Abstract
Fibrostenotic inflammatory bowel disease classically refers to Crohn’s disease, where stricture and submucosal fibrosis are frequent and defining histopathologic features. Descriptions of histologic fibrosis in ulcerative colitis have existed for over half a century, but are not currently part of the clinical diagnostic framework. Histologic scoring systems for fibrosis in inflammatory bowel disease are varied and highlight the need for improved histopathologic correlation, given recent advances in our understanding of the pathophysiology of intestinal fibrosis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Fibrosis
- Histopathology
- Muscularis mucosae
- Submucosa
- Stricture
- Inflammatory bowel disease
- Histologic fibrosis score
11.1 Histopathology of Fibrosis in Crohn’s Disease
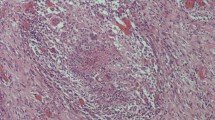
Submucosal fibrosis is a pathologic hallmark of Crohn’s disease. Normal submucosal collagen and adipose tissue are replaced by fibrous tissue which contracts the submucosal area (Fig. 11.1). Strictures are areas of marked submucosal fibrosis, along with hyperplasia of the muscularis mucosae, which can become so thick as to obliterate the submucosa [1] (Fig. 11.2). Expansion of the muscularis mucosae, including hyperplasia, architectural disarray, and collagen deposition, accounts for about half of the increased wall thickness of an ileal stricture in Crohn’s disease [2]. Strictures also often contain hypertrophic nerves (Fig. 11.3). Submucosal arteries and veins often have fibromuscular hyperplasia in strictured areas [2] (Fig. 11.4). Deeper in the bowel wall, muscularis propria hypertrophy can be seen, and along with disorganization and fibrosis, leads to an overall thickened muscularis propria, although this feature is not a diagnostic hallmark [3]. On gross examination, creeping fat or fat wrapping, is a common finding and a major pathologic feature, characterized by fat extending along the antimesenteric border.
It is not known whether hyperplasia of the muscularis mucosae and nerves occur as a result of a prolific response following ulcerating injury (i.e. aberrant wound healing [4]) or if they develop in response to other factors, such as mesenchymal growth factors, related to inflammation or gut bacteria; although a combination of these factors is most likely involved [5,6,7]. For example, intestinal fibroblasts express Toll-like receptor-4, which is acted upon by bacterial lipopolysaccharide (LPS) to activate a nuclear factor kappa B pathway, resulting in collagen contraction [7]. LPS also enhances connective tissue growth factor expression by decreasing expression of the transforming growth factor-beta inhibitor, smad-7 [7]. Other TLRs, including TLR-9, as well as chemokines, such as CXCL8, and cytokines also play a role in mesenchymal-bacterial interactions at the molecular level [6].
11.2 Histopathology of Fibrosis in Ulcerative Colitis
Standard descriptions used in diagnostic pathology do not include fibrosis as a histologic feature of ulcerative colitis. Furthermore, as ulcerative colitis is defined as having pathologic features restricted to the mucosa and superficial submucosa, the presence of a stricture in UC is immediately concerning for an infiltrative carcinoma, rather than a benign process. Looking to the published literature, however, 71% to 100% of all clinically detected strictures in UC patients were benign [8,9,10]. The risk of a stricture being due to malignancy is associated with longer duration of disease and location of the stricture, with rectal strictures being more common (68%), and therefore more often benign (90%), and strictures of the right colon being malignant 87–100% of the time [8, 11].
Histologic studies of benign strictures in UC have of necessity been performed on resection specimens. Goulston et al. compared the thickness of the muscularis mucosae and inner layer of muscularis propria in benign strictured and non-strictured UC areas, and found 40-fold and 20-fold thickening, respectively, as compared to non-strictured UC controls; concluding that fibrosis alone was insufficient to explain the stricture [11]. Other studies have described fibrosis along with muscular hypertrophy, including marked submucosal fibrosis in 20 of 28 benign UC strictures [12]. Microscopic examination of benign UC strictures has also revealed expansion of the submucosa by fat, which may be a factor contributing to luminal narrowing [13].
