Abstract
The chapter on healthcare consequences of non-adherence initially presents the thematic of global prevalence and healthcare costs of uncontrolled hypertension, followed by the clinical consequences of non-adherence to antihypertensive drugs. Drug adherence is a complex phenomenon and may be influenced by many factors, one of which is the coexistence of other chronic diseases. Thus, a discussion exposing the relationship of drug adherence with the presence of associated morbidities is presented. Subsequently, an overview of the risk prediction and the population impact of implementing guidelines and interventions on drug adherence are depicted. The discussion is further followed by the technology advances and healthcare reform efforts creating an opportunities to reshape the current system where evidence generated from observational studies could contribute to better meet stakeholder needs. Several considerations of the clinical consequences of healthcare professional and system on drug adherence are introduced. Finally, the last section considers the clinical consequences of implementing patient-centered approaches and personalized evaluations of adherence to antihypertensive drugs, as well as the clinical consequences of changes to healthcare professional- and policy-related factors on adherence.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Global Prevalence and Healthcare Costs of Uncontrolled Hypertension
Firstly, hypertension is a chronic disease that affects over one billion people worldwide [1]. Suboptimal control of blood pressure is a major public health challenge because it is a major risk factor for major cardiovascular events [2]. It has been estimated that 7.5 million deaths per year worldwide [3,4,5] and about 4.58 million deaths per year in Europe are attributed to cardiovascular diseases [1, 6].
Therefore, improving blood pressure control is a major priority of clinical practice worldwide [3, 7]. Many individuals with hypertension, however, are unaware of their disorder. Among patients who are aware of their disorder, many are not treated and many are treated but their blood pressure remains poorly controlled [8]. The factors associated with the lack of treatment and control of hypertension are very complex, but may include the patient’s non-adherence to prescribed drugs, patient behavioral factors, healthcare professional-related factors, and characteristics of the healthcare system [7,8,9,10].
In Europe, the blood pressure has been still persistently high [2], and this holds especially true for the general population of Europe compared with the Americans [11]. The proportions of patients with controlled hypertension in the United States approximately doubled from 27% in 1988–1994 to 52% in 2007–2010 [12, 13]. This improvement was associated with an increase in the proportion of patients using antihypertensive drugs and an improvement in blood pressure control among treated patients [12,13,14]. The proportion of treated patients but uncontrolled hypertension who were using more than three antihypertensive drugs increased from 16% in 1988–1994 to 28% in 2005–2008 [14]. Again, there is still improvement in the underlying reasons of inadequate control of hypertension in older patients, since up to 50% of them still had inadequate control [15,16,17,18,19]. More optimal pharmacotherapy of hypertension needs to assess if the lack of optimal control is related to the suboptimal adherence to medication or a true treatment resistant hypertension [20].
Secondly, health expenditure for cardiovascular conditions and hypertension represent a large proportion of global healthcare costs. In 2006, within Europe, the annual expenditure associated with the treatment of cardiovascular conditions was estimated to be €169 billion, 60% of which was for direct medical costs [21]. In 2012, a recent analysis of data from five European countries estimated that the direct cost of treating hypertension was €51.5 billion [22]. In 2001, the global healthcare cost related to uncontrolled hypertension in the United States was estimated to be US$378 billion, about 10% of the global healthcare expenditure [5, 23].
Non-adherence to antihypertensive drugs results in poor blood pressure control [24] and increases in healthcare use and expenditure. In 2004 in the United States, it was estimated that non-adherence to treatment increased healthcare expenditure by US$792 million [25]. It was also reported that up to 33% of drug-related admissions to hospital were due to non-adherence to prescribed drug regimens [26]. Recently, a study published in 2015 that simulated data over a 10-year period suggested that improving antihypertensive drug adherence to 70% would save approximately €332 million from a national perspective of five European countries, e.g., Italy, Germany, France, Spain, and the UK [22].
2 Clinical Consequences of Non-adherence to Antihypertensive Drugs
One of the most effective strategies to control blood pressure is to prescribe antihypertensive drugs, which reduce the risk of cardiovascular events, and hence decrease the economic and clinical burden of hypertension and cardiovascular disease [27,28,29,30]. However, the clinical effectiveness of antihypertensive drugs is closely linked to the patient’s adherence to the prescribed treatment [31, 32].
Elevated blood pressure is associated with about 54% of cases of stroke and 47% of cases of ischemic heart disease worldwide [33]. A meta-analysis of randomized controlled trials demonstrated that the management of blood pressure among patients with hypertension is important mainly in terms of reducing the risks of cardiovascular disease and mortality [34, 35]. It is notable of a 5 mmHg of diastolic blood pressure from antihypertensive drugs compared to the pretreatment level reduced the risk of stroke by about 34% and the risk of ischemic heart disease by 21% [36].
Optimal drug adherence means that the patient takes the drugs as prescribed and continues to take the prescribed drug in accordance with the recommendations of the patient’s physician, pharmacist, and health professionals [37]. In the real world, however, the adherence to prescribed drugs is often low in patients with chronic diseases, and frequently declines in the first year after starting the drug [38,39,40,41,42,43]. Indeed, several reports have shown that nearly half of all patients who start antihypertensive drugs will stop taking their prescribed drug within 1 year [41, 44,45,46].
Patients with chronic diseases need a strong partnership with their physicians, pharmacists, and other healthcare professionals in order to achieve the desired long-term goals of treatment. Patients with good adherence to their antihypertensive drugs are more likely to experience the desired improvements in blood pressure, have a lower risk of adverse cardiovascular outcomes (all-cause hospitalization, cardiovascular hospitalization, cardiovascular revascularization, all-cause mortality, and cardiovascular mortality), and lower healthcare costs, compared with patients with poor adherence [27, 34, 47,48,49,50,51,52,53].
A meta-analysis of three decades of empirical research revealed that patients with good adherence to their antihypertensive drug had better blood pressure control than non-adherent patients to their antihypertensive therapies (odds ratio [OR]: 3.44; 95% confidence interval [CI]: 1.60–7.37) [32].
