Abstract
Modern trauma damage control (DC) integrates the stages of DC surgery into the process of DC resuscitation. Although widely believed to improve survival when appropriately indicated, there is limited evidence supporting a benefit of DC surgery (and its component DC interventions) in injured patients. Further, the procedure is associated with a number of potentially severe and often resource-intensive complications. Several studies have recently reported data suggesting that a variation exists in the use of DC laparotomy across trauma centers or that the procedure may be overused. These and other studies have also suggested that overutilization of the procedure may be associated with increased morbidity and mortality. Variation in the use of DC surgery between trauma centers may occur because surgeons are frequently uncertain which “operative profile” (i.e., DC or definitive surgery) is best in varying clinical situations. In this chapter, I review the structure, effectiveness, and safety of modern trauma DC; recent studies suggesting variation in and potential harm related to the overuse of DC surgery between trauma centers; and published consensus indications for the use of DC surgery and DC interventions that aim to reduce this variation and guide future research.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Abbreviated surgical procedures
- Damage control intervention
- Damage control laparotomy
- Damage control surgery
- Indication
2.1 Background
In injured patients receiving traditional, crystalloid-based resuscitation, significant hemorrhage is frequently complicated by development of a “bloody vicious cycle” (a.k.a., “lethal triad”) of hypothermia, acidosis, and coagulopathy [1,2,3]. Resuscitation of hemorrhagic shock also produces ischemia-reperfusion injury of the bowel, which increases intestinal wall permeability, leading to sequestration of fluid in the bowel wall and its supporting mesenteries (i.e., abdominal visceral edema) [1, 4, 5]. This process, when combined with large-volume crystalloid fluid administration, increases intra-abdominal pressure (IAP) and may culminate in post-injury abdominal compartment syndrome (ACS; defined by the Abdominal Compartment Society as a sustained IAP >20 associated with new organ dysfunction/failure) [1, 6,7,8]. The vicious cycle and ACS have historically been associated with a high risk of death after major injury despite attempts at definitively controlling hemorrhage and preventing and/or treating intra-abdominal hypertension (IAH), respectively [1, 2].
In an attempt to prevent the onset of and/or limit the effects of the vicious cycle and post-injury ACS, surgeons adopted damage control (DC) laparotomy to manage severely injured civilians in the 1980s/early 1990s [1]. In 1983, Stone et al. reported that “staged” laparotomy [i.e., abbreviated initial laparotomy with planned reoperation after a period of ongoing resuscitation in the intensive care unit (ICU)] was associated with improved survival in injured patients who developed “major coagulopathy” during operation [9]. Rotondo, Schwab, and colleagues subsequently proposed in 1993 that abbreviated trauma laparotomy be termed “damage control” and reported data suggesting that it improved survival in a “maximum injury subset” of patients with abdominal vascular and multiple concomitant abdominal visceral injuries [10]. In 1998 (during the early dispersion and exploration stage of the innovation of trauma DC), during a time when high-volume crystalloid fluid resuscitation (and therefore severe abdominal visceral edema) was common, Ivatury and colleagues advocated for routine temporary abdominal closure (TAC) of the open abdomen (i.e., open abdominal management) after DC to prevent the adverse physiologic consequences of IAH [1, 11]. Finally, beginning largely in the mid-1990s, the DC concept was adapted to rapidly manage visceral and vascular injuries in the neck, chest, and extremities [1].
In contrast to definitive (i.e., single-stage) surgery, DC allows the initial operation for control of exsanguinating hemorrhage and/or gross contamination to be abbreviated using what Feliciano et al. termed “rapid conservative operative techniques” (now also referred to, using the DC lexicon, as “DC interventions”) [1, 12, 13]. This approach has long been thought to benefit critically injured patients who are “more likely to die from an uncorrected shock state than from failure to complete organ repairs” [14]. In the abdomen, DC interventions include therapeutic perihepatic packing, closed suction drainage of pancreaticobiliary injuries, rapid intestinal resection without re-anastomosis (leaving the intestinal tract in discontinuity until a later operation), and lateral arteriorrhaphy (e.g., superior mesenteric artery injuries), temporary intravascular shunting (e.g., common iliac artery injuries), and ligation (e.g., infrarenal inferior vena cava injuries) of major abdominal vascular injuries [15]. Abbreviating the index operation during DC theoretically limits further declines in core body temperature and pH and therefore allows for rewarming and correction of metabolic and coagulation disturbances in the ICU [16]. Once physiology is deemed adequately restored, injured patients are returned to the operating room (OR) for additional surgery (e.g., removal of temporary intravascular shunts and performance of vascular repairs or intestinal anastomoses for reestablishment of bowel continuity) and/or primary fascial closure (i.e., fascia-to-fascia closure of the open abdomen within the index hospitalization), often within 6–48 h of initial operation [1, 16].
In this chapter, I review the structure, effectiveness, and safety of modern trauma DC; recent studies suggesting variation in and potential harm related to the overuse of DC surgery between trauma centers; and published consensus indications for the use of DC surgery and DC interventions that aim to reduce this variation and guide future research.
