Abstract
For the most part, there are no specific guidelines for the management of upper gastrointestinal symptoms and disorders in the diabetic patient. Given the impact of hyperglycemia on upper gastrointestinal motility, attention must always be paid to glycemic control. Conversely, the impact of poor oral intake and recurrent vomiting on blood sugar levels and overall nutritional status must, at all times, be borne in mind. In the assessment of the diabetic with GERD, the possible contribution of impaired motility to symptomatology and its implications for therapy must be remembered. Many options are available for the symptomatic and supportive management of diabetic gastroparesis; their efficacy is often supported by a slim evidence base.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Diabetes
- Gastroparesis
- Esophageal dysmotility
- GERD
- Prokinetic
- Proton pump inhibitor
- Gastric electrical stimulation
- Pylorus
Esophageal Dysmotility
It is likely that the most clinically relevant aspect of the disorders of esophageal motility that have been described in diabetes is their potential contribution to the development and/or progression of GERD. With the possible exception of esophagogastric outflow obstruction whose association with diabetes needs to be confirmed [1], the esophageal motility abnormalities described in GERD are relatively nonspecific [2] and not amenable to specific pharmacotherapy. Effective management of GERD may, in theory at least, ameliorate motor dysfunction .
GERD
There are no specific guidelines for identifying and managing GERD in diabetic patients given the absence of any real body of literature relating to the concurrence of these entities. Guidelines for the management of GERD, in general, should therefore be followed [3].
Proton pump inhibitors (PPIs) have become the mainstay in the management of symptomatic acid reflux and, especially, reflux esophagitis and its complications [3]. However, between 10 and 40% of GERD sufferers will fail to respond to a full course of a PPI in its standard, recommended dose [4]. These therapy-resistant patients pose a significant therapeutic challenge. PPI failure is more likely among type 2 diabetes patients than among nondiabetic GERD sufferers [5] and, in this population, was significantly associated with female gender, increased BMI, and general comorbidities. There does not appear to be a discernible relationship between PPI-refractory GERD and the duration of diabetes or the presence of any of its long-term complications [5].
One issue that will come up with regard to the use of PPIs, especially in the long term, among diabetics is risk. Of late, long-term PPI use has been linked with several entities that diabetics are already at increased risk for—enteric infections, Clostridium difficile infection, myocardial infarction, ischemic stroke, kidney injury, osteoporosis, and dementia [6]. For many of these, a cause and effect relationship has not been established and studies reporting these associations have been criticized on several grounds, including a failure to account for confounding factors [6,7,8]. Furthermore, some of these associations have not survived more rigorous study [9] and may be limited to certain at-risk populations [10]. Finally, in many instances, the effect size is small, even in positive studies [6]. On the positive side, one, albeit retrospective, study reported a significant (0.6%) decrease in the level of glycated hemoglobin (HbA1c) in diabetic patients with GERD treated with a PPI [11].
If surgery becomes a consideration in the diabetic patient with GERD, it stands to reason that esophageal motility should be carefully assessed in view of the high prevalence of esophageal motor dysfunction in this patient population.
Esophageal Candidiasis
Candidiasis limited to the oropharyngeal cavity can be treated with nystatin in a swish-and-swallow fashion [12]. In cases with persistent symptoms, oral fluconazole should be initiated. Endoscopically confirmed esophageal candidiasis should be treated with oral fluconazole [13]. Similarly, oral thrush with associated odynophagia is highly suggestive of esophageal involvement and, in of itself, should be an indication for fluconazole therapy [14].
Gastroparesis
General Aspects
As described in Chap. 5, relationships between blood sugar levels and gastric emptying are complex. What is clear, however, is that, first, poor glycemic control is a predictor of gastrointestinal symptoms in diabetes [15, 16] and, second, that hyperglycemia disturbs gastric motor function [17]. Consequently, tight control of blood sugar levels under the supervision of a diabetologist should be a fundamental component of the management of gastroparesis [18]. Interestingly and surprisingly, longitudinal studies showed no impact of glycemic control on gastric emptying rate [19,20,21]—yet another diabetic gastroparesis conundrum.