There is increasing evidence showing that patients with poor adherence to antihypertensive drugs are at much higher risk of adverse outcomes, including cardiovascular and all-cause hospitalization, than patients with good adherence [27, 53]. For instance, a cohort study showed that, among patients with low or moderate adherence, the risk of being hospitalized for cardiovascular-related diseases was increased by 33% (OR: 1.33; 95% CI: 1.25–1.41) and the risk of emergency visits by 45% (OR: 1.45; 95% CI: 1.33–1.58) compared with patients with adherence ≥80% [52]. Similarly, another cohort study revealed that a good level of adherence (>80%) to antihypertensive drugs significantly lowered the incidence of acute cardiovascular events, compared with a poor level of adherence (<40%) to antihypertensive drugs (hazard ratio [HR]: 0.62; 95% CI: 0.40–0.96) [54].
There is also evidence that the impact of non-adherence to antihypertensive agents is not only observed among patients in secondary prevention but also in primary prevention. Many observational studies based on administrative databases of patients in primary prevention reported that high adherence to antihypertensive drugs reduced the risk of cardiovascular diseases. First, high adherence to antihypertensive medications (≥80%) was associated with a risk reduction of 18% [RR: 0.82 (95% CI: 0.77–0.87)] of coronary artery disease compared to an adherence level of <20% [55]; second, high adherence (≥80%) to antihypertensive drugs significantly decreased the risk of cerebrovascular disease by 22% (rate ratio, 0.78; 95% CI, 0.70–0.87) compared to a lower level (<80%) [56]; and thirdly, high adherence level (≥80%) to antihypertensive therapy compared with lower adherence level (<80%) was associated with a risk reduction of chronic heart failure events (RR: 0.89; 0.80–0.99) [57]. In addition to the primary prevention, observational studies also reported significant result in secondary prevention. For instance, high adherence to antihypertensive therapy (≥80%) was mirrored by similar adherence to statins and antiplatelet agents and was associated with a lower risk of nonfatal vascular events after an ischemic stroke compared with lower adherence (>80%) (Rate Ratio 0.77 [0.70–0.86]) [58].
To date, however, few studies have investigated the impact of adherence to antihypertensive drugs on all-cause mortality or cardiovascular mortality [59]. In a cohort study using the Korean National Health Insurance Claims Databases, non-adherence to antihypertensive drugs (<80%) was associated with a significant increase in all-cause mortality and the risk of hospitalization for cardiovascular diseases (HR: 1.57; 95% CI: 1.40–1.76) [27]. The study of Kim et al., 2016 assessed the impact of adherence to antihypertensive drug on the risk of specific causes of cardiovascular-related death [60]. Among 33,728 Korean patients, 670 of them died because of ischemic heart disease or stroke during the follow-up period. Patient with poor adherence to antihypertensive drugs (<50%) were at increased risk of dying due to ischemic heart disease (HR: 1.64; 95% CI: 1.16–2.31), cerebral hemorrhage (HR: 2.19; 95% CI: 1.28–3.77), and cerebral infarction (HR: 1.92; 95% CI: 1.25–2.96) compared with patients with good adherence to antihypertensive drugs. The hazard ratios for hospitalization due to cardiovascular disease hospitalization were consistent with those for mortality.
Those results emphasize the importance of an effective management system and strategies to improve drug adherence in clinical practice. This is especially important when we consider that uncontrolled hypertension is also associated with increased risks of diabetes, stroke, atherosclerosis, and chronic kidney disease such as end stage of renal disease [61]. For instance, a high adherence level of 80% or more to antihypertensive agents compared to a lower one (<80%) was related to a risk reduction of end stage of renal disease (hazard ratio 0.67; 95% confidence intervals 0.54–0.83) [62].
They are always challenges with the estimation using real-world datasets because the impact of good adherence seems to be linked with positive clinical outcomes. But, we need to pay attention that the results of observational study designs may be biased by unmeasured residual confounding. The real-world evidence has the potential to improve efficiency across the drug development, and also the clinical usage decisions with appropriate method development for confounding such as super learning technologies. Super learning, an ensemble learning technique that can incorporate a greater number and complexity of variables, has been shown to improve outcome prediction modeling [63,64,65]. And also, the approach of “causal LASSO” aiming to replicate the context where treatment regimen has been randomized though unmeasured confounding that can impact the validity of the estimates, as is unavoidable in observational studies.
Technology advances and health care reform efforts are creating an opportunities to reshape the current system by which evidence generated from “Big Data” to better meet stakeholder needs but the reliability of those data needs to be considered. We can argue that validated and facile tools, based on large datasets, can help to inform at the real-time decision making to improve the clinical practice and would be invaluable but are currently limited.
3 Clinical Consequences of Associated Morbidities on Drug Adherence Level
Drug adherence is a complex phenomenon and may also be influenced by many factors, one of which is the coexistence of other chronic diseases [66]. On the one hand, several studies have demonstrated the protective effects of antihypertensive drugs in terms of the risks of cardiovascular morbidity and mortality [35, 67], and many patients fail to adhere to the prescribed drug, possibly due to asymptomatic and lifelong treatment of hypertension. But, on the other side, in many patients, hypertension rarely occurs in isolation. In some studies, it was noted that adherence to antihypertensive drugs was lower in patients with comorbidities [68, 69]. The existence of multiple chronic conditions is thought to reduce the likelihood of patients with hypertension adhering to the prescribed treatment [70]. It has also been noted that the presence of psychiatric conditions (e.g., depression) has adverse effects on adherence to antihypertensive drugs [66] and ultimately leads to poor blood pressure control [71].