2.2 The Structure of Modern Trauma DC (Integrating the Stages of DC Surgery with the Process of DC Resuscitation)
The stages of DC surgery were initially suggested by Rotondo, Schwab, and colleagues to include DC 1 [immediate operation for control of hemorrhage and contamination using one or more DC interventions followed by temporary closure of the abdomen (or thorax) and transfer to the ICU], DC 2 (resuscitation in the ICU with the goal of correcting hypothermia, acidosis, and coagulopathy), and DC 3 [reoperation for definitive repair of injuries and closure of the abdomen (or thorax)] [1, 16]. This group and others later expanded these stages to include DC 0 [or “damage control ground zero,” which includes those interventions performed in the prehospital and immediate in-hospital setting before operation (e.g., prehospital transport/care, rewarming, and initiation of a predesigned massive transfusion protocol)] and DC 4 (abdominal wall reconstruction, frequently using component separation methods and synthetic or biological mesh reinforcement) [17, 18].
DC interventions are rapid, often technically simple procedures that may be used in either the pre- [e.g., balloon catheter tamponade of significant, ongoing hemorrhage from a zone III neck wound in the emergency department (ED)] or intraoperative setting [15]. These interventions are designed to temporarily or sometimes definitively manage exsanguinating hemorrhage, gross contamination, and/or a massive pulmonary air leak in situations where several uncommonly encountered thoracic (e.g., a penetrating, through-and-through pulmonary parenchymal injury that does not involve the hilar structures), abdominal (e.g., devascularization or massive destruction of the pancreas, duodenum, or pancreaticoduodenal complex), pelvic (e.g., severe blunt pelvic trauma with ongoing, massive extraperitoneal hemorrhage), and/or vascular (e.g., significant, ongoing bleeding from a zone I or III penetrating neck injury) injuries are encountered [15, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. These injuries are characteristic of those that few surgeons have experience treating and therefore are associated with massive hemorrhage, physiological exhaustion (hypothermia, acidosis, and coagulopathy), and a high mortality when attempts are made to manage them definitively (see Table 2.1 for consensus definitions of a number of DC interventions reported in 2015) [15, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46].
In modern civilian trauma care, many surgeons have suggested that DC surgery (or, more specifically, DC 1) should most appropriately be considered one of the first, essential components of the process of DC resuscitation [47]. DC resuscitation is characterized by rapid hemorrhage control (open or endovascular, including the use of DC interventions in the preoperative setting or in the OR during DC 1), permissive hypotension, administration of blood products in a ratio approximating whole blood [i.e., 1:1:1 plasma/platelets/packed red blood cells (PRBCs)], and minimal use of crystalloid fluids [48,49,50]. This now internationally adopted resuscitation strategy is initiated in the prehospital setting (a.k.a., during DC 0) and continued through DC stages 1–4. DC resuscitation was developed in order to preemptively treat the lethal triad (including the acute coagulopathy of trauma, which occurs early after injury, is likely caused by the degree of tissue injury after trauma, and is independent of the amount of crystalloid fluids administered to the patient), preserve oxygen-carrying capacity, repair the endothelium, and prevent the adverse physiological consequences of large-volume crystalloid fluid resuscitation [47,48,49,50]. In the recently reported PROPPR randomized controlled trial (RCT) comparing a 1:1:1 versus 1:1:2 ratio of plasma/platelets/PRBCs, although 24-h and 30-day mortality was similar between the study groups, more patients in the 1:1:1 group achieved hemostasis, and fewer experienced death due to exsanguination at 24 h [50]. Thus, DC resuscitation with a 1:1:1 ratio of blood products likely has a hemostatic benefit among exsanguinating civilian trauma patients.
2.3 Effectiveness and Safety of DC Surgery in Civilian Trauma Patients
Although widely believed to improve survival when appropriately indicated, there is limited evidence supporting a benefit of DC surgery in injured patients [1, 16]. A Cochrane systematic review on DC laparotomy conducted in 2013 identified few relevant observational studies and no RCTs [16, 51]. Importantly, as the “operative profile” (DC versus definitive surgery) chosen in these seven observational studies was not randomly assigned, their conclusions are inherently limited by confounding by indication. This relatively common limitation of observational treatment studies occurs when other, unmeasured reasons associated with the choice to perform DC surgery and with patient outcome confound the association between DC surgery and outcomes (i.e., those selected for DC are inherently different from those selected for definitive surgery because they were selected to undergo DC surgery for a reason) [52].
