Abstract
Heat shock protein (HSP) 70 has been investigated from various aspects in experimental studies, since it is the most abundant form of HSP in cells. HSP 70 is involved in response to various acute and chronic insults of kidney and also other parts of the urinary tract. Although it is not a specific biomarker for any of the kidney diseases, HSP 70 level of body fluids may be beneficial as a biomarker in some specific circumstances, for example for the differential diagnosis of “a children with fever”. The number of possible diseases in this situation is limited and an infection is most likely to be the reason of fever. Additionally, clarifying the exact role of HSP 70 in different kidney diseases enables to discover new therapeutic options in order to prevent renal fibrosis and chronic renal failure in the future. This chapter reviews experimental and clinical studies to find out the opportunities to utilize HSP 70 in daily clinical practice.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Heat shock proteins (HSP) are intracellular chaperones which are classified according to their molecular weight such as small HSP (16–40 kDa), HSP60 (60 kDa), HSP70 (70 kDa), HSP90 (90 kDa) (Beck et al. 2000; Musial and Zwolinska 2011). The main function of these chaperones is contributing to maintain cell survival by restoring proteins in cells (Beck et al. 2000). HSP are involved in correct folding of proteins, refolding of misfolded proteins and degradation of irrecoverable proteins to protect structure of cytoskeleton (Beck et al. 2000; Musial and Zwolinska 2011; Barutta et al. 2008; Buraczynska et al. 2009). They are expressed under normal conditions and can be induced by various stressors including thermal, osmotic, oxidative, toxic, ischemic injury (Beck et al. 2000; Mueller et al. 2003; O’Neill et al. 2014). Heat shock protein (HSP) 70 is a member of HSP protein families which is the most abundant form of HSP in cells (Beck et al. 2000). Hence, HSP 70 has been investigated from various aspects in experimental studies. HSP 70 usually acts as a protective part of the inflammatory and immune response in case of tissue damage (Manucha 2014). It has been demonstrated that HSP 70 contributes to development, infection, inflammation, apoptosis and fibrosis of kidney (Mazzei and Manucha 2017; Manucha 2014; Kennedy et al. 2014; Zhou et al. 2016). Based on these studies which are mostly experimental, our goal for the future should be to benefit from HSP 70 in favor of patients in our daily practice. One of the best ways to achieve this goal may be to use HSP 70 as a biomarker to diagnose kidney diseases. First of all, HSP 70 must be detectable in body fluids to be utilized as a biomarker, since blood, urine and the other body fluids have been employed to detect the presence of diagnostic biomarkers in practice.
Acute Kidney Diseases and HSP 70
Although HSP 70 is mostly considered to be an intracellular chaperone, several clinical studies have demonstrated that it might be found in extracellular space, serum and urine of human (Mambula et al. 2007). HSP 72, a member of HSP 70 protein family, has been shown to be elevated in body fluids secondary to bacterial infections (Tang et al. 2008; Varano Della Vergiliana et al. 2013). Tang et al (2008) evaluated level of HSP 72 in cerebrospinal fluid (CSF) of the patients who underwent lumbar puncture due to the suspicion of meningitis. They reported that HSP72 level in CSF of patients with meningitis was significantly higher than in the patients without meningitis according to assessment of CSF (Tang et al. 2008). Moreover, HSP 72 level was found to be higher in bacterial meningitis than in aseptic meningitis (Tang et al. 2008). Similarly, another study showed that level of HSP 72 was significantly increased in exudates than in transudates in the patients with pleural effusion (Varano Della Vergiliana et al. 2013). The authors claimed that the reason of increased HSP 72 was the stimulation of mesothelial cells by the pneumococcal products (Varano Della Vergiliana et al. 2013). Likewise, cell culture studies demonstrated that HSP 70 released from macrophages due to exposure of bacterial products of Escherichia coli which was the most common causative microorganism in urinary tract infection (UTI) (Davies et al. 2006). The prevailing opinion in the past was that HSP 70 was released to extracellular space due to the cell death. However, it has been shown that HSP 70 is secreted by kidney cells actively rather than because of cell death (Evdokimovskaya et al. 2010). Molinas et al (2010) reported that HSP 70 levels increased in urine and in renal cortex simultaneously in rats after receiving Acetaminophen which caused renal toxicity. This finding suggest not only that nephrotoxic agents stimulate HSP 70 expression in renal cortex but also that urine may be a good indicator of HSP 70 expression in kidney related to renal injury. All these evidences imply that urine level of HSP 70 may be an indicator for infection in the urinary tract.
Urinary tract infection is one of the most common infections in children and should be included in the differential diagnosis of children with the symptoms of systemic infections (Roberts 2011). Nowadays, UTI is diagnosed with significant bacterial growing in urine culture and positive of leukocyte esterase and/or nitrite tests in urinalysis. However, urinalysis is not specific for the UTI. There are some limitations of urine culture as well, although it is essential for the diagnosis. First, three days are required for identifying the bacterial growth in culture. Second, invasive methods are required to obtain sterile urine sample for culture because urine may be contaminated by microorganisms which are originated outside of the urinary tract. A reliable biomarker is needed to distinguish UTI from contamination as well as other infections for the accurate diagnosis. Therefore, we evaluated urine level of HSP 70 (uHSP70) and urine HSP 70/creatinine ratio (uHSP70/Cr) to determine whether these parameters could indicate UTI in children. In this study, both uHSP70 and uHSP70/Cr were found to be elevated in patients with UTI at the onset of the infection and they decreased after antibiotic treatment proving that the elevation of HSP 70 in urine was secondary to UTI (Yilmaz et al. 2016a, b). Additionally, our results demonstrated that both these parameters were higher in the patients with UTI than in the contamination and non-UTI infection group including upper and lower respiratory tract infection, gastroenteritis etc. (Fig. 1) (Yilmaz et al. 2016a, b). All these findings demonstrated that increase of these parameters may help to distinguish UTI from not only the other infections but also bacterial contamination of the urine.