The optimal management of common chronic cardiovascular diseases, including hypertension, coronary artery disease, and other relevant diseases such as diabetes mellitus, is important because they are among the most frequent causes of morbidity and mortality [72]. An important component of managing patients with multiple chronic diseases involves evaluating the patient’s adherence to the prescribed drugs. Poor adherence weakens the effectiveness of the prescribed drugs and is related to adverse health outcomes, increased healthcare expenditure (due to hospital admissions and an excess hospital burden), impaired quality of life, and an increased mortality rate [37, 47]. In recent years, several studies of non-adherence to drugs with proven efficacy in chronically ill patients have focused specifically on various chronic diseases, especially diabetes [73,74,75], chronic heart failure [76,77,78], neurologic and psychiatric diseases [79,80,81], cardiovascular disease [82,83,84,85,86], and chronic obstructive pulmonary disease [87, 88]. And, some of those studies have also investigated the factors that may influence adherence [86, 89, 90].
In real clinical setting, patients often have complex healthcare issues due to the presence of multiple chronic diseases and interrelated health and social difficulties, and such factors may directly or indirectly interfere with healthcare priorities, self-care, behavior, and ultimately adherence [91]. A Swedish primary care study noted that the presence cardiovascular morbidity was not associated with persistence to treatment, except in patients with diabetes, who actually showed greater persistence to antihypertensive drugs [92]. Meanwhile, other studies in Germany [93] and the United States [94] found no association between the presence of associated morbidities and the persistence [93] and the adherence [94] to antihypertensive therapy. However, several coexisting diseases, such as ischemic heart disease, chronic heart failure, and dysrhythmia, were linked to higher adherence levels [54, 95].
Recently, other studies demonstrated an association between the presence of multiple comorbidities and poor adherence to cardiovascular drugs [96, 97]. In a recent cross-sectional study of approximately 113,397 adults with hypertension assigned to public health service of primary care of a south region of Spain in 2010, about one-fifth of the patients (22,952) showed poor adherence (<80%) to antihypertensive drugs [98]. The predictors of poor adherence to antihypertensive drugs were being female, younger age, rural residency, low blood pressure, polypharmacy, and the presence of mental disorders. By contrast, the presence of other cardiovascular risk factors and more frequent medical visits per year were associated with better adherence to antihypertensive drugs [98]. And, Saadat et al., 2015 reported that the proportion of patients with a high level of adherence decreased from 22% among patients with no associated comorbidities to 11% among patients with 3–5 associated comorbidities [99].
Actually, the impact of coexisting disorders on adherence to antihypertensive drugs remains unclear. The highly variable and conflicting results may be due to the type of study population, the tool used to measure adherence, the inclusion of predictors of adherence, and the number and type of comorbidities [100]. Other predictors of drug adherence such as polypharmacy, healthcare use, site of residency, and social status need also to be simultaneously considered as potential confounding factors. Moreover, none of the studies mentioned above included more than ten comorbidities, and most of them focused on cardiovascular diseases and risk factors, underestimating the impact of multiple chronic diseases.
Thus, the overall message is that the impact of coexisting disorders and polypharmacy on adherence to antihypertensive drugs or other cardiovascular therapies remains unclear. And, further research works are needed not only on the impact of associated morbidities on adherence level but also on the impact of polypharmacy on clinical outcomes, healthcare use, and its related costs. The technology advances and big data sets give the opportunity to develop appropriate methodology to assess the impact of polypharmacy on clinical outcomes and its related impact on healthcare system.
4 Risk Prediction of Population Impact of Implementing Guidelines and Interventions on Drug Adherence
In 2014, the Eight Joint National Committee issued revised guidelines with three important changes to the 2003 guidelines that were aimed at shifting the focus of treatment from systolic blood pressure to diastolic blood pressure in patients aged <60 years and those aged >60 years, and in patients with diabetes or chronic kidney disease [101]. Based on these changes, implementation of the 2014 guidelines would reduce the number of patients eligible for antihypertensive treatment of 1% among younger adults and of 8% in older adults [102].
The American College of Cardiology and the American Heart Association recommended cost-effectiveness evaluations should be included with the recommendations of clinical guidelines [103]. Moran et al. [104] recently applied the competing risk Cox proportional hazard model proposed by the Framingham Heart Study to predict the clinical outcomes of patients without cardiovascular disease based on the following predictors: age, sex, diastolic and systolic blood pressure, high-density lipoprotein–cholesterol and low-density lipoprotein–cholesterol levels, the presence of chronic kidney disease, smoking status, the presence of diabetes, and the self-reported antihypertensive drug exposure. They estimated the outcomes of treating previously untreated patients aged 35–74 years over a 10-year period. The results suggest that the full implementation of the 2014 guidelines would prevent approximately 56,000 cardiovascular events and 13,000 deaths from cardiovascular causes per year, and would also provide an overall cost savings.
In addition to risk prediction based on clinical guidelines, other models, such as microsimulation, can be used to assess the population-level benefits of healthcare interventions [105]. For example, Fontil et al. [106] developed a Blood Pressure Control Model as a decision aid to assess and compare the impact of patient-level, physician-level, and system-level interventions in order to improve the clinical management of hypertension in the US population. The model combined evidence from published observational and experimental studies together with a national data survey. The Blood Pressure Control Model was also validated in two large clinical trials on the control of hypertension. The validated model was used to predict the outcomes of specific improvements, such as the frequency of medical visits, the probability of intensifying treatment according to the patient’s blood pressure, and the level of drug adherence. The authors reported that a substantial improvement in blood pressure control can be achieved if there are major improvements in the care process, especially increasing the frequency of face-to-face contact. In addition, improving the physician’s prescribing habits was expected to have a greater impact on blood pressure control than efforts to improve the patient’s level of adherence. The proposed model can help researchers and healthcare decision-makers to invest in interventional approaches, by targeting specific approaches used in the management of particular patient populations, and to help identify methods of meeting the public health goals for managing hypertension.
Future research works and development of interventions should assess how to build drug adherence improvement intervention in longer consultations required for patients with multiples morbidities. For instance, building predictive models with electronic medical records (including filled drug claims) incorporated in real time of the consultation will allow the physicians, pharmacist, healthcare professionals, and patients to discuss in real time of the predicted risk of outcomes and the observed level of medication adherence in order to improve the clinical practice outcome and adherence to medication. At the physician level, the prediction models could have the potential to enhance decision-making on medication prescribing, target high-risk individuals, and discuss strategies to promote treatment adherence with their patients. At the patient level, we expect that the risk prediction will motivate high-risk individuals to modify their medication adherence [64, 107, 108].
