Abstract
Immune checkpoint inhibitors (ICI) represent a class of immuno-oncology drugs consisting of monoclonal antibodies occurring against inhibitory receptors or ligands within the immune system including CTLA-4, PD-1, and PD-L1. ICI has transformed oncology in the last decade leading to increased response rates and improved overall survival across several advanced malignancies. ICI is associated with a unique array of toxicities termed immune-related adverse events (IrAEs) which are T-cell-mediated autoimmune toxicities reported in nearly every organ system; most commonly affecting the skin, liver, gastrointestinal tract, and endocrine system. Most IrAEs are manageable with prompt recognition and initiation of appropriate management. General treatment of IrAEs is based on immunosuppression using varying strengths of glucocorticoids. Severe steroid-refractory IrAEs have required nonsteroidal immunosuppressive agents. In this chapter, we describe IrAEs observed with CTLA-4 and PD-1/PDL-1 inhibition by system describing clinical presentation, grading, incidence, time of onset, management, and time to resolution.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Immune-related adverse events
- Immune checkpoint inhibition
- Cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4)
- Programmed cell death-1 (PD-1)
- Side effects
- Toxicity
- Immunotherapy
- Rash
- Vitiligo
- Pruritus
- Diarrhea
- Colitis
- Hepatitis
- Pneumonitis
- Hypophysitis
- Thyroiditis
- Nephritis
12.1 Immune Checkpoint Inhibition
In the past 10 years, immune checkpoint inhibition (ICI) has transformed the management of advanced cancer. Checkpoint inhibitors represent a class of drugs consisting of monoclonal antibodies (mAbs) against naturally occurring inhibitory receptors within the immune system, called “immune checkpoints.” In healthy individuals, these immune checkpoints function to downregulate the immune response, prevent autoimmunity, and limit damage to normal tissue following activation of the immune response. Immune checkpoints are also up-regulated in several tumors and are involved in tumor escape mechanisms from immune surveillance. By blocking an inhibitory pathway, treatment with immune checkpoint inhibitors unleashes the immune response and has been shown to have an antitumor effect in several malignancies [1].
Inhibitors of CTLA-4, PD-1 , and programmed cell death ligand-1 (PD-L1) immune checkpoints are currently commercially available or under clinical investigation across multiple malignancies. Ipilimumab, a CTLA-4 inhibitor, became the first ICI to achieve Federal Drug Administration (FDA) approval in 2011, when it was approved for metastatic melanoma on the basis of improved survival in a phase III clinical trial [2]. Its label has since been expanded to include the use of adjuvant treatment for patients with stage III melanoma [3]. Ipilimumab has been studied at different doses and schedules, and its toxicity is dose dependent [4]. The PD-1 inhibitor pembrolizumab is also FDA approved for advanced melanoma [5] as well as metastatic non-small cell lung carcinoma (NSCLC) [6] both second line [7] and first line [8] based on phase III trials showing survival benefit in both of those settings. FDA approval has also been granted for pembrolizumab in squamous cell carcinoma of the head and neck (SCCHN) after progression on platinum-based chemotherapy, refractory classical Hodgkin’s lymphoma treated with greater than three lines of therapy [9], metastatic urothelial carcinoma not eligible for or after progression on cisplatin-based chemotherapy [10], and microsatellite instability-high (MSI-H) solid tumors with no alternative options [11]. Another PD-1 inhibitor nivolumab is FDA approved for metastatic NSCLC [12, 13], metastatic renal cell carcinoma (RCC) [14], and squamous cell carcinoma of the head and neck (SCCHN) [13], based on improved survival in phase III trials. Nivolumab was also recently granted accelerated approval in the treatment of relapsed refractory Hodgkin’s lymphoma and metastatic urothelial carcinoma that is platinum refractory based on the results of phase II trials [15, 16]. The PD-L1 inhibitor atezolizumab is approved for cisplatin-ineligible metastatic urothelial carcinoma [17], as well as NSCLC [18]. Durvalumab and avelumab both recently received accelerated approval for platinum refractory advanced or metastatic urothelial carcinoma [19, 20]. In addition to these FDA-approved indications, PD-1 and PD-L1 inhibitors have shown activity in several tumor types [11, 17, 21, 22], and more regulatory approvals are anticipated. Multiple mAbs against PD-1 and programmed cell death ligand-1 (PD-L1) are under development, expanded regulatory approval of these agents and others are anticipated in Europe and globally, and our understanding of the biology of these agents continues to rapidly grow. This chapter will discuss ICIs that have passed regulatory approval and are commercially available for oncologic practice outside of clinical trials shown in Table 12.1.
ICI clinical trials have generally excluded patients with underlying autoimmune disease, a medical condition requiring systemic treatment with corticosteroids or other immunosuppressive medication, hepatitis B or C, or a history of HIV. However, a number of retrospective case series have suggested that ICI is possible in patients with underlying autoimmune disorders or hepatitis. The use can be associated with exacerbations of autoimmune disease, and it is important to weigh the risks and benefits of therapy on an individual patient basis [23].
12.2 Immune-Related Adverse Events: Overview
The benefits of ICI are numerous, including increased response rates and improved overall survival in several malignancies. The price for these benefits is a new toxicity profile that is distinct from the side effects of cytotoxic chemotherapy and other targeted agents. ICI is associated with a unique array of toxicities termed immune-related adverse events (irAEs). IrAEs are T-cell-mediated autoimmune toxicities reported in every organ system but most commonly affecting the skin, liver, gastrointestinal tract, and endocrine system. Histopathological analysis of affected organs usually reveals T-cell-rich lymphocytic and neutrophilic infiltration. IrAEs are theorized to be caused by immune recognition and activation against self-antigens that would normally be dampened by intact immune surveillance.
The overall incidence of all-grade and high-grade irAEs with CTLA-4 checkpoint blockade is 72% and 24%, respectively, with death occurring in less than 1% of patients [4]. IrAEs associated with CTLA-4 inhibition most commonly occur in the dermatologic (44%), gastrointestinal (35%), hepatic (5%), and endocrine (6%) systems. Other rare events have included neurologic, hematologic, ophthalmologic, or rheumatologic diseases [4].
Compared to treatment with CTLA-4 mAbs, PD-1 /PD-L1 inhibition results in less frequent and less severe irAEs. There is a lack of standardization of reporting irAEs across trials making cumulative incidence reporting difficult. All-grade toxicity, both immune and nonimmune, for anti-PD-1 mAbs occurs in 58–79% of patients with high-grade toxicity observed in 7–19% [13, 14, 24]. A pooled safety analysis of nivolumab in 4 phase I–III clinical trials including 576 patients with advanced melanoma found grade 3–4 irAEs in 4% of patients with no drug-related deaths [25]. Most common irAEs included the skin (34%), GI tract (13%), endocrine glands (8%), and liver (4%).
Combination of ipilimumab and nivolumab therapy has a higher incidence and severity of irAEs than either agent alone. This increased toxicity was demonstrated in a phase III study assessing combined nivolumab and ipilimumab or monotherapy in untreated metastatic melanoma leading to grade 3 or 4 toxicity in more than half of patients [26]. An analysis of the expanded access program for ipilimumab and nivolumab at one institution reported that nearly half of all patients were hospitalized at least once during a course of therapy, most commonly related to severe irAEs [25].