In the management of acute severe episodes of gastroparesis, which often occur almost cyclically in some diabetics, the correction of fluid and electrolyte deficits is critical and it is remarkable how many will improve quickly with this measure combined with blood sugar control, antiemetics, and prokinetics , as needed.
In the longer term, the management of gastroparesis requires a comprehensive and targeted approach that combines glycemic control with dietary modification (s) and pharmacological therapy and aims at optimizing nutritional status and glycemic control and alleviating symptoms as much as possible [22]. Although there are no prospective randomized controlled trials, dietary modifications are recommended based on physiological principles [23]: small frequent meals, low-fat and fiber food, and increased calorie intake in liquid form are generally recommended [24, 25]. Regardless of the route of food intake, nutritional status should be carefully monitored on a regular basis. In patients with refractory symptoms in whom oral intake is insufficient, poorly tolerated direct enteral feeding into the small intestine should be considered via the naso-enteric route before endoscopic or surgical placement of a jejunostomy is considered [22]. It has been the experience of these authors that both endoscopically- and surgically-placed jejunostomy catheters are prone to failure and require to be replaced on a regular basis—the decision to embark on this path should, therefore, not be taken lightly.
Pharmacotherapy
In the absence of a curative therapy, available therapeutic approaches to gastroparesis focus on the alleviation of symptoms [26]. For decades and depending on local availability, the prokinetic agents metoclopramide, erythromycin, and domperidone have been the mainstays of the gastroparesis treatment algorithm .
Metoclopramide has a number of advantages. First, it is not only a foregut prokinetic through 5-hydroxytryptamine (5-HT) type 4 effects on the stomach but also exerts central antiemetic effects via antagonism of dopamine type 2 and 5-HT3 receptors on vagal and brainstem pathways [22, 25, 27]. Second, metoclopramide is available for administration by oral, subcutaneous, and intravenous routes; the latter two being especially useful in the patient who has already commenced vomiting. One strategy adopted in some centers is to have the patient self-inject metoclopramide subcutaneously once an episode of nausea and vomiting begins in an attempt to abort its progression. Unfortunately, the medium- to long-term use of metoclopramide is limited by neurological adverse events including drowsiness, agitation, tardive dyskinesia, and rarely acute dystonias; some of these extrapyramidal adverse events may not be reversible [28]. Domperidone, also a dopamine D2 antagonist, does not cross the blood–brain barrier, does not result in these neurological effects but does still exert antiemetic effects via its actions on the vomiting center which lies on the blood side of the blood–brain barrier [29]. Though widely available in Europe and elsewhere for decades, domperidone has never been approved by the Food and Drugs Administration for use in the United States. Lately, a cloud has also descended on domperidone in relation to its association with Q-T prolongation and related dysrhythmias [30].
Erythromycin is a macrolide antibiotic, which accelerates gastric emptying by acting as a motilin receptor agonist [31]. When administrated intravenously, it is a potent prokinetic and has been used extensively in the short-term, acute treatment of hospitalized patients with severe gastroparesis [32]. Longterm efficacy is limited by poor bioavailability and the development of tolerance due to the downregulation of motilin receptors [32]. More limited data suggests that azithromycin, a related macrolide, may be more effective when given orally in the medium term [33].