5 Clinical Consequences of Healthcare Professional and System on Drug Adherence
In the near future, we believe that eHealth, self-monitoring, prescriber continuity, adherence among complex patients, ensuring continuity of adherence by the pharmacy, and preventive strategies (e.g., diet, healthy behavioral and physical activities) will be important components of the strategies used to help meet the public health goals for the management of hypertension. Electronic tools based on prescription refills integrated into electronic medical records may provide innovative and objective tools to measure adherence and its clinical consequence.
Moreover, the medical home visit is also intended to provide a comprehensive, patient-centered, coordinated primary care that is combined with system-based quality improvement. This model is expected to increase primary care access, improve the quality of healthcare delivery, and reduce healthcare expenditure [109,110,111]. The potential benefits of the medical home visit are beginning to accrue, specifically in the improvement of the quality of healthcare and reducing inappropriate healthcare interventions [112]. The emerging evidence is promising, but the inherent benefits of the medical home among persons with multiple chronic disease is still largely unknown [113]. Nevertheless, the medical home could be used to review and improve adherence in patients with multiple chronic disease [114]. In fact, better healthcare coordination could help to reduce the number of prescribers and facilitate the prescription of optimal drugs. Drug reconciliation could improve the management of the prescribed drugs by the clinicians and pharmacists, may reduce polypharmacy and drug complexity, and may ultimately improve drug adherence.
6 Clinical Consequences of Implementing Patient-Centered Approaches and Personalized Evaluations of Adherence to Antihypertensive Drugs
Patients with multiple comorbidities, especially cardiometabolic diseases, represent a particular challenge in clinical practice because a combination of drugs is often required to prevent and treat the diseases and their complications. A typical patient with cardiometabolic diseases may therefore require a treatment regimen composed of numerous drugs. Such patients may also require treatment for other comorbidities. Indeed, the number of elderly patients prescribed multiple drugs is rising. In 2009, 63% of patients receiving public drug insurance in six provinces in Canada claimed ≥5 classes of drugs while 23% had claims for ≥10 classes of drugs [115]. Notably, the number of classes of drugs prescribed to elderly patients increased with age: in 2009, 18% of patients aged 65–74 years, 26% of patients aged 75–84 years, and 30% of patients aged ≥85 years had claims for ≥10 drug classes.
Using multiple drugs may lead to problems such as inappropriate dosing, drug interactions, adverse drug reactions, treatment failure, and patient non adherence. The burden of drug-related morbidity in countries like Canada is enormous in terms of healthcare expenditure and avoidable morbidity and mortality [116, 117]. The US Food and Drug Administration (FDA) and its Center for Drug Evaluation and Research estimated that the fourth leading cause of death is inappropriate use of drugs [118]. The FDA also reported that as many as 110,000 deaths per year might be due to inappropriate use of drugs. Extrapolating these estimates to Canada suggests that about 10,000 deaths per year might be related to inappropriate use of drugs, and many of these deaths could be avoided by optimizing the patients’ treatment regimens. Studies, especially in the elderly, have estimated that up to 30% of hospital admissions are attributable to these unintended events [116, 117]. Several factors may explain this staggering statistic: (1) concomitant use of multiple drugs in an aging population with comorbid conditions; (2) inadvertent drug–drug interactions; and (3) high intersubject variability in the pharmacodynamic and pharmacokinetic properties of the drugs. It is well documented that the risk of drug–drug interactions increases as a function of the number of prescribed drugs: use of >5 drugs increases the risk of drug–drug interactions by four times and the use of >8 drugs increases the risk by eight times [119]. The reactions to drugs also vary between patients, and are frequently attributable to the different sequences of genes involved in the metabolism or biological effect of individual drugs. Indeed, single nucleotide polymorphisms in specific genes have been identified as major determinants of the pharmacokinetics and pharmacodynamics of drugs that are routinely administered to patients with cardiometabolic diseases, including oral antidiabetic drugs, antihypertensive drugs, statins, anticoagulants, antiplatelet drugs, and antidepressants.
The regulatory drug approval process for industry requires that in vitro and in vivo studies be conducted to test for drug–drug interactions to facilitate the prediction and prevention of these interactions. Despite the importance of drug–drug interactions to patients and industry, most in vivo and in vitro studies evaluate only one combination (two drug profiles) of potentially interacting drugs at a time. Thus, these studies cannot be generalized to patients with chronic conditions who are taking complex multidrug regimens. In addition, these studies do not consider the high intersubject variability in the pharmacodynamic effects of drugs. These limitations are very important, and new guidelines issued by the FDA recommend improvements to pharmacokinetic tests in elderly patients and in patients with multiple comorbidities.
Until recently, there was no simple way to make evidence-based predictions about the likelihood or severity of clinically important interactions in patients on multidrug regimens. The rationale for testing potential multidrug interactions is to provide clinical evidence that can support clinical decision-making in the context of risk reduction in patients on multidrug regimens [120,121,122]. A newly developed technology (InterMed-Rx) incorporates relevant pharmacokinetic information (bioavailability, urinary excretion, drug metabolism pathways, and drug transporters) relevant to all drugs available in Canada, and healthcare professionals to predict possible drug–drug interactions among various drugs [120]. Recent advances in molecular biology testing and genetics, as well as knowledge integration and analysis technologies, have allowed us to develop improved decision trees and algorithms to establish optimized treatment strategies, which integrate all relevant pharmacogenetic, pharmacokinetic, and pharmacodynamic information related to individual drugs. These strategies consider genetic information, environmental factors, and the patient’s unique clinical condition.
