2008;17(2):229–36.
Kovacic B, Sajko MC, Vlaisavljevic V. A prospective, randomized trial on the effect of atmospheric versus reduced oxygen concentration on the outcome of intracytoplasmic sperm injection cycles. Fertil Steril. 2010;94(2):511–9. https://doi.org/10.1016/j.fertnstert.2009.03.077; [pii] S0015–0282(09)00747-X.
Waldenstrom U, Engstrom AB, Hellberg D, Nilsson S. Low-oxygen compared with high-oxygen atmosphere in blastocyst culture, a prospective randomized study. Fertil Steril. 2009;91(6):2461–5. https://doi.org/10.1016/j.fertnstert.2008.03.051; [pii]: S0015-0282(08)00714-0.
Kea B, Gebhardt J, Watt J, Westphal LM, Lathi RB, Milki AA, Behr B. Effect of reduced oxygen concentrations on the outcome of in vitro fertilization. Fertil Steril. 2007;87(1):213–6. https://doi.org/10.1016/j.fertnstert.2006.05.066; [pii]: S0015-0282(06)03160-8.
Dumoulin JC, Meijers CJ, Bras M, Coonen E, Geraedts JP, Evers JL. Effect of oxygen concentration on human in-vitro fertilization and embryo culture. Hum Reprod. 1999;14(2):465–9.
Catt JW, Henman M. Toxic effects of oxygen on human embryo development. Hum Reprod. 2000;15(Suppl 2):199–206.
Ciray HN, Aksoy T, Yaramanci K, Karayaka I, Bahceci M. In vitro culture under physiologic oxygen concentration improves blastocyst yield and quality: a prospective randomized survey on sibling oocytes. Fertil Steril. 2009;91(4 Suppl):1459–61. https://doi.org/10.1016/j.fertnstert.2008.07.1707; [pii]: S0015-0282(08)01482-9.
Bahceci M, Ciray HN, Karagenc L, Ulug U, Bener F. Effect of oxygen concentration during the incubation of embryos of women undergoing ICSI and embryo transfer: a prospective randomized study. Reprod Biomed Online. 2005;11(4):438–43.
Nanassy L, Peterson CA, Wilcox AL, Peterson CM, Hammoud A, Carrell DT. Comparison of 5% and ambient oxygen during days 3-5 of in vitro culture of human embryos. Fertil Steril. 2010;93(2):579–85. https://doi.org/10.1016/j.fertnstert.2009.02.048.
Gomes Sobrinho DB, Oliveira JB, Petersen CG, Mauri AL, Silva LF, Massaro FC, Baruffi RL, Cavagna M, Franco JG Jr. IVF/ICSI outcomes after culture of human embryos at low oxygen tension: a meta-analysis. Reprod Biol Endocrinol. 2011;9:143. https://doi.org/10.1186/1477-7827-9-143.
Petersen A, Mikkelsen AL, Lindenberg S. The impact of oxygen tension on developmental competence of post-thaw human embryos. Acta Obstet Gynecol Scand. 2005;84(12):1181–4. https://doi.org/10.1111/j.0001-6349.2005.00630.x.
Bedaiwy MA, Mahfouz RZ, Goldberg JM, Sharma R, Falcone T, Abdel Hafez MF, Agarwal A. Relationship of reactive oxygen species levels in day 3 culture media to the outcome of in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril. 2010;94(6):2037–42. https://doi.org/10.1016/j.fertnstert.2009.12.020; [pii]: S0015-0282(09)04206-X.
Meintjes M, Chantilis SJ, Douglas JD, Rodriguez AJ, Guerami AR, Bookout DM, Barnett BD, Madden JD. A controlled randomized trial evaluating the effect of lowered incubator oxygen tension on live births in a predominantly blastocyst transfer program. Hum Reprod. 2009;24(2):300–7. https://doi.org/10.1093/humrep/den368; [pii]: den368.
Kaser DJ. On developing a thesis for reproductive endocrinology and infertility fellowship: a case study of ultra-low (2%) oxygen tension for extended culture of human embryos. J Assist Reprod Genet. 2017;34(3):303–8. https://doi.org/10.1007/s10815-017-0887-5.