Descriptions of fibrosis in UC outside of the presence of strictures is also lacking [14]. In a study of UC proctocolectomy resections with dysplasia in an American center as compared to a Japanese center, lamina propria fibrosis in non-dysplastic areas was more prominent in American cases as compared to Japanese cases [15]. Interestingly, in control cases without dysplasia, there was no difference in lamina propria fibrosis in the two populations [15]. The authors suggested longer disease duration in the American group and differences in medications as possible explanations for the findings [15]. One very early study from 1949 describes fibrosis in the wall of UC resections in the context of extensive ulceration [16]. This concept was also discussed in the 1950s and 1960s by Lumb et al. [17, 18]. Indeed, in the wound repair process after epithelial injury, including gut epithelial injury, it is generally accepted that fibrosis is part of the post-inflammatory organization of granulation tissue [19, 20].
We described histologic patterns of lamina propria fibrosis and muscularis mucosae alterations in non-strictured UC resections, and found these histologic features to be correlated with prior medication use and inflammatory activity [21]. The most striking pattern of lamina propria fibrosis is a band of fibrosis between the base of the crypts and the muscularis mucosae, essentially replacing the more typical basal lymphoplasmacytosis (Fig. 11.5). Similar to other studies finding alterations and thickening of the muscularis mucosae in UC, we have also seen altered muscularis mucosae with patterns of splaying, usually with interspersed fibrosis (Fig. 11.6), as well as thickening of the muscularis mucosae, and finally splitting and even duplication of the inner and outer layers of muscularis mucosae (Fig. 11.7).
Muscularis mucosae alterations in ulcerative colitis. In these two cases of ulcerative colitis with mucosal healing, contrast the thin and nearly intact muscularis mucosae with splayed muscularis hyperplasia within the superficial submucosa (Top), with the thickened muscularis mucosae with duplication on the mucosal aspect (Bottom). [black bar demarcates the original two layers of muscularis mucosae, black star indicates the alteration] (Masson Trichrome, original magnification 4×)
Regarding submucosal fibrosis in non-strictured UC resections, we observe this phenomenon in ulcerated areas (Fig. 11.8) as well as in non-ulcerated areas. In non-ulcerated areas, fibrous bands within the submucosa typically form adjacent to the muscularis mucosae and muscularis propria and are otherwise perpendicular to the luminal flow (Fig. 11.9). Submucosal fibrosis can be identified in diagnostic H&E stained sections without the aid of a trichrome stain, and the degree of submucosal fibrosis is associated with the severity of intestinal inflammation [22]. Apart from fibrosis associated with deep mucosal ulceration in fulminant disease, significant changes in the muscularis propria are not typically seen.
11.3 Pathology Fibrosis Scoring Systems in Inflammatory Bowel Disease
Fibrosis scoring systems in inflammatory bowel disease are typically based on imaging and biomarkers [23]. Histologic scoring of fibrosis in Crohn’s disease originated from studies in rodents [24, 25], as well as human studies comparing radiographic findings with resection specimen findings [26,27,28,29], and early studies examining resection specimen margins to determine factors associated with recurrent disease [30, 31].
The earlier rat scoring system by Theiss et al. (Table 11.1) is progressive and cumulative, and is based on evaluation of sections stained with Masson trichrome and Sirius red [24]. Progression starts from submucosal collagen deposition (score 1), and adds on mucosal collagen deposition (score 2), muscularis mucosae collagen deposition and disorganization (score 3), muscularis propria collagen deposition (score 4), and finally all layers including serosa (score 5). Interestingly, there is also consideration of the percent of the section involved by fibrosis (Table 11.1), an important consideration given the segmental, and microscopically patchy, nature of Crohn’s disease. The more recent mouse scoring system by Higgins et al. (Table 11.2) utilizes a progressive score considering only fibrosis (collagen deposition) affecting the mucosa and submucosa on Masson trichrome stained sections, with four tiers, from no fibrosis (score 0) to severe fibrosis (score 3). This scoring system is much less detailed than the earlier one, and has also been used on human tissue comparing fibrosis on pathology to ex vivo ultrasound evaluation in patients with inflammatory bowel disease [29].