The Common Terminology Criteria for Adverse Events (CTCAE) is a set of standardized definitions for adverse events published by the National Cancer Institute. It consists of a grading severity score from 1 to 5 with associated descriptive terminology. These criteria are widely accessible and can be found at http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf [27]. More specific irAE grading systems have been proposed but not yet adopted. There is marked heterogeneity in irAE reporting across trials and a need for standardization.
Patient reporting and physician recognition are encouraged as soon as possible because outcomes in irAE treatment are time sensitive. IrAEs are manageable with prompt recognition and initiation of appropriate management usually resulting in reversibility. General treatment of irAEs is based on immunosuppression using varying strengths of glucocorticoids. More severe grade irAEs that are steroid refractory have required nonsteroidal immunosuppressive agents. Surgical intervention for severe colitis leading to perforation has also been required. Fatigue, nausea, asthenia, pyrexia, and infusion reactions are common side effects of ICI. The management of these side effects is supportive and will not be discussed.
In this chapter, we describe irAEs observed with mAbs targeting CTLA-4 and PD-1 /PDL-1 by system describing clinical presentation, grading, incidence, time of onset, management, and time to resolution. ICI is a new and rapidly evolving therapeutic class; therefore, its toxicity profile, incidence, and management are continually under investigation and ongoing.
12.3 Cutaneous Toxicity
12.3.1 Clinical Presentation
Cutaneous toxicities are common irAEs for both CTLA-4 and PD-1 inhibition including rash (maculopapular, lichenoid, eczema, etc.), vitiligo -like skin hypopigmentation, and pruritus. Severe and life-threatening cutaneous toxicity such as Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis are rare but have occurred.
12.3.1.1 Rash
Several diverse presentations of rash can manifest including maculopapular, lichenoid, eczema, Sweet’s syndrome, urticarial dermatitis, bullous pemphigoid, TENS, and SJS. The rash most commonly observed with ICI is similar to drug rash seen in commonly used medications such as antibiotics, nonsteroidal anti-inflammatory drugs [28]. This entity is described as discrete, erythematous, pruritic papules coalescing into thin plaques. The rash most often involves the trunk and extremities; sparing the face, head, palms, and soles. These lesions can be pruritic but are not always. Histologically, biopsy of these lesions has shown perivascular immune cell infiltrates in superficial dermis extending to the epidermis with lymphoid aggregates composed of a mixture of CD4+ and CD8+ T cells [29]. Figure 12.1 demonstrates a typical maculopapular rash seen with ipilimumab therapy for advanced melanoma.
Two cases of rash related to ipilimumab in patients with metastatic melanoma. (a) Generalized erythema, erythematous macules, and papules. (b) Generalized erythema, erythematous macules, erythematous and some heme-crusted papules, and exfoliative scale on upper extremities. Adapted from Kira Minkis, Benjamin C. Garden, Shenhong Wu, Melissa P. Pulitzer, Mario E. Lacouture. The risk of rash associated with ipilimumab in patients with cancer: A systematic review of the literature and meta-analysis. Journal of the American Academy of Dermatology, Volume 69, Issue 3, 2013, e121–e128
Lichenoid reactions have been described in several patients receiving anti-PD-1 mAbs [30]. These lesions are characterized as multiple discrete, erythematous, violaceous, papules, or plaques mainly on the chest or back sparing mucous membranes. Figure 12.2 demonstrates three cases of lichenoid reactions manifesting after ICI.
Three cases of cutaneous lichenoid drug eruption from PD-L1 inhibition. Case 1: (a) erythematous to violaceous eruption of hyperkeratotic papules and plaques on the legs of case 1. (b) Close-up view of lesion on upper extremity. Case 2: (c) discrete, erythematous, edematous papules and plaques with minimal scaling of the torso and extremities with sparing of the face. (d) Close-up view of lesions on lower back. Case 3: (e) papular eruption with monomorphic, flat-topped, faintly erythematous papules and plaques with fine scale distributed over his chest, back, and abdomen. (f) Close-up view of lesions on shoulder. Adapted from Ref. [31]
Biopsy revealed lichenoid interface dermatitis with occasional eosinophils and scattered apoptotic basal keratinocytes consistent with a lichenoid drug reaction. CD3-positive infiltrate with approximately 10% of the T cells staining positive for PD-1 [31].
Severe, life-threatening rashes are rarely seen in ICI. Bullous pemphigoid has been described in anti-PD-1 mAb treatment [30, 32]. Toxic epidermal necrolysis has been seen with anti-CTLA-4 and anti-PD-1 mAbs [2, 33]. Any rash complicated by full-thickness dermal ulceration, necrosis, bullous, or hemorrhagic manifestations should be considered severe and treated accordingly.
12.3.1.2 Skin Hypopigmentation/Vitiligo
Vitiligo -like depigmentation is a harmless autoimmune toxicity that can be esthetically distressing to patients. Vitiligo presents as the presence of pale, patchy areas of depigmented skin. The hypopigmentation results from strong anti-melanocyte immunity that also targets healthy melanocytes in the case of advanced melanoma treated with anti-CTLA-4 and anti-PD-1 mAbs [34]. The cumulative incidence of vitiligo was 2.0% in a large meta-analysis of patients with stage III–IV melanoma receiving immunotherapy including CTLA-4 blockade or anti-PD-1 mAbs [34]. However, vitiligo has been seen in up to 10% of melanoma patients treated with anti-PD-1 mAbs [24].
Development of vitiligo is associated with significant progression-free survival and overall survival in advanced melanoma, which can be encouraging to both the patient and physician [34]. Vitiligo occurs often in melanoma patients treated with ICI but is less frequently reported in other malignancies including NSCLC and RCC clinical trials.
12.3.1.3 Pruritus
Development of pruritus with ICI is relatively common with or without associated rash. Pruritus is an unpleasant skin sensation that provokes scratching that can lead to self-inflicted skin changes such as edema, papulation, excoriations, and lichenification. This sensation can be very distressing to patients and can markedly impact quality of life.
12.3.2 Grading
The CTCAE (version 4.03 published June 14, 2010) for rash maculopapular, vitiligo , and pruritus is below. Rash grading is based on body surface area (BSA) involvement and quality of life. Surface area quantification can be difficult to calculate, and the Lund and Browder chart shown below in Fig. 12.3 can be used for accurate quantification [35]. Any skin toxicity that is life-threatening is considered grade 4. Any skin toxicity leading to death is considered grade 5.
Rash maculopapular:
-
Grade 1: Macules/papules covering <10% BSA with or without symptoms (pruritus, burning, tightness)
-
Grade 2: Macules/papules covering 10–30% BSA with or without symptoms (pruritus, burning, tightness); limiting instrumental ADL
-
Grade 3: Macules/papules covering >30% BSA with or without symptoms (pruritus, burning, tightness); limiting self-care ADL
Skin hypopigmentation (vitiligo ):
-
Grade 1: Hypopigmentation or depigmentation covering <10% BSA; no psychosocial impact
-
Grade 2: Hypopigmentation or depigmentation covering >10% BSA; no psychosocial impact
Pruritus:
-
Grade 1: Mild or localized; topical intervention indicated
-
Grade 2: Intense or widespread; intermittent; skin changes from scratching (edema, papulation, excoriations, lichenification, oozing/crusts); oral intervention indicated; limiting instrumental ADL
-
Grade 3: Intense or widespread; constant; limiting self-care ADL or sleep; oral corticosteroid or immunosuppressive therapy indicated
12.3.3 Incidence
The incidence and severity of dermatologic irAEs vary in different tumor types with the highest rates of skin toxicity occurring in melanoma. Cutaneous irAEs of all grades occur in approximately 40% of patients treated with PD-1 inhibition and between 40 and 50% treated with CTL-4 inhibition in advanced melanoma [4, 30, 36, 37]. Severe (grade 3 or 4) cutaneous reactions are rare occurring in <2% of patients with anti-CTLA-4 mAbs and <1% with anti-PD-1 mAbs.
