Abstract
The pancreas should be considered as a single endocrine–exocrine gland with complex insulo-acinar-ductal communications. Insulin exerts a trophic and stimulatory effect on the acinar cells, digestive enzymes secreted by the acinar cells are involved in the release of gut-incretin hormones by the enteroendocrine L-cells, and gut-incretin hormones exert a stimulatory effect on insulin release and improve insulin sensitivity. Exocrine pancreatic function is altered in patients with type 1 and type 2 diabetes. Pancreatic atrophy and infiltration of inflammatory cells within the exocrine pancreas may explain reduced pancreatic secretion in type 1 diabetes. The normal structural islet–exocrine interface is lost due to fibrosis in type 2 diabetes. As interstitial fibrosis progresses, the trophic and stimulatory effects of insulin on acinar cells may be impaired and pancreatic enzyme secretion reduced. A low pancreatic enzyme secretion may be associated with gastrointestinal symptoms, and may potentially interfere with the glycemic control in diabetes, but the impact of pancreatic exocrine disturbance in these patients is unclear, and it deserves further investigation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The endocrine and exocrine pancreas is classically considered to be two separate organs. Diseases of the exocrine pancreas are mainly managed by gastroenterologists and surgeons, whereas diseases of the endocrine pancreas are managed by endocrinologists and diabetologists. This artificial subdivision of the pancreas into two different organs, which additionally are usually managed by different specialists, has limited the investigation and therefore the knowledge of the pancreatic endocrine–exocrine interaction, both in heath and disease [1].
The pancreas is in fact a single endocrine tubule-acinar gland with complex cell-to-cell insulo-acinar-ductal communications through a pancreatic hormone–enzyme–incretin gut hormone axis. The pancreatic endocrine–exocrine cell interface plays a major role in the communication between the islet and acinar cells. Insulin diffuses in the extracellular space, and interacts with the plasma membrane of all pancreatic cells. Pancreatic cells are thus exposed to very high levels of insulin that decrease progressively from peri-insular to tele-insular areas [2]. Insulin exerts a trophic and stimulatory effect on the acinar cells, thus playing a key role in the physiological exocrine pancreatic function and morphology [3]. A normal exocrine pancreatic function is needed for a normal digestion of nutrients. Digested nutrients by pancreatic enzymes synthesized by the acinar cells and delivered into the gut play, on the other hand, a major role in activating the enteroendocrine L-cells of the ileum to synthesize and release incretin hormones such as the glucagon-like peptide-1 (GLP-1). Finally, incretin-gut hormones are well known to exert a stimulatory effect on insulin and an inhibitory effect on glucagon release, and to improve insulin sensitivity [4]. Pancreatic hormones, pancreatic enzymes, and incretin-gut hormones are therefore constituents of a single physiological system. Alteration of any of the components of this insulo-acinar-incretin gut hormone axis has thus a negative functional impact on the others.
Exocrine Pancreatic Secretion in Health
Secretion of pancreatic enzymes, such as lipase, amylase, and proteases, play a key role in digestion of macronutrients. Optimal digestion is obviously needed for absorption of nutrients, and thus it has a very relevant impact in the nutritional status of subjects. A low pancreatic secretion of enzymes and bicarbonate may thus be associated with maldigestion of nutrients, which in turn causes nutritional deficiencies and symptoms of malabsorption (diarrhea, steatorrhea, abdominal cramps, flatulence, abdominal distention, and weight loss) [5,6,7]. Pancreatic exocrine insufficiency is defined as the presence of maldigestion-related symptoms and/or nutritional deficiencies as a consequence of a low pancreatic secretion.