Morin SJ. Oxygen tension in embryo culture: does a shift to 2% O2 in extended culture represent the most physiologic system? J Assist Reprod Genet. 2017;34(3):309–14. https://doi.org/10.1007/s10815-017-0880-z.
Quinn P, Wales RG. Fixation of carbon dioxide by preimplantation rabbit embryos in vitro. J Reprod Fertil. 1974;36(1):29–39.
Quinn P, Wales RG. Fixation of carbon dioxide by pre-implantation mouse embryos in vitro and the activities of enzymes involved in the process. Aust J Biol Sci. 1971;24(6):1277–90.
Wales RG, Quinn P, Murdoch RN. The fixation of carbon dioxide by the eight-cell mouse embryo. J Reprod Fertil. 1969;20(3):541–3.
Swain J. Embryo culture and pH. Fertil Steril. 2011;95(8):e67; author reply e68. https://doi.org/10.1016/j.fertnstert.2011.04.024.
Swain JE. Optimizing the culture environment in the IVF laboratory: impact of pH and buffer capacity on gamete and embryo quality. Reprod Biomed Online. 2010;21(1):6–16. https://doi.org/10.1016/j.rbmo.2010.03.012.
Swain JE. Is there an optimal pH for culture media used in clinical IVF? Hum Reprod Update. 2012;18(3):333–9. https://doi.org/10.1093/humupd/dmr053.
Adolfsson E, Meintjes M, Guerami A, Mehta R, Davidson K, Qing Y. Shift in pH during transition to the embryonic genome impacts embryo development. Hum Reprod. 2016;31(1).
Sun XF, Wang WH, Keefe DL. Overheating is detrimental to meiotic spindles within in vitro matured human oocytes. Zygote. 2004;12(1):65–70.
Wang WH, Meng L, Hackett RJ, Oldenbourg R, Keefe DL. Rigorous thermal control during intracytoplasmic sperm injection stabilizes the meiotic spindle and improves fertilization and pregnancy rates. Fertil Steril. 2002;77(6):1274–7; [pii]: S0015028202031175.
Wang WH, Meng L, Hackett RJ, Odenbourg R, Keefe DL. Limited recovery of meiotic spindles in living human oocytes after cooling-rewarming observed using polarized light microscopy. Hum Reprod. 2001;16(11):2374–8.
Leese HJ, Baumann CG, Brison DR, McEvoy TG, Sturmey RG. Metabolism of the viable mammalian embryo: quietness revisited. Mol Hum Reprod. 2008;14(12):667–72. https://doi.org/10.1093/molehr/gan065; [pii]: gan065.
Pollard JW, Martino A, Rumph ND, Songsasen N, Plante C, Leibo SP. Effect of ambient temperatures during oocyte recovery on in vitro production of bovine embryos. Theriogenology. 1996;46(5):849–58.
Lane M, Mitchell M, Cashman KS, Feil D, Wakefield S, Zander-Fox DL. To QC or not to QC: the key to a consistent laboratory? Reprod Fertil Dev. 2008;20(1):23–32.
Grinsted J, Kjer JJ, Blendstrup K, Pedersen JF. Is low temperature of the follicular fluid prior to ovulation necessary for normal oocyte development? Fertil Steril. 1985;43(1):34–9.
David A, Vilensky A, Nathan H. Temperature changes in different parts of the rabbit oviduct. Preliminary report. Harefuah. 1971;80(4):180–2.
Hunter RH, Bogh IB, Einer-Jensen N, Muller S, Greve T. Pre-ovulatory graafian follicles are cooler than neighbouring stroma in pig ovaries. Hum Reprod. 2000;15(2):273–83.
Hunter RH, Grondahl C, Greve T, Schmidt M. Graafian follicles are cooler than neighbouring ovarian tissues and deep rectal temperatures. Hum Reprod. 1997;12(1):95–100.
Hunter RH, Nichol R. A preovulatory temperature gradient between the isthmus and ampulla of pig oviducts during the phase of sperm storage. J Reprod Fertil. 1986;77(2):599–606.
Hunter RH. Temperature gradients in female reproductive tissues. Reprod Biomed online. 2012;24(4):377–80. https://doi.org/10.1016/j.rbmo.2011.12.007; [pii]: S1472-6483(12)00009-0.