Histologic scoring of fibrosis in studies comparing to radiographic findings are also somewhat less detailed, and do not include the percent section involvement, presumably due to examining only strictured segments. These studies use human tissue with Hematoxylin & Eosin stained sections. Adler et al. [26] separates fibrosis grade from muscle thickness, specifically thickening of the muscularis propria (Table 11.3). Unlike the earlier rodent scoring systems described above, this scoring does not recognize mucosal fibrosis, or muscularis mucosae fibrosis or hyperplasia. Fibrosis is scored progressively, but considers submucosa, muscularis propria, and subserosa in each grade (Table 11.3). Chiorean et al. [28] takes a simplified approach with fewer score options in a three-tiered system (Table 11.4). Focus is again on submucosal fibrosis and on muscularis hyperplasia, though it is not specified whether this is referring to muscularis mucosae or muscularis propria.
Scoring schema from studies looking at resection specimen margins are probably the most generally applicable, as they consider pathologic features of Crohn’s disease generally, not just findings from a stricture. Fibrosis of muscularis mucosae and submucosa are the focus, without specific mention of mucosa, muscularis propria, or subserosa, and a three-tiered progressive intensity grade was used [30, 31]. Interestingly, Maconi et al. [27] applied this scoring system, slightly modified to include four-tiers, to a group of Crohn’s patients resected for ileal stenosis (stricture), where representative sections along the entire resected segment length were analyzed, and correlated the histologic findings with ultrasound echo patterns.
Neither the mouse nor the human scoring systems described here have been validated. As fibrosis in Crohn’s disease is not generally thought to progress from lumen to serosa, a scoring system that accounts for all layers of the bowel wall simultaneously is preferred. A similar scoring system should be applicable to both mice and human studies. The ideal Crohn’s fibrosis scoring system would account for changes in the muscularis mucosae, including both hyperplasia and fibrosis, submucosal fibrosis and muscularization, muscularis propria hyperplasia and fibrosis, and subserosal fibrosis. A four-tiered scoring system (e.g. none, mild, moderate, severe) applied to each site (i.e. mucosa, muscularis mucosae, submucosa, muscularis propria, and subserosa) would be ideal, at least in early studies until clinical correlation could be established, and then perhaps the score could be contracted into three tiers. As Crohn’s disease is patchy, multiple sections per specimen should be assessed, and a unified “per specimen” score could also be generated. Again, clinical correlation studies would be needed to best understand whether the unified score would reflect the highest overall score, or a combination of the scores from each section examined.
As the recognition and understanding of fibrosis in ulcerative colitis lags behind that of Crohn’s disease, so does the concept of fibrosis scoring schema for ulcerative colitis. Measurement of the bowel wall layers has revealed muscularis mucosae thickening in ulcerative colitis [22], as well as increased fibronectin and collagen I in the mucosa, increased collagen I in the muscularis mucosae, and increased collagen I and III in the muscularis propria [32].
We developed a histologic fibrosis burden score for ulcerative colitis with a three-tiered approach focusing on the percent of submucosal fibrosis, and found moderate interobserver agreement on Hematoxylin & Eosin stained sections, and significant correlation when compared to Masson trichrome stain and Sirius red stain [22]. Bowel wall layer measurements revealed thickening of the muscularis mucosae, and this correlated with the presence of chronic mucosal injury [22].