In addition to patient-centered approach and personalized evaluation, other factors need also to be discussed. Despite increasing familiarity with international guidelines, physicians do not always adhere to the guidelines and they are not always fully implemented in clinical practice [123,124,125]. The failure to adhere to treatment guidelines may represent a conscious decision by the physician when treating a patient. The physician’s knowledge of the guidelines is also a major factor that will influence the physician’s ability to adhere them [126]. This not only applies to physicians, but may also be relevant to pharmacists and other healthcare professionals who are involved in the management of patients with hypertension. It is also possible that the physician’s decisions are influenced by the patient’s concerns and preferences [125, 127, 128]. Clearly, comprehensive analyses of the treatment practices of physicians, pharmacists, and other healthcare professionals involved in the management of patients with hypertension (with or without associated morbidities) are needed if we hope to propose remedial and curative measures to support healthcare professionals in the management of these patients [129].
Moreover, more precise algorithms for gendered approaches may lead to a more specific and effective strategic treatment [130]. For doing so, more evidence-based clinical trial data are required, and the implementation of new gender-sensitive finding into the research and healthcare strategies is needed [130].
7 Clinical Consequences of Changes to Healthcare Professional- and Policy-Related Factors on Adherence
Despite the availability of clinical guidelines, clinical awareness of hypertension, and self-awareness of hypertension, the treatment and control of hypertension are far from adequate [131,132,133,134]. Some of the major challenges are the number of guidelines on this topic and the quality of these guidelines [135,136,137,138]. Al-Ansary et al. wrote a systematic review [131] on the quality, methodology, and consistency of the recommendations of several recent national clinical practice guidelines on the diagnosis, assessment, and management of hypertension. The recommendations for non-pharmacological management of hypertension were fairly consistent across the guidelines. However, the recommendations for the initial intention to treat, changes to treatment, and multidrug regimens varied among the guidelines. Moreover, important aspects of the management of drug resistance were reported in just 50% of 11 clinical practice guidelines. The variations in the methodologic quality of the guidelines suggest that their implementation may not result in worse management or better outcomes. The authors proposed that more effort is needed in order to establish a realistic approach and to be able to implement high-quality clinical practice guidelines within a national context.
One important reason why the healthcare system does not implement prevention and treatment guidelines constantly may be due to the lack of a patient-centered approach and prioritization at the point of care. We need to evaluate the time needs to fully assess and implement all clinical relevant recommendations in order to improve their implementation [139,140,141,142,143,144,145,146,147,148,149,150,151]. A more systematic approach to personalizing and prioritizing guidelines may improve patient outcomes [152]. However, several studies have suggested that clinicians and healthcare professionals need to know which guidelines provide the greatest benefit to each patient, and it may be difficult to prioritize the most appropriate guideline [153,154,155,156].
In addition to implement treatment guidelines, the enforcement of outcome predictive models derived from numerical data in real time could certainly change the clinical practice model and the optimal implementation of guidelines to better organize healthcare, and improve adherence level and health-related outcomes [64, 107, 108]. We also need to fully understand the impact the implementation of predictive models in clinical practice at the patient-, physician-, pharmacist-, and healthcare professional level.
Moreover, we need to have more understanding of the role in initial medication adherence of chronic care, health system, health professionals, and patient factors that collectively influence the treatment trajectory. Patient adherence to prescribed dosing regimen is recognized as a significant challenge in the healthcare field. Objective measures of patient adherence patterns have the potential to facilitate product design to ameliorate these behaviors in real clinical setting and also to impact clinical trial design in a way that accounts for such patterns.
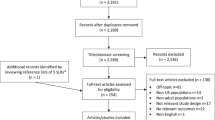
Strategies for the management of hypertension should continue to not only focus on preventable and modifiable risk factors but also consider the societal issues [157]. The challenge in global health practices will include challenge for health systems (governance, actors, and patients) and sustainable economic models, access to precision medicine (diagnostic strategies, precision treatment, effectiveness, and safety), health science (data access, data science, research development), new information channels (training, formation, quality of formation), and all ethical issues relevant to the challenge in global health practices (Fig. 22.1).
References
World Health Organization. A global brief on hypertension. Silent killer, global public health crisis. 2016.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55.
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. p. 1–62.
Heidenreich PA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44.
Gaziano TA, Bitton A, Anand S, Weinstein MC, International Society of Hypertension. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–7.
Townsend N, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37:3232–45.
World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–9.
Lewanczuk R. Innovations in primary care: implication for hypertension detection and treatment. Can J Cardiol. 2006;22:614–6.
Gee ME, et al. Antihypertensive medication use, adherence, stops, and starts in Canadians with hypertension. Can J Cardiol. 2012;28:383–9.
Wolf-Maier K, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–9.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–50.
Egan BM, Zhao Y. Different definitions of prevalent hypertension impact: the clinical epidemiology of hypertension and attainment of Healthy People goals. J Clin Hypertens (Greenwich). 2013;15:154–61.
Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–58.
Resnick HE, Shorr RI, Kuller L, Franse L, Harris TB. Prevalence and clinical implications of American Diabetes Association-defined diabetes and other categories of glucose dysregulation in older adults: the health, aging and body composition study. J Clin Epidemiol. 2001;54:869–76.
Smith NL, et al. Glucose, blood pressure, and lipid control in older people with and without diabetes mellitus: the Cardiovascular Health Study. J Am Geriatr Soc. 2002;50:416–23.
de Rekeneire N, et al. Racial differences in glycemic control in a well-functioning older diabetic population: findings from the Health, Aging and Body Composition Study. Diabetes Care. 2003;26:1986–92.
Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55:1056–65.
Robinson JG, Booth B. Statin use and lipid levels in older adults: National Health and Nutrition Examination Survey, 2001 to 2006. J Clin Lipidol. 2010;4:483–90.
Egan BM, et al. Prevalence of optimal treatment regimens in patients with apparent treatment-resistant hypertension based on office blood pressure in a community-based practice network. Hypertension. 2013;62:691–7.
Leal J, Luengo-Fernandez R, Gray A, Petersen S, Rayner M. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J. 2006;27:1610–9.