Hong K, Forman E, Lee H, Ferry K, Treff N, Scott R. Optimizing the temperature for embyo culture in IVF: a randomized controlled trial (RCT) comparing standard culture temperature of 37C to the reduced more physiologic temperature of 36C. Fertil Steril. 2012;98(3):s167.
Mains LM, Christenson L, Yang B, Sparks AE, Mathur S, Van Voorhis BJ. Identification of apolipoprotein A1 in the human embryonic secretome. Fertil Steril. 2011;96(2):422–7. e422. https://doi.org/10.1016/j.fertnstert.2011.05.049.
Cortezzi SS, Garcia JS, Ferreira CR, Braga DP, Figueira RC, Iaconelli A Jr, Souza GH, Borges E Jr, Eberlin MN. Secretome of the preimplantation human embryo by bottom-up label-free proteomics. Anal Bioanal Chem. 2011;401(4):1331–9. https://doi.org/10.1007/s00216-011-5202-1.
Beardsley AJ, Li Y, O'Neill C. Characterization of a diverse secretome generated by the mouse preimplantation embryo in vitro. Reprod Biol Endocrinol. 2010;8:71. https://doi.org/10.1186/1477-7827-8-71; [pii]: 1477-7827-8-71.
Brison DR, Hollywood K, Arnesen R, Goodacre R. Predicting human embryo viability: the road to non-invasive analysis of the secretome using metabolic footprinting. Reprod Biomed Online. 2007;15(3):296–302.
Katz-Jaffe MG, Schoolcraft WB, Gardner DK. Analysis of protein expression (secretome) by human and mouse preimplantation embryos. Fertil Steril. 2006;86(3):678–85.
Bormann C, Swain J, Ni Q, Kennedy R, Smith G. Preimplantation embryo secretome identification. Fertil Steril. 2006;86(Suppl 2):s116.
Giacomini E, Vago R, Sanchez AM, Podini P, Zarovni N, Murdica V, Rizzo R, Bortolotti D, Candiani M, Vigano P. Secretome of in vitro cultured human embryos contains extracellular vesicles that are uptaken by the maternal side. Sci Rep. 2017;7(1):5210. https://doi.org/10.1038/s41598-017-05549-w.
Butler SA, Luttoo J, Freire MO, Abban TK, Borrelli PT, Iles RK. Human chorionic gonadotropin (hCG) in the secretome of cultured embryos: hyperglycosylated hCG and hCG-free beta subunit are potential markers for infertility management and treatment. Reprod Sci. 2013;20(9):1038–45. https://doi.org/10.1177/1933719112472739.
Katz-Jaffe MG, McCallie BR, Janesch A, Filipovits JA, Schoolcraft WB, Gardner DK. Blastocysts from patients with polycystic ovaries exhibit altered transcriptome and secretome. Reprod Biomed Online. 2010;21(4):520–6. https://doi.org/10.1016/j.rbmo.2010.05.010.
Katz-Jaffe MG, McReynolds S, Gardner DK, Schoolcraft WB. The role of proteomics in defining the human embryonic secretome. Mol Hum Reprod. 2009;15(5):271–7. https://doi.org/10.1093/molehr/gap012.
Canseco RS, Sparks AE, Pearson RE, Gwazdauskas FC. Embryo density and medium volume effects on early murine embryo development. J Assist Reprod Genet. 1992;9(5):454–7.
Lane M, Gardner DK. Effect of incubation volume and embryo density on the development and viability of mouse embryos in vitro. Hum Reprod. 1992;7(4):558–62.
Kato Y, Tsunoda Y. Effects of the culture density of mouse zygotes on the development in vitro and in vivo. Theriogenology. 1994;41(6):1315–22.
Salahuddin S, Ookutsu S, Goto K, Nakanishi Y, Nagata Y. Effects of embryo density and co-culture of unfertilized oocytes on embryonic development of in-vitro fertilized mouse embryos. Hum Reprod. 1995;10(9):2382–5.
Teruel M, Smith R. Effect of embryo density and growth factors on in vitro preimplantation development of mouse embryos. Acta Physiol Pharmacol Ther Latinoam. 1997;47(2):87–96.