Following the demise of cisapride, a drug that was widely regarded as an effective prokinetic, because of Q-T prolongation-related cardiac toxicity [34], the search has been on to find a safe and effective upper gastrointestinal prokinetic—many have been proposed but few have survived, mainly on the basis of a lack of convincing evidence of efficacy. Mosapride , for example, was shown to accelerate gastric emptying [35] and showed efficacy in a small study of interferon-induced gastroparesis [36] but failed to provide symptom relief, in dyspepsia, in general [37]. To date, cinitapride, a 5-HT4 agonist and dopamine 2 antagonist, has shown some promise in functional dyspepsia but has not been evaluated in gastroparesis [38]. Itopride is a novel prokinetic agent that acts as an acetylcholinesterase inhibitor and dopamine D2 receptor antagonist and has been shown to accelerate liquid and solid emptying in patients with long-standing diabetes [39]; yet again, this prokinetic effect has not translated into clinical efficacy in dyspepsia [40]. Acotiamide , a muscarinic antagonist and acetylcholinesterase inhibitor devoid of Q-T effects [41], has also been shown to accelerate gastric emptying [42] but, to date, has not been evaluated in diabetic gastroparesis. One agent that does show promise is the ghrelin agonist, relamorelin, which accelerates gastric emptying [43] but also produces symptomatic improvement in gastroparesis [44].
A variety of antiemetic agents are used in the symptomatic control of nausea and vomiting in gastroparesis including 5HT3 antagonists (ondansetron and granisetron), phenothiazine derivatives (e.g., promethazine), cannabinoids (dronabinol), anticholinergics (such as transdermal scopolamine), and antihistamines (such as diphenhydramine). There are few if any controlled or comparative trials to guide the physician—empirical trials are the order of the day [25, 27]. The neurokinin 1 antagonist aprepitant is a potent antiemetic agent developed for use in chemotherapy-induced and postoperative nausea; regrettably, it did not diminish nausea related to gastroparesis [45].
Attempts to ameliorate symptoms by pharmacologically addressing other processes that might be relevant to the pathogenesis of symptoms in gastroparesis, such as visceral hypersensitivity [46] or defects in the enteric nervous system [47], have, so far, proven disappointing.
In the management of symptoms thought to be related to gastroparesis, attention must be paid to the possible influence of more distal disease on gastric function. Constipation is common in diabetes and it has been recognized for some time that constipation delays gastric emptying [48, 49]—relief of constipation may also reduce upper GI symptoms.
A major challenge in the management of gastroparesis, in general, is pain which is now being reported as a common symptom in this disorder [50,51,52]. Moderate-to-severe pain is less common in diabetic than idiopathic gastroparesis and often results in chronic opiate use, which will, in turn, delay gastric emptying [52]. Caution must be exercised in the interpretation of gastric emptying rates in the context of opiate use, otherwise one runs the risk of labeling what is, in effect, a chronic pain syndrome as gastroparesis.
Management of Accelerated Gastric Emptying
There are few studies available to guide the treatment of accelerated gastric emptying . In postoperative dumping syndrome, dietary measures, such as the addition of acarbose, guar gum, and pectin, have been shown to delay gastric emptying [53, 54]. In diabetes, agents such as amylin analogs [55] and glucagon-like peptide-1 agonists [56] that can slow gastric emptying might, in theory, offer some relief, improve symptoms but have not been formally tested [57].
Non-pharmacological Approaches: Endoscopy, External Stimulation, and Surgery
Given the relative paucity of effective drug therapies , it should come as little surprise that a number of non-pharmacological approaches to the management of diabetic gastroparesis have been explored.
One of the least invasive of these is the intrapyloric injection of botulinum toxin under direct endoscopic control; a strategy based on the assumption that increased pyloric tone or contractility contributes to a functional impediment to gastric outflow in gastroparesis [58]. Initial case series and anecdotal reports suggested efficacy; a randomized controlled trial failed to confirm this [59]. Multiple factors may contribute to these conflicting results including technique, dose, and patient selection [60]. With regard to the latter, it must be conceded that botulinum toxin has been used regardless of any evidence of pyloric dysfunction. While the concept of “pylorospasm” based on conventional perfused catheter manometry may be an oversimplification [61], recent work using the EndoFLIP® system has renewed interest in the role of the pylorus in gastroparesis [62] and may help to refine patient selection for pyloric therapies. Impaired compliance, identified on EndoFLIP®, has been shown to predict response to pyloric dilation [63].