The possibility of having UTI is increased in children with unexplained fever when uHSP70/Cr is above a cut-off 158 pg/mgCr in the study. Urine HSP70/Cr has 100% sensitivity and specificity using this cut-off value to distinguish UTI from other infections. As an alternative, urinalysis has lower sensitivity and specificity (Yilmaz et al. 2016a, b). Previous reports showed that either leucocyte esterase or nitrite positivity has a sensitivity of 88% and a specificity of 79% (Williams et al. 2010). These promising results of our study suggest that urine level of HSP 70, especially uHSP70/Cr, may be used as a reliable biomarker in UTI in children.
HSP 70 in urine can be originated not only from kidney but also from bladder. Urine HSP 70 level was found to be increased in bladder cancer and the authors concluded that this increase might be related to HSP 70 secretion from the tumor cells to urine (Margel et al. 2011). However, uHSP70/Cr was significantly higher in pyelonephritis than in cystitis in our study implying that the reaction against the infection was stronger when the kidney was involved rather than the bladder only. Our study showed that bacterial infection of the urinary tract as an acute insult may give rise to increase of HSP 70 in urine. It has been notified that HSP 70 is a part of the response to tissue damage due to various acute conditions causing kidney injury. Studies that investigate the role of HSP70/72 in acute kidney injury (AKI) have intensified on ischemia-reperfusion models. Ischemia-reperfusion injury results from decreasing of oxygen supply of the kidney tissue due to reduction of blood flow, and subsequently sudden restoration of the blood flow to the kidney tissue. Ischemia and thereafter reperfusion cause to increase of reactive oxygen species (ROS), apoptotic molecules, necrosis, inflammatory cells (Friedewald and Rabb 2004). These cellular responses finally lead to tissue injury (Friedewald and Rabb 2004). Cellular ATP decreases after renal ischemia and HSP70 expression is induced when the ATP reduction reaches 35–50% (van Why et al. 1994, 1999).
Acute kidney injury results from an ischemic or toxic incident. Amongst kidney cells, renal tubular cells are the most vulnerable to AKI. Renal tubule cells loss their structural integrity and polarity in AKI and regain their functions through remodeling (Molitoris 1991). Primary mechanism of cellular repair is recycling of damaged proteins following ATP depletion (Molitoris et al. 1996). HSP 70, as an important chaperon, participates in restoring of damaged proteins (Mayer 2013). Detachment of Na-K-ATPase from the cytoskeleton causes loss of tubule polarity in ischemic renal injury (Riordan et al. 2005). HSP 70 binds to Na-K-ATPase and overexpression of HSP 70 reduces of detachment of Na-K-ATPase (Riordan et al. 2005). Binding of HSP70 to Na-K-ATPase increases in response to injury and decreases during recovery period (Riordan et al. 2005).
Besides, it has been reported that HSP 70 has various effects in AKI. Geranylgeranylacetone (GGA), an HSP 70 inducer, prevents morphine induced renal damage by inhibition of caspase-3 and caspase-9 (Luo et al. 2013). Also, HSP 70 reduces apoptosis in AKI inhibiting the c-Jun N-terminal kinase phosphorylation as well as caspase-3 inhibition (Kim et al. 2009). Overexpression of HSP 72 activates MEK/ERK signaling pathway via phosphorylation and provides cell survival form nephrotoxic injury (Wang et al. 2009). Expression or activation of Ste20-like kinase (SLK) activates HSP 70 induction (Cybulsky et al. 2016). Expression of HSP 70 mitigates SLK associated apoptosis. Conversely, inhibition of HSP 70 enhances the pro-apoptotic activity of SLK (Cybulsky et al. 2016). Selective COX2 inhibitors reduce papillary HSP 70 induction which is associated with caspase-3 activity and apoptotic cells (Neuhofer et al. 2004).
