Abstract
Food allergy (FA), a pathologic immune response to food proteins, affects 8% of children and adolescents in the United States. Effective FA diagnosis incorporates a comprehensive clinical history, physical examination, and diagnostic testing. Patients with FA are at risk for anaphylaxis, a life-threatening allergic reaction involving two or more organ systems. Prompt administration of epinephrine is the only lifesaving treatment for anaphylaxis. Additionally, lifestyle modifications are necessary to ensure the safety of patients with FA. These modifications include, but are not limited to, strict avoidance of food allergens, careful reading of food labels, comprehensive education on anaphylaxis management, taking precautions when outside of the home, and raising food allergy awareness. This chapter will discuss prevalence, pathophysiology, diagnosis, treatment, differential diagnosis, prognosis, and common misperceptions of food allergy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Background
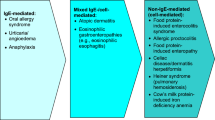
Food allergy (FA), a pathologic immunologic response to food proteins, affects 8% of children and adolescents in the United States [1] and has been increasing in prevalence [2]. In general, the overall economic cost of FA for families and society is estimated to be $24.8 billion annually [3]. The most common food allergens include peanut (25.2% of children with food allergy), milk (21.1%), shellfish (17.2%), tree nuts (13.1%), egg (9.8%), finfish (6.2%), wheat (5.0%), and soy (4.6%) [1]. Additionally, many children and adolescents with food allergy are allergic to more than one food [1]. FA is classified into immunoglobulin E (IgE)-mediated , non-IgE-mediated , and mixed reactions ; this chapter will focus on IgE-mediated food allergy.
The onset of a pathologic food allergy response is sensitization , during which a T helper 2 (Th2) cell response is initiated against a food antigen, resulting in antigen-specific IgE production by B cells. Once antigen-specific IgE antibodies (sIgE) are in production, an individual is considered to be sensitized to the antigen. Importantly, sensitization is not equivalent to clinical allergy; it is not uncommon for an individual to produce sIgE antibodies to foods that are clinically tolerated. Once in circulation, IgE binds to high-affinity receptors on the surface of mast cells (inside tissues) and basophils (inside blood vessels), thus priming these cells for activation. Mast cells, located in the skin, gut, and respiratory tract, are the primary agents of the allergic response. Upon reexposure to the antigen, mast cells degranulate, releasing histamine and a variety of cytokines, chemokines, enzymes (e.g., tryptase) and eicosanoids (e.g., leukotrienes, prostaglandins, and platelet-activating factor) into the extracellular space. Histamine , in particular, is responsible for several of the responses typically associated with acute allergic reactions , including urticaria, angioedema, nausea/vomiting, coughing/wheezing, hypotension, and increased nasal mucus production and heart rate. Table 9.1 presents common symptoms associated with anaphylaxis [4]. These symptoms may occur alone or in combination and typically begin within minutes of ingestion of the food antigen . When symptoms involve two or more organ systems (e.g., skin and cardiovascular), the reaction is classified as anaphylaxis , a severe and potentially life-threatening allergic reaction which requires immediate treatment with epinephrine . Among children with food allergy, 38.7% have experienced a severe reaction [1].
In addition to the possibility of allergic reactions, including severe reactions and anaphylaxis, food allergies are associated with a range of comorbid conditions (e.g., asthma, atopic dermatitis, and allergic rhinitis), as well as negative outcomes such as limited social interactions and decreased quality of life for affected individuals and their families [5]. This chapter will review diagnosis, treatment, prognosis, and common misperceptions of IgE-mediated food allergies .
Diagnosis
Clinical History
A comprehensive clinical history is essential to distinguish food allergy from other food-related adverse reactions and to accurately diagnose and manage FA. Information to be collected includes the route and quantity of exposure of the suspected food allergen, symptoms, timing of onset, duration, and reproducibility of symptoms, as well as treatment administered and response to the treatment. Family history and medical history should also be obtained, as well as factors such as concurrent alcohol consumption, exercise, fever, and/or drug use, which have the potential to exacerbate allergic reactions [6]. Dietary history , including any food that the patient may be avoiding, can help narrow down suspected food allergens. For example, if a food has been tolerated and is included in the diet, further testing for that food is not needed. If it is not clear to which food an individual is showing adverse reaction, the possibility of cross-contact should be considered.