Considering the above limitation, Stone et al., Rotondo et al., and Chinnery et al. each reported a large improvement in unadjusted survival when DC or staged laparotomy was used instead of definitive surgery to manage: (1) patients who developed a “major coagulopathy” during laparotomy, (2) hemodynamically unstable patients with combined abdominal vascular and pancreas gunshot injuries, and (3) those who received >10 U PRBCs and had ≥1 major abdominal vascular and ≥2 abdominal visceral injuries, respectively [9, 10, 53, 54]. Further, Rice and colleagues reported that, when compared to only minor deviations, moderate or major deviations from a protocol that suggested the use of DC surgery in patients with a temperature <35 °C, lactate >4 mmol/L (or more than twice the upper limit of normal), or corrected pH <7.3 were independently associated with improved survival [54, 55]. Finally, Asensio et al. reported that implementing a guideline that suggested the use of DC surgery for patients with 1 of 12 different clinical findings/events (transfusion >4 L PRBCs or >5 L PRBCs/whole blood combined; total OR fluid replacement >12 L; OR patient temperature ≤34°C, serum [HCO3-] ≤15 mEq/L, or arterial pH ≤7.2; a thoracic or abdominal vascular injury or complex hepatic injury requiring packing; those requiring ED or OR thoracotomy; or patients that develop intraoperative coagulopathy or dysrhythmias) was associated with a decreased unadjusted odds of infections, an increased unadjusted odds of abdominal wall closure, and a reduced unadjusted length of ICU and hospital stay [54, 56].
As DC surgery became widely adopted worldwide in the 1990s and 2000s, it was increasingly reported to be associated with a number of potentially severe and often resource-intensive complications considered by some (at least initially) to be “diseases of survivorship” [1, 54, 57, 58]. DC surgery and open abdominal management have been reported to be associated with an ~10–25% risk of an intra-abdominal abscess or abscesses, a mean of approximately five reoperations, an ~15% risk of readmission to hospital, and an ~8% risk of subsequent surgical procedures, especially those relating to massive or complex ventral herniae [54, 59,60,61]. Development of an enteroatmospheric fistula, defined as an enteric fistula in the middle of an open abdomen, occurs in approximately 5% of patients with an open abdominal wound and is considered to be a “surgical nightmare” by international surgical opinion leaders [54, 61, 62]. Defining characteristics include the absence of a fistula tract, the lack of well-vascularized surrounding tissue, a low probability of spontaneous closure, and the spillage of enteric content directly into the peritoneal cavity [8, 54, 62, 63]. These fistulae are difficult to control and may result in repeated episodes of intra-abdominal sepsis, long lengths of ICU and hospital stay, significant costs to the health-care system, and an elevated risk of mortality [54, 64]. Moreover, although many patients can ultimately have their abdomen closed after DC laparotomy, those who cannot are often managed with a “planned ventral hernia,” in which a split-thickness skin graft or mobilized native skin flap is used to cover the granulated viscera of the open abdomen, resulting in a massive and complex abdominal wall hernia that may be repaired using a components separation technique in 6–12 months [54, 65]. Possibly because of the above complications, survivors of open abdominal management have been reported to suffer from decreased physical functioning, a reduced quality of life (at least in the short term), and an increased incidence of depression and post-traumatic stress disorder [54, 66,67,68,69].
2.4 Variation in and Potential Harm Related to Overuse of DC Surgery Between Trauma Centers
Several authors have recently reported data suggesting that a variation in the use of DC laparotomy may exist across trauma centers or that the procedure may be overused [57, 70]. DC was used in 9% of patients undergoing emergent laparotomy at a level 1 trauma center in the United States in 2008 as compared to a relatively consistent rate of 29–37% in trauma patients at a different American level 1 center between 2004 and 2010 [54, 71, 72]. This variation in the use of DC across trauma centers could relate to increasing use of the procedure for indications other than those that have been previously studied or suggested to be appropriate in the literature [16, 54]. In support of this, one retrospective cohort study reported that one in five patients who received DC laparotomy at a level 1 trauma center between 2004 and 2008 failed to meet at least one of the traditional indications [16, 73]. In this study, only 33% were acidotic, 43% hypothermic, and 48% coagulopathic upon arrival to the ICU from the OR [16, 54, 73].
Variation in rates of use of DC surgery across trauma centers is concerning as accumulating evidence suggests that overutilization of the procedure for inappropriate indications may be associated with increased morbidity and mortality [57, 58, 70, 73,74,75]. In one retrospective cohort study conducted at a level 1 trauma center between 2005 and 2009, the use of DC instead of definitive laparotomy in trauma patients without severe head injury, a systolic blood pressure (BP) >90 mmHg, and no combined abdominal injuries was independently associated with a three times increased odds of major postoperative complications and a 10-day longer length of hospital stay [16, 75]. Further, in a propensity-matched cohort study conducted at the same trauma center, the use of DC instead of definitive laparotomy (for packing, hemodynamic instability, or intra-abdominal contamination; to facilitate a second look laparotomy, expedite postoperative care/interventions, or prophylax against ACS; or for other/unclear reasons) in injured patients was associated with a 13% increased probability of postoperative ileus, a 4% increased probability of postoperative gastrointestinal bleeding, an 11% increased probability of fascial dehiscence, a 19% increased probability of superficial surgical site infection, and an 18% increased probability of perioperative death [58].
Several other authors and I have therefore suggested that clinical outcomes and health system costs may improve with more selective use of DC surgery, especially given that DC resuscitation may effectively prevent or treat hypothermia, acidosis, and coagulopathy in trauma patients [1, 70]. In support of this, Higa et al. observed that the rate of use of DC decreased from 36 to 9% among trauma patients undergoing emergent laparotomy between 2006 and 2008 despite similar patient demographics and Injury Severity Scale (ISS) scores among the patients managed between these time periods [71]. This decline in the rate of use of DC laparotomy was associated with a significant improvement in primary fascial closure rates (50% in 2006 versus 86% in 2008), perioperative mortality (22% in 2006 versus 13% in 2008), and total hospital costs ($44,312 in 2006 versus $32,992 in 2008) among patients undergoing emergent trauma laparotomy [54, 71].