11.4 Conclusion
In summary, fibrosis is a defining histopathologic feature of Crohn’s disease. A variety of histologic scoring systems have been developed to evaluate fibrosis of inflammatory bowel disease, with a focus on Crohn’s disease. In ulcerative colitis, recognition of histologic fibrosis has not been part of the diagnostic cadre, but has certainly been recognized and described in the literature. More studies evaluating the clinicopathologic correlation of fibrosis in ulcerative colitis are needed. Current histologic scoring systems reveal a variety of definitions of fibrosis and are incongruent as to the importance of fibrosis and mesenchymal cell hyperplasia in each of the bowel wall layers. Perhaps a unified histologic fibrosis scoring system, which can account for Crohn’s disease, ulcerative colitis, strictured and non-strictured areas, and which incorporates the current understanding of the pathophysiology of fibrosis in inflammatory bowel disease, would be needed before widespread use could be established for clinical trials.
References
Koukoulis G, Ke Y, Henley JD, Cummings OW. Obliterative muscularization of the small bowel submucosa in Crohn disease: a possible mechanism of small bowel obstruction. Arch Pathol Lab Med. 2001;125(10):1331–4.
Zhang X, Ko H-BM, Cai Z, Zhu H, Polydorides AD, Torres J, et al. Fibromuscular strictures in Ileal Crohn’s disease: a detailed morphometric and Histopathologic analysis. Mod Pathol. 2017;30(S2):209A–10A.
Burke JP, Mulsow JJ, O’Keane C, Docherty NG, Watson RW, O’Connell PR. Fibrogenesis in Crohn’s disease. Am J Gastroenterol. 2007;102(2):439–48.
Rieder F, Brenmoehl J, Leeb S, Scholmerich J, Rogler G. Wound healing and fibrosis in intestinal disease. Gut. 2007;56(1):130–9.
Rieder F, Fiocchi C. Intestinal fibrosis in IBD—a dynamic, multifactorial process. Nature Rev. 2009;6(4):228–35.
Scales BS, Huffnagle GB. The microbiome in wound repair and tissue fibrosis. J Pathol. 2013;229(2):323–31.
Burke JP, Cunningham MF, Watson RW, Docherty NG, Coffey JC, O’Connell PR. Bacterial lipopolysaccharide promotes profibrotic activation of intestinal fibroblasts. Br J Surg. 2010;97(7):1126–34.
Gumaste V, Sachar DB, Greenstein AJ. Benign and malignant colorectal strictures in ulcerative colitis. Gut. 1992;33(7):938–41.
De Dombal FT, Watts JM, Watkinson G, Goligher JC. Local complications of ulcerative colitis: stricture, pseudopolyposis, and carcinoma of colon and rectum. Br Med J. 1966;1(5501):1442–7.
Hunt RH, Teague RH, Swarbrick ET, Williams CB. Colonoscopy in management of colonic strictures. Br Med J. 1975;3(5979):360–1.
Goulston SJ, McGovern VJ. The nature of benign strictures in ulcerative colitis. N Engl J Med. 1969;281(6):290–5.
Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1964;5:1–22.
Gore RM. Colonic contour changes in chronic ulcerative colitis: reappraisal of some old concepts. AJR Am J Roentgenol. 1992;158(1):59–61.
Gordon IO, Agrawal N, Goldblum JR, Fiocchi C, Rieder F. Fibrosis in ulcerative colitis: mechanisms, features, and consequences of a neglected problem. Inflamm Bowel Dis. 2014;20(11):2198–206.
Mitomi H, Okayasu I, Bronner MP, Kanazawa H, Nishiyama Y, Otani Y, et al. Comparative histologic assessment of proctocolectomy specimens from Japanese and American patients with ulcerative colitis with or without dysplasia. Int J Surg Pathol. 2005;13(3):259–65.
Warren S, Sommers SC. Pathogenesis of ulcerative colitis. Am J Pathol. 1949;25(4):657–79.
Lumb G. Pathology of ulcerative colitis. Gastroenterology. 1961;40:290–8.
Lumb G, Protheroe RH. Ulcerative colitis; a pathologic study of 152 surgical specimens. Gastroenterology. 1958;34(3):381–407.