Physical Examination
The physical examination may help identify acute symptoms of an allergic reaction if conducted within minutes to hours after exposure to the suspected food allergen. More commonly, it leads to identification of atopic diseases which have a high rate of co-occurrence with food allergy, including atopic dermatitis, asthma, allergic rhinitis, and/or allergic urticaria [7]. The physical examination also provides an opportunity to assess growth parameters, nutritional status, and chronic oropharyngeal, gastrointestinal, pulmonary, and/or cutaneous symptoms. These factors may be suggestive of other food-related sensitivities which may warrant further investigation.
Diagnostic Testing
With supportive evidence from the clinical history and physical examination , various tests can be utilized to assess and confirm suspected IgE-mediated food allergy. Allergen-specific IgE (sIgE) testing is an in vitro assessment which measures blood serum levels of IgE to a specific allergen. It is important to note that sIgE only reflects immunologic sensitization to an allergen and is not indicative, in and of itself, of clinical food allergy. Thus, panel testing of large numbers of allergens is not recommended in diagnostic practice . sIgE should only be conducted in the case of specific foods that are in question for causing a reaction and not currently tolerated in the diet. While general practitioners may perform sIgE testing, an elevated result (≥0.35 kU/L) warrants referral to an allergy specialist for further testing and management.
Skin prick testing (SPT) is an in vivo assessment performed by an allergy specialist in which a small amount of allergen is introduced into the epidermis to assess allergen-induced mast cell activation . In sensitized individuals, a wheal and flare reaction at the site of placement develops within minutes and is compared to positive and negative controls. A wheal ≥3 mm larger than the negative control is often considered an elevated result and indicates that sIgE is bound to cutaneous mast cells. While SPTs are indicative of sensitization and have a strong negative predictive value (NPV ~95%), they have a poor positive predictive value (PPV ~50%). Therefore, SPTs should not be used as a definitive diagnostic test for clinical food allergy [2]. For both sIgE and SPT results, the size of the test result can indicate the likelihood that a food allergy may be present, when the clinical history is highly suggestive. An elevated IgE by itself does not diagnose food allergy. In addition, the size of the IgE result does not indicate the severity of future reactions but can only be utilized to help determine the likelihood that a food allergy may be present.
The most accurate method for food allergy diagnosis is the graded oral food challenge (OFC), in which the patient ingests incremental amounts of a food allergen under close monitoring for the appearance of any symptoms of an allergic reaction. If the patient exhibits symptoms consistent with an IgE-mediated reaction during the challenge, a food allergy is considered present and the patient should avoid the food. If the patient successfully consumes a full serving of the food without symptoms, they may include the food in the diet. OFCs are often used in cases of an indeterminate patient history, inconclusive IgE tests, and/or to test if an allergy has been outgrown. Table 9.2 lists testing thresholds for SPT and sIgE tests [8]. Due to the risk inherent in OFCs , the procedure should only be performed in a specialized medical facility under the supervision of a qualified allergy specialist.
Clinical Vignette
Jon, a 15-year-old African American male, referred by his primary care physician, presents with a history of chest tightness, urticaria, and vomiting after eating clam. He has a medical history of asthma which is currently well-controlled with as needed use of albuterol and daily budesonide. Three weeks prior to his visit, he tried clam chowder for the first time and developed full-body urticaria and chest tightness within 5 min of consumption. After 10 min, he complained of nausea and started vomiting. He was driven to the emergency department, and upon epinephrine and albuterol administration, his symptoms subsided. He also reports an episode of urticaria 1 month ago following consumption of a bowl of lobster bisque containing lobster and a combination of fish and clam broth. Within 5 min after consumption, his mother noticed urticaria on his torso, arms, and legs. Symptoms resolved following administration of diphenhydramine. He has had previous exposure to lobster and did not have any history of previous adverse reactions. Currently, he eats wheat, egg, soy, milk, tree nuts, and peanuts without a problem. Prior to this month, he regularly consumed salmon and shrimp with no complaints. He does not recall eating other finfish, scallops, or oysters.