A recent meta-analysis performed including 1265 melanoma patients from 22 clinical trials treated with anti-CTLA-4 mAbs found all-grade skin toxicity in 44% of patients and high-grade toxicity in 1.4% [4]. A recent pooled safety analysis of four clinical trials of BRAF wild-type melanoma patients treated with nivolumab found the following cutaneous toxicities: pruritus (16.5%), rash (12%), vitiligo (5.4%), and maculopapular rash (5.4%) [38].
All dermatologic toxicity occurs less frequently in the treatment of other solid tumors such as NSCLC and renal carcinoma. The use of pembrolizumab in 495 patients with advanced NSCLC led to grade 1 or 2 cutaneous toxicity in only 10% of patients with only 1 patient developing grade 3 or 4 cutaneous toxicity [6].
Rare cases of severe rash including Stevens-Johnson syndrome, bullous pemphigoid, and toxic epidermal necrolysis are reported in <1% of patients [2, 32, 33].
12.3.4 Time of Onset
Skin toxicity is usually the earliest irAE to occur. Median time to onset of moderate, severe, or life-threatening immune-mediated rash is 3 weeks and ranged up to 4.0 months with ipilimumab [39, 40]. The median time to onset of cutaneous toxicity with nivolumab therapy was 5 weeks in a pooled safety analysis [25].
12.3.5 Management
Algorithms have been developed to aid in the treatment of skin toxicity and are recommended [35, 41]. Providers should encourage the use of moisturizers, limited sun exposure, and UV protection. Grade 1 toxicity can be treated for symptomatic relief with topical corticosteroid ointments, oral antihistamines such as diphenhydramine or hydroxyzine, and moisturizing lotions. Serum liver and renal function tests should be performed. Grade 1 cutaneous toxicity does not require interruption in of ICI.
For grade 2 skin toxicity, symptomatic relief as well as topical corticosteroids can be used initially. Systemic corticosteroids should be considered at 0.5 mg/kg/day prednisone or equivalent if there is no improvement in symptoms within 1 week. Experienced practitioners recommend continuation of ICI if patients are asymptomatic and have involvement of <30% of body surface area or toxicity can be managed with topical corticosteroid creams and antihistamines. For patients with 10–30% of body surface area involvement that is symptomatic, ICI should be held, and steroids at 0.5–1 mg/kg prednisone or equivalent should be administered for control of symptoms. Dermatologic evaluation and biopsy should be considered.
For grade 3 skin toxicity, ICI should be held. Patients should be given symptom management and 1–2 mg/kg prednisone or equivalent daily to control symptoms. Dermatologic consultation is recommended. Therapy can be reinitiated after resolution of symptoms or improvement to grade 1 toxicity, and steroids have been tapered to less than 10 mg of prednisone daily.
Development of grade 4 (life-threatening) skin toxicity including SJS or TEN requires admission to the hospital for supportive care including intravenous corticosteroids, intravenous fluids, consideration of antibiotics, pain management, and a formal dermatology consultation. ICI should be discontinued permanently for rashes that show signs of blistering, dermal ulceration, necrosis, bullous, or hemorrhagic changes. Systemic corticosteroids initiated at 1–2 mg/kg/day prednisone or equivalent should be administered and tapered over at least 1 month.
Cessation of drug is not usually recommended for vitiligo . There are dermatologic treatments for vitiligo including immunosuppression, UV therapy, and depigmentation therapy; however, this toxicity is cosmetic in the setting of life-threatening malignancy. Vitiligo is permanent, and referral to dermatologist is warranted if depigmentation causes the patient significant emotional distress.
Lichenoid reactions do not require cessation of drug in general. Treatment including topical steroids such as triamcinolone can be used in symptomatic cases and have improved pruritus and rash. In a series of three patients treated with anti-PD-1 mAbs developing lichenoid reactions, two patients continued therapy without any intervention and rash remained mild [31].
Studies have shown that development of cutaneous irAEs, specifically vitiligo -like depigmentation, may be of positive prognostic value. In a meta-analysis of 27 studies, vitiligo development was significantly associated with both improved progression-free survival (p < 0.005) and overall survival (p < 0.003) [34]. Retrospective analyses showed that patients who developed any cutaneous irAEs, not limited to vitiligo , while treated with pembrolizumab for advanced melanoma or NSCLC had significantly longer progression-free intervals [36].
12.3.6 Time to Resolution
In phase III clinical trials, ipilimumab-mediated moderate rash was treated with systemic steroids for a median of 15 days. Patients with severe rash were treated with systemic steroids for a median of 21 days with a time to resolution ranging up to 3.6–4.3 months [39]. In nivolumab -mediated rash, median time to resolution in a pooled safety analysis was 29 weeks [25]. Most patients have resolution of rash, and only a minority of patients experienced rash upon reinitiating drug.
12.4 Gastrointestinal Toxicity
12.4.1 Clinical Presentation
Diarrhea and enterocolitis are well-described toxicities of ICI. Patients will report loose, watery stools several times daily, depending on severity. Frequency of diarrhea should be assessed carefully. Stool containing blood or mucous is concerning for colitis. Physicians should inquire about the presence of abdominal pain, fever, nausea, or vomiting, as these symptoms are concerning for colitis, impending ileus/obstruction, or perforation. Physical exam should be performed specifically looking for abdominal tenderness or peritoneal signs. In the case of severe abdominal pain, stat imaging should be obtained to rule out ileus, colitis, or abdominal perforation.
The most common computed tomography (CT) findings of ipilimumab-mediated colitis are mesenteric vessel engorgement and bowel wall thickening, followed by fluid-filled colonic distention in either diffuse or segmental patterns [42]. Gastrointestinal consultation is recommended in the case of prolonged grade 2 or grade 3/4 diarrhea or colitis in order to obtain flexible sigmoidoscopy or colonoscopy, which can aid in the diagnosis of immune-mediated colitis. On endoscopy in patients with immune-mediated enterocolitis, gross ulceration or erythema is typically observed, and three histologic patterns have been described: neutrophilic inflammation only (46%), lymphocytic inflammation only (15%), or combined neutrophilic and lymphocytic inflammation (38%) [43].