The healthy exocrine pancreas has a cyclical basal secretion of enzymes and bicarbonate during the fasting state, which is closely coordinated with interdigestive phases of gastrointestinal motility, and release of hormones such as pancreatic polypeptide (PP) [8]. This coordinated fasting pancreatic secretion and gastrointestinal motility is considered as an intestinal housekeeper, sweeping the gut free of luminal debris and bacteria and preparing it for the next meal. Interdigestive cycles of pancreatic enzyme secretion and PP release are shortened and no longer temporally coordinated with gastrointestinal motility in pancreatic diseases such as ch ronic pancreatitis [9]. This could at least partly explain the high prevalence of intestinal bacterial overgrowth in these patients [10]. Hyperglycemia is known to reduce gastrointestinal motility [11]. In addition, small intestinal bacterial overgrowth is a frequent finding in diabetes, which has been associated with chronic diarrhea in these patients [12]. The role of interdigestive pancreatic secretion and its coordination with the gastrointestinal motility pattern in this scenario has not been properly addressed, but if altered, it could play a relevant role in the development of diabetes-associated gastrointestinal symptoms.
Ingestion of a meal disrupts the interdigestive pattern and induces a rapid increase of pancreatic enzyme secretion, to reach a stable stimulated enzyme delivery into the duodenum lasting for 3–4 h [13]. Before meal ingestion, sight, smell, and taste of food initiate the cephalic phase of digestive pancreatic enzyme secretion, which is mediated by the vagal cholinergic system [14]. Later, food-mediated gastric distention accounts for further stimulation of pancreatic secretion through cholinergic gastropancreatic reflexes. Once the nutrients reach the duodenal lumen, cholecystokinin (CCK) is released by the duodenal I cells. CCK is the major mediator of the postprandial pancreatic secretion of enzymes [13]. The intensity and duration of the postprandially stimulated pancreatic enzyme secretion are influenced by the caloric content, the nutrient composition, and the physical properties of the meal. Termination of the postprandial pattern of pancreatic enzyme secretion is probably mediated by hormones released from the distal intestinal mucosa, such as peptide YY and the glucagon-like peptide-1 (GLP-1). Therefore, GLP-1 is involved in the physiological function of both the endocrine and the exocrine pancreas.
Evaluation of Exocrine Pancreatic Function
Exocrine pancreatic function may be mainly evaluated by means of direct tests, tubeless indirect tests, and fecal tests. Direct tests are based on the direct measurement of pancreatic enzymes and bicarbonate output in samples of duodenal juice obtained after stimulation of the gland, either by intravenous administration of secretin and CCK or caerulein (secretin–pancreozymin test) or by ingestion of a test meal (Lundh’s test) [15]. These tests are the most sensitive method for evaluating pancreatic secretion, but they are invasive, cumbersome, time-consuming, and expensive, thus limiting their use in clinical practice. A modification of the classical secretin test is the so-called endoscopy pancreatic function test (ePFT) . The ePFT is based on the measurement of bicarbonate concentration in samples of duodenal juice obtained during upper gastrointestinal endoscopy after intravenous secretin administration [16]. This test is more frequently used and more easily applicable into clinical practice than the standard secretin–pancreozymin test.
Indirect tests evaluate exocrine pancreatic function by quantifying the digestive ability of the gland. A substrate is orally given together with a test meal. Pancreatic enzymes hydrolyze the substrate within the duodenum, and the released metabolites are absorbed from the gut and can be measured either in serum, urine, or breath [15]. Indirect tests used in the past, such as the pancreolauryl test and the p-aminobenzoic acid (PABA)-test , are no longer commercially available in the majority of countries. More recently, an optimized breath test with 13C-labeled mixed triglycerides (13C-MTG) as substrate has been reported [17], and it is commercially available in some countries.
Fecal tests are based on the quantification of pancreatic enzyme concentration (elastase) or activity (chymotrypsin) in feces. Enzymes are deactivated and diluted or concentrated to a variable degree during the intestinal passage; this must be taken into account for an adequate interpretation of the test results.