Gardner DK, Lane M, Spitzer A, Batt PA. Enhanced rates of cleavage and development for sheep zygotes cultured to the blastocyst stage in vitro in the absence of serum and somatic cells: amino acids, vitamins, and culturing embryos in groups stimulate development. Biol Reprod. 1994;50(2):390–400.
Donnay I, Van Langendonckt A, Auquier P, Grisart B, Vansteenbrugge A, Massip A, Dessy F. Effects of co-culture and embryo number on the in vitro development of bovine embryos. Theriogenology. 1997;47(8):1549–61.
O’Doherty EM, Wade MG, Hill JL, Boland MP. Effects of culturing bovine oocytes either singly or in groups on development to blastocysts. Theriogenology. 1997;48(1):161–9. https://doi.org/10.1016/S0093-691X(97)00199-4; [pii]: S0093-691X(97)00199-4.
Fujita T, Umeki H, Shimura H, Kugumiya K, Shiga K. Effect of group culture and embryo-culture conditioned medium on development of bovine embryos. J Reprod Dev. 2006;52(1):137–42.
Keefer CL, Stice SL, Paprocki AM, Golueke P. In vitro culture of bovine IVM-IVF embryos: cooperative interaction among embryos and the role of growth factors. Theriogenology. 1994;41(6):1323–31.
Khurana NK, Niemann H. Effects of oocyte quality, oxygen tension, embryo density, cumulus cells and energy substrates on cleavage and morula/blastocyst formation of bovine embryos. Theriogenology. 2000;54(5):741–56. https://doi.org/10.1016/S0093-691X(00)00387-3.
Nagao Y, Iijima R, Saeki K. Interaction between embryos and culture conditions during in vitro development of bovine early embryos. Zygote. 2008;16(2):127–33. https://doi.org/10.1017/S0967199408004644.
Larson MA, Kubisch HM. The effects of group size on development and interferon-tau secretion by in-vitro fertilized and cultured bovine blastocysts. Hum Reprod. 1999;14(8):2075–9.
Reed M, Woodward B, Swain J. Single versus group culture of mammalian embryos: the verdict of the literature. J Reprod Stem Cell Biotechnol. 2011;2(2):77–87.
Moessner J, Dodson WC. The quality of human embryo growth is improved when embryos are cultured in groups rather than separately. Fertil Steril. 1995;64(5):1034–5.
Almagor M, Bejar C, Kafka I, Yaffe H. Pregnancy rates after communal growth of preimplantation human embryos in vitro. Fertil Steril. 1996;66(3):394–7.
Rebollar-Lazaro I, Matson P. The culture of human cleavage stage embryos alone or in groups: effect upon blastocyst utilization rates and implantation. Reprod Biol. 2010;10(3):227–34.
Spyropoulou I, Karamalegos C, Bolton VN. A prospective randomized study comparing the outcome of in-vitro fertilization and embryo transfer following culture of human embryos individually or in groups before embryo transfer on day 2. Hum Reprod. 1999;14(1):76–9.
Smith GD, Takayama S, Swain JE. Rethinking in vitro embryo culture: new developments in culture platforms and potential to improve assisted reproductive technologies. Biol Reprod. 2012;86(3):62. https://doi.org/10.1095/biolreprod.111.095778.
Swain JE, Smith GD. Advances in embryo culture platforms: novel approaches to improve preimplantation embryo development through modifications of the microenvironment. Hum Reprod Update. 2011;17(4):541–57. https://doi.org/10.1093/humupd/dmr006.
Vajta G, Korosi T, Du Y, Nakata K, Ieda S, Kuwayama M, Nagy ZP. The well-of-the-well system: an efficient approach to improve embryo development. Reprod Biomed Online. 2008;17(1):73–81.
Morbeck DE. Importance of supply integrity for in vitro fertilization and embryo culture. Semin Reprod Med. 2012;30(3):182–90. https://doi.org/10.1055/s-0032-1311520.
Lee BE, Boone WR, Brackelsberg PO, Carmichael RA. Development of screening systems for evaluation of materials used in mammalian embryo transfer. Theriogenology. 1988;30(3):605–12; [pii]: 0093-691X(88)90210-5.
Scott LF, Sundaram SG, Smith S. The relevance and use of mouse embryo bioassays for quality control in an assisted reproductive technology program. Fertil Steril. 1993;60(3):559–68.