12.4.2 Grading
Diarrhea:
-
Grade 1: Increase of <4 stools per day over baseline; mild increase in ostomy output compared to baseline
-
Grade 2: Increase of 4–6 stools per day over baseline; moderate increase in ostomy output compared to baseline
-
Grade 3: Increase of >7 stools per day over baseline; incontinence; hospitalization indicated; severe increase in ostomy output compared to baseline; limiting self-care ADL
-
Grade 4: Life-threatening consequences; urgent intervention indicated
-
Grade 5: Death
Enterocolitis:
-
Grade 1: Asymptomatic; clinical or diagnostic observations only; intervention not indicated
-
Grade 2: Abdominal pain; mucus or blood in stool
-
Grade 3: Severe or persistent abdominal pain; fever; ileus, peritoneal signs
-
Grade 4: Life-threatening consequences; urgent intervention indicated
-
Grade 5: Death
12.4.3 Incidence
Diarrhea and enterocolitis are common gastrointestinal (GI) irAEs associated with ICI with a higher incidence in patients treated with anti-CTLA-4 mAbs, compared to PD-1 /PDL-1inhibition. Approximately 1/3 of patients treated with CTLA-4 checkpoint blockade will develop diarrhea and/or colitis of any grade, and up to 11% will develop severe grade 3 or 4 toxicity [4]. In contrast, approximately 8–19% of patients treated with anti-PD-1 mAbs developed diarrhea and/or colitis of any grade with severe GI toxicity occurring in only 1% [6, 14, 24, 26]. Concurrent use of anti-CTLA-4 and anti-PD-1 mAbs leads to GI toxicity in up to 44% of patients with severe GI toxicity in 9.3% of patients [26].
12.4.4 Time to Presentation
Across several clinical trials, ipilimumab-mediated enterocolitis presents at a median of 6.3 weeks for grade 2 enterocolitis and 7.4 weeks for grade 3–5 enterocolitis [39]. When nivolumab is given as a single agent, median time to onset of immune-mediated colitis is 2.7–5.6 months, developing as early as 2 days and as late as 15 months [44]. The median time to onset of colitis with concurrent ipilimumab and nivolumab is shorter at 1.6 months [44]. The median time to onset of colitis is 3.4 months for pembrolizumab [45].
12.4.5 Management
Patients must be educated to report loose stools, diarrhea, and/or abdominal pain immediately to their physician and to track frequency. Thorough history and physical should be performed. Other possible causes of diarrhea should be assessed including viral gastroenteritis, medication-induced diarrhea, or infectious diarrhea. It is possible for patients to have a superimposed infection, such as clostridium difficile, with ICI-induced diarrhea/colitis. In patients who receive ICI, there should be a high index of suspicion for immune-related diarrhea and/or colitis. While small series have investigated the role of specific genomic variants that may predispose patients to the development of colitis, currently there is no test in clinical use [46], and there are no recommended preventative measures. In a phase II randomized study, prophylactic oral budesonide failed to prevent the onset of gastrointestinal irAEs in patients treated with ipilimumab compared with placebo [46].
Rapid treatment of ICI-mediated colitis is imperative. Delay of 3 weeks from the onset of symptoms to the initiation of steroid treatment has been linked to at least two colitis deaths [40, 47]. Initiation of steroid treatment within 5 days of the onset of ICI-mediated enterocolitis led to faster resolution of symptoms than when steroid was delayed >5 days [48].
Algorithms for the management of ICI-mediated diarrhea have been developed, and their use is recommended [35, 40]. Initial management for grade 1 diarrhea is symptomatic with encouragement of oral hydration, antidiarrheal medications such as loperamide, and electrolyte repletion. Patients should be monitored with vigilance for worsening diarrhea or development of colitis.
Grade 2 diarrhea is managed symptomatically initially with supportive care. ICI should be withheld. If diarrhea persists for greater than 3–5 days, prednisone or equivalent at 0.5–1 mg/kg/day should be administered. Oral diphenoxylate hydrochloride, atropine sulfate four times per day, and budesonide 9 mg once per day have been used by experienced practitioners to treat grade 2 diarrhea [40]. Referral to gastroenterologist for sigmoidoscopy or colonoscopy to diagnose colitis is indicated for persistent grade 2 diarrhea, grade 3–4 diarrhea, or rectal bleeding. The presence of any colitis mandates a course of systemic steroids. Treatment can be resumed upon resolution of symptoms after steroids have been tapered for at least 1 month.
Grade 3–4 diarrhea or colitis requires discontinuation of ICI. Admission to the hospital should be considered for intravenous steroids, intravenous fluids, electrolytes, and careful monitoring. Prednisone or its equivalent of 1–2 mg/kg/day should be administered as soon as possible. Upon improvement to grade 1 or less, initiate corticosteroid tapers over at least 4 weeks to ensure complete resolution of symptoms. Resumption of ICI can be considered in grade 3 diarrhea or colitis when symptoms are grade 1 and steroids have been tapered for at least 1 month. Permanent cessation of ICI is recommended for grade 4 colitis, hemorrhage, or perforation.
For patients with refractory symptoms despite treatment with high-dose steroids for approximately 5 days, a single dose of infliximab 5 mg/kg has demonstrated rapid resolution of symptoms and durable efficacy [43, 49]. Infliximab may also be considered for persistent grade 2 symptoms that do not resolve despite treatment with steroids or with recurrence of symptoms and difficulty tapering off of steroids. Consider a surgical consult for patients with severe diarrhea/colitis or ileus early in the treatment course. Colitis can progress to intestinal perforation which can be fatal.
12.4.6 Time to Resolution
In patients with metastatic melanoma who developed grade 3–5 ipilimumab-mediated enterocolitis in a phase III trial, median duration of treatment with high-dose steroids was 16 days (ranging up to 3.2 months) followed by corticosteroid taper [39]. The median duration of pembrolizumab -mediated colitis is 1.4 months (range, 1 day to 7.2 months) [45]. Nivolumab -mediated colitis led to treatment with high-dose steroids for a median duration of 3 weeks to 4.2 months in various clinical trials followed by steroid taper [44].
12.5 Hepatotoxicity
12.5.1 Clinical Presentation
Hepatotoxicity is a less common but serious irAE characterized by immune-mediated hepatitis. In general, routine laboratory assessment will find elevations in serum levels of hepatic enzymes aspartate aminotransferase (AST) and alanine aminotransferase (ALT) and/or bilirubin. Most episodes are asymptomatic though associated fever, right upper quadrant pain, and malaise have been described. Concomitant elevations in total bilirubin can occur usually with prolonged transaminitis due to inflammation and cholestasis. Hyperbilirubinemia can cause jaundice, scleral icterus, and tea-colored urine.
12.5.2 Grading
-
Grade 1: AST and/or ALT >3.0 times the upper limit of normal, bilirubin >1.5 times the upper limit of normal
-
Grade 2: AST and/or ALT >3.0–5.0 times the upper limit of normal, bilirubin >1.5–3.0 times the upper limit of normal
-
Grade 3: AST and/or ALT >5.0–20.0 times the upper limit of normal, bilirubin >3.0–10.0 times the upper limit of normal
-
Grade 4: AST and/or ALT >20.0 times the upper limit or normal, bilirubin >10 times the upper limit of normal
-
Grade 5: Death
12.5.3 Time to Presentation
The median time to onset of grade 3–4 immune-mediated hepatitis was 2.0 months in patients receiving adjuvant ipilimumab for locally advanced melanoma. Lower grade 2 hepatitis occurred earlier at 1.4 months [39]. In patients treated with pembrolizumab , the median time to hepatitis onset is 26 days (range, 8 days to 21.4 months) [45]. In patients treated with nivolumab , the median time to hepatitis onset is 3.7 months (range, 6 days to 9 months) [44].
12.5.4 Incidence
A large meta-analysis revealed the incidence of all-grade and high-grade hepatotoxicity among patients treated with CTLA-4 inhibitors is 5% and 2%, respectively [4].