Mueller T et al. evaluated urine HSP 72 in rat with exposure heat and ischemia, and also first urine after the renal transplantation in six pediatric renal allograft recipients (Mueller et al. 2003). They reported that renal HSP 72 expression was stimulated both by renal ischemia or hyperthermia in rats, whereas only renal ischemia led to HSP 72 excretion into urine (Mueller et al. 2003). Urine HSP 72 is detectable in the first urine after renal transplantation and presence of HSP 72 in urine continues during the first 12 h following renal transplantation (Mueller et al. 2003). In another study, it has been demonstrated that both renal HSP 72 mRNA and urine HSP 72 level increase gradually in rats as renal ischemia is prolonged (Barrera-Chimal et al. 2011). Moreover, 9 patients with AKI were evaluated in the same study and increased urine HSP 72 was observed in clinical AKI before serum creatinine elevation (Barrera-Chimal et al. 2011). The authors concluded that urinary HSP 72 was a useful biomarker for detection of AKI before fulfilled of AKI criteria (Barrera-Chimal et al. 2011). Another study of the same group compared urine HSP 72 levels of 17 patients with AKI and 20 controls (Morales-Buenrostro et al. 2014). Urine HSP 72 levels remained stable at the level of 0.3 ng/ml in the patients without AKI, while they progressively increase before development of AKI beginning from -3. day and reach a level of up to 15fold higher in patients with AKI (Morales-Buenrostro et al. 2014). Sensitivity and specificity of urine HSP 72 levels were 100% and 83.3%, respectively, using the cut-off value as 1 ng/ml at -1. day (Morales-Buenrostro et al. 2014). Moreover, increase of HSP 72 was earlier than other markers including neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule type 1 (KIM-1) and interleukin 18 (IL-18) (Morales-Buenrostro et al. 2014). Upregulation of HSP72 by renal ischemia is only seen in renal cortex, although it does not occur in renal medulla or in other tissues such as brain, liver, intestine, lung and heart (Ortega-Trejo et al. 2015). Urinary HSP 72 level is constant at room temperature for 48 h and remains stable at -80 C storage for 9 months, also is not affected by several freeze/thaw cycles (Ortega-Trejo et al. 2015). HSP 72 has become one of the most important candidates among biomarkers recommended for early detection of AKI according to all these studies. Conversely, Vaara et al did not find any differences between the critically ill patients with and without AKI in terms of urinary HSP70 level (Vaara et al. 2016). Ramirez-Sandoval et al. demonstrated that urinary HSP72 did not differentiate between immunologic rejection with AKI, pre-renal AKI and other causes of AKI in renal transplant recipients (Ramirez-Sandoval et al. 2014). Kierulf-Lassen et al. evaluated effects of remote ischemic conditioning on renal ischemia-reperfusion injury. They found that remote ischemic pre-conditioning or per-conditioning strategies did not alter HSP70 upregulation (Kierulf-Lassen et al. 2015).
It has been notified that toxic injury of kidney may affect HSP 70 levels. Ochratoxin A, a mycotoxin secreted by Aspergillus, prevents HSP 70 induction in rat kidney and cell culture (Barisic et al. 2002). The authors stated that kidney damage due to Ochratoxin A is enhanced in the absence of protective effect of HSP 70 (Barisic et al. 2002). Molinas et al. investigated HSP 70 levels in urine, kidney and liver samples of the rats receiving Acetaminophen (Molinas et al. 2010). The authors established that HSP 70 levels increased in urine and in renal cortex simultaneously, whereas HSP 70 levels in liver tissue did not increase despite the elevation of plasma ALT levels due to hepatic damage (Molinas et al. 2010). Injury of proximal tubular cells via gentamicin induces HSP 72 according to degree of proximal tubular injury (Wang et al. 2006).
Chronic Kidney Diseases and HSP 70
Oxidative stress, inflammation and apoptosis increase in chronic kidney disease (CKD) as well as AKI (Lebherz-Eichinger et al. 2013). All these factors have a potential inducing role for HSP 70 response in CKD (Lebherz-Eichinger et al. 2013). HSP70 can inhibit apoptosis in different ways (Gotoh et al. 2004; Stankiewicz et al. 2005; Gurbuxani et al. 2003; Ravagnan et al. 2001). Also, HSP72 prevents synthesis of pro-inflammatory cytokines by repressing NF-kB (Jo et al. 2006). Especially, inflammation is an important part of progression in CKD, in fact in all chronic diseases. It has been considered that intracellular HSP have a protective role, although extracelluar HSP have immunogenic and inflammatory effect (Sreedharan and Van Why 2016). It has been claimed that HSP70 may have long-term detrimental effects in chronic inflammation, although it has been shown to be beneficial in the acute phase (Sreedharan and Van Why 2016, Schmitt et al. 2007). On the contrary, cell culture and animal model studies revealed that HSP70 is a protective factor in the case of urea elevated environment (Maddock and Westenfelder 1996; Neuhofer et al. 2001). Kim et al. demonstrated that inhibition of HSP70 suppresses Treg cells as well as suppressed their renoprotective effects (Kim et al. 2014).
The main reason for the progression of chronic kidney diseases to end stage renal disease (ESRD) is development of renal fibrosis in glomeruli and tubulointerstitial area regardless of the underlying renal disease. The effect of HSP 70/72 on renal fibrosis was studied in obstructive nephropathy models as a good example for renal fibrosis. It has been observed that HSP 70 concentration of the kidney increases in a model of obstructive nephropathy and returns to baseline after the obstruction was removed (Lin et al. 1998). Similarly, HSP 70 induction was also demonstrated in patients with uretheropelvic junction obstruction (Valles et al. 2003). Induction of HSP 72 by GGA reduces sclerotic damage, tubulointerstitial fibrosis, interstitial fibroblast accumulation and collagen deposition (Mao et al. 2008). Additionally, HSP 72 induction decreases apoptosis and cell proliferation in tubular epithelium (Mao et al. 2008). Besides these effects, GGA as an HSP 72 inducer prevent tubular epithelial-mesenchmal transition (EMT), retaining E-cadherin and inhibiting α-smooth muscle actin (Mao et al. 2008). The effect of HSP 72 on EMT has been shown to be independent of apoptotic mechanisms (Mao et al. 2008). TGF-β signaling pathways, particularly phosphorylation of Smad3, have an important role on EMT and kidney fibrosis (Zhou et al. 2010). HSP 72 inhibits TGF-β1 induced Smad3 activation and EMT. Peptide-binding domain of HSP 72 is required for these inhibitions (Zhou et al. 2010). Zhou et al confirmed that HSP 72 expression was increased in fibrotic human kidneys. This increase is accompanied by the expression of p-STAT3 and α-smooth muscle actin. HSP 72 deficiency significantly increases collagen and α-smooth muscle actin, aggravates STAT3 phosphorylation and kidney fibrosis in the fibrotic kidneys of HSP72 knockout mice (Zhou et al. 2016). Further, CD4+CD28null and CD4+CD28+T-cells incubated with HSP 70 increases the expression of IFN- and cytotoxic molecule, perforin, granzyme B in CKD subjects unlike healthy controls (Yadav et al. 2013). Blockade of angiotensin II, a pro-fibrotic cytokine, with losartan suppresses oxidative stress via decreasing superoxide dismutase and this process is strongly associated with HSP70 increase (Manucha et al. 2005). Downregulation of endothelial nitric oxide synthase (NOS) and HSP 70 coexist in obstructed kidney and induce apoptosis via increased Bax/BcL2 and caspase-3 activity (Manucha et al. 2011). Conversely, induction of HSP 70 expression is linked to decrease apoptosis on tubular cells during obstruction via the augmentation of nitric oxide (Manucha et al. 2011). The interaction between NOS and HSP 70 modulates WT-1 expression in obtrusive kidney (Mazzei and Manucha 2017). It is known that the WT-1 gene has crucial functions in kidney formation and development (Menke and Schedl 2003). The relationship between WT-1 gene and HSP 70 suggests that HSP70 is a chaperone that also plays a role in kidney development (Mazzei and Manucha 2017). Taken all together, HSP 70/72 has an important role in the development kidney fibrosis by different ways. These features make HSP 70 an attractive drug target to prevent or mitigate progression of kidney fibrosis.