Esterhuizen AD, Bosman E, Botes AD, Groenewald OA, Giesteira MV, Labuschagne GP, Lindeque HW, Rodriques FA, van Rensburg JJ, van Schouwenburg JA. A comparative study on the diagnostic sensitivity of rodent sperm and embryos in the detection of endotoxin in Earle’s balanced salt solution. J Assist Reprod Genet. 1994;11(1):38–42.
Rinehart JS, Bavister BD, Gerrity M. Quality control in the in vitro fertilization laboratory: comparison of bioassay systems for water quality. J In Vitro Fert Embryo Transf. 1988;5(6):335–42.
van den Bergh M, Baszo I, Biramane J, Bertrand E, Devreker F, Englert Y. Quality control in IVF with mouse bioassays: a four years’ experience. J Assist Reprod Genet. 1996;13(9):733–8.
Gardner DK, Reed L, Linck D, Sheehan C, Lane M. Quality control in human in vitro fertilization. Semin Reprod Med. 2005;23(4):319–24. https://doi.org/10.1055/s-2005-923389.
Punt-van der Zalm JP, Hendriks JC, Westphal JR, Kremer JA, Teerenstra S, Wetzels AM. Toxicity testing of human assisted reproduction devices using the mouse embryo assay. Reprod Biomed Online. 2009;18(4):529–35.
Morimoto Y, Hayashi E, Ohno T, Kawata A, Horikoshi Y, Kanzaki H. Quality control of human IVF/ICSI program using endotoxin measurement and sperm survival test. Hum Cell. 1997;10(4):271–6.
Fleetham JA, Pattinson HA, Mortimer D. The mouse embryo culture system: improving the sensitivity for use as a quality control assay for human in vitro fertilization. Fertil Steril. 1993;59(1):192–6.
Davidson A, Vermesh M, Lobo RA, Paulson RJ. Mouse embryo culture as quality control for human in vitro fertilization: the one-cell versus the two-cell model. Fertil Steril. 1988;49(3):516–21.
Khan Z, Wolff HS, Fredrickson JR, Walker DL, Daftary GS, Morbeck DE. Mouse strain and quality control testing: improved sensitivity of the mouse embryo assay with embryos from outbred mice. Fertil Steril. 2013;99(3):847–854.e2. https://doi.org/10.1016/j.fertnstert.2012.10.046; [pii]: S0015-0282(12)02390-4
Wolff HS, Fredrickson JR, Walker DL, Morbeck DE. Advances in quality control: mouse embryo morphokinetics are sensitive markers of in vitro stress. Hum Reprod. 2013;28(7):1776–82. https://doi.org/10.1093/humrep/det102.
Pool TB, Schoolfield J, Han D. Human embryo culture media comparisons. Methods Mol Biol. 2012;912:367–86. https://doi.org/10.1007/978-1-61779-971-6_21.
Mantikou E, Youssef MA, van Wely M, van der Veen F, Al-Inany HG, Repping S, Mastenbroek S. Embryo culture media and IVF/ICSI success rates: a systematic review. Hum Reprod Update. 2013;19(3):210–20. https://doi.org/10.1093/humupd/dms061.
Mauri AL, Petersen CG, Baruffi RL, Franco JG Jr. A prospective, randomized comparison of two commercial media for ICSI and embryo culture. J Assist Reprod Genet. 2001;18(7):378–81.
Ben-Yosef D, Amit A, Azem F, Schwartz T, Cohen T, Mei-Raz N, Carmon A, Lessing JB, Yaron Y. Prospective randomized comparison of two embryo culture systems: P1 medium by Irvine scientific and the Cook IVF medium. J Assist Reprod Genet. 2004;21(8):291–5.
Van Langendonckt A, Demylle D, Wyns C, Nisolle M, Donnez J. Comparison of G1.2/G2.2 and Sydney IVF cleavage/blastocyst sequential media for the culture of human embryos: a prospective, randomized, comparative study. Fertil Steril. 2001;76(5):1023–31.
Balaban B, Urman B. Comparison of two sequential media for culturing cleavage-stage embryos and blastocysts: embryo characteristics and clinical outcome. Reprod Biomed Online. 2005;10(4):485–91.