In parallel to this resurgence in interest in the pylorus, new literature has emerged suggesting efficacy for surgical [64, 65] and endoscopic pyloromyotomy [66, 67] in the management of refractory gastroparesis. An important caveat—impressive as these results may be in terms of symptom relief and acceleration of gastric emptying, these are all case series and randomized controlled trials are awaited.
Gastric electrical stimulation (GES) delivers high-frequency, low-amplitude stimulation via electrodes implanted in the smooth muscle layer of the gastric wall. The original goal was to “pace” the stomach and accelerate gastric emptying; this is not achieved, regardless of effects on symptoms and the mode of action of GES remains to be defined [68]. Its impact is unclear; though one large multicenter study showed a benefit for active stimulation over sham in a randomized, double-blind phase [69], a recent meta-analysis could not identify an effect on total symptom severity from data collated from five randomized studies [70]. In contrast, 16 open-label studies, when submitted to the same meta-analysis protocol, showed a significant benefit [70]. GES implantation is invasive and complications do occur; its place in the overall management of gastroparesis either on its own, or in combination with pyloroplasty [71], remains unclear, despite apparently positive outcomes in case series [72].
If all of the above approaches fail, more drastic surgeries may be indicated. Small case series report good outcomes following Roux-en-Y gastric bypass [73] and gastrectomy [74].
Conclusions
Gastroparesis is a relatively uncommon and poorly understood complication of diabetes whose pathophysiology is incompletely understood. Poor correlations between symptoms and gastric dysfunction, together with confounding factors such as psychopathology and opiate use, make management challenging. To make matters worse, available medical therapies are at best modestly effective and more invasive approaches are, for the most part, unproven in high-quality clinical trials .
Peptic Ulcer Disease
Apart from the suggestion that there may be an increased prevalence of infection with Helicobacter pylori among those with type 2 diabetes [75] and the observation that mortality from two complications of peptic ulcer disease, namely, hemorrhage [76, 77] and perforation [78], may be increased in diabetics, there are no other features of peptic ulcer disease among diabetics that would warrant any different approach to its management.
Abbreviations
- 5-HT:
-
5-Hydroxytryptamine
- EndoFLIP® :
-
Endoscopic functional luminal imaging probe
- GERD:
-
Gastroesophageal reflux disease
- GES:
-
Gastric electrical stimulation
- HbA1c:
-
Glycated hemoglobin
- PPI:
-
Proton pump inhibitor
References
George NS, Rangan V, Geng Z, Khan F, Kichler A, Gabbard S, et al. Distribution of esophageal motor disorders in diabetic patients with dysphagia. J Clin Gastroenterol. 2017;51:890–5.
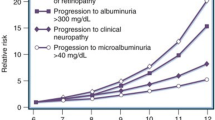
Gustafsson RJ, Littorin B, Berntorp K, Frid A, Thorsson O, Olsson R, et al. Esophageal dysmotility is more common than gastroparesis in diabetes mellitus and is associated with retinopathy. Rev Diabet Stud. 2011;8:268–75.
Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308–28.
Hershcovici T, Fass R. Management of gastroesophageal reflux disease that does not respond well to proton pump inhibitors. Curr Opin Gastroenterol. 2010;26:367–78.
Hershcovici T, Jha LK, Gadam R, Cui H, Gerson L, Thomson S, et al. The relationship between type 2 diabetes mellitus and failure to proton pump inhibitor treatment in gastroesophageal reflux disease. J Clin Gastroenterol. 2012;46(8):662.
Malfertheiner P, Kandulski A, Venerito M. Proton-pump inhibitors: understanding the complications and risks. Nat Rev Gastroenterol Hepatol. 2017;14:697–710.