Mennini FS, et al. Cost of poor adherence to anti-hypertensive therapy in five European countries. Eur J Health Econ. 2015;16:65–72.
Lim SS, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Breekveldt-Postma NS, et al. Effect of persistent use of antihypertensives on blood pressure goal attainment. Curr Med Res Opin. 2008;24:1025–31.
LaFleur J, Oderda GM. Methods to measure patient compliance with medication regimens. J Pain Palliat Care Pharmacother. 2004;18:81–7.
McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36:1331–6.
Shin S, et al. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res. 2013;36:1000–5.
Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49:69–75.
Krousel-Wood MA, Muntner P, He J, Whelton PK. Primary prevention of essential hypertension. Med Clin North Am. 2004;88:223–38.
Chobanian AV, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10:348–54.
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811.
Lawes CM, Vander Hoorn S, Rodgers A, International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
Blood Pressure Lowering Treatment Trialists’ Collaboration, et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336:1121–3.
Law M, Wald N, Morris J. Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy. Health Technol Assess. 2003;7:1–94.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Burke TA, et al. Discontinuation of antihypertensive drugs among newly diagnosed hypertensive patients in UK general practice. J Hypertens. 2006;24:1193–200.
Benner JS, et al. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–61.
Perreault S, et al. Persistence and determinants of statin therapy among middle-aged patients free of cardiovascular disease. Eur J Clin Pharmacol. 2005;61:667–74.
Perreault S, et al. Persistence with treatment in newly treated middle-aged patients with essential hypertension. Ann Pharmacother. 2005;39:1401–8.
Perreault S, et al. Persistence and determinants of statin therapy among middle-aged patients for primary and secondary prevention. Br J Clin Pharmacol. 2005;59:564–73.
Simard P, et al. Persistence and adherence to oral antidiabetics: a population-based cohort study. Acta Diabetol. 2015;52:547–56.
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114–7.
Mazzaglia G, et al. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens. 2005;23:2093–100.
Sung SK, et al. First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther. 2009;31:1309–20.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30.
Liu L, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009;32:1032–40.
Ho PM, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155:772–9.
Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract. 2008;62:76–87.
Dragomir A, et al. Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Med Care. 2010;48:418–25.
Pittman DG, Tao Z, Chen W, Stettin GD. Antihypertensive medication adherence and subsequent healthcare utilization and costs. Am J Manag Care. 2010;16:568–76.
Wu PH, et al. Relationship of blood pressure control and hospitalization risk to medication adherence among patients with hypertension in Taiwan. Am J Hypertens. 2010;23:155–60.
Mazzaglia G, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120:1598–605.
Perreault S, et al. Adherence level of antihypertensive agents in coronary artery disease. Br J Clin Pharmacol. 2010;69:74–84.
Kettani FZ, et al. Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke. 2009;40:213–20.
Perreault S, et al. Better adherence to antihypertensive agents and risk reduction of chronic heart failure. J Intern Med. 2009;266:207–18.
Perreault S, et al. Adherence to antihypertensive agents after ischemic stroke and risk of cardiovascular outcomes. Neurology. 2012;79:2037–43.
Wong MC, et al. Drug adherence and the incidence of coronary heart disease- and stroke-specific mortality among 218,047 patients newly prescribed an antihypertensive medication: a five-year cohort study. Int J Cardiol. 2013;168:928–33.
Kim S, et al. Medication adherence and the risk of cardiovascular mortality and hospitalization among patients with newly prescribed antihypertensive medications. Hypertension. 2016;67:506–12.
Schafer HH, Scheunert U. Costs of current antihypertensive therapy in Switzerland: an economic evaluation of 3,489 patients in primary care. Swiss Med Wkly. 2013;143:w13854.
Roy L, et al. Adherence to antihypertensive agents improves risk reduction of end-stage renal disease. Kidney Int. 2013;84:570–7.
van der Laan MJ, Polley EC, Hubbard AE. Super learner. Stat Appl Genet Mol Biol. 2007;6:Article25.
Obermeyer Z, Emanuel EJ. Predicting the future—big data, machine learning, and clinical medicine. N Engl J Med. 2016;375:1216–9.
Kennedy EH, Ma Z, McHugh MD, Small DS. Nonparametric methods for doubly robust estimation of continuous treatment effects. J R Stat Soc Ser B. 2017;79(4):1229–45.
Krousel-Wood M, et al. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010;40:248–57.
ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31:1925–38.
Ghembaza MA, Senoussaoui Y, Tani MK, Meguenni K. Impact of patient knowledge of hypertension complications on adherence to antihypertensive therapy. Curr Hypertens Rev. 2014;10:41–8.
An J, Nichol MB. Multiple medication adherence and its effect on clinical outcomes among patients with comorbid type 2 diabetes and hypertension. Med Care. 2013;51:879–87.
Carretero OA, Oparil S. Essential hypertension: part II: treatment. Circulation. 2000;101:446–53.
Scalco AZ, Scalco MZ, Azul JB, Lotufo Neto F. Hypertension and depression. Clinics (Sao Paulo). 2005;60:241–50.
Munger MA, Van Tassell BW, LaFleur J. Medication nonadherence: an unrecognized cardiovascular risk factor. MedGenMed. 2007;9:58.
Jamous RM, et al. Adherence and satisfaction with oral hypoglycemic medications: a pilot study in Palestine. Int J Clin Pharm. 2011;33:942–8.
Ahmad NS, Ramli A, Islahudin F, Paraidathathu T. Medication adherence in patients with type 2 diabetes mellitus treated at primary health clinics in Malaysia. Patient Prefer Adherence. 2013;7:525–30.
Simard P, et al. Impact of adherence to oral antidiabetics on all-cause mortality: a population based study. Value Health. 2015;18:A611.
Dunlay SM, Eveleth JM, Shah ND, McNallan SM, Roger VL. Medication adherence among community-dwelling patients with heart failure. Mayo Clin Proc. 2011;86:273–81.