The combination of CTLA-4 and PD-1 blockade increases the risk of liver toxicity. For example, in melanoma patients treated with combined nivolumab plus ipilimumab, the rates of all-grade and high-grade transaminitis were 15.3% and 6.1%, respectively [26].
Compared to treatment with anti-CTLA-4 monotherapy and combined CTLA-4 and PD-1 checkpoint blockade, treatment with PD-1 inhibition results in the least hepatotoxicity. In a large phase III clinical trial of NSCLC patients, the use of pembrolizumab resulted in elevated liver enzymes in 3.0% and severe hepatotoxicity in 0.6% of patients [6]. In a pooled analysis of four clinical trials utilizing nivolumab in advanced melanoma, liver toxicity of all grades was reported in 4% of patients [25].
12.5.5 Management
Current guidelines recommend evaluation of hepatic enzymes (AST, ALT, alkaline phosphatase, bilirubin) at baseline, prior to each dose, and periodically after completion of therapy. Patients should be counseled to minimize intake of other hepatotoxic medications such as alcohol or excessive acetaminophen. It is reasonable to check baseline viral hepatitis serologies prior to administration of ICI, particularly in patients with identified risk factors. Most clinical trials excluded patients with active hepatitis B or C though use of ICI in a small series of patients with active hepatitis B or C has yielded similar hepatotoxicity to the general population [50].
Management algorithms have been developed and are recommended [35, 39, 40]. For grade 1 hepatotoxicity, ICI can be continued. Monitoring should increase with laboratory drawings at least twice weekly. Work-up for autoimmunity should be considered, including serum antinuclear antibody, smooth muscle antibody, anti-mitochondrial antibodies, anti-liver–kidney microsomal-1 antibodies, and others as appropriate. Viral hepatitis panels should be performed if not already completed. Liver imaging should be performed to rule out obstruction or disease progression as possible confounding diagnoses. Alcohol consumption should be quantified and intake should be stopped.
For grade 2 hepatotoxicity, ICI should be held. Liver enzymes should be tested at least every 3 days. A dose of 0.5 to 1 mg/kg/day prednisone equivalents should be administered. ICI can be resumed upon resolution to grade 1 toxicity once steroids have been tapered for at least 1 month. Autoimmune work-up as above is recommended.
For grade 3 or 4 hepatotoxicity, ICI should be held. Administer corticosteroids at a dose of 1–2 mg/kg/day prednisone equivalents. Admission to the hospital for 24–48 h of IV steroids should be considered. Liver enzymes should be checked daily until improvement is ensured. It is recommended in grade 3 or 4 hepatotoxicity that ICI is held indefinitely. Steroids should be tapered over at least 1 month. If liver enzyme elevations persist, worsen, or rebound for greater than 3–5 days, non-corticosteroid immunosuppressive medications such as oral mycophenolate mofetil should be administered [40]. Infliximab should be avoided due to its potential for hepatotoxicity. Anti-thymocyte globulin (ATG) has been used in a severe steroid and mycophenolate mofetil refractory case of autoimmune hepatitis [51].
12.5.6 Time to Resolution
With ipilimumab treatment for melanoma, patients were treated for grade 3–4 hepatitis with systemic corticosteroids for a median of 4.4 months (ranging up to 56.1 months). Patients with moderate hepatitis were treated with systemic corticosteroids for a median duration of 2.6 months (ranging up to 41.4 months) [39]. In patients treated with nivolumab , hepatotoxicity treated with high-dose corticosteroids led to resolution in a median of 3–4 weeks (range, 5 days to 2 months) [25, 44].
12.6 Pneumonitis
12.6.1 Clinical Presentation
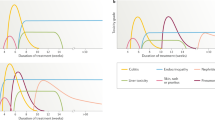
Although rare, pneumonitis is a feared complication of ICI. It should be suspected when a patient on an immune checkpoint inhibitor develops a nonproductive cough, progressive shortness of breath, fine crackles on examination, and hypoxia. CT imaging of pneumonitis shows a spectrum of findings typically seen in interstitial pneumonias including diffuse ground-glass opacities and reticular opacities in the peripheral and lower lungs [52]. The primary differential diagnoses include infection, progression of disease, and pulmonary edema (Fig. 12.4).
12.6.2 Grading
-
Grade 1: Asymptomatic; clinical or diagnostic observations only; intervention not indicated
-
Grade 2: Symptomatic; medical intervention indicated; limiting instrumental ADL
-
Grade 3: Severe symptoms; limiting self-care ADL; oxygen indicated
-
Grade 4: Life-threatening respiratory compromise; urgent intervention indicated (e.g., tracheostomy or intubation)
-
Grade 5: Death
12.6.3 Incidence
In randomized phase II and phase III trials, the incidence of all-grade pneumonitis in patients treated with ipilimumab ranged from 0.4% to 1.6%. High-grade pneumonitis occurred in 0.3–0.4% of patients that received ipilimumab [5, 53, 54]. These numbers do not include data from a relatively small randomized phase III study by Postow et al., in which 142 patients with advanced melanoma were randomized 2:1 to ipilimumab combined with nivolumab vs. ipilimumab combined with placebo. In this trial, the rates of all-grade and high-grade pneumonitis in the ipilimumab monotherapy arm (4% all grade, 2% high grade) were about four times as high as the incidence of pneumonitis observed with ipilimumab in other trials [55].
Randomized phase II and phase III studies of nivolumab have demonstrated incidence of all-grade pneumonitis between 1.3% and 5% and high-grade pneumonitis between 0% and 1% in treated patients [12,13,14, 24, 56]. Phase II and III trials of pembrolizumab show similar rates of all-grade (0.4–5%) and high-grade (0–2%) pneumonitis [5, 7].
Combining ipilimumab with nivolumab increases toxicity. In two-phase III trials, all-grade and high-grade pneumonitis occurred in 6.4–11% and 1–2%, respectively, of patients treated with both ipilimumab and nivolumab . There was also one death due to drug-related pneumonitis in the combination arm [54, 55]. A meta-analysis of randomized phase II and III studies of ipilimumab, nivolumab , and pembrolizumab in patients with solid tumors revealed that compared to treatment with ipilimumab alone, combining ipilimumab with nivolumab increases the incidence of all-grade pneumonitis but is not associated with increased risk of high-grade pneumonitis (OR of all-grade pneumonitis with nivolumab /ipilimumab vs. ipilimumab monotherapy is 3.68 [95% CI 1.59–8.50, p = 0.002]). OR for high-grade pneumonitis is 1.86 [95% CI 0.36–9.53, p = 0.46] [57].
The same meta-analysis demonstrated no difference in the risk of either all-grade or high-grade pneumonitis between PD-1 inhibitors and ipilimumab (OR for all-grade pneumonitis 1.26, 95% CI 0.44–3.63, p = 0.66. OR for high-grade pneumonitis 0.71, 95% CI 0.10–5.08, p = 0.74). Similarly, there was no difference in risk of pneumonitis according to type of cancer treated (NSCLC vs. other cancer) (OR for all-grade pneumonitis 3.96, 95% CI 2.02–7.79, p < 0001. OR for high-grade pneumonitis 2.87, 95% CI 0.90–9.20, p = 0.08) [57].