2.5 Published Consensus Indications for Use of DC Surgery and DC Interventions in Civilian Trauma Patients
Variation in the use of DC surgery between trauma centers may occur because surgeons are frequently uncertain which operative profile is best in varying clinical situations [15, 70, 76]. This uncertainty is likely exacerbated by the fact that limited data exists on the effectiveness and safety of DC surgery and DC interventions [15, 70, 76]. These procedures are also difficult to study, especially considering the multitude of potential clinical situations that may be encountered by surgeons who (routinely or uncommonly) perform emergent thoracic, abdominal, and/or peripheral vascular operations on injured patients across level 1, 2, and/or 3 trauma centers [15, 70, 76]. Despite this, however, surgeons must decide when to use DC (or specific DC interventions) over definitive surgery (or specific definitive surgical interventions) in their practice [15].
Therefore, the indications for trauma damage control international study group and I initiated a program of research in 2013 to determine the specific clinical situations in which the expected survival benefit of conducting DC surgery (or a specific DC intervention) is likely to exceed the expected risk of negative consequences [15, 16]. We first conducted a scoping review to synthesize the literature on DC surgery and DC interventions, identify a comprehensive list of their reported indications for use, and examine the content and evidence upon these indications were based [15, 54, 77]. An indication was defined as “a clinical finding/scenario that advised use of DC surgery (or a DC intervention) over definitive surgery (or a definitive surgical intervention)” [57]. This study identified 270 published, peer-reviewed articles (58% of which represented original research) that reported 1107 indications for DC surgery and 424 indications for the 16 different DC interventions previously listed in Table 2.1 [54, 77].
We used qualitative research methods to synthesize the above indications into 123 codes representing unique indications for DC surgery and 101 codes representing unique indications for DC interventions [15, 57]. Within these codes, we included summarized or commonly used decision thresholds for reported indications with cutoffs (e.g., temperature or pH <X) [15, 57]. In an expert appropriateness rating study, an international panel of trauma surgery experts (n = 9 surgeons) then rated 101 (82.1%) of the coded indications for DC surgery and 78 (77.2%) of the coded indications for DC interventions to be appropriate for use in surgical practice [15, 57].
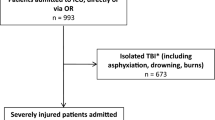
In 2014, we subsequently surveyed 366 surgeons who treat injured patients in level 1–3 trauma centers in the United States, Canada, Australia, and New Zealand to determine their opinions on the appropriateness of many of the indications rated in the expert appropriateness rating study [70]. In total, 201 (56.0%) of the surveyed surgeons responded [70]. These respondents rated 15 (78.9%) preoperative and 23 (95.8%) intraoperative indications to be appropriate for use in their practices [70]. There was substantial agreement between the opinions of practicing surgeons with different training, experience, and practice settings on the appropriateness of reported candidate indications for the use of DC surgery (Fig. 2.1) [70]. The reduced list of candidate indications for DC surgery that were rated to be appropriate by both experts and practicing surgeons (in both the expert appropriateness rating study and the survey of practicing surgeons) is listed in Table 2.2 [57, 70].
Color map of respondents’ appropriateness ratings of published candidate pre- and intraoperative indications for the use of damage control surgery stratified by surgeon- and trauma center-level characteristics, where ANZ indicates Australia and New Zealand (i.e., Australasia); BP, blood pressure; ED, emergency department; GSWs, gunshot wounds; INR, international normalized ratio; ISS, Injury Severity Scale; PT, prothrombin time; and PTT, partial thromboplastin time. Interpolated median values that lied halfway between two integers were rounded upward. Disagreement was defined as at least 33% of respondents rating the indication as 1–2 (significant harm-harm) on the Likert Scale and at least another 33% rating it 4–5 (benefit-significant benefit). Figure and figure legend reproduced with permission from reference [70]
Nearly all agreed that the expected benefits of DC surgery outweighed the expected risks when adults requiring emergent operation were found to have (1) persistent hemodynamic instability (systolic BP <90 mmHg) in the preoperative setting or during operation (or if they were reported to have a successfully resuscitated cardiac arrest during transport to hospital), (2) persistent hypothermia (core body temperature <34 °C) or acidosis (arterial pH <7.2) during operation, or (3) hypothermia, acidosis, and clinical (absence of visible blood clots during surgery) or laboratory [international normalized ratio (INR)/prothrombin time (PT) or partial thromboplastin time (PTT) >1.5 times normal] coagulopathy in the preoperative setting or during operation [54, 57, 70]. They also agreed that injured patients with physiologic derangements that improve or reverse during resuscitation and operation were candidates for definitive closure of their injured cavity at the end of the index operation [70]. These findings suggest that surgeons likely believe that unless patients present with or develop the entire lethal triad or have hypotension, hypothermia, and/or acidosis that persists during DC resuscitation (including the emergent operation for rapid hemorrhage control), it is likely frequently safe to perform a definitive (instead of DC) operation (provided that the other scenarios listed in Table 2.2 have not been encountered) [70].