His father has a history of allergy to peanuts, cats, and horses. His mother and younger brother do not have a history of food allergy or any other atopic disease. The patient lives with his mother, father, younger brother, and their dog. He has no smoke exposure in the house.
Physical Examination
General appearance: Well-developed 15 year-old boy. Not in acute distress.
HEENT: No eye discharge/erythema/swelling. TMs clear bilaterally, no bulging/erythema. No nasal discharge, polyp, or airway blockage. No angioedema of lips. Moist mucous membranes . No erythema or swelling on nasopharynx.
Chest: Inspection normal. No urticaria/scar/lesion. Clear to auscultation bilaterally.
CV: Regular rate and rhythm. + S1/S2. No murmur/gallop/rubs.
Abdomen: No urticaria/scar/lesion on inspection. Bowel sounds positive in all four quadrants. No mass/tenderness on palpation.
Skin: No erythema/urticaria/scar.
Laboratory Data
In light of the clinical history, SPT and sIgE testing were performed for shellfish and finfish. SPT results were elevated for clam (5 mm), oyster (3 mm), and scallop (3 mm) and negative for finfish, lobster, crab, and shrimp. sIgE testing was elevated for clam (9 kU/L), oyster (0.9 kU/L), and scallop (0.78 kU/L).
Differential Diagnoses
Food poisoning , viral gastroenteritis , food intolerance , acute generalized urticaria , alcohol consumption , scombroid syndrome
Treatment Plan and Follow-Up
The patient and his family were counseled on the prognosis of food allergy, signs, and symptoms, treatment of allergic reactions and anaphylaxis, and lifestyle modifications including dietary avoidance. The patient was instructed to avoid clam. Since he has no history of eating oysters and scallops, recommendation for OFC was made and scheduled. He was told that he could continue consuming lobster, crab, and shrimp but was counseled on the risks of cross-contact. A food allergy action plan was developed and discussed along with the use of an epinephrine auto-injector. A follow-up visit was scheduled in 1 year.
Treatment: Medications
Epinephrine
Epinephrine (adrenaline) is the only lifesaving medication that can terminate anaphylaxis. It should be prescribed for patients with a history of anaphylaxis, a prior systemic allergic reaction, comorbid asthma and food allergy, and/or a known food allergy, especially to peanut, tree nuts, fish, and shellfish, all of which are associated with increased risk for future anaphylaxis. However, since allergic reactions to food are inherently unpredictable (i.e., they may vary among patients and between exposures within a given patient), prescription of epinephrine should be considered for all patients diagnosed with an IgE-mediated food allergy.
Epinephrine plays a critical role in the reversal of all symptoms of anaphylaxis. Epinephrine administration results in blood vessel constriction, effectively reversing anaphylaxis-induced decreases in blood pressure by increasing peripheral vascular resistance. Epinephrine binding to α-adrenergic receptors elicits an increase in coronary artery perfusion. Additionally, vasoconstriction in other systemic vessels including the skin and mucosal surfaces prompts a decrease in angioedema, urticaria, and potentially systemic absorption of the allergen. Epinephrine also binds to β1-adrenergic receptors, causing an increase in heart rate and contractility, and to β2-adrenergic receptors which leads to inhibition of cytokine release and mediates bronchodilation [9]. See Fig. 9.1 .