Clinical studies evaluating the role of HSP 70/72 in CKD are limited. Marzec et al. demonstrated that HSP 72 expression was significantly decreased in monocytes of adult pre-dialysis CKD patients and the level of HSP 72 was negatively correlated with serum creatinine levels (Marzec et al. 2009). In the same study, HSP 70 expression in monocytes found to be lower in hemodialysis patients than in the pre-dialysis patients (Marzec et al. 2009). On the contrary, Musial et al found that serum HSP 70 was not different whereas anti-HSP 70 was increased in children with CKD (Musial et al. 2010). In addition, anti-HSP 70 is a negative prognostic factor for cardiovascular complications in children with CKD (Musial et al. 2010). Urine HSP 70 in stage 4–5 CKD was found to be elevated approximately fourfold comparing the healthy controls (Lebherz-Eichinger et al. 2012).
Reuter et al. evaluated HSP 72 expression in monocyte of patients receiving hemodialysis due to end-stage renal disease (Reuter et al. 2009). They found no difference between monocytes of patients and controls although the response of HSP 72 to heat shock was decreased and apoptosis was enhanced in patient’s monocytes but not affected by dialysis itself (Reuter et al. 2009). Crowe et al. observed that HSP 70 was higher in muscle specimen of hemodialysis patients than in the control group although the difference was not statistically significant (Crowe et al. 2007). Musial et al reported that pre-dialysis serum anti-HSP 70 levels in hemodialysis patients were not different from controls. After the hemodialysis session, the anti-HSP 70 levels decrease (Musial et al. 2009). It has been demonstrated that the expression of HSP 72/73 in renal tubules was higher in the hemodialysed patients than in the non-dialysed patients (Dinda et al. 1998). Shioshita et al. reported that expression of HSP 70 in peritoneal tissue of the patients on peritoneal dialysis was significantly higher than in the non-dialysed CKD patients (Shioshita et al. 2000). The expression of HSP 70 was much higher in patients with ultrafiltration loss, while there was no difference between in the patient with and without recurrent peritonitis (Shioshita et al. 2000).
Despite these studies, the role of HSP 70 in CKD is still unclear. Whether HSP 70 has positive or negative effects on the progression of CKD and whether therapeutic modulation of HSP 70 prevents the progression of CKD or not need to be clarified in order to the features of HSP 70 in practice.
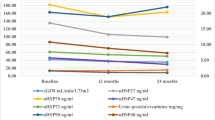
One of the most important causes of CKD in adults is diabetic nephropathy (Caramori and Mauer 2009; Marcovecchio and Chiarelli 2009). However, it may emerge in childhood because the age of onset of the type 1 diabetes mellitus (T1DM) has decreased over the last decade (Marcovecchio and Chiarelli 2009). The first sign of diabetic nephropathy is accepted to be microalbuminuria which occurs 6–15 years after the T1DM diagnosis whereas diabetic injury begins before microalbuminuria emerges (Caramori and Mauer 2009; Marcovecchio and Chiarelli 2009). Exposure consistently to high plasma glucose concentration and other metabolic factors including advanced glycosylated-end products (AGEs), oxidative stress, growth factors and cytokines contributes to developing nephropathy in T1DM (Caramori and Mauer 2009; Marcovecchio and Chiarelli 2009). High glucose concentration directly induces HSP70 gene expression in renal proximal tubular cells (Qi et al. 2007). Moreover, AGEs induce cellular oxidative stress and proliferation of interstitial fibroblasts in rat kidney activating Janus kinase 2- signal transducers and activators of transcription (JAK2/STAT) pathway (Marcovecchio and Chiarelli 2009; Chen et al. 2007; Guh et al. 2001). HSP70 expression was increased by JAK/STAT pathway activation (Madamanchi et al. 2001). It has been reported that HSP27/25, HSP60 and HSP70/72 overexpressed in the outer medulla of rat kidney in a model of diabetic nephropathy (Barutta et al. 2008). Therefore, we evaluated urine HSP27, HSP40, HSP60, HSP70, HSP90 levels in 33 children with T1DM twice, a year apart (Yilmaz et al. 2016a, b). The results were expressed as urine HSP/creatinine ratios (uHSP/Cr). In the first year of the study, all of these parameters were significantly higher in diabetic children than in the controls indicating that diabetic kidney injury has already started before microalbuminuria and renal insufficiency begin (Yilmaz et al. 2016a, b). Comparing all HSP with each other, uHSP70/Cr appears to be the best indicator for diabetic kidney injury because of the highest AUC (0.957), sensitivity (85%) and specificity (96%) (Yilmaz et al. 2016a, b). The possibility of diabetic kidney injury increases 20fold, when uHSP70/Cr is higher than a cut-off 22.59 pg/mgCr (Yilmaz et al. 2016a, b). Comparing the results of first year, uHSP70/Cr significantly increased at the second year of the study whereas uHSP60/Cr decreased and the others remained stable (Yilmaz et al. 2016a, b). According to our results, uHSP70/Cr increases over time and may indicate progressive damage in kidney of diabetic children (Yilmaz et al. 2016a, b). Our study demonstrated that urine level of HSP 70 increases as a response to a chronic insult for kidney.