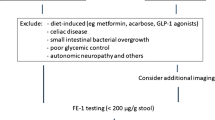
Pancreatic elastase is highly stable along the gastrointestinal transit, and the fecal concentration of this enzyme significantly correlates with the amount of enzyme secreted by the exocrine pancreas. The fecal elastase test is based on the quantification of this pancreatic specific enzyme in a small sample of feces. The enzyme is stable at room temperature for 1 week, and the quantification of its concentration is based on a standard enzyme-immunoassay technique, which makes the test easily applicable to clinical practice [18]. A fecal elastase concentration below 200 μg/g is considered abnormally low, whereas concentrations below 100 μg/g and 50 μg/g are considered as moderate and severe reduction of pancreatic secretion, respectively [18].
Exocrine pancreatic function can also be measured indirectly in feces by means of the quantification of the coefficient of fat absorption (CFA) . CFA quantification is still considered to be the gold standard for the diagnosis of pancreatic exocrine insufficiency with fat maldigestion [7, 15]. However, this test has several and important disadvantages, limiting its clinical applicability. Patients must stay on a standard diet containing 100 g of fat daily during 5 consecutive days, and they have to collect the whole amount of feces produced over the last 3 days of diet. This is not easy to comply with for many patients. Patient compliance is not only a limitation for fecal fat quantification but also for the handling of stool samples in the lab.
Exocrine Pancreatic Secretion in Type 1 Diabetes
The exocrine pancreas becomes atrophic in patients with type 1 diabetes. This finding has been consistently demonstrated both in autopsy studies [18, 19] and in studies using imaging techniques [19,20,21]. Pancreatic atrophy in type 1 diabetes is at least partly secondary to the loss of the trophic and stimulatory effect of insulin on the exocrine pancreas. However, inflammatory infiltration of the exocrine pancreas may play a role in the pathogenesis of type 1 diabetes, and the disease is likely to affect the entire pancreas rather than solely the islet beta cells [22]. In fact, CD8+ T cells, which are generally accepted to be involved in the destruction of beta cells, and thus in the pathogenesis of type 1 diabetes, have been shown to significantly infiltrate the exocrine pancreas as well [23]. The impact of CD8+ T cells infiltrating the exocrine pancreas remains to be determined, but they could be involved in the atrophy of the gland and the decreased exocrine function.
Several studies have evaluated the pancreatic secretion of enzymes in patients with type 1 diabetes by means of the classical secretin–pancreozymin test and by the quantification of pancreatic enzymes, mainly elastase, in feces [24,25,26,27,28]. Studies using the secretin–pancreozymin test have consistently reported an abnormally low secretion of pancreatic enzymes and bicarbonate in about 70–80% of type 1 diabetic patients [24,25,26,27]. Decreased pancreatic secretion of enzymes and bicarbonate correlates with diabetes duration [26] and diabetes control [27]. Similarly, studies using the fecal elastase test in patients with type 1 diabetes show a moderate to severe decrease of pancreatic secretion in up to 44% of the cases [28, 29].
Together with a low pancreatic secretion, non-pancreatic mechanisms seem to contribute to maldigestion in diabetes. This was suggested in a recent study that evaluated fat digestion by means of the 13C-MTG breath test [30]. An abnormally low breath test result was reported in more than half of the patients with diabetes, but few of them had a low output of pancreatic lipase as evaluated by the secretin–caerulein test.
Reduced exocrine pancreatic secretion in type 1 diabetes is generally considered clinically irrelevant, and is even frequently ignored. However, a decreased pancreatic secretion in these patients could be associated with symptoms of maldigestion and malabsorption of nutrients (diarrhea, flatulence, abdominal distention, abdominal cramps) and to a low incretin-gut hormone release. Further studies are needed to further understand the impact of a low secretion of pancreatic enzymes in patients with type 1 diabetes.