Moayyedi P, Lewis MA. Proton pump inhibitors and dementia: deciphering the data. Am J Gastroenterol. 2017;112:1809–11.
Villafuerte-Gálvez JA, Kelly CP. Proton pump inhibitors and risk of Clostridium difficile infection: association or causation? Curr Opin Gastroenterol. 2018;34:11–8.
Landi SN, Sandler RS, Pate V, Lund JL. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology. 2017. https://doi.org/10.1053/j.gastro.2017.10.042. [epub ahead of print].
Cheung KS, Chan EW, Wong AYS, Chen L, Wong ICK, Leung WK. Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study. Gut. 2018;67:28–35.
Crouch MA, Mefford IN, Wade EU. Proton pump inhibitor therapy associated with lower glycosylated hemoglobin levels in type 2 diabetes. J Am Board Fam Med. 2012;25:50–4.
Laudenbach JM, Epstein JB. Treatment strategies for oropharyngeal candidiasis. Expert Opin Pharmacother. 2009;10:1413–21.
O'Rourke A. Infective oesophagitis: epidemiology, cause, diagnosis and treatment options. Curr Opin Otolaryngol Head Neck Surg. 2015;23:459–63.
Asayama N, Nagata N, Shimbo T, Nishimura S, Igari T, Akiyama J, et al. Relationship between clinical factors and severity of esophageal candidiasis according to Kodsis classification. Dis Esophagus. 2013;27:214–9.
Bytzer P, Talley NJ, Leemon M, Young LJ, Jones MP, Horowitz M. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch Intern Med. 2001;161:1989–96.
Bytzer P, Talley NJ, Hammer J, Young LJ, Jones MP, Horowitz M. GI symptoms in diabetes mellitus are associated with both poor glycemic control and diabetic complications. Am J Gastroenterol. 2002;97:604–11.
Marathe CS, Rayner CK, Jones KL, Horowitz M. Novel insights into the effects of diabetes on gastric motility. Expert Rev Gastroenterol Hepatol. 2016;10:581–93.
Sharma D, Morrison G, Joseph F, Purewal TS, Weston PJ. The role of continuous subcutaneous insulin infusion therapy in patients with diabetic gastroparesis. Diabetologia. 2011;54:2768–70.
Jones KL, Russo A, Berry MK, Stevens JE, Wishart JM, Horowitz M. A longitudinal study of gastric emptying and upper gastrointestinal symptoms in patients with diabetes mellitus. Am J Med. 2002;113:449–55.
Chang J, Rayner CK, Jones KL, Horowitz M. Prognosis of diabetic gastroparesis—a 25-year evaluation. Diabet Med. 2013;30:e185–8.
Bharucha AE, Kudva Y, Basu A, Camilleri M, Low PA, Vella A, et al. Relationship between glycemic control and gastric emptying in poorly controlled type 2 diabetes. Clin Gastroenterol Hepatol. 2015;13:466–76.
Thazhath SS, Jones KL, Horowitz M, Rayner CK. Diabetic gastroparesis: recent insights into pathophysiology and implications for management. Expert Rev Gastroenterol Hepatol. 2013;7:127–39.
Vanormelingen C, Tack J, Andrews CN. Diabetic gastroparesis. Br Med Bull. 2013;105:213–30.
Bouras EP, Vazquez Roque MI, Aranda-Michel J. Gastroparesis: from concepts to management. Nutr Clin Pract. 2013;28:437–47.
Stevens JE, Jones KL, Rayner CK, Horowitz M. Pathophysiology and pharmacotherapy of gastroparesis: current and future perspectives. Expert Opin Pharmacother. 2013;14:1171–86.
Horváth VJ, Izbéki F, Lengyel C, Kempler P, Várkonyi T. Diabetic gastroparesis: functional/morphologic background, diagnosis, and treatment options. Curr Diab Rep. 2014;14:527.