Zollner KP, Zollner U, Schneider M, Dietl J, Steck T. Comparison of two media for sequential culture after IVF and ICSI shows no differences in pregnancy rates: a randomized trial. Med Sci Monit. 2004;10(1):CR1–7.
Hambiliki F, Sandell P, Yaldir F, Stavreus-Evers A. A prospective randomized sibling-oocyte study of two media systems for culturing cleavage-stage embryos-impact on fertilization rate. J Assist Reprod Genet. 2011;28(4):335–41. https://doi.org/10.1007/s10815-010-9518-0.
Sifer C, Handelsman D, Grange E, Porcher R, Poncelet C, Martin-Pont B, Benzacken B, Wolf JP. An auto-controlled prospective comparison of two embryos culture media (G III series versus ISM) for IVF and ICSI treatments. J Assist Reprod Genet. 2009;26(11–12):575–81. https://doi.org/10.1007/s10815-009-9357-z.
Paternot G, Debrock S, D'Hooghe TM, Spiessens C. Early embryo development in a sequential versus single medium: a randomized study. Reprod Biol Endocrinol. 2010;8:83. https://doi.org/10.1186/1477-7827-8-83.
Sepulveda S, Garcia J, Arriaga E, Diaz J, Noriega-Portella L, Noriega-Hoces L. In vitro development and pregnancy outcomes for human embryos cultured in either a single medium or in a sequential media system. Fertil Steril. 2009;91(5):1765–70. https://doi.org/10.1016/j.fertnstert.2008.02.169.
Basile N, Morbeck D, Garcia-Velasco J, Bronet F, Meseguer M. Type of culture media does not affect embryo kinetics: a time-lapse analysis of sibling oocytes. Hum Reprod. 2013;28(3):634–41. https://doi.org/10.1093/humrep/des462.
Ciray HN, Aksoy T, Goktas C, Ozturk B, Bahceci M. Time-lapse evaluation of human embryo development in single versus sequential culture media--a sibling oocyte study. J Assist Reprod Genet. 2012;29(9):891–900. https://doi.org/10.1007/s10815-012-9818-7.
Reed ML, Hamic A, Thompson DJ, Caperton CL. Continuous uninterrupted single medium culture without medium renewal versus sequential media culture: a sibling embryo study. Fertil Steril. 2009;92(5):1783–6. https://doi.org/10.1016/j.fertnstert.2009.05.008.
Werner MD, Hong KH, Franasiak JM, Forman EJ, Reda CV, Molinaro TA, Upham KM, Scott RT Jr. Sequential versus monophasic media impact trial (SuMMIT): a paired randomized controlled trial comparing a sequential media system to a monophasic medium. Fertil Steril. 2016;105(5):1215–21. https://doi.org/10.1016/j.fertnstert.2016.01.005.
Lane M, Gardner DK. Differential regulation of mouse embryo development and viability by amino acids. J Reprod Fertil. 1997;109(1):153–64.
Lane M, Hooper K, Gardner DK. Effect of essential amino acids on mouse embryo viability and ammonium production. J Assist Reprod Genet. 2001;18(9):519–25.
Summers MC, McGinnis LK, Lawitts JA, Biggers JD. Mouse embryo development following IVF in media containing either L-glutamine or glycyl-L-glutamine. Hum Reprod. 2005;20(5):1364–71. https://doi.org/10.1093/humrep/deh756; [pii]:deh756.
Hammer MA, Kolajova M, Leveille M, Claman P, Baltz JM. Glycine transport by single human and mouse embryos. Hum Reprod. 2000;15(2):419–26.
Devreker F, Van den Bergh M, Biramane J, Winston RL, Englert Y, Hardy K. Effects of taurine on human embryo development in vitro. Hum Reprod. 1999;14(9):2350–6.
Devreker F, Winston RM, Hardy K. Glutamine improves human preimplantation development in vitro. Fertil Steril. 1998;69(2):293–9.
Lane M, Gardner DK. Ammonium induces aberrant blastocyst differentiation, metabolism, pH regulation, gene expression and subsequently alters fetal development in the mouse. Biol Reprod. 2003;69(4):1109–17. https://doi.org/10.1095/biolreprod.103.018093.