Published indications that were independent of patient physiology and assessed to be appropriate by experts and the broader surgical community included an estimated blood loss >4 L, the administration of a massive transfusion (>10 U) of PRBCs, and the identification of one of the four different injury patterns during operation [57, 70]. The assessment of massive blood loss or requirement for massive transfusion as appropriate indications for DC surgery is not surprising as DC surgery has long been used as a strategy to improve the increased morbidity and mortality associated with exsanguination in trauma patients [78,79,80]. Further, the above injury patterns assessed to appropriately indicate the use of DC are characteristic of those that (1) often result in exsanguination during exposure and attempts at definitive repair (juxtahepatic venous injuries), (2) require urgent transport to the angiography suite for embolization soon after they are discovered intraoperatively (an expanding and difficult to access pelvic hematoma), (3) are complicated by competing management priorities (hemorrhage and contamination) or multifocal hemorrhage (an abdominal vascular injury and at least one major associated abdominal solid or hollow organ injury), or (4) require a pancreaticoduodenectomy (devascularization or destruction of the pancreas, duodenum, or pancreaticoduodenal complex) [70, 81, 82].
Table 2.3 provides a list of the indications for the use of DC interventions that were assessed by the expert panel to be appropriate for use in the ED or OR setting [15]. Interestingly, several of the indications for the use of DC surgery and intraoperative DC interventions were identical or nearly identical [15, 54, 57]. Experts assessed these identical or nearly identical indications to have a similar appropriateness for use in practice [15, 54, 57]. Thus, surgeons may believe that in certain intraoperative circumstances, one or more specific DC interventions should be preferentially performed when patients are selected to undergo DC surgery [54]. These include extraperitoneal pelvic packing (severe pelvic trauma and an expanding and difficult to access pelvic hematoma or massive, ongoing hemorrhage in the OR), therapeutic perihepatic packing (a juxtahepatic venous injury), and staged pancreaticoduodenectomy (devascularization of massive disruption of the pancreas, duodenum, or pancreaticoduodenal complex) [15, 54, 57, 70]. Finally, the expert panel suggested that DC surgery and TAC/open abdominal management were appropriate when patients have been administered a large volume of crystalloid fluids and/or PRBCs, when the abdominal wall is unable to be closed without tension at the conclusion of laparotomy, or when signs of post-injury ACS develop during attempted abdominal wall closure [15, 54, 57].
The above indications may be used as a type of consensus opinion to guide surgical practice in the current era of DC resuscitation [70]. They may also be used to educate surgical trainees and surgeons on the appropriate use of DC surgery and DC interventions in practice, to guide trauma center quality improvement practices regarding choice of operative profile (through morbidity and mortality rounds, audit and feedback, and other mechanisms), and to design future (adjusted/propensity-matched) prospective observational and experimental studies focused on examining outcomes between patients treated with DC (or a specific DC intervention) versus definitive surgery (or a specific definitive surgical intervention) [54].
2.6 Summary
Modern trauma DC integrates the stages of DC surgery into the process of DC resuscitation. Although widely believed to improve survival when appropriately indicated, there is limited evidence supporting a benefit of DC surgery in injured patients [1, 16]. Further, the procedure is associated with a number of potentially severe and often resource-intensive complications [1, 57, 58]. Several studies have recently reported data suggesting that a variation exists in the use of DC laparotomy across trauma centers or that the procedure may be overused [57, 70]. These and other studies have also suggested that overutilization of the procedure may be associated with increased morbidity and mortality [57, 58, 70, 73,74,75]. The list of indications identified as being appropriate by both experts and practicing surgeons described in this chapter may be used to guide practice and reduce variation in the use of DC surgery until results of appropriately designed prospective studies become available in the future [54].
References
Roberts DJ, Ball CG, Feliciano DV, Moore EE, Ivatury RR, Lucas CE, et al. History of the innovation of damage control for management of trauma patients: 1902-2016. Ann Surg. 2017;265(5):1034–44.
Elerding SC, Aragon GE, Moore EE. Fatal hepatic hemorrhage after trauma. Am J Surg. 1979;138(6):883–8.
Kashuk JL, Moore EE, Millikan JS, Moore JB. Major abdominal vascular trauma--a unified approach. J Trauma. 1982;22(8):672–9.
Malbrain ML, Vidts W, Ravyts M, De Laet I, De Waele J. Acute intestinal distress syndrome: the importance of intra-abdominal pressure. Minerva Anestesiol. 2008;74(11):657–73.
Malbrain ML, De Laet I. It’s all in the gut: introducing the concept of acute bowel injury and acute intestinal distress syndrome. Crit Care Med. 2009;37(1):365–6.
Burch JM, Moore EE, Moore FA, Franciose R. The abdominal compartment syndrome. Surg Clin N Am. 1996;76(4):833–42.
Meldrum DR, Moore FA, Moore EE, Franciose RJ, Sauaia A, Burch JM. Prospective characterization and selective management of the abdominal compartment syndrome. Am J Surg. 1997;174(6):667–72. discussion 72-3
Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the world Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190–206.