Exocrine Pancreatic Secretion in Type 2 Diabetes
The normal structural islet–exocrine interface is lost due to fibrosis during the remodeling changes associated with type 2 diabetes [31]. Patients with type 2 diabetes develop fibrosis of the islet–exocrine interface and the endoacinar and interlobular periacinar interstitium. This rupture of the close islet–exocrine interface is associated with the loss of the endocrine–exocrine cell–cell crosstalk [32]. A pericapillary remodeling fibrosis has been also identified in animal models of type 2 diabetes, which may result in a diffusion barrier to islet secretory granules [33]. Together with loss of β-cell due to apoptosis, there is a loss of acinar cells in patients with type 2 diabetes due to apoptosis. Both endocrine and exocrine parenchyma are thus replaced by fibrosis and adipose tissue. These changes develop in parallel with pancreatic vascular remodeling changes [31]. All these changes result in impaired insulin delivery to the hepatic portal system and delivery of pancreatic enzymes to the gut. As interstitial fibrosis progresses, the trophic and stimulatory effects of insulin on acinar cells may be importantly impaired. Pancreatic enzyme secretion may be thus markedly reduced and intraluminal digestion of nutrients may be impaired, which may lead to a reduced gut-hormone release [34].
Exocrine pancreatic secretion of enzymes and bicarbonate in patients with type 2 diabetes has been studied by means of the secretin–pancreozymin test by several authors [26, 27, 35, 36]. These studies reported a reduced pancreatic secretion in 27–100% of patients. In addition, type 2 diabetes is associated with a fecal elastase concentration lower than 200 μg/g in one-third of the patients [37], and with moderate to severe reduction of fecal elastase concentration in 12–20% of the patients [28, 38]. Fecal elastase appeared to positively correlate with circulating levels of C-peptide, lipase and C-reactive protein, gender, and body mass index in one study, but not with duration of diabetes or HbA1c levels [37]. Nevertheless, patients with HbA1C ≥ 7% have significantly lower fecal elastase levels than patients with HbA1C < 7% [39]. In addition, low fecal elastase concentrations have been associated with high fasting plasma triglycerides levels in type 2 diabetes [40].
The impact of decreased exocrine pancreatic secretion of enzymes and bicarbonate in patients with type 2 diabetes deserves further investigation. This exocrine impairment may be associated with gastrointestinal symptoms similar to those usually related to diabetic neuropathy, as well as with a low gut-incretin hormone release and poor glycemic control.
References
Pieler T, Chen Y. Forgotten and novel aspects in pancreas development. Biol Cell. 2006;98(2):79–88.
Bendayan M. Pathway of insulin in pancreatic tissue on its release by the B-cell. Am J Phys. 1993;264(2 Pt 1):G187–94.
Williams JA, Goldfine ID. The insulin-pancreatic acinar axis. Diabetes. 1985;34(10):980–6.
Tasyurek HM, Altunbas HA, Balci MK, Sanlioglu S. Incretins: their physiology and application in the treatment of diabetes mellitus. Diabetes Metab Res Rev. 2014;30(5):354–71.
Lindkvist B, Phillips ME, Domínguez-Muñoz JE. Clinical, anthropometric and laboratory nutritional markers of pancreatic exocrine insufficiency: prevalence and diagnostic use. Pancreatol. 2015;15(6):589–97.
Lindkvist B, Domínguez-Muñoz JE, Luaces-Regueira M, Castiñeiras-Alvariño M, Nieto-Garcia L, Iglesias-Garcia J. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatol. 2012;12(4):305–10.
Domínguez-Muñoz JE. Pancreatic exocrine insufficiency: diagnosis and treatment. J Gastroenterol Hepatol. 2011;26(Suppl 2):12–6.
Vantrappen GR, Peeters TL, Janssens J. The secretory component of the interdigestive migrating motor complex in man. Scand J Gastroenterol. 1979;14(6):663–7.
Pieramico O, Dominguez-Muñoz JE, Nelson DK, Böck W, Büchler M, Malfertheiner P. Interdigestive cycling in chronic pancreatitis: altered coordination among pancreatic secretion, motility, and hormones. Gastroenterology. 1995;109(1):224–30.