Epinephrine auto-injectors (EAIs) are used to deliver a single dose of epinephrine into the thigh muscle and are available in 0.15 mg (patients weighing 15–25 kg) or 0.3 mg (≥25 kg) doses according to patient weight, with recent approval for a 0.1 mg dose for infants who weigh less than 15 kg. Previous literature suggests that >35% of patients experiencing anaphylaxis required >1 dose of epinephrine, and, therefore, two EAIs should be carried at all times [10]. It is important to note that epinephrine should be administered immediately upon suspicion of anaphylaxis. The risks of administration are low and delayed administration is associated with poorer outcomes and higher mortality rates [11]. To administer an EAI: (1) remove the safety cap, (2) press the auto-injector into the lateral thigh, and (3) hold for 3–10 s (depending on the manufacturer). Following the initial injection, 9-1-1 should be called for transfer to a medical facility for further monitoring and treatment. If symptoms persist after 5–15 min, a second dose of epinephrine should be administered. Patients should also be aware of the possibility of biphasic reactions, in which signs and symptoms resolve but recur after a period of hours. The recommendation to seek emergency care after any use of epinephrine is based upon the potential for symptoms to be partially treated or return. Thus, additional monitoring is indicated for anyone who has anaphylaxis. Reviewing this indication and rationale can be helpful for adolescents and parents, who may misinterpret the need for emergency room care as being due to dangers or side effects stemming from the epinephrine auto-injector. Hence, they may be reluctant to use their epinephrine when indicated.
Antihistamines, Albuterol, and Steroids
Antihistamines such as diphenhydramine (Benadryl) and cetirizine (Zyrtec) are frequently administered for mild allergic reactions including urticaria and pruritus. However, while antihistamines may be palliative for mild symptoms, they do not halt the progression of an allergic reaction and should therefore be considered an adjunct to epinephrine in the case of suspected anaphylaxis. They are typically slow to act (30–60 min) and have no significant effect in the treatment of anaphylaxis [12].
Asthma medications, such as short-acting bronchodilators (e.g., albuterol), should be used adjunctively during an allergic reaction to address respiratory symptoms, especially for patients with a history of asthma or bronchospasm. In those with a history of asthma, lower respiratory symptoms (e.g., wheeze, cough) should always be treated with epinephrine during a food-induced allergic reaction. Corticosteroids have no role in the acute management of anaphylaxis due to their delayed onset of action. Corticosteroids have traditionally been given to patients with anaphylaxis in an effort to prevent a biphasic reaction from occurring, but a recent meta-analysis demonstrated no protective effect [13].
Treatment: Lifestyle Modification and Environmental Controls
Although epinephrine is safe and effective for the emergency treatment of anaphylaxis, lifestyle modifications are necessary for effective FA management and the prevention of allergic reactions to food.
Avoidance
Strict avoidance of food allergens is the only certain way to prevent allergic reactions. While exposure to food antigens may occur via the skin (cutaneous exposure), mouth (oral exposure), or lungs (inhalation exposure), severe reactions most commonly develop following oral exposure [14]. For example, previous literature suggests that children with peanut allergy do not experience a systemic or respiratory reaction following peanut exposure via cutaneous or inhalation routes [15]. It should be noted that while food odors cannot elicit a clinical reaction, food proteins that are aerosolized during cooking may provoke respiratory symptoms in children with food allergy and asthma. Additionally, due to the possibility of cross-contact, patients should be counseled to avoid foods that are manufactured or prepared in environments in which their allergens are present, unless strict allergen containment precautions are known to be in place.
Food Labels
In order to effectively avoid food allergens , patients and families should be counseled to pay attention to food ingredients and labels. In 2004, the Food Allergen Labeling and Consumer Protection Act (FALCPA) was passed, requiring food manufacturers to clearly state if a packaged food sold in the United States contains any of the top eight food allergens (peanut, tree nuts, milk, egg, wheat, soy, finfish, and shellfish) as ingredients [16]. It is important to note that such labeling is not required for meat, poultry, certain egg products, or alcoholic beverages, if allergens are in the form of highly refined oils, if scientific evidence establishes that food ingredients do not contain allergenic protein(s), and/or if the FDA determines that a food does not prompt an allergic response in sensitized individuals. It should also be emphasized that labeling for possible cross-contact during the manufacturing or packaging process is not required. While some manufacturers choose to utilize precautionary allergen labeling (PAL) , such labeling is voluntary and phrasing is not standardized. These phrases include “may contain,” “may contain traces of,” and “manufactured in a facility that also processes.”