Khoo J, Rayner CK, Jones KL, Horowitz M. Pathophysiology and management of gastroparesis. Expert Rev Gastroenterol Hepatol. 2009;3:167–81.
Pasricha PJ, Pehlivanov N, Sugumar A, Jankovic J. Drug insight: from disturbed motility to disordered movement—a review of the clinical benefits and medicolegal risks of metoclopramide. Nat Clin Pract Gastroenterol Hepatol. 2006;3:138–48.
Brogden RN, Carmine AA, Heel RC, Speight TM, Avery GS. Domperidone. A review of its pharmacological activity, pharmacokinetics and therapeutic efficacy in the symptomatic treatment of chronic dyspepsia and as an antiemetic. Drugs. 1982;24:360–400.
Leelakanok N, Holcombe A, Schweizer ML. Domperidone and risk of ventricular arrhythmia and cardiac death: a systematic review and meta-analysis. Clin Drug Investig. 2016;36:97–107.
Peeters TL. Erythromycin and other macrolides as prokinetic agents. Gastroenterology. 1993;105:1886–99.
Camilleri M. The current role of erythromycin in the clinical management of gastric emptying disorders. Am J Gastroenterol. 1993;88:169–71.
Potter TG, Snider KR. Azithromycin for the treatment of gastroparesis. Ann Pharmacother. 2013;47:411–5.
Quigley EM. Cisapride: what can we learn from the rise and fall of a prokinetic? J Dig Dis. 2011;12:147–56.
Sakamoto Y, Sekino Y, Yamada E, Ohkubo H, Higurashi T, Sakai E, et al. Mosapride accelerates the delayed gastric emptying of high-viscosity liquids: a crossover study using continuous real-time C breath test (BreathID System). J Neurogastroenterol Motil. 2011;17:395–401.
Kawamura E, Enomoto M, Kotani K, Hagihara A, Fujii H, Kobayashi S, et al. Effect of mosapride citrate on gastric emptying in interferon-induced gastroparesis. Dig Dis Sci. 2012;57:1510–6.
Bang CS, Kim JH, Baik GH, Kim HS, Park SH, Kim EJ, et al. Mosapride treatment for functional dyspepsia: a meta-analysis. J Gastroenterol Hepatol. 2015;30:28–42.
Du Y, Su T, Song X, Gao J, Zou D, Zuo C, et al. Efficacy and safety of cinitapride in the treatment of mild to moderate postprandial distress syndrome-predominant functional dyspepsia. J Clin Gastroenterol. 2014;48:328–35.
Stevens JE, Russo A, Maddox AF, Rayner CK, Phillips L, Talley NJ, et al. Effect of itopride on gastric emptying in longstanding diabetes mellitus. Neurogastroenterol Motil. 2008;20:456–63.
Veldhuyzen Van Zanten SJ. Pitfalls in designing trials of functional dyspepsia: the ascent and demise of itopride. Gut. 2008;57:723–4.
Matsunaga Y, Tanaka T, Yoshinaga K, Ueki S, Hori Y, Eta R, et al. Acotiamide hydrochloride (Z-338), a new selective acetylcholinesterase inhibitor, enhances gastric motility without prolonging QT interval in dogs: comparison with cisapride, itopride, and mosapride. J Pharmacol Exp Ther. 2011;336:791–800.
Kusunoki H, Haruma K, Manabe N, Imamura H, Kamada T, Shiotani A, et al. Therapeutic efficacy of acotiamide in patients with functional dyspepsia based on enhanced postprandial gastric accommodation and emptying: randomized controlled study evaluation by real-time ultrasonography. Neurogastroenterol Motil. 2012;24:540–5.
Nelson AD, Camilleri M, Acosta A, Busciglio I, Linker Nord S, Boldingh A, et al. Effects of ghrelin receptor agonist, relamorelin, on gastric motor functions and satiation in healthy volunteers. Neurogastroenterol Motil. 2016;28:1705–13.