Biggers JD, McGinnis LK, Lawitts JA. Enhanced effect of glycyl-L-glutamine on mouse preimplantation embryos in vitro. Reprod Biomed Online. 2004;9(1):59–69.
Lane M. Mechanisms for managing cellular and homeostatic stress in vitro. Theriogenology. 2001;55(1):225–36.
McKiernan SH, Clayton MK, Bavister BD. Analysis of stimulatory and inhibitory amino acids for development of hamster one-cell embryos in vitro. Mol Reprod Dev. 1995;42(2):188–99. https://doi.org/10.1002/mrd.1080420208.
Virant-Klun I, Tomazevic T, Vrtacnik-Bokal E, Vogler A, Krsnik M, Meden-Vrtovec H. Increased ammonium in culture medium reduces the development of human embryos to the blastocyst stage. Fertil Steril. 2006;85(2):526–8. https://doi.org/10.1016/j.fertnstert.2005.10.018.
Zhu J, Li M, Chen L, Liu P, Qiao J. The protein source in embryo culture media influences birthweight: a comparative study between G1 v5 and G1-PLUS v5. Hum Reprod. 2014;29(7):1387–92. https://doi.org/10.1093/humrep/deu103.
Leonard PH, Charlesworth MC, Benson L, Walker DL, Fredrickson JR, Morbeck DE. Variability in protein quality used for embryo culture: embryotoxicity of the stabilizer octanoic acid. Fertil Steril. 2013;100(2):544–9. https://doi.org/10.1016/j.fertnstert.2013.03.034.
Morbeck DE, Paczkowski M, Fredrickson JR, Krisher RL, Hoff HS, Baumann NA, Moyer T, Matern D. Composition of protein supplements used for human embryo culture. J Assist Reprod Genet. 2014;31(12):1703–11. https://doi.org/10.1007/s10815-014-0349-2.
Meintjes M. Media composition: macromolecules and embryo growth. Methods Mol Biol. 2012;912:107–27. https://doi.org/10.1007/978-1-61779-971-6_8.
Dyrlund TF, Kirkegaard K, Poulsen ET, Sanggaard KW, Hindkjaer JJ, Kjems J, Enghild JJ, Ingerslev HJ. Unconditioned commercial embryo culture media contain a large variety of non-declared proteins: a comprehensive proteomics analysis. Hum Reprod. 2014;29(11):2421–30. https://doi.org/10.1093/humrep/deu220.
Borini A, Bulletti C, Cattoli M, Serrao L, Polli V, Alfieri S, Flamigni C. Use of recombinant leukemia inhibitory factor in embryo implantation. Ann N Y Acad Sci. 1997;828:157–61.
Sjoblom C, Wikland M, Robertson SA. Granulocyte-macrophage colony-stimulating factor promotes human blastocyst development in vitro. Hum Reprod. 1999;14(12):3069–76.
O’Neill C, Ryan JP, Collier M, Saunders DM, Ammit AJ, Pike IL. Supplementation of in-vitro fertilisation culture medium with platelet activating factor. Lancet. 1989;2(8666):769–72.
Hegde A, Behr B. Media composition: growth factors. Methods Mol Biol. 2012;912:177–98. https://doi.org/10.1007/978-1-61779-971-6_11.
Weathersbee PS, Pool TB, Ord T. Synthetic serum substitute (SSS): a globulin-enriched protein supplement for human embryo culture. J Assist Reprod Genet. 1995;12(6):354–60.
Pool TB, Martin JE. High continuing pregnancy rates after in vitro fertilization-embryo transfer using medium supplemented with a plasma protein fraction containing alpha- and beta-globulins. Fertil Steril. 1994;61(4):714–9.
Schneider EG, Hayslip CC. Globulin-enriched protein supplements shorten the pre-compaction mitotic interval and promote hatching of murine embryos. Am J Reprod Immunol. 1996;36(2):101–6.
Desai NN, Sheean LA, Martin D, Gindlesperger V, Austin CM, Lisbonna H, Peskin B, Goldfarb JM. Clinical experience with synthetic serum substitute as a protein supplement in IVF culture media: a retrospective study. J Assist Reprod Genet. 1996;13(1):23–31.