12.6.4 Timing of Onset
Only two of the phase II and III trials of ipilimumab, nivolumab , and pembrolizumab describe the timing of onset of pneumonitis. Both of these studies were phase III randomized trials investigating nivolumab in patients with advanced NSCLC. In one of these trials, the median time to onset of treatment-related pneumonitis was 15.1 weeks (ranged, 2.6–85.1 weeks) [13]. In the second study, median time to onset was 31.1 weeks (range, 11.7–56.9 weeks) [12]. Based on these data, pneumonitis usually occurs within the first 3–6 months of treatment with a checkpoint inhibitor but can occur at any time.
12.6.5 Management
There are no formal guidelines for the management of ICI-mediated pneumonitis. ICI should be held in all cases of suspected pneumonitis. Bronchoscopy with bronchoalveolar lavage and transbronchial biopsy of a lymph node can be useful to rule out infection or progression of metastatic disease as alternative diagnoses. Empiric antibiotics should also be considered. For grade ≥2 pneumonitis, steroids (e.g., prednisone 1–2 mg/kg/day PO or methylprednisolone 1–2 mg/kg/day IV) are the mainstay of treatment. If symptoms improve on steroids, a gradual taper over several weeks is recommended. If there is no improvement after 48–72 h on steroids, additional immunosuppressive therapy, such as infliximab, should be considered [55, 58].
12.6.6 Time to Resolution
In phase II and III clinical trials, pneumonitis resolved with treatment in 66.7–100% of cases. Median time to resolution varied from 3.2 to 6.1 weeks [12, 13, 54, 55].
12.7 Endocrine Toxicity
12.7.1 Thyroid Dysfunction
12.7.1.1 Clinical Presentation
ICI can cause a number of different thyroid disorders including primary hypothyroidism due to destructive thyroiditis (high TSH, low free T4), secondary hypothyroidism as a result of hypophysitis (low TSH, low free T4), acute thyroiditis with transient hyperthyroidism (low TSH, high free T4) followed by hypothyroidism (high TSH, low free T4), and hyperthyroidism associated with Graves’ disease (low TSH, high free T4). Symptoms are non-specific and may include fatigue, weight change, temperature intolerance, constipation, diarrhea, bradycardia, and/and tachycardia, depending on the direction and degree of thyroid hormone imbalance [58,59,60].
Because hypo- and hyperthyroidism are relatively common side effects of immune checkpoint blockade and are associated with non-specific symptoms, TSH and free T4 should be monitored at baseline, periodically throughout treatment and more frequently if clinically indicated.
12.7.1.2 Grading
-
Grade 1: Asymptomatic; clinical or diagnostic observations only; intervention not indicated
-
Grade 2: Symptomatic; thyroid replacement (hypothyroidism) or suppression therapy (hyperthyroidism) indicated; limiting instrumental ADL
-
Grade 3: Severe symptoms; limiting self-care ADL; hospitalization indicated
-
Grade 4: Life-threatening consequences; urgent intervention indicated
-
Grade 5: Death
12.7.1.3 Incidence
Thyroid dysfunction is more common with PD-1 blockade than CTLA-4 inhibition, and hypothyroidism occurs more often than hyperthyroidism. In phase II and III trials, all-grade hypothyroidism was reported in 4–8.6% of patients treated with nivolumab [12, 13, 24, 54], 7–10% of patients who received pembrolizumab [5,6,7, 61], and 1.5–4.2% of patients on ipilimumab [2, 5, 54]. In those same trials, all-grade hyperthyroidism developed in 3.4–4.2% of nivolumab patients [24, 54], 4–6.5% of patients treated with pembrolizumab [5, 7, 61], and 1–2.3% of patients that received ipilimumab [5, 54]. Although fairly common, both hypo- and hyperthyroidism are usually mild, and rates of high-grade (grade 3–4) thyroid dysfunction are low (0–0.4%) [5,6,7, 12, 13, 24, 54, 57, 61]. The combination of nivolumab and ipilimumab increases the rates of all-grade hypothyroidism (15–16%) and hyperthyroidism (4.3–9.9%) but does not appear to increase the risk of high-grade thyroid disorders (0–1%) [54, 62].
12.7.1.4 Timing of Onset
The onset of ICI-mediated thyroid dysfunction varies from within 4 weeks of initiation of therapy to 3 years. In general, acute thyroiditis and hyperthyroidism occur early in treatment (median time of onset 4–6 weeks), and hypothyroidism occurs a little later (median time of onset 12 weeks) [63, 64].
12.7.1.5 Management
As noted above, thyroid dysfunction is usually mild and rarely an indication for interrupting or discontinuing ICI. Hypothyroidism should be managed with levothyroxine thyroid hormone replacement, initiated at a dose of 1–1.5 mcg/kg and titrated to TSH levels of 1–2 mU/l. Hyperthyroidism may resolve spontaneously, but patients should be monitored carefully for the development of subsequent hypothyroidism. If the patient is symptomatic, a steroid burst could be considered for acute thyroiditis . A nonselective beta-blocker, such as propranolol, could also be started for tachycardia. If hyperthyroidism persists, endocrinology should be consulted for management guidance and recommendations regarding role for thyroid suppression therapy, such as methimazole [58,59,60].
12.7.1.6 Time to Resolution
When it occurs as a side effect of ICI, hypothyroidism is usually permanent. By contrast, hyperthyroidism resolves in most patients. The time to resolution of immune-related thyroid dysfunction has not been well studied, but a pooled analysis of endocrine side effects in several pivotal PD-1 trials demonstrated a median time to resolution of 20.6 weeks (range 0.4–47.6; n = 6) [63].
12.7.2 Hypophysitis
12.7.2.1 Clinical Presentation
Hypophysitis , or inflammation of the pituitary gland, can present with a range of symptoms related to both mass effect and hormonal deficiencies resulting from anterior hypopituitarism. The most common initial symptoms are new-onset headache, fatigue, and asthenia. Other symptoms may include anorexia, nausea, vomiting, diarrhea, constipation, temperature intolerance, decreased libido, erectile dysfunction, confusion, and mental status changes [65, 66]. Based on several series, hypocortisolism (60–100% of cases), hypothyroidism (60–100% of cases), and hypogonadism (71–87% of cases) are usually present. Prolactin and growth hormone levels are usually normal but have been reported to be abnormally high or low in up to 25% of patients [4, 67,68,69,70]. Visual disturbances due to pituitary swelling are rare [67]. A few cases of diabetes insipidus have been reported [65, 70]. Brain MRI is important to rule out sellar metastatic disease as a cause of the patient’s presentation. Classic MRI findings include symmetric enlargement and homogeneous enhancement of the pituitary gland, but a normal MRI does not rule out hypophysitis [67]. Interestingly, there appears to be a male predominance of checkpoint inhibitor-associated hypophysitis (~6:1, male/female). However, the true male/ female distribution is unknown because the sex of patients with hypophysitis is not reported in several studies. Furthermore, this apparent finding may be partially explained by the higher incidence of metastatic melanoma in men [71].
12.7.2.2 Grading
Hypophysitis is not an adverse event specifically defined by CTCAE version 4. However, the toxicity grading structure for “endocrine disorders—other” has been applied to hypophysitis and is listed below.