Camilleri M, McCallum RW, Tack J, Spence SC, Gottesdiener K, Fiedorek FT. Efficacy and safety of relamorelin in diabetics with symptoms of gastroparesis: a randomized, placebo-controlled study. Gastroenterology. 2017;153:1240–50.
Pasricha PJ, Yates KP, Sarosiek I, McCallum RW, Abell TL, Koch KL, et al. Aprepitant has mixed effects on nausea and reduces other symptoms in patients with gastroparesis and related disorders. Gastroenterology. 2018;154:65–76.e11.
Parkman HP, Van Natta ML, Abell TL, McCallum RW, Sarosiek I, Nguyen L, et al. Effect of nortriptyline on symptoms of idiopathic gastroparesis: the NORIG randomized clinical trial. JAMA. 2013;310:2640–9.
Bharucha AE, Daley SL, Low PA, Gibbons SJ, Choi KM, Camilleri M, et al. Effects of hemin on heme oxygenase-1, gastric emptying, and symptoms in diabetic gastroparesis. Neurogastroenterol Motil. 2016;28:1731–40.
Tjeerdsma HC, Smout AJ, Akkermans LM. Voluntary suppression of defecation delaysgastric emptying. Dig Dis Sci. 1993;38:832–6.
van der Sijp JR, Kamm MA, Nightingale JM, Britton KE, Granowska M, Mather SJ, et al. Disturbed gastric and small bowel transit in severe idiopathic constipation. Dig Dis Sci. 1993;38:837–44.
Hoogerwerf WA, Pasricha PJ, Kalloo AN, Schuster MM. Pain: the overlooked symptom in gastroparesis. Am J Gastroenterol. 1999;94:1029–33.
Cherian D, Sachdeva P, Fisher RS, Parkman HP. Abdominal pain is a frequent symptom of gastroparesis. Clin Gastroenterol Hepatol. 2010;8:676–81.
Hasler WL, Wilson LA, Parkman HP, Koch KL, Abell TL, Nguyen L, et al. Factors related to abdominal pain in gastroparesis: contrast to patients with predominant nausea and vomiting. Neurogastroenterol Motil. 2013;25:427–38.
Leeds AR, Ralphs DN, Ebied F, Metz G, Dilawari JB. Pectin in the dumping syndrome: reduction of symptoms and plasma volume changes. Lancet. 1981;1:1075–8.
Tack J, Arts J, Caenepeel P, De Wulf D, Bisschops R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol. 2009;6:583–90.
Hieronymus L, Griffin S. Role of amylin in type 1 and type 2 diabetes. Diabetes Educ. 2015;41(1 Suppl):47S–56S.
Chia CW, Egan JM. Role and development of GLP-1 receptor agonists in the management of diabetes. Diabetes Metab Syndr Obes. 2009;2:37.
Boland BS, Edelman SV, Wolosin JD. Gastrointestinal complications of diabetes. Endocrinol Metab Clin N Am. 2013;42:809–32.
Mearin F, Camilleri M, Malagelada JR. Pyloric dysfunction in diabetics with recurrent nausea and vomiting. Gastroenterology. 1986;90:1919–25.
Arts J, Holvoet L, Caenepeel P, Bisschops R, Sifrim D, Verbeke K, Janssens J, Tack J. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26:1251–8.
Ukleja A, Tandon K, Shah K, Alvarez A. Endoscopic botox injections in therapy of refractory gastroparesis. World J Gastrointest Endosc. 2015;7:790–8.
Fraser R, Horowitz M, Dent J. Hyperglycaemia stimulates pyloric motility in normal subjects. Gut. 1991;32:475–8.
Malik Z, Sankineni A, Parkman HP. Assessing pyloric sphincter pathophysiology using EndoFLIP in patients with gastroparesis. Neurogastroenterol Motil. 2015;27:524–31.