Capurso G, Signoretti M, Archibugi L, Stigliano S, DelleFave G. Systematic review and meta-analysis: small intestinal bacterial overgrowth in chronic pancreatitis. United Eur Gastroenterol J. 2016;4(5):697–705.
Björnsson ES, Urbanavicius V, Eliasson B, Attvall S, Smith U, Abrahamsson H. Effects of hyperglycemia on interdigestive gastrointestinal motility in humans. Scand J Gastroenterol. 1994;29(12):1096–104.
Virally-Monod M, Tielmans D, Kevorkian JP, Bouhnik Y, Flourie B, Porokhov B, et al. Chronic diarrhoea and diabetes mellitus: prevalence of small intestinal bacterial overgrowth. Diabetes Metab. 1998;24(6):530–6.
Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54(Suppl 6):1–28.
Anagnostides A, Chadwick VS, Selden AC, Maton PN. Sham feeding and pancreatic secretion. Evidence for direct vagal stimulation of enzyme output. Gastroenterology. 1984;87(1):109–14.
Domínguez Muñoz JE. Diagnosis of chronic pancreatitis: functional testing. Best Pract Res Clin Gastroenterol. 2010;24(3):233–41.
Stevens T, Conwell DL, Zuccaro G, Van Lente F, Lopez R, Purich E, et al. A prospective crossover study comparing secretin-stimulated endoscopic and Dreiling tube pancreatic function testing in patients evaluated for chronic pancreatitis. Gastrointest Endosc. 2008;67(3):458–66.
Domínguez-Muñoz JE, Nieto L, Vilariño M, Lourido MV, Iglesias-García J. Development and diagnostic accuracy of a breath test for pancreatic exocrine insufficiency in chronic pancreatitis. Pancreas. 2016;45(2):241–7.
Rahier J, Goebbels RM, Henquin JC. Cellular composition of the human diabetic pancreas. Diabetologia. 1983;24(5):366–71.
Williams AJK, Thrower SL, Sequeiros IM, Ward A, Bickerton AS, Triay JM, et al. Pancreatic volume is reduced in adult patients with recently diagnosed type 1 diabetes. J Clin Endocrinol Metab. 2012;97(11):E2109–13.
Altobelli E, Blasetti A, Verrotti A, Di Giandomenico V, Bonomo L, Chiarelli F. Size of pancreas in children and adolescents with type I (insulin-dependent) diabetes. J Clin Ultrasound. 1998;26(8):391–5.
Gilbeau JP, Poncelet V, Libon E, Derue G, Heller FR. The density, contour, and thickness of the pancreas in diabetics: CT findings in 57 patients. AJR Am J Roentgenol. 1992;159(3):527–31.
Campbell-Thompson M, Rodriguez-Calvo T, Battaglia M. Abnormalities of the exocrine pancreas in type 1 diabetes. Curr Diab Rep. 2015;15(10):79.
Rodriguez-Calvo T, Ekwall O, Amirian N, Zapardiel-Gonzalo J, von Herrath MG. Increased immune cell infiltration of the exocrine pancreas: a possible contribution to the pathogenesis of type 1 diabetes. Diabetes. 2014;63(11):3880–90.
Lankisch PG, Manthey G, Otto J, Koop H, Talaulicar M, Willms B, et al. Exocrine pancreatic function in insulin-dependent diabetes mellitus. Digestion. 1982;25(3):211–6.
Vacca JB, Henke WJ, Knight WA. The exocrine pancreas in diabetes mellitus. Ann Intern Med. 1964;61:242–7.
Frier BM, Saunders JH, Wormsley KG, Bouchier IA. Exocrine pancreatic function in juvenile-onset diabetes mellitus. Gut. 1976;17(9):685–91.
Harano Y, Kim CI, Kang M, Shichiri M, Shimizu Y, Li H, et al. External pancreatic dysfunction associated with diabetes mellitus. J Lab Clin Med. 1978;91(5):780–90.