Wu JR, Lennie TA, Dekker RL, Biddle MJ, Moser DK. Medication adherence, depressive symptoms, and cardiac event-free survival in patients with heart failure. J Card Fail. 2013;19:317–24.
Perreault S, et al. Older adults with heart failure treated with carvedilol, bisoprolol, or metoprolol tartrate: risk of mortality. Pharmacoepidemiol Drug Saf. 2017;26:81–90.
Dibonaventura M, Gabriel S, Dupclay L, Gupta S, Kim E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry. 2012;12:20.
Sweileh WM, et al. Self-reported medication adherence and treatment satisfaction in patients with epilepsy. Epilepsy Behav. 2011;21:301–5.
De las Cuevas C, Penate W, Sanz EJ. Risk factors for non-adherence to antidepressant treatment in patients with mood disorders. Eur J Clin Pharmacol. 2014;70:89–98.
Cooper DC, et al. Antidepressant adherence and risk of coronary artery disease hospitalizations in older and younger adults with depression. J Am Geriatr Soc. 2014;62:1238–45.
Hashmi SK, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One. 2007;2:e280.
Li WW, Kuo CT, Hwang SL, Hsu HT. Factors related to medication non-adherence for patients with hypertension in Taiwan. J Clin Nurs. 2012;21:1816–24.
Holt E, et al. Sex differences in barriers to antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc. 2013;61:558–64.
Wang W, Lau Y, Loo A, Chow A, Thompson DR. Medication adherence and its associated factors among Chinese community-dwelling older adults with hypertension. Heart Lung. 2014;43:278–83.
Agh T, Inotai A, Meszaros A. Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respiration. 2011;82:328–34.
Blais L, Forget A, Ramachandran S. Relative effectiveness of budesonide/formoterol and fluticasone propionate/salmeterol in a 1-year, population-based, matched cohort study of patients with chronic obstructive pulmonary disease (COPD): effect on COPD-related exacerbations, emergency department visits and hospitalizations, medication utilization, and treatment adherence. Clin Ther. 2010;32:1320–8.
Jansa M, et al. Multidimensional analysis of treatment adherence in patients with multiple chronic conditions. A cross-sectional study in a tertiary hospital. Patient Educ Couns. 2010;81:161–8.
Tsai KT, et al. Medication adherence among geriatric outpatients prescribed multiple medications. Am J Geriatr Pharmacother. 2012;10:61–8.
Tinetti ME, Bogardus ST Jr, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351:2870–4.
Qvarnstrom M, et al. Persistence to antihypertensive drug treatment in Swedish primary healthcare. Eur J Clin Pharmacol. 2013;69:1955–64.
Hasford J, Schroder-Bernhardi D, Rottenkolber M, Kostev K, Dietlein G. Persistence with antihypertensive treatments: results of a 3-year follow-up cohort study. Eur J Clin Pharmacol. 2007;63:1055–61.
Morris AB, et al. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy. 2006;26:483–92.
Chapman RH, Petrilla AA, Benner JS, Schwartz JS, Tang SS. Predictors of adherence to concomitant antihypertensive and lipid-lowering medications in older adults: a retrospective, cohort study. Drugs Aging. 2008;25:885–92.
Wong MC, et al. The association between multimorbidity and poor adherence with cardiovascular medications. Int J Cardiol. 2014;177:477–82.
Wong MC, et al. Factors associated with multimorbidity and its link with poor blood pressure control among 223,286 hypertensive patients. Int J Cardiol. 2014;177:202–8.
Calderon-Larranaga A, et al. Non-adherence to antihypertensive medication: the role of mental and physical comorbidity. Int J Cardiol. 2016;207:310–6.
Saadat Z, et al. Adherence to antihypertensives in patients with comorbid condition. Nephrourol Mon. 2015;7:e29863.
Stewart M, Fortin M, Britt HC, Harrison CM, Maddocks HL. Comparisons of multi-morbidity in family practice—issues and biases. Fam Pract. 2013;30:473–80.
James PA, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Navar-Boggan AM, Pencina MJ, Williams K, Sniderman AD, Peterson ED. Proportion of US adults potentially affected by the 2014 hypertension guideline. JAMA. 2014;311:1424–9.
Anderson JL, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. Circulation. 2014;129:2329–45.
Moran AE, et al. Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med. 2015;372:447–55.
Abraham JM. Using microsimulation models to inform U.S. health policy making. Health Serv Res. 2013;48:686–95.
Fontil V, et al. Simulating strategies for improving control of hypertension among patients with usual source of Care in the United States: the blood pressure control model. J Gen Intern Med. 2015;30:1147–55.
Jha AK. Learning from the past to improve VA health care. JAMA. 2016;315:560–1.
Rumsfeld JS, Joynt KE, Maddox TM. Big data analytics to improve cardiovascular care: promise and challenges. Nat Rev Cardiol. 2016;13:350–9.
Hussey PS, Eibner C, Ridgely MS, McGlynn EA. Controlling U.S. health care spending—separating promising from unpromising approaches. N Engl J Med. 2009;361:2109–11.
Fields D, Leshen E, Patel K. Analysis & commentary. Driving quality gains and cost savings through adoption of medical homes. Health Aff (Millwood). 2010;29:819–26.
Rosenthal MB, et al. Will the patient-centered medical home improve efficiency and reduce costs of care? A measurement and research agenda. Med Care Res Rev. 2010;67:476–84.
Peikes D, Zutshi A, Genevro JL, Parchman ML, Meyers DS. Early evaluations of the medical home: building on a promising start. Am J Manag Care. 2012;18:105–16.
Sidorov JE. The patient-centered medical home for chronic illness: is it ready for prime time? Health Aff (Millwood). 2008;27:1231–4.
Beadles CA, et al. Do medical homes increase medication adherence for persons with multiple chronic conditions? Med Care. 2015;53:168–76.
https://secure.cihi.ca/free_products/HCIC_2011_seniors_report_en.pdf. 2011.