Education on Anaphylaxis Management
Due to the possibility of accidental exposures to food allergens despite best efforts at avoidance, it is important for patients and families to learn how to manage an allergic reaction. Families should be counseled on how to recognize common symptoms of an allergic reaction, the identification of anaphylaxis, and appropriate administration of epinephrine. An emergency action plan should be completed by the clinician and reviewed with the patient periodically. This form includes patient-specific food allergen(s), guidelines for treatment, and emergency contact information. Templates can be found on the American Academy of Allergy, Asthma, and Immunology (www.aaaai.org) and American Academy of Pediatrics (www.aap.org) websites in English and Spanish.
Past research indicates that despite the fact that adolescents are at greater risk for severe reactions and fatal anaphylaxis due to food, this age group is less likely to report their allergic reactions as “anaphylactic,” even when symptoms indicate anaphylaxis [17]. With increasing independence, risk-taking, and activities outside the home, this age group in particular should be counseled on the risks and symptoms of anaphylaxis and the safety and effectiveness of epinephrine administration.
Dining Out
A large proportion of food-induced fatal reactions are related to eating food not prepared at home [2]. Although five states (Illinois, Maryland, Massachusetts, Rhode Island, Virginia) and two cities (New York City, NY, and St. Paul, MN) have legislation related to restaurants and food allergies in place, dining out requires that patients with food allergy take additional precautions. Before planning to eat out, it may be useful for families to check menus online to see if there are any safe options and/or to call ahead to ask about ingredients and methods of preparation, including the possibility of cross-contact. Fried foods, baked goods, and desserts may be at particularly high risk for cross-contact. It is often advisable to communicate directly with the chef in order to obtain accurate information. Food allergies should be disclosed to wait staff prior to ordering. The patient should always carry epinephrine while dining out, and in the event of anaphylaxis, epinephrine should be administered immediately. Similar precautions should be taken while dining out at athletic events, camps, church events, workplaces, and when traveling.
School
Up to 25% of students experience their first allergic reaction at school [18]. Since food exposures may occur in a variety of ways during the school day (e.g., meals and snacks, classroom activities, celebrations, school events), successful management of food allergy at school requires collaboration between the student’s family, school staff, and medical professionals. Clinicians can provide guidance to families on federal and regional school policies and should encourage families to talk with school administration and health staff about establishing appropriate precautions and preparedness plans. It should be noted that every state in the United States is currently required to allow students to self-carry and self-administer an EAI at school and that nearly every state allows or requires that schools stock undesignated (nonstudent-specific) epinephrine on the premises. Families may also be counseled on the types of health management plans that may be put in place for students, including emergency action plans , individualized healthcare plans (IHPs) , and Section 504 Plans [19]. Additionally, counseling is necessary for common concerns that may arise for school age children including reluctance to carry or use an EAI or to disclose their food allergy to school peers [20]. The use of a medical alert bracelet may also be suggested, particularly for younger children. Finally, clinicians can work directly with school administrators in the development and implementation of school policies for the prevention and management of allergic reactions.
College presents unique challenges for students with food allergy. Students should be encouraged to discuss food allergy policies and protocols with school administration prior to enrollment and during orientation. Dining hall precautions and safe food options, housing options , and EAI training of college staff should be covered, and students may wish to schedule an appointment with the staff nutritionist. Patients approaching drinking age should also be counseled on the potential effects of alcohol consumption on food allergic reactions.
Advocacy and Food Allergy Awareness
In addition to counseling patients on food allergen avoidance, clinicians can support patients and their families in advocating for effective food allergy policies and increased food allergy awareness among the general public. Patients and families should be supported and empowered to advocate for themselves and for policy changes and may be directed toward resources to assist them in doing so. Food allergy advocacy organizations , support groups , and peer education materials may be useful sources of information.
Common Misperceptions
Differential Diagnosis
Food allergies may be misdiagnosed as other adverse reactions to food. For accurate diagnoses, it is important to distinguish the mechanism of a reaction: immune-mediated or nonimmune-mediated . Immune-mediated disorders are a result of an abnormal immune response. Common immune-mediated disorders that are often mistaken for food allergy include:
-
Celiac disease : An autoimmune disorder in which gluten consumption causes damage to the small intestine. Symptoms include abdominal pain, diarrhea, vomiting, weight loss, and malabsorption. It is typically hereditary and occurs in genetically predisposed individuals.