Stone HH, Strom PR, Mullins RJ. Management of the major coagulopathy with onset during laparotomy. Ann Surg. 1983;197(5):532–5.
Rotondo MF, Schwab CW, McGonigal MD, Phillips GR 3rd, Fruchterman TM, Kauder DR, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35(3):375–82. discussion 82-3
Ivatury RR, Porter JM, Simon RJ, Islam S, John R, Stahl WM. Intra-abdominal hypertension after life-threatening penetrating abdominal trauma: prophylaxis, incidence, and clinical relevance to gastric mucosal pH and abdominal compartment syndrome. J Trauma. 1998;44(6):1016–21. discussion 21-3
Feliciano DV, Burch JM, Spjut-Patrinely V, Mattox KL, Jordan GL Jr. Abdominal gunshot wounds. An urban trauma center’s experience with 300 consecutive patients. Ann Surg. 1988;208(3):362–70.
Rotondo MF, Zonies DH. The damage control sequence and underlying logic. Surg Clin N Am. 1997;77(4):761–77.
Ball CG. Damage control surgery. Curr Opin Crit Care. 2015;21(6):538–43.
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, et al. Indications for use of thoracic, abdominal, pelvic, and vascular damage control interventions in trauma patients: a content analysis and expert appropriateness rating study. J Trauma Acute Care Surg. 2015;79(4):568–79.
Roberts DJ, Zygun DA, Kirkpatrick AW, Ball CG, Faris PD, Bobrovitz N, et al. A protocol for a scoping and qualitative study to identify and evaluate indications for damage control surgery and damage control interventions in civilian trauma patients. BMJ Open. 2014;4(7):e005634.
Johnson JW, Gracias VH, Schwab CW, Reilly PM, Kauder DR, Shapiro MB, et al. Evolution in damage control for exsanguinating penetrating abdominal injury. J Trauma. 2001;51(2):261–9. discussion 9-71
Ramirez OM, Ruas E, Dellon AL. "Components separation" method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990;86(3):519–26.
Petrone P, Asensio JA. Surgical management of penetrating pulmonary injuries. Scand J Trauma Resusc Emerg Med. 2009;17:8.
Trauma. 7th ed. China: McGraw Hill Companies Inc.; 2013.
Asensio JA, Mazzini FN, Perez-Alonso AJ, Petrone P, Ceballos J, Karsidag T, et al. Pulmonary injuries. In: Cioffi WG, Asensio JA, Adams CA, Biffl WL, Connolly MD, Jurkovich GJ, editors. Atlas of trauma/emergency surgical techniques. Philadelphia, PA: Elsevier Saunders; 2014. p. 93–104.
Wall MJ Jr, Hirshberg A, Mattox KL. Pulmonary tractotomy with selective vascular ligation for penetrating injuries to the lung. Am J Surg. 1994;168(6):665–9.
Asensio JA, Demetriades D, Berne JD, Velmahos G, Cornwell EE 3rd, Murray J, et al. Stapled pulmonary tractotomy: a rapid way to control hemorrhage in penetrating pulmonary injuries. J Am Coll Surg. 1997;185(5):486–7.
Wagner JW, Obeid FN, Karmy-Jones RC, Casey GD, Sorensen VJ, Horst HM. Trauma pneumonectomy revisited: the role of simultaneously stapled pneumonectomy. J Trauma. 1996;40(4):590–4.
Chovanes J, Cannon JW, Nunez TC. The evolution of damage control surgery. Surg Clin N Am. 2012;92(4):859–75. vii-viii
Rotondo MF, Bard MR. Damage control surgery for thoracic injuries. Injury. 2004;35(7):649–54.
Caceres M, Buechter KJ, Tillou A, Shih JA, Liu D, Steeb G. Thoracic packing for uncontrolled bleeding in penetrating thoracic injuries. South Med J. 2004;97(7):637–41.
Moriwaki Y, Toyoda H, Harunari N, Iwashita M, Kosuge T, Arata S, et al. Gauze packing as damage control for uncontrollable haemorrhage in severe thoracic trauma. Ann R Coll Surg Engl. 2013;95(1):20–5.
Vargo DJ, Battistella FD. Abbreviated thoracotomy and temporary chest closure: an application of damage control after thoracic trauma. Arch Surg. 2001;136(1):21–4.
Rosenblatt MS, Aldridge SC, Millham FH, Woodson J, Hirsch EF. Temporary thoracotomy wound closure following penetrating thoracic aorta injury. Military Med. 1993;158(1):58–9.
Eastlick L, Fogler RJ, Shaftan GW. Pancreaticoduodenectomy for trauma: delayed reconstruction: a case report. J Trauma. 1990;30(4):503–5.
Carrillo C, Fogler RJ, Shaftan GW. Delayed gastrointestinal reconstruction following massive abdominal trauma. J Trauma. 1993;34(2):233–5.
Koniaris LG, Mandal AK, Genuit T, Cameron JL. Two-stage trauma pancreaticoduodenectomy: delay facilitates anastomotic reconstruction. J Gastrointest Surg. 2000;4(4):366–9.