Jones MK, Tomikawa M, Mohajer B, Tarnawski AS. Gastrointestinal mucosal regeneration: role of growth factors. Front Biosci. 1999;4:D303–9.
Dammeier J, Brauchle M, Falk W, Grotendorst GR, Werner S. Connective tissue growth factor: a novel regulator of mucosal repair and fibrosis in inflammatory bowel disease? Int J Biochem Cell Biol. 1998;30(8):909–22.
Willis E, Lopez R, Agrawal N, Rieder F, Gordon I. Alterations in lamina propria and muscularis mucosa in ulcerative colitis are associated with prior medication and degree of histologic inflammatory activity. Mod Pathol. 2017;30(S2):206A.
Gordon IO, Agrawal N, Willis E, Goldblum JR, Lopez R, Allende D, Liu X, Patil DY, Yerian L, El-Khider F, Fiocchi C, Rieder F. Fibrosis in ulcerative colitis is directly linked to severity and chronicity of mucosal inflammation. Aliment Pharmacol Ther. 2018;47(7):922–39.
Higgins PD. Measurement of fibrosis in Crohn’s disease strictures with imaging and blood biomarkers to inform clinical decisions. Dig Dis. 2017;35(1–2):32–7.
Theiss AL, Fuller CR, Simmons JG, Liu B, Sartor RB, Lund PK. Growth hormone reduces the severity of fibrosis associated with chronic intestinal inflammation. Gastroenterology. 2005;129(1):204–19.
Higgins PD, Johnson LA, Sauder K, Moons D, Blanco L, Taube S, et al. Transient or persistent norovirus infection does not alter the pathology of salmonella typhimurium induced intestinal inflammation and fibrosis in mice. Comp Immunol Microbiol Infect Dis. 2011;34(3):247–57.
Adler J, Punglia DR, Dillman JR, Polydorides AD, Dave M, Al-Hawary MM, et al. Computed tomography enterography findings correlate with tissue inflammation, not fibrosis in resected small bowel Crohn’s disease. Inflamm Bowel Dis. 2012;18(5):849–56.
Maconi G, Carsana L, Fociani P, Sampietro GM, Ardizzone S, Cristaldi M, et al. Small bowel stenosis in Crohn’s disease: clinical, biochemical and ultrasonographic evaluation of histological features. Aliment Pharmacol Ther. 2003;18(7):749–56.
Chiorean MV, Sandrasegaran K, Saxena R, Maglinte DD, Nakeeb A, Johnson CS. Correlation of CT enteroclysis with surgical pathology in Crohn’s disease. Am J Gastroenterol. 2007;102(11):2541–50.
Dillman JR, Stidham RW, Higgins PD, Moons DS, Johnson LA, Keshavarzi NR, et al. Ultrasound shear wave elastography helps discriminate low-grade from high-grade bowel wall fibrosis in ex vivo human intestinal specimens. J Ultrasound Med. 2014;33(12):2115–23.
Fazio VW, Marchetti F, Church M, Goldblum JR, Lavery C, Hull TL, et al. Effect of resection margins on the recurrence of Crohn’s disease in the small bowel. A randomized controlled trial. Ann Surg. 1996;224(4):563–71. Discussion 71–3.
Kotanagi H, Kramer K, Fazio VW, Petras RE. Do microscopic abnormalities at resection margins correlate with increased anastomotic recurrence in Crohn’s disease? Retrospective analysis of 100 cases. Dis Colon Rectum. 1991;34(10):909–16.
de Bruyn JR, Meijer SL, Wildenberg ME, Bemelman WA, van den Brink GR, D’Haens GR. Development of fibrosis in acute and longstanding ulcerative colitis. J Crohns Colitis. 2015;9(11):966–72.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Gordon, I.O. (2018). Histopathology of Intestinal Fibrosis. In: Rieder, F. (eds) Fibrostenotic Inflammatory Bowel Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-90578-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-90578-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-90577-8
Online ISBN: 978-3-319-90578-5
eBook Packages: MedicineMedicine (R0)