Another multicenter study including our patients showed that increased serum HSP 70 level may be associated with glomerular diseases. Patients with IgA nephropathy were compared with the patients with idiopathic nephrotic syndrome (INS) as a patient control group, and healthy controls in terms of serum levels of HSP70. Serum HSP70 level was significantly higher in the IgA nephropathy group than in the INS group and controls whereas it was almost comparable between the patients with INS and controls (unpublished data).
Conclusions
Obviously, HSP 70 is involved in response to various acute and chronic insults of kidney and also other parts of the urinary tract. In this point of view, it does not seem to be a specific biomarker for any of the kidney diseases. However, HSP 70 level of body fluids may be beneficial as a biomarker, if we use it in some specific circumstances, for example for the differential diagnosis of “a children with fever”. The number of possible diseases in this situation is limited and an infection is most likely to be the reason of fever. Our study showed that UTI can be distinguished from other infections and contamination in “a children with fever” by measuring urine HSP 70 level. Thus, objective and accurate diagnosis of UTI will be possible. Another expectation from the studies on HSP 70 is to provide information to use this protein to ameliorate the kidney diseases. Clarifying the exact role of HSP 70 in different kidney diseases enables to discover new therapeutic options in order to prevent renal fibrosis and chronic renal failure in the future.
Abbreviations
- AGEs:
-
advanced glycosylated-end products
- AKI:
-
acute kidney injury
- AUC:
-
area under the curve
- CKD:
-
chronic kidney disease
- CSF:
-
cerebrospinal fluid
- EMT:
-
epithelial-mesenchymal transition
- ESRD:
-
end stage renal disease
- GGA:
-
geranylgeranylacetone
- HSP:
-
heat shock protein
- IFNγ:
-
interferon gamma
- IL-18:
-
interleukin 18
- INS:
-
idiopathic nephrotic syndrome
- JAK/STAT:
-
janus kinase/signal transducers and activators of transcription
- KIM-1:
-
kidney injury molecule type 1
- MEK/ERK:
-
Mitogen-activated protein kinase/ERK kinase/extracellular-signal-regulated kinase
- NGAL:
-
neutrophil gelatinase-associated lipocalin
- NF-kB:
-
nuclear factor kappa B
- NOS:
-
nitric oxide synthase
- p-STAT3:
-
phospho-signal transducer and activator of transcription 3
- ROS:
-
reactive oxygen species
- SLK:
-
Ste20-like kinase
- STAT3:
-
Signal transducer and activator of transcription 3
- TGF-β:
-
transforming growth factor beta
- T1DM:
-
type 1 diabetes mellitus
- uHSP70:
-
urine level of heat shock proetin 70
- uHSP/Cr:
-
urine heat shock protein/creatinine ratio
- UTI:
-
urinary tract infection
- WT1:
-
wilms tumor 1
References
Barisić, K., Petrik, J., Rumora, L., Cepelak, I., & Grubisić, T. Z. (2002). Expression of Hsp70 in kidney cells exposed to ochratoxin A. Archives of Toxicology, 76(4), 218–226.
Barrera-Chimal, J., Pérez-Villalva, R., Cortés-González, C., et al. (2011). Hsp72 is an early and sensitive biomarker to detect acute kidney injury. EMBO Molecular Medicine, 3(1), 5–20.
Barutta, F., Pinach, S., Giunti, S., et al. (2008). Heat shock protein expression in diabetic nephropathy. American Journal of Physiology. Renal Physiology, 295(6), 1817–1824.
Beck, F. X., Neuhofer, W., & Müller, E. (2000). Molecular chaperones in the kidney: Distribution, putative roles and regulation. American Journal of Physiology. Renal Physiology, 279(2), 203–215.
Buraczynska, M., Swatowski, A., Buraczynska, K., Dragan, M., & Ksiazek, A. (2009). Heat-shock protein gene polymorphisms and the risk of nephropathy in patients with Type 2 diabetes. Clinical Science, 116(1), 81–86.
Caramori, M. L., & Mauer, M. (2009). Pathogenesis and pathophysiology of diabetic nephropathy. In A. Greenberg (Ed.), Primer on kidney diseases (pp. 214–223). Philadelphia: Saunders.
Chen, S. C., Guh, J. Y., Chen, H. C., Yang, Y. L., Huang, J. S., & Chuang, L. Y. (2007). Advanced glycation end-product-induced mitogenesis is dependent on Janus kinase 2-induced heat shock protein 70 in normal rat kidney interstitial fibroblast cells. Translational Research, 149(5), 274–281.