Hardt PD, Hauenschild A, Nalop J, Marzeion AM, Jaeger C, Teichmann J, et al. High prevalence of exocrine pancreatic insufficiency in diabetes mellitus. A multicenter study screening fecal elastase 1 concentrations in 1,021 diabetic patients. Pancreatol. 2003;3(5):395–402.
Hardt PD, Krauss A, Bretz L, Porsch-Ozcürümez M, Schnell-Kretschmer H, Mäser E, et al. Pancreatic exocrine function in patients with type 1 and type 2 diabetes mellitus. Acta Diabetol. 2000;37(3):105–10.
Keller J, Layer P, Brückel S, Jahr C, Rosien U. 13C-mixed triglyceride breath test for evaluation of pancreatic exocrine function in diabetes mellitus. Pancreas. 2014;43(6):842–8.
Hayden MR, Patel K, Habibi J, Gupta D, Tekwani SS, Whaley-Connell A, et al. Attenuation of endocrine-exocrine pancreatic communication in type 2 diabetes: pancreatic extracellular matrix ultrastructural abnormalities. J Cardiometab Syndr. 2008;3(4):234–43.
Bertelli E, Bendayan M. Association between endocrine pancreas and ductal system. More than an epiphenomenon of endocrine differentiation and development? J Histochem Cytochem. 2005;53(9):1071–86.
Hayden MR, Karuparthi PR, Habibi J, Lastra G, Patel K, Wasekar C, et al. Ultrastructure of islet microcirculation, pericytes and the islet exocrine interface in the HIP rat model of diabetes. Exp Biol Med Maywood. 2008;233(9):1109–23.
Laakso M, Zilinskaite J, Hansen T, Boesgaard TW, Vänttinen M, Stancáková A, et al. Insulin sensitivity, insulin release and glucagon-like peptide-1 levels in persons with impaired fasting glucose and/or impaired glucose tolerance in the EUGENE2 study. Diabetologia. 2008;51(3):502–11.
Bretzke G. Diabetes mellitus and exocrine pancreas function. Z Gesamte Inn Med. 1984;39(16):388–90.
el Newihi H, Dooley CP, Saad C, Staples J, Zeidler A, Valenzuela JE. Impaired exocrine pancreatic function in diabetics with diarrhea and peripheral neuropathy. Dig Dis Sci. 1988;33(6):705–10.
Kangrga RN, Ignjatović SD, Dragašević MM, Jovičić SŽ, Majkić-Singh NT. Pancreatic elastase levels in feces as a marker of exocrine pancreatic function in patients with diabetes mellitus. Lab Med. 2016;47(2):140–8.
Rathmann W, Haastert B, Icks A, Giani G, Hennings S, Mitchell J, et al. Low faecal elastase 1 concentrations in type 2 diabetes mellitus. Scand J Gastroenterol. 2001;36(10):1056–61.
Terzin V, Várkonyi T, Szabolcs A, Lengyel C, Takács T, Zsóri G, et al. Prevalence of exocrine pancreatic insufficiency in type 2 diabetes mellitus with poor glycemic control. Pancreatol. 2014;14(5):356–60.
Rathmann W, Haastert B, Oscarsson J, Berglind N, Lindkvist B, Wareham NJ. Association of faecal elastase 1 with non-fasting triglycerides in type 2 diabetes. Pancreatol. 2016;16(4):563–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Enrique Domínguez-Muñoz, J., Cigarrán, B. (2018). Exocrine Pancreatic Function in Diabetes. In: Duvnjak, M., Smirčić-Duvnjak, L. (eds) Gastrointestinal Complications of Diabetes . Clinical Gastroenterology. Humana Press, Cham. https://doi.org/10.1007/978-3-319-75856-5_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-75856-5_16
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-75855-8
Online ISBN: 978-3-319-75856-5
eBook Packages: MedicineMedicine (R0)