-
Eosinophilic gastrointestinal disorders : Examples include eosinophilic esophagitis and allergic inflammation in the esophagus. Symptoms include failure to thrive, vomiting, dysphagia, or food impaction. The GI tissue can be affected.
-
Food protein-induced enterocolitis syndrome (FPIES ): A non-IgE-mediated immune reaction that impacts the GI system. Common triggers include dairy and soy, but rice, oat, and barley are also known triggers. Symptoms include delayed onset vomiting and diarrhea (typically 2–3 h after ingestion) which cease when the trigger food is removed.
-
Oral Allergy Syndrome (OAS) : May occur among individuals with seasonal allergies. Proteins found in some fruits, vegetables, and some tree nuts are similar to those found in pollen. The immune system recognizes both pollen and the similar proteins in food being consumed and prompts an allergic response. Symptoms do not usually progress beyond the mouth and quickly subside upon food ingestion or removal. Symptoms include itchy mouth, scratchy throat, swelling lips, mouth, tongue, and/or throat. Common associations include (1) birch pollen (apple, almond, carrot, celery, and cherry), (2) grass pollen (celery, melons, oranges, peaches, and tomatoes), and (3) ragweed pollen (banana, cucumber, melons, sunflower seeds, zucchini). Interestingly, the proteins that cause OAS are labile, and patients can often tolerate the same fruits/vegetables that cause symptoms if those foods are cooked, peeled, canned, or processed.
Nonimmune-mediated disorders include:
-
Auriculotemporal (Frey) syndrome : A rare neurological disorder consisting of unilateral sweating and flushing after eating.
-
Gustatory rhinitis : rhinorrhea caused by spicy food.
-
Food intolerance : Consists of digestive problems when consuming food. Onset is gradual and includes symptoms such as nausea, stomach pain, diarrhea, vomiting, gas, cramps, bloating, and headaches. Reactions are not life-threatening.
-
Pharmacologic reactions: Examples include adverse effects related to caffeine, tryptamine, or alcohol consumption.
-
Toxic reactions: Examples include scombroid food poisoning or food poisoning in general. Scombroid food poisoning occurs upon consuming decayed fish. A toxin related to histamine is produced during the decay process. Food poisoning is the result of consuming spoiled or contaminated food. Symptoms include nausea, vomiting, and/or diarrhea.
-
Psychological reactions: Food aversions or food phobias.
Quality of Life
The management of food allergy often presents psychological and economic burdens on patients and their families; see Chap. 10 for an in-depth discussion. The avoidance of allergen exposure not only requires constant vigilance but can impose limitations on social interactions and induce strain in familial and peer relationships [5]. Children and adolescents with food allergy may experience a range of emotions around their diagnosis and the threat of an allergic reaction, including anxiety, fear, embarrassment, stress, and isolation. Adolescence, in particular, is a transitional period during which patients begin to take on increased personal responsibility for managing their food allergy. Expectedly, greater independence is often accompanied by greater anxiety. Food allergy-specific quality of life questionnaires, primarily for research purposes, have been established and may be a useful tool for clinicians to utilize in assessing the quality of life effects of food allergy on patients and their families. Referral to a clinical social worker or therapist may also be beneficial for some patients; these professionals may support patients and their families in developing strategies to combat food allergy-related anxiety and stress. Furthermore, ensuring that patients and families feel empowered to manage their food allergy and prepared to respond in the event of a reaction can help improve health-related quality of life for patients with food allergy and their families.