Crowe, A. V., McArdle, A., McArdle, F., et al. (2007). Markers of oxidative stress in the skeletal muscle of patients on hemodialysis. Nephrology, Dialysis, Transplantation, 22, 1177–1183.
Cybulsky, A. V., Guillemette, J., & Papillon, J. (2016). Ste20-like kinase, SLK, activates the heat shock factor 1 – Hsp70 pathway. Biochimica et Biophysica Acta, 1863(9), 2147–2155.
Davies, E. L., Bacelar, M. M., Marshall, M. J., Johnson, E., Wardle, T. D., Andrew, S. M., & Williams, J. H. (2006). Heat shock proteins form part of danger signal cascade in response to lipopolysaccharide and GroEL. Clinical and Experimental Immunology, 145(1), 183–189.
Dinda, A. K., Mathur, M., Guleria, S., Saxena, S., Tiwari, S. C., & Dash, C. (1998). Heat shock protein (HSP) expression and proliferation of tubular cells in end stage renal disease with and without haemodialysis. Nephrology, Dialysis, Transplantation, 13(1), 99–105.
Evdokimovskaya, Y., Skarga, Y., Vrublevskaya, V., & Morenkov, O. (2010). Secretion of the heat shock proteins HSP70 and HSC70 by baby hamster kidney (BHK-21) cells. Cell Biology International, 34(10), 985–990.
Friedewald, J. J., & Rabb, H. (2004). Inflammatory cells in ischemic acute renal failure. Kidney International, 66(2), 486–491.
Gotoh, T., Terada, K., Oyadomari, S., & Mori, M. (2004). hsp70-DnaJ chaperone pair prevents nitric oxide- and CHOP-induced apoptosis by inhibitingtranslocation of Bax to mitochondria. Cell Death and Differentiation, 11(4), 390–402.
Guh, J. Y., Huang, J. S., Chen, H. C., Hung, W. C., Lai, Y. H., & Chuang, L. Y. (2001). Advanced glycation end product-induced proliferation in NRK-49F cells is dependent on the JAK2/STAT5 pathway and cyclin D1. American Journal of Kidney Diseases, 38(5), 1096–1104.
Gurbuxani, S., Schmitt, E., Cande, C., et al. (2003). Heat shock protein 70 binding inhibits the nuclear import of apoptosis-inducing factor. Oncogene, 22(43), 6669–6678.
Jo, S. K., Ko, G. J., Boo, C. S., Cho, W. Y., & Kim, H. K. (2006). Heat preconditioning attenuates renal injury in ischemic ARF in rats: Role of heat-shock protein70 on NF-kappaB-mediated inflammation and on tubular cell injury. Journal of the American Society of Nephrology, 17(11), 3082–3092.
Kennedy, D., Jäger, R., Mosser, D. D., & Samali, A. (2014). Regulation of apoptosis by heat shock proteins. International Union of Biochemistry and Molecular Biology Life, 66(5), 327–338.
Kierulf-Lassen, C., Kristensen, M. L., Birn, H., Jespersen, B., & Nørregaard, R. (2015). No effect of remote ischemic conditioning strategies on recovery from renal ischemia-reperfusion injury and protective molecular mediators. PLoS One, 10(12), e0146109.
Kim, M. G., Jung Cho, E., Won Lee, J., et al. (2014). The heat-shock protein-70-induced renoprotective effect is partially mediated by CD4+ CD25+ Foxp3 + regulatory T cells in ischemia/reperfusion-induced acute kidney injury. Kidney International, 85(1), 62–71.
Kim, Y. S., Jung, M. H., Choi, M. Y., et al. (2009). Glutamine attenuates tubular cell apoptosis in acute kidney injury via inhibition of the c-Jun N-terminal kinase phosphorylation of 14-3-3. Critical Care Medicine, 37(6), 2033–2044.
Lebherz-Eichinger, D., Ankersmit, H. J., Hacker, S., et al. (2012). HSP27 and HSP70 serum and urine levels in patients suffering from chronic kidney disease. Clinica Chimica Acta, 413(1–2), 282–286.
Lebherz-Eichinger, D., Krenn, C. G., & Roth, G. A. (2013). Keratin 18 and heat-shock protein in chronic kidney disease. Advances in Clinical Chemistry, 62, 123–149.
Lin, K. C., Krieg, R. J., Jr., Saborio, P., & Chan, J. C. (1998). Increased heat shock protein-70 in unilateral ureteral obstruction in rats. Molecular Genetics and Metabolism, 65(4), 303–310.
Luo, F. C., Zhao, L., Deng, J., et al. (2013). Geranylgeranylacetone protects against morphine-induced hepatic and renal damage in mice. Molecular Medicine Reports, 7(2), 694–700.
Madamanchi, N. R., Li, S., Patterson, C., & Runge, M. S. (2001). Reactive oxygen species regulate heat-shock protein 70 via the JAK/STAT pathway. Arteriosclerosis, Thrombosis, and Vascular Biology, 21(3), 321–326.
Maddock, A. L., & Westenfelder, C. (1996). Urea induces the heat shock response in human neuroblastoma cells. Journal of the American Society of Nephrology, 7, 275–282.
Mambula, S. S., Stevenson, M. A., Ogawa, K., & Calderwood, S. K. (2007). Mechanisms for Hsp70 secretion: Crossing membranes without a leader. Methods, 43(3), 168–175.
Manucha, W., Carrizo, L., Ruete, C., Molina, H., & Vallés, P. (2005). Angiotensin II type I antagonist on oxidative stress and heat shock protein 70 (HSP 70) expression in obstructive nephropathy. Cellular and Molecular Biology (Noisy-le-Grand, France), 51(6), 547–555.