-
Grade 1: Asymptomatic or mild symptoms; clinical or diagnostic observations only; intervention not indicated
-
Grade 2: Moderate; minimal, local, or noninvasive intervention indicated; limiting age-appropriate instrumental ADL
-
Grade 3: Severe or medically significant but not immediately life-threatening; hospitalization or prolongation of existing hospitalization indicated; disabling; limiting self-care ADL
-
Grade 4: Life-threatening consequences; urgent intervention indicated
-
Grade 5: Death
12.7.2.3 Incidence
Hypophysitis is a relatively uncommon complication of ICI that is most often associated with CTLA-4 inhibition and rarely occurs with PD-1 blockade. For example, in randomized phase II and III trials, all-grade hypophysitis was reported in 1.5–3.9% of patients receiving ipilimumab [2, 5, 54], compared to 0.6% of patients on nivolumab [54] and <1–0.7% of patients treated with pembrolizumab [5, 7, 61]. Rates of high-grade hypophysitis in these trials were lower but had a similar distribution (ipilimumab 1.5–1.9% vs. nivolumab 0.3% vs. pembrolizumab <1%) [2, 5, 7, 54, 61]. The combination of ipilimumab and nivolumab increases the risk of hypophysitis (all grade 7.7–12%, high grade 1.6–2%) [54, 62].
12.7.2.4 Timing of Onset
The median time of onset of hypophysitis is 9–16 weeks following initiation of checkpoint blockade, but cases have been reported as early as 4 weeks and as late as 19 months after starting treatment [40, 64, 65, 67, 70, 72].
12.7.2.5 Management
High index of suspicion is needed for diagnosis of all endocrine irAEs. The diagnosis of hypophysitis is established by low levels of all or several of the hormones produced by the anterior pituitary including thyroid-stimulating hormone (TSH), free T4, adrenocorticotropic hormone (ACTH), morning cortisol, follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol in females, testosterone in males, growth hormone (GH), IGF-1, and prolactin. Brain MRI is recommended to evaluate for enlargement and enhancement of the pituitary and rule out sellar metastatic disease. Brain MRI may be normal in the presence of hypopituitarism.
There are no formal guidelines for the management of ICI-mediated hypophysitis . Treatment primarily involves high-dose steroids, replacement of the affected pituitary hormones, and consideration of ICI discontinuation. Multidisciplinary management, in conjunction with an endocrinologist, is critical. Once symptoms are managed and the patient is on stable doses of steroids, ICI can often be resumed.
For grade 1 hypophysitis , some authors have recommended continuation of ICI with close observation for 1 week and initiation of high-dose corticosteroids (e.g., prednisone or solumedrol 1 mg/kg/day) if symptoms persist after that time [73].
For grade ≥2 hypophysitis , conventional recommendations have been to hold ICI until all adverse events resolve to grade 1 or less, initiate high-dose corticosteroids, and replace deficient pituitary hormones. However, both the recommendation to discontinue ICI and the role for high-dose steroids have been questioned recently, following one cohort study in which most patients continued ICI with concurrent hormone replacement [72] and two cohort studies that suggested steroids did not improve pituitary function recovery [70, 72]. If high-dose steroids are used, they should be tapered gradually to physiologic replacement doses of hydrocortisone (see below) [74, 75].
Finally, replacement of the affected hormones should be done under the guidance of an endocrinologist. In general, hydrocortisone (20 mg morning, 10 mg evening) is typically used to treat secondary adrenal insufficiency resulting from hypopituitarism. In contrast to primary adrenal insufficiency, mineralocorticoid replacement is usually not necessary. Hypothyroidism is treated with levothyroxine. Importantly, levothyroxine should not be administered until adrenal insufficiency has been treated because treatment of hypothyroidism alone in a patient with coexisting hypothyroidism and adrenal insufficiency can increase the severity of the cortisol deficiency. Treatment of LH and FSH deficiency depends on gender and fertility goals [58, 76, 77].
12.7.2.6 Time to Resolution
Adrenal insufficiency associated with ICI-mediated hypophysitis is usually permanent, and most patients require lifelong glucocorticoid replacement. To date, only a handful of cases of corticotroph recovery have been reported [74, 78]. By contrast, recovery of thyroid function occurs in 37–50% of patients [40, 67, 70], and gonadal function returns in 57% of men [67, 79]. The median time to resolution of hypothyroidism and hypogonadism was 13 and 10 weeks, respectively, in one study [70]. The time to resolution of MRI findings varies and has been reported as early as 2 weeks and as late as 27 weeks [70, 74].
12.8 Hematologic Toxicity
12.8.1 Clinical Presentation
Rare immune-related hematologic toxicities have been reported with CTLA-4 inhibition including thrombocytopenia, neutropenia, acquired hemophilia A, and red cell aplasia. Minor decreases and fluctuations in cell counts are common in patients with advanced cancer. However, these immune-related phenomena are profound and persistent without treatment.
Pure red cell aplasia presented in the setting of ipilimumab with an isolated anemia and low reticulocyte count in the absence of bleeding or hemolysis. Other cell lines including platelets and white blood cells were grossly normal. Peripheral blood film revealed normochromic and normocytic red blood cells with marked anemia. Bone marrow biopsy showed marked erythroid hypoplasia, granulocytic hyperplasia, and adequate maturing megakaryocytes without myelodysplasia, malignancy, or parvovirus [80].
Severe neutropenia during treatment with ICI has been described in a case report. Bone marrow aspiration and biopsy revealed marked myeloid hypoplasia with unremarkable erythropoiesis and megakaryopoiesis [81].
Acquired hemophilia caused by the presence of an acquired factor VIII inhibitor has been seen in a patient treated with CTLA-4 inhibition. The clinical presentation started with hematuria and isolated prolongation of activated partial thromboplastin time. Factor VIII inhibitor was confirmed with a factor VIII level <1% and inhibitor titer of 26 Bethesda units [82].
Grade 4 immune-mediated thrombocytopenia has also been described with ipilimumab. Bone marrow biopsy revealed increased megakaryocytes supporting a diagnosis of drug-induced immune-mediated thrombocytopenia [83].
12.8.2 Grading
-
Grade 1: Hgb <LLN–10.0 g/dL; <LLN–75,000/mm3; <LLN–1500/mm3
-
Grade 2: Hgb <10.0–8.0 g/dL; <75,000–50,000/mm3; <1500–1000/mm3
-
Grade 3: Hgb <8.0 g/dL; <50,000–25,000/mm3; <1000–500/mm3
-
Grade 4: Life-threatening consequences; urgent intervention indicated; <25,000/mm3; <500/mm
-
Grade 5: Death
12.8.3 Incidence
Grade 1 or 2 anemia has been reported in up to 4.2% of patients with ICI [6]. It is not clear if this is due to the effects of ICI or variable other causes of anemia. Grade 3 or 4 anemia is rarely reported. Anemia and neutropenia are much more common with the use of cytotoxic chemotherapy. For example, a large phase III clinical trial in patients with advanced non-squamous NSCLC showed an incidence of all-grade anemia in 2% versus 20% of patients with nivolumab and docetaxel, respectively [12]. All-grade neutropenia in the same trial showed an incidence of <1% versus 31% in nivolumab and docetaxel groups [12].
Grade 3 or 4 immune-mediated hematologic toxicity is rare and occurs in far less than 1% of patients treated with anti-PD-1 or anti-CTLA-4 mAbs.
12.8.4 Time to Presentation
Hematologic presentations are rare and a specific time to presentation has not been reported.