Tucker KE, Hurst BS, Guadagnoli S, Dymecki C, Mendelsberg B, Awoniyi CA, Schlaff WD. Evaluation of synthetic serum substitute versus serum as protein supplementation for mouse and human embryo culture. J Assist Reprod Genet. 1996;13(1):32–7.
Meintjes M, Chantilis SJ, Ward DC, Douglas JD, Rodriguez AJ, Guerami AR, Bookout DM, Barnett BD, Madden JD. A randomized controlled study of human serum albumin and serum substitute supplement as protein supplements for IVF culture and the effect on live birth rates. Hum Reprod. 2009;24(4):782–9. https://doi.org/10.1093/humrep/den396; [pii]: den396.
Bungum M, Humaidan P, Bungum L. Recombinant human albumin as protein source in culture media used for IVF: a prospective randomized study. Reprod Biomed Online. 2002;4(3):233–6.
Ben-Yosef D, Yovel I, Schwartz T, Azem F, Lessing JB, Amit A. Increasing synthetic serum substitute (SSS) concentrations in P1 glucose/phosphate-free medium improves implantation rate: a comparative study. J Assist Reprod Genet. 2001;18(11):588–92.
Morbeck DE, Khan Z, Barnidge DR, Walker DL. Washing mineral oil reduces contaminants and embryotoxicity. Fertil Steril. 2010;94(7):2747–52. https://doi.org/10.1016/j.fertnstert.2010.03.067; [pii]: S0015-0282(10)00528-5.
Otsuki J, Nagai Y, Chiba K. Damage of embryo development caused by peroxidized mineral oil and its association with albumin in culture. Fertil Steril. 2009;91(5):1745–9. https://doi.org/10.1016/j.fertnstert.2008.03.001.
Otsuki J, Nagai Y, Chiba K. Peroxidation of mineral oil used in droplet culture is detrimental to fertilization and embryo development. Fertil Steril. 2007;88(3):741–3. https://doi.org/10.1016/j.fertnstert.2006.11.144.
Hughes PM, Morbeck DE, Hudson SB, Fredrickson JR, Walker DL, Coddington CC. Peroxides in mineral oil used for in vitro fertilization: defining limits of standard quality control assays. J Assist Reprod Genet. 2010;27(2–3):87–92. https://doi.org/10.1007/s10815-009-9383-x.
Chen M, Wei S, Hu J, Yuan J, Liu F. Does time-lapse imaging have favorable results for embryo incubation and selection compared with conventional methods in clinical in vitro fertilization? A meta-analysis and systematic review of randomized controlled trials. PLoS One. 2017;12(6):e0178720. https://doi.org/10.1371/journal.pone.0178720.
Kaser DJ, Racowsky C. Clinical outcomes following selection of human preimplantation embryos with time-lapse monitoring: a systematic review. Hum Reprod Update. 2014;20(5):617–31. https://doi.org/10.1093/humupd/dmu023.
Goodman LR, Goldberg J, Falcone T, Austin C, Desai N. Does the addition of time-lapse morphokinetics in the selection of embryos for transfer improve pregnancy rates? A randomized controlled trial. Fertil Steril. 2016;105(2):275–85. e210. https://doi.org/10.1016/j.fertnstert.2015.10.013.
Kaser DJ, Bormann CL, Missmer SA, Farland LV, Ginsburg ES, Racowsky C. A pilot randomized controlled trial of day 3 single embryo transfer with adjunctive time lapse selection versus day 5 single embryo transfer with or without adjunctive time lapse selection. Hum Reprod. 2017;32(8):1598–603.
Meseguer M, Rubio I, Cruz M, Basile N, Marcos J, Requena A. Embryo incubation and selection in a time-lapse monitoring system improves pregnancy outcome compared with a standard incubator: a retrospective cohort study. Fertil Steril. 2012;98(6):1481–9. e1410. https://doi.org/10.1016/j.fertnstert.2012.08.016.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Swain, J.E. (2018). Is There an Optimum System for Culturing Human Embryos?. In: Carrell, D., Racowsky, C., Schlegel, P., DeCherney, A. (eds) Emerging Topics in Reproduction. Springer, Cham. https://doi.org/10.1007/978-3-319-90823-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-90823-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-90822-9
Online ISBN: 978-3-319-90823-6
eBook Packages: MedicineMedicine (R0)