Manucha, W., Kurbán, F., Mazzei, L., et al. (2011). eNOS/Hsp70 interaction on rosuvastatin cytoprotective effect in neonatal obstructive nephropathy. European Journal of Pharmacology, 650(2–3), 487–495.
Manucha, W. (2014). HSP70 family in the renal inflammatory response. Inflammation & Allergy Drug Targets, 13(4), 235–240.
Mao, H., Li, Z., Zhou, Y., et al. (2008). HSP72 attenuates renal tubular cell apoptosis and intertistitial fibrosis in obstructive nephropathy. Journal of the American Society of Nephrology, 295, 202–214.
Marcovecchio, M. L., & Chiarelli, F. (2009). Diabetic nephropathy. In D. E. Avner, E. V. Harmon, P. Niaudet, & N. Yoshikawa (Eds.), Pediatric nephrology (pp. 1199–1217). Berlin/Heidelberg: Springer.
Margel, D., Pevsner-Fischer, M., Baniel, J., Yossepowitch, O., & Cohen, I. R. (2011). Stress proteins and cytokines are urinary biomarkers for diagnosis and staging of bladder cancer. European Urology, 59(1), 113–119.
Marzec, L., Zdrojewski, Z., Liberek, T., et al. (2009). Expression of Hsp72 protein in chronic kidney disease patients. Scandinavian Journal of Urology and Nephrology, 43, 400–408.
Mayer, M. P. (2013). Hsp70 chaperone dynamics and molecular mechanism. Trends in Biochemical Sciences, 38(10), 507–514.
Mazzei, L., & Manucha, W. (2017). Growing evidence suggests WT1 effects in the kidney development are modulated by Hsp70/NO interaction. Journal of Nephrology, 30, 11–18.
Menke, A. L., & Schedl, A. (2003). WT1 and glomerular function. Seminars in Cell & Developmental Biology, 14(4), 233–240.
Molinas, S. M., Rosso, M., & Wayllace, N. Z. (2010). Heat shock protein 70 induction and its urinary excretion in a model of acetaminophen nephrotoxicity. Pediatric Nephrology, 25(7), 1245–1253.
Molitoris, B. A. (1991). New insights into the cell biology of ischemic acute renal failure. Journal of the American Society of Nephrology, 1(12), 1263–1270.
Molitoris, B. A., Dahl, R., & Hosford, M. (1996). Cellular ATP depletion induces disruption of the spectrin cytoskeletal network. The American Journal of Physiology, 271, 790–798.
Morales-Buenrostro, L. E., Salas-Nolasco, O. I., Barrera-Chimal, J., et al. (2014). Hsp72 is a novel biomarker to predict acute kidney injury in critically ill patients. PLoS One, 9(10), e109407.
Mueller, T., Bidmon, B., Pichler, P., et al. (2003). Urinary heat shock protein-72 excretion in clinical and experimental renal ischemia. Pediatric Nephrology, 18(2), 97–99.
Musiał, K., Szprynger, K., Szczepańska, M., & Zwolińska, D. (2009). Heat shock proteins in children and young adults on chronic hemodialysis. Pediatric Nephrology, 24(10), 2029–2034.
Musial, K., Szprynger, K., Szczepanska, M., & Zwolinska, D. (2010). The heat shock protein profile in children with chronic kidney disease. Peritoneal Dialysis International, 30, 227–232.
Musial, K., & Zwolinska, D. (2011). Heat shock proteins in chronic kidney disease. Pediatric Nephrology, 26(7), 1031–1037.
Neuhofer, W., Lugmayr, K., Fraek, M. L., & Beck, F. X. (2001). Regulated overexpression of heat shock protein 72 protects Madin-Darby canine kidney cells from the detrimental effects of high urea concentration. Journal of the American Society of Nephrology, 12, 2565–2571.
Neuhofer, W., Holzapfel, K., Fraek, M. L., Ouyang, N., Lutz, J., & Beck, F. X. (2004). Chronic COX-2 inhibition reduces medullary HSP70 expression and induces papillary apoptosis in dehydrated rats. Kidney International, 65(2), 431–441.
O’Neill, S., Harrison, E. M., Ross, J. A., Wigmore, S. J., & Hughes, J. (2014). Heat-shock proteins and acute ischaemic kidney injury. Nephron. Experimental Nephrology, 126(4), 167–174.
Ortega-Trejo, J. A., Pérez-Villalva, R., Barrera-Chimal, J., et al. (2015). Heat shock protein 72 (Hsp72) specific induction and temporal stability in urine samples as a reliable biomarker of acute kidney injury (AKI). Biomarkers, 20(6–7), 453–459.
Qi, W., Chen, X., Gilbert, R. E., et al. (2007). High glucose-induced thioredoxin-interacting protein in renal proximal tubule cells is independent of transforming growth factor-beta1. The American Journal of Pathology, 171(3), 744–754.
Ramirez-Sandoval, J. C., Barrera-Chimal, J., Simancas, P. E., Correa-Rotter, R., Bobadilla, N. A., & Morales-Buenrostro, L. E. (2014). Tubular urinary biomarkers do not identify aetiology of acute kidney injury in kidney transplant recipients. Nephrology (Carlton), 19(6), 352–358.
Ravagnan, L., Gurbuxani, S., Susin, S. A., et al. (2001). Heat-shock protein 70 antagonizes apoptosis-inducing factor. Nature Cell Biology, 3(9), 839–843.