Ivatury RR, Nassoura ZE, Simon RJ, Rodriguez A. Complex duodenal injuries. Surg Clin N Am. 1996;76(4):797–812.
Coburn M. Damage control for urological injuries. Surg Clin N Am. 1997;77(4):821–34.
Ertel W, Keel M, Eid K, Platz A, Trentz O. Control of severe hemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. J Orthop Trauma. 2001;15(7):468–74.
Smith WR, Moore EE, Osborn P, Agudelo JF, Morgan SJ, Parekh AA, et al. Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: report of two representative cases and a description of technique. J Trauma. 2005;59(6):1510–4.
Cothren CC, Osborn PM, Moore EE, Morgan SJ, Johnson JL, Smith WR. Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: a paradigm shift. J Trauma. 2007;62(4):834–9. discussion 9-42
DuBose J, Inaba K, Barmparas G, Teixeira PG, Schnuriger B, Talving P, et al. Bilateral internal iliac artery ligation as a damage control approach in massive retroperitoneal bleeding after pelvic fracture. J Trauma. 2010;69(6):1507–14.
Morimoto RY, Birolini D, Junqueira AR Jr, Poggetti R, Horita LT. Balloon tamponade for transfixing lesions of the liver. Surg Gynecol Obstet. 1987;164(1):87–8.
Poggetti RS, Moore EE, Moore FA, Mitchell MB, Read RA. Balloon tamponade for bilobar transfixing hepatic gunshot wounds. J Trauma. 1992;33(5):694–7.
Feliciano DV, Burch JM, Mattox KL, Bitondo CG, Fields G. Balloon catheter tamponade in cardiovascular wounds. Am J Surg. 1990;160(6):583–7.
Gilroy D, Lakhoo M, Charalambides D, Demetriades D. Control of life-threatening haemorrhage from the neck: a new indication for balloon tamponade. Injury. 1992;23(8):557–9.
Ball CG, Wyrzykowski AD, Nicholas JM, Rozycki GS, Feliciano DVA. Decade’s experience with balloon catheter tamponade for the emergency control of hemorrhage. J Trauma. 2011;70(2):330–3.
Ding W, Wu X, Li J. Temporary intravascular shunts used as a damage control surgery adjunct in complex vascular injury: collective review. Injury. 2008;39(9):970–7.
Subramanian A, Vercruysse G, Dente C, Wyrzykowski A, King E, Feliciano DV. A decade’s experience with temporary intravascular shunts at a civilian level I trauma center. J Trauma. 2008;65(2):316–24. discussion 24-6
Bogert JN, Harvin JA, Cotton BA. Damage control resuscitation. J Intensive Care Med. 2014.
Hess JR, Holcomb JB, Hoyt DB. Damage control resuscitation: the need for specific blood products to treat the coagulopathy of trauma. Transfusion. 2006;46(5):685–6.
Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62(2):307–10.
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471–82.
Cirocchi R, Montedori A, Farinella E, Bonacini I, Tagliabue L, Abraha I. Damage control surgery for abdominal trauma. Cochrane Database Syst Rev. 2013;28(3):CD007438.
Sox HC, Goodman SN. The methods of comparative effectiveness research. Annu Rev Public Health. 2012;33:425–45.
Chinnery GE, Krige JE, Kotze UK, Navsaria P, Nicol A. Surgical management and outcome of civilian gunshot injuries to the pancreas. Br J Surg. 2012;99(Suppl 1):140–8.
Roberts DJ. Identification and evaluation of the indications for use of damage control surgery and damage control interventions in civilian trauma patients: Doctor of Philosophy (Specialization in Epidemiology) Thesis. Department of Community Health Sciences, University of Calgary; 2015. P. 402.
Rice TW, Morris S, Tortella BJ, Wheeler AP, Christensen MC. Deviations from evidence-based clinical management guidelines increase mortality in critically injured trauma patients*. Crit Care Med. 2012;40(3):778–86.
Asensio JA, McDuffie L, Petrone P, Roldan G, Forno W, Gambaro E, et al. Reliable variables in the exsanguinated patient which indicate damage control and predict outcome. Am J Surg. 2001;182(6):743–51.
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, et al. Indications for use of damage control surgery in civilian trauma patients: a content analysis and expert appropriateness rating study. Ann Surg. 2016;263(5):1018–27.
Harvin JA, Wray CJ, Steward J, Lawless RA, MvcNutt MK, Love JD, et al. Control the damage: morbidity and mortality after emergent trauma laparotomy. Am J Surg. 2016;212(1):34–9.
Miller RS, Morris JA Jr, Diaz JJ Jr, Herring MB, May AK. Complications after 344 damage-control open celiotomies. J Trauma. 2005;59(6):1365–71. discussion 71-4
Montalvo JA, Acosta JA, Rodriguez P, Alejandro K, Sarraga A. Surgical complications and causes of death in trauma patients that require temporary abdominal closure. Am Surg. 2005;71(3):219–24.