Gourcerol G, Tissier F, Melchior C, Touchais JY, Huet E, Prevost G, Leroi AM, Ducrotte P. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41:360–7.
Mancini SA, Angelo JL, Peckler Z, Philp FH, Farah KF. Pyloroplasty for refractory gastroparesis. Am Surg. 2015;81:738–46.
Shada AL, Dunst CM, Pescarus R, Speer EA, Cassera M, Reavis KM, Swanstrom LL. Laparoscopic pyloroplasty is a safe and effective first-line surgical therapy for refractory gastroparesis. Surg Endosc. 2016;30:1326–32.
Benias PC, Khashab MA. Gastric peroral endoscopic pyloromyotomy therapy for refractory gastroparesis. Curr Treat Options Gastroenterol. 2017;15:637–47.
Rodriguez JH, Haskins IN, Strong AT, Plescia RL, Allemang MT, Butler RS, Cline MS, et al. Per oral endoscopic pyloromyotomy for refractory gastroparesis: initial results from a single institution. Surg Endosc. 2017;31:5381–8.
Lacy BE, Weiser K. Gastric motility, gastroparesis, and gastricstimulation. Surg Clin North Am. 2005;85:967–87.
Abell T, McCallum R, Hocking M, Koch K, Abrahamsson H, Leblanc I, et al. Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology. 2003;125:421–8.
Levinthal DJ, Bielefeldt K. Systematic review and meta-analysis: gastricelectrical stimulation for gastroparesis. Auton Neurosci. 2017;202:45–55.
Davis BR, Sarosiek I, Bashashati M, Alvarado B, McCallum RW. The long-term efficacy and safety of pyloroplasty combined with gastric electrical stimulation therapy in gastroparesis. J Gastrointest Surg. 2017;21:222–7.
Jayanthi NV, Dexter SP, Sarela AI, Leeds Gastroparesis Multi-Disciplinary Team. Gastric electrical stimulation for treatment of clinically severe gastroparesis. J Minim Access Surg. 2013;9:163–7.
Papasavas PK, Ng JS, Stone AM, Ajayi OA, Muddasani KP, Tishler DS. Gastric bypass surgery as treatment of recalcitrant gastroparesis. Surg Obes Relat Dis. 2014;10:795–9.
Bhayani NH, Sharata AM, Dunst CM, Kurian AA, Reavis KM, Swanstrom LL. End of the road for a dysfunctional end organ: laparoscopic gastrectomy for refractory gastroparesis. J Gastrointest Surg. 2015;19:411–7.
Li J-Z, Li J-Y, Wu T-F, Xu J-H, Huang C-Z, Chen D, et al. Helicobacter pylori infection is associated with type 2 diabetes, not type 1 diabetes: an updated meta-analysis. Gastroenterol Res Pract. 2017;2017:5715403.
Wei F, Lin X. Diabetes increases morbidity and mortality rates in peptic ulcer bleeding: an updated systematic review and meta-analysis. Turk J Gastroenterol. 2016;27:304–11.
Leontiadis GI, Molloy-Bland M, Moayyedi P, Howden CW. Effect of comorbidity on mortality in patients with peptic ulcer bleeding: systematic review and meta-analysis. Am J Gastroenterol. 2013;108:331–45.
Thomsen RW, Riis A, Christensen S, Nørgaard M, Sørensen HT. Diabetes and 30-day mortality from peptic ulcer bleeding and perforation: a Danish population-based cohort study. Diabetes Care. 2006;29:805–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Oglat, A., Quigley, E.M.M. (2018). Treatment. In: Duvnjak, M., Smirčić-Duvnjak, L. (eds) Gastrointestinal Complications of Diabetes . Clinical Gastroenterology. Humana Press, Cham. https://doi.org/10.1007/978-3-319-75856-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-75856-5_7
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-75855-8
Online ISBN: 978-3-319-75856-5
eBook Packages: MedicineMedicine (R0)