Committee on Quality of Health Care in America, Institute of Medicine. To err is human: building a safer health system. Washington, DC: National Academies Press; 2000.
Baker GR, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170:1678–86.
Center for Drug Evaluation And Research (CDER), FDA. http://www.Fda.Gov/drugs/developmentapprovalprocess/developmentresources/druginteractionslabeling/ucm110632.Htm#adrs: Prevalence and incidence.
Juurlink DN, Mamdani M, Kopp A, Laupacis A, Redelmeier DA. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003;289:1652–8.
Turgeon J, Michaud V. Clinical decision support systems: great promises for better management of patients’ drug therapy. Expert Opin Drug Metab Toxicol. 2016;12:993–5.
Zakrzewski-Jakubiak H, et al. Detection and prevention of drug-drug interactions in the hospitalized elderly: utility of new cytochrome p450-based software. Am J Geriatr Pharmacother. 2011;9:461–70.
Doan J, Zakrzewski-Jakubiak H, Roy J, Turgeon J, Tannenbaum C. Prevalence and risk of potential cytochrome P450-mediated drug-drug interactions in older hospitalized patients with polypharmacy. Ann Pharmacother. 2013;47:324–32.
Wang L. Physician-related barriers to hypertension management. Med Princ Pract. 2004;13:282–5.
Mehta SS, Wilcox CS, Schulman KA. Treatment of hypertension in patients with comorbidities: results from the study of hypertensive prescribing practices (SHyPP). Am J Hypertens. 1999;12:333–40.
Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med. 2000;160:2281–6.
Milchak JL, Carter BL, James PA, Ardery G. Measuring adherence to practice guidelines for the management of hypertension: an evaluation of the literature. Hypertension. 2004;44:602–8.
McAlister FA, O’Connor AM, Wells G, Grover SA, Laupacis A. When should hypertension be treated? The different perspectives of Canadian family physicians and patients. CMAJ. 2000;163:403–8.
Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–86.
Ragot S, Beneteau M, Guillou-Bonnici F, Herpin D. Prevalence and management of hypertensive patients in clinical practice: cross-sectional registry in five countries outside the European Union. Blood Press. 2016;25:104–16.
EUGenMed Cardiovascular Clinical Study Group, et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37:24–34.
Al-Ansary LA, et al. A systematic review of recent clinical practice guidelines on the diagnosis, assessment and management of hypertension. PLoS One. 2013;8:e53744.
Cai L, Liu A, Zhang L, Li S, Wang P. Prevalence, awareness, treatment, and control of hypertension among adults in Beijing, China. Clin Exp Hypertens. 2012;34:45–52.
Whelton PK, He J, Muntner P. Prevalence, awareness, treatment and control of hypertension in North America, North Africa and Asia. J Hum Hypertens. 2004;18:545–51.
Alsuwaida A, Alghonaim M. Gender disparities in the awareness and control of hypertension. Clin Exp Hypertens. 2011;33:354–7.
Wang YR, Alexander GC, Stafford RS. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007;167:141–7.
Fervers B, et al. Predictors of high quality clinical practice guidelines: examples in oncology. Int J Qual Health Care. 2005;17:123–32.
Watine J, et al. Conflict between guideline methodologic quality and recommendation validity: a potential problem for practitioners. Clin Chem. 2006;52:65–72.
Nagy E, et al. Do guidelines for the diagnosis and monitoring of diabetes mellitus fulfill the criteria of evidence-based guideline development? Clin Chem. 2008;54:1872–82.
Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42:1871–94.
Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–41.
Maciosek MV, et al. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52–61.
Ostbye T, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209–14.
Flocke SA, Frank SH, Wenger DA. Addressing multiple problems in the family practice office visit. J Fam Pract. 2001;50:211–6.
Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15-minute visit. Arch Intern Med. 2008;168:1843–52.
Pimlott N. Preventive care: so many recommendations, so little time. CMAJ. 2005;173:1345–6.
Tarn DM, et al. How much time does it take to prescribe a new medication? Patient Educ Couns. 2008;72:311–9.
Hadley J, Mitchell JM, Sulmasy DP, Bloche MG. Perceived financial incentives, HMO market penetration, and physicians’ practice styles and satisfaction. Health Serv Res. 1999;34:307–21.
Nutting PA, Rost K, Smith J, Werner JJ, Elliot C. Competing demands from physical problems: effect on initiating and completing depression care over 6 months. Arch Fam Med. 2000;9:1059–64.
Linzer M, et al. Managed care, time pressure, and physician job satisfaction: results from the physician worklife study. J Gen Intern Med. 2000;15:441–50.
Mechanic D. Physician discontent: challenges and opportunities. JAMA. 2003;290:941–6.
Nutting PA, et al. Competing demands in the office visit: what influences mammography recommendations? J Am Board Fam Pract. 2001;14:352–61.
Taksler GB, Keshner M, Fagerlin A, Hajizadeh N, Braithwaite RS. Personalized estimates of benefit from preventive care guidelines: a proof of concept. Ann Intern Med. 2013;159:161–8.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29:725–31.
O’Connor PJ. Setting evidence-based priorities for diabetes care improvement. Int J Qual Health Care. 2003;15:283–5.
Braithwaite RS, Concato J, Chang CC, Roberts MS, Justice AC. A framework for tailoring clinical guidelines to comorbidity at the point of care. Arch Intern Med. 2007;167:2361–5.
Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296:2336–42.
Melgarejo JD, et al. Prevalence, treatment, and control rates of conventional and ambulatory hypertension across 10 populations in 3 continents. Hypertension. 2017;70:50–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Perreault, S. (2018). Global Clinical Consequences of Poor Adherence. In: Burnier, M. (eds) Drug Adherence in Hypertension and Cardiovascular Protection. Updates in Hypertension and Cardiovascular Protection. Springer, Cham. https://doi.org/10.1007/978-3-319-76593-8_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-76593-8_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-76592-1
Online ISBN: 978-3-319-76593-8
eBook Packages: MedicineMedicine (R0)