Reuter, S., Bangen, P., Edemir, B., et al. (2009). The HSP72 stress response of monocytes from patients on haemodialysis is impaired. Nephrology, Dialysis, Transplantation, 24, 2838–2846.
Riordan, M., Sreedharan, R., Wang, S., et al. (2005). HSP70 binding modulates detachment of Na-K-ATPase following energy deprivation in renal epithelial cells. American Journal of Physiology. Renal Physiology, 288, 1236–1242.
Roberts, K. B., & Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management. (2011). Urinary tract infection: Clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics, 128(3), 595–610.
Schmitt, E., Gehrmann, M., Brunet, M., Multhoff, G., & Garrido, C. (2007). Intracellular and extracellular functions of heat shock proteins: Repercussions in cancer therapy. Journal of Leukocyte Biology, 81(1), 15–27.
Shioshita, K., Miyazaki, M., Ozono, Y., et al. (2000). Expression of heat shock proteins 47 and 70 in the peritoneum of patients on continuousambulatory peritoneal dialysis. Kidney International, 57(2), 619–631.
Sreedharan, R., & Van Why, S. K. (2016). Heat shock proteins in the kidney. Pediatric Nephrology, 31(10), 1561–1570.
Stankiewicz, A. R., Lachapelle, G., Foo, C. P., Radicioni, S. M., & Mosser, D. D. (2005). Hsp70 inhibits heat-induced apoptosis upstream of mitochondria by preventing Bax translocation. The Journal of Biological Chemistry, 280(46), 38729–38739.
Tang, D., Kang, R., Cao, L., et al. (2008). A pilot study to detect high mobility group box 1 and heat shock protein 72 in cerebrospinal fluid of pediatric patients with meningitis. Critical Care Medicine, 36(1), 291–295.
Vaara, S. T., Lakkisto, P., Immonen, K., Tikkanen, I., Ala-Kokko, T., Pettilä, V., & FINNAKI Study Group. (2016). Urinary biomarkers indicative of apoptosis and acute kidney injury in the critically Ill. PLoS One, 11(2), e0149956.
Vallés, P., Jorro, F., Carrizo, L., Manucha, W., Oliva, J., Cuello-Carrión, F. D., & Ciocca, D. R. (2003). Heat shock proteins HSP27 and HSP70 in unilateral obstructed kidneys. Pediatric Nephrology, 18(6), 527–535.
Van Why, S. K., Mann, A. S., Thulin, G., Zhu, X. H., Kashgarian, M., & Siegel, N. J. (1994). Activation of heat-shock transcription factor by graded reductions in renal ATP, in vivo, in the rat. The Journal of Clinical Investigation, 94(4), 1518–1523.
Van Why, S. K., Kim, S., Geibel, J., Seebach, F. A., Kashgarian, M., & Siegel, N. J. (1999). Thresholds for cellular disruption and activation of the stress response in renal epithelia. The American Journal of Physiology, 277(2), 227–234.
Varano Della Vergiliana, J. F., Lansley, S. M., Porcel, J. M., et al. (2013). Bacterial infection elicits heat shock protein 72 release from pleural mesothelial cells. PLoS One, 8(5), e63873.
Wang, Z., Liu, L., Mei, Q., Liu, L., Ran, Y., & Zhang, R. (2006). Increased expression of heat shock protein 72 protects renal proximal tubular cells from gentamicin-induced injury. Journal of Korean Medical Science, 21(5), 904–910.
Wang, Z., Jin, H., Li, C., Hou, Y., Mei, Q., & Fan, D. (2009). Heat shock protein 72 protects kidney proximal tubule cells from injury induced by triptolide by means of activation of the MEK/ERK pathway. International Journal of Toxicology, 28(3), 177–189.
Williams, G. J., Macaskill, P., Chan, S. F., Turner, R. M., Hodson, E., & Craig, J. C. (2010). Absolute and relative accuracy of rapid urine tests for urinary tract infection in children: A meta-analysis. The Lancet Infectious Diseases, 10(4), 240–250.
Yadav, A. K., Kumar, V., & Jha, V. (2013). Heat shock proteins 60 and 70 specific proinflammatory and cytotoxic response of CD4+CD28null cells in chronic kidney disease. Mediators of Inflammation, 2013, 384807.
Yilmaz, A., Gedikbasi, A., Yuruk Yildirim, Z., et al. (2016a). Higher urine heat shock protein 70/creatinine ratio in type 1 diabetes mellitus. Renal Failure, 38(3), 404–410.
Yilmaz, A., Yildirim, Z. Y., Emre, S., et al. (2016b). Urine heat shock protein 70 levels as a marker of urinary tract infection in children. Pediatric Nephrology, 31(9), 1469–1476.
Zhou, Y., Mao, H., Li, S., et al. (2010). HSP72 inhibits Smad3 activation and nuclear translocation in renal epithelial-to-mesenchymal transition. Journal of the American Society of Nephrology, 21(4), 598–609.
Zhou, Y., Cao, S., Li, H., et al. (2016). Heat shock protein 72 antagonizes STAT3 signaling to inhibit fibroblast accumulation in renal fibrogenesis. The American Journal of Pathology, 186(4), 816–882.
Acknowledgements
None
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Yilmaz, A., Yildirim, Z.N.Y. (2018). Clinical Implication of Heat Shock Protein 70 in Kidney Disease. In: Asea, A., Kaur, P. (eds) HSP70 in Human Diseases and Disorders. Heat Shock Proteins, vol 14. Springer, Cham. https://doi.org/10.1007/978-3-319-89551-2_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-89551-2_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-89550-5
Online ISBN: 978-3-319-89551-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)