Dubose JJ, Scalea TM, Holcomb JB, Shrestha B, Okoye O, Inaba K, et al. Open abdominal management after damage-control laparotomy for trauma: a prospective observational American Association for the Surgery of Trauma multicenter study. J Trauma Acute Care Surg. 2013;74(1):113–20. discussion 1120-2
Di Saverio S, Tarasconi A, Inaba K, Navsaria P, Coccolini F, Navarro DC, et al. Open abdomen with concomitant enteroatmospheric fistula: attempt to rationalize the approach to a surgical nightmare and proposal of a clinical algorithm. J Am Coll Surg. 2015;220(3):e23–33.
Bjorck M, Kirkpatrick AW, Cheatham M, Kaplan M, Leppaniemi A, De Waele JJ. Amended classification of the open abdomen. Scand J Surg. 2016;105(1):5–10.
Demetriades D, Salim A. Management of the open abdomen. Surg Clin N Am. 2014;94(1):131–53.
Fabian TC, Croce MA, Pritchard FE, Minard G, Hickerson WL, Howell RL, et al. Planned ventral hernia. Staged management for acute abdominal wall defects. Ann Surg. 1994;219(6):643–50. discussion 51-3
Zarzaur BL, DiCocco JM, Shahan CP, Emmett K, Magnotti LJ, Croce MA, et al. Quality of life after abdominal wall reconstruction following open abdomen. J Trauma. 2011;70(2):285–91.
Codner PA, Brasel KJ, Deroon-Cassini TA. Staged abdominal repairs reduce long-term quality of life. Injury. 2012;43(9):1513–6.
Cheatham ML, Safcsak K, Llerena LE, Morrow CE Jr, Block EF. Long-term physical, mental, and functional consequences of abdominal decompression. J Trauma. 2004;56(2):237–41. discussion 41-2
Cheatham ML, Safcsak K. Longterm impact of abdominal decompression: a prospective comparative analysis. J Am Coll Surg. 2008;207(4):573–9.
Roberts DJ, Zygun DA, Faris PD, Ball CG, Kirkpatrick AW, Stelfox HT. Opinions of practicing surgeons on the appropriateness of published indications for use of damage control surgery in trauma patients: an international cross-sectional survey. J Am Coll Surg. 2016;223(3):515–29.
Higa G, Friese R, O’Keeffe T, Wynne J, Bowlby P, Ziemba M, et al. Damage control laparotomy: a vital tool once overused. J Trauma. 2010;69(1):53–9.
Cotton BA, Reddy N, Hatch QM, LeFebvre E, Wade CE, Kozar RA, et al. Damage control resuscitation is associated with a reduction in resuscitation volumes and improvement in survival in 390 damage control laparotomy patients. Ann Surg. 2011;254(4):598–605.
Hatch QM, Osterhout LM, Podbielski J, Kozar RA, Wade CE, Holcomb JB, et al. Impact of closure at the first take back: complication burden and potential overutilization of damage control laparotomy. J Trauma. 2011;71(6):1503–11.
Hatch QM, Osterhout LM, Ashraf A, Podbielski J, Kozar RA, Wade CE, et al. Current use of damage-control laparotomy, closure rates, and predictors of early fascial closure at the first take-back. J Trauma. 2011;70(6):1429–36.
Martin MJ, Hatch Q, Cotton B, Holcomb J. The use of temporary abdominal closure in low-risk trauma patients: helpful or harmful? J Trauma Acute Care Surg. 2012;72(3):601–6. discussion 6-8
Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121–9.
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, et al. Indications for use of damage control surgery and damage control interventions in civilian trauma patients: a scoping review. J Trauma Acute Care Surg. 2015;78(6):1187–96.
Wade CE, del Junco DJ, Holcomb JB, Holcomb JB, Wade CE, Brasel KJ, et al. Variations between level I trauma centers in 24-hour mortality in severely injured patients requiring a massive transfusion. J Trauma. 2011;71(2 Suppl 3):S389–93.
Rahbar E, Fox EE, del Junco DJ, Harvin JA, Holcomb JB, Wade CE, et al. Early resuscitation intensity as a surrogate for bleeding severity and early mortality in the PROMMTT study. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S16–23.
Asensio JA, Petrone P, O’Shanahan G, Kuncir EJ. Managing exsanguination: what we know about damage control/bailout is not enough. Proc (Bayl Univ Med Cent). 2003;16(3):294–6.
Buckman RF Jr, Miraliakbari R, Badellino MM. Juxtahepatic venous injuries: a critical review of reported management strategies. J Trauma. 2000;48(5):978–84.
Asensio JA, Petrone P, Roldan G, Kuncir E, Demetriades D. Pancreaticoduodenectomy: a rare procedure for the management of complex pancreaticoduodenal injuries. J Am Coll Surg. 2003;197(6):937–42.
Disclosure
I have no conflicts of interest to declare.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Roberts, D.J. (2018). Applications of Damage Control Surgery in Modern Civilian Trauma Care. In: Duchesne, J., Inaba, K., Khan, M. (eds) Damage Control in Trauma Care. Springer, Cham. https://doi.org/10.1007/978-3-319-72607-6_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-72607-6_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72606-9
Online ISBN: 978-3-319-72607-6
eBook Packages: MedicineMedicine (R0)