Prognosis: Outgrowing Food Allergy
It is not uncommon for children with food allergy to develop tolerance to a food allergen, also known as “outgrowing” a food allergy . Past studies indicate that many children outgrow egg, soy, wheat, and milk allergies. In one study, 82% of patients had developed tolerance to egg by age 16, 69% of patients had developed tolerance to soy by age 10, 65% had developed tolerance to wheat by age 12, and 80% had developed tolerance to milk by age 5 [21]. Allergies to peanut , tree nuts, shellfish, and finfish are less frequently outgrown. Periodic assessment by an allergy specialist will help determine whether a patient may be outgrowing a food allergy. If sIgE and SPT testing indicate that a patient may have outgrown an allergy, an OFC may be conducted. Following a successful OFC , the food may be introduced back into the diet in accordance with allergist recommendations.
Conclusion
Food allergy is a growing public health concern , impacting 8% of children and adolescents in the United States. Strict allergen avoidance and prompt treatment of anaphylaxis with epinephrine are currently the mainstays of food allergy management. Additionally, patients should be counseled on ways to effectively manage food allergies while out of the home. It is important to raise food allergy awareness among family, friends, school personnel, and the general public to better protect children with FA.
References
Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1):e9–17.
Burks AW, Tang M, Sicherer S, Muraro A, Eigenmann PA, Ebisawa M, et al. ICON: food allergy. J Allergy Clin Immunol. 2012;129(4):906–20.
Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167(11):1026–31.
Sharma HP, Bansil S, Uygungil B. Signs and symptoms of food allergy and food-induced anaphylaxis. Pediatr Clin N Am. 2015;62(6):1377–92.
Walkner M, Warren C, Gupta RS. Quality of life in food allergy patients and their families. Pediatr Clin N Am. 2015;62(6):1453–61.
Niggemann B, Beyer K. Factors augmenting allergic reactions. Allergy. 2014;69(12):1582–7.
Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133(2):291–307.e5.
Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, et al. Food allergy: a practice parameter update—2014. J Allergy Clin Immunol. 2014;134(5):1016–25.e43.
Simons FER. Anaphylaxis: recent advances in assessment and treatment. J Allergy Clin Immunol. 2009;124(4):625–36.
Korenblat P, Lundie MJ, Dankner RE, Day JH. A retrospective study of epinephrine administration for anaphylaxis: how many doses are needed? Allergy Asthma Proc. 1999;20(6):383–6.
Sampson HA, Mendelson L, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327(6):380–4.
Wright BL, Walkner M, Vickery BP, Gupta RS. Clinical management of food allergy. Pediatr Clin N Am. 2015;62(6):1409–24.
Alqurashi W, Ellis AK. Do corticosteroids prevent biphasic anaphylaxis? J Allergy Clin Immunol Pract. 2017;5(5):1194–205.
Sicherer SH, Furlong TJ, Muñoz-Furlong A, Burks AW, Sampson HA. A voluntary registry for peanut and tree nut allergy: characteristics of the first 5149 registrants. J Allergy Clin Immunol. 2001;108(1):128–32.
Simonte SJ, Ma S, Mofidi S, Sicherer SH. Relevance of casual contact with peanut butter in children with peanut allergy. J Allergy Clin Immunol. 2003;112(1):180–2.
Public Law 108-282-Aug. 2, 2004 (Food Allergen Labeling and Consumer Protection Act). 2004.
Gupta RS. Anaphylaxis in the young adult population. Am J Med. 2014;127(1, Supplement):S17–24.
Sicherer SH, Mahr T. Management of food allergy in the school setting. Pediatrics. 2010;126(6):1232–9.
Pistiner M, Devore CD, Schoessler S. School food allergy and anaphylaxis management for the pediatrician--extending the medical home with critical collaborations. Pediatr Clin N Am. 2015;62(6):1425–39.
Sampson MA, Muñoz-Furlong A, Sicherer SH. Risk-taking and coping strategies of adolescents and young adults with food allergy. J Allergy Clin Immunol. 2006;117(6):1440–5.
Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 0):S1–58.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Jiang, J., Kao, L.M., Aktas, O.N., Gupta, R.S. (2018). Food Allergies: An Overview. In: Stukus, D. (eds) Allergies and Adolescents. Springer, Cham. https://doi.org/10.1007/978-3-319-77485-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-77485-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-77484-8
Online ISBN: 978-3-319-77485-5
eBook Packages: MedicineMedicine (R0)