12.8.5 Management
Complete blood count (CBC) assessment is recommended prior to initiation of ICI and prior to each dose. Any abnormality should prompt closer interval evaluation. As previously mentioned, minor fluctuations in cell lines, particularly anemia, are common in advanced cancer. Grade 1–2 anemia is commonly reported in clinical trials and does not require treatment or cessation of ICI. Routine investigation of all hematologic toxicity for alternate etiologies is initially recommended.
Immune-related anemia, thrombocytopenia, and neutropenia are usually profound (grade 3 or 4). Isolated anemia should be evaluated comprehensively ruling out other etiologies such as hemorrhage, hemolysis, vitamin or iron deficiencies, and thyroid disorders. Peripheral blood film is useful initially. Supportive care and blood transfusion as needed are recommended. If underlying cause cannot be found, bone marrow biopsy is useful to rule out bone marrow involvement from malignancy, myelodysplastic syndrome especially in patients exposed to prior chemotherapy or radiation, or pure red cell aplasia.
If immune-related etiology of anemia is suspected, prednisone 1–2 mg/kg/day or equivalent can be administered. ICI should be withheld for grade 3 or 4 hematologic toxicity. If no improvement is seen within several days, intravenous immunoglobulin (IVIG) led to rapid reticulocytosis and normalization of hemoglobin in pure red cell aplasia caused by ipilimumab refractory to steroids.
Leukopenia, thrombocytopenia, and neutropenia found on routine CBC should be evaluated for other causes including medications, infection, disseminated intravascular coagulation, etc. Bone marrow biopsy should be considered. Patients should be instructed to monitor their temperature and seek immediate medical care for fever in the setting of neutropenia. If immune-mediated etiology is suspected, prednisone 1–2 mg/kg/day or equivalent should be administered for grade 3 or 4 hematologic toxicity. When neutropenia or thrombocytopenia does not respond to steroids, IVIG rapidly improved immune-related anemia, neutropenia, and thrombocytopenia in case reports [80, 81, 83].
12.8.6 Time to Resolution
Immune-related red cell aplasia and neutropenia improved rapidly upon administration of IVIG. Thrombocytopenia resolution began improving after 9 days of therapy.
12.9 Ocular Toxicity
12.9.1 Clinical Presentation
Ocular adverse events are rare but have been reported with ICI, especially ipilimumab. A variety of inflammatory conditions involving different ocular locations have been described in case reports and series of patients treated with ipilimumab including conjunctivitis, bilateral anterior uveitis , vitritis, papillitis, choroiditis, serous retinal detachment, peripheral ulcerative keratitis (PUK), inflammatory orbitopathy, choroidal neovascularization, neuroretinitis, orbital myositis, and bilateral optic neuropathy [84]. Bilateral anterior uveitis with neuroretinitis presented as unilateral metamorphopsias (distorted vision in which grid of straight lines appears wavy), scotoma, bilateral eye pain, redness, and photophobia [84]. Comprehensive ophthalmologic exam revealed anterior chamber inflammation and bilateral optic nerve edema. Bilateral uveitis alone presented with blurred vision, flashes, floaters, and headache [85]. Development of uveitis is often associated with ICI-related colitis. Inflammatory orbitopathy presented with tearing, diplopia, pain, conjunctival chemosis, and limitation in extraocular motility [85]. PUK presented with bilateral eye pain.
Ocular toxicity is rare with PD-1 inhibition but has been described in case reports describing uveitis [86, 87].
12.9.2 Grading
Eye disorders:
-
Grade 1: Asymptomatic or mild symptoms; clinical or diagnostic observations only; intervention not indicated
-
Grade 2: Moderate; minimal, local, or noninvasive intervention indicated; limiting safe-appropriate instrumental ADL
-
Grade 3: Severe or medically significant but not immediately sight-threatening; hospitalization indicated; disabling; limiting self-care ADL
-
Grade 4: Sight-threatening consequences; urgent intervention indicated; blindness (20/200 or worse) in the affected eye
12.9.3 Incidence
The incidence of ocular irAEs in ipilimumab phase II and III trials was 1.3%, with 0.4% being grade 3 or higher [88]. The incidence of ocular events in clinical trials using anti-PD-1 mAbs is not well described but is less than 1%.
12.9.4 Time to Presentation
The majority of patients developed ocular irAEs after second or third dose of ipilimumab [85].
12.9.5 Management
Treatment of ipilimumab-associated ocular irAEs depends on the severity and location of inflammation and presence of systemic complications. Topical corticosteroid drops are sufficient in mild cases of anterior uveitis , iritis, episcleritis, and PUK [84, 85]. Posterior uveitis or sight-threatening orbital inflammation warrants systemic corticosteroids [84, 85]. Prompt referral to an ophthalmologist should be made for any visual complaints. MRI brain should be considered to rule out central nervous system metastatic disease when symptoms such as diplopia, headache, or blurred vision occur. Thyroid and adrenal function tests should be performed in the case of orbital inflammation.
Ocular irAEs from ipilimumab usually resolve with corticosteroid treatment. Permanently discontinue ICI for immune-mediated ocular disease that is unresponsive to local immunosuppressive therapy [39].
12.9.6 Time to Resolution
Ocular irAEs usually resolve with topical or systemic corticosteroids. Uveitis and PUK resolved within 1–6 weeks [85]. Inflammatory orbitopathy took several months to resolve.
12.10 Rheumatologic Toxicity
12.10.1 Clinical Presentation
Joint and muscular pain is often described with ICI. Arthralgias are commonly reported with anti-PD-1 mAbs and can present as monoarticular or polyarticular joint pain. Polyarticular inflammatory arthritis has been described with pembrolizumab use. This can present as severe tenosynovitis, synovitis, and/or myositis [89]. Changes to the joint including redness, erythema, and swelling are concerning for inflammatory arthritis.
Myalgias are the second most commonly reported musculoskeletal toxicity. Myalgias present as muscular pain, which can be diffuse or localized. Rare cases of severe autoimmune inflammatory myopathy and necrotic myositis have been described with ipilimumab and pembrolizumab therapy [90, 91].
An array of other immune-related rheumatologic toxicities have been reported in less than 1% of patients treated with ICI including as polymyalgia rheumatic/giant cell arteritis, sarcoid-like reaction [92,93,94,95], and vasculitis (granulomatosis with polyangiitis) [96].
Polymyalgia rheumatica has occurred in several patients on ipilimumab therapy presenting as pain, stiffness, and/or weakness involving the proximal muscles of the neck, shoulders, upper arms, and hips [97]. Both cases were associated with giant cell arteritis (GCA) which is a vasculitis involving the large and medium arteries of the head. Inflammatory markers including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are usually elevated.
Sarcoidosis has presented in a variety of ways including cutaneous, pulmonary, and splenic lesions. Biopsy is needed to differentiate sarcoidosis from disease progression.
12.10.2 Grading
Arthralgia:
-
Grade 1: Mild pain
-
Grade 2: Moderate pain; limiting instrumental ADL
-
Grade 3: Severe pain; limiting self-care ADL
Myositis:
-
Grade 1: Mild pain
-
Grade 2: Moderate pain associated with weakness; pain limiting instrumental ADL
-
Grade 3: Pain associated with severe weakness; pain limiting self-care ADL
12.10.3 Incidence
In clinical trials using anti-PD-1 mAbs in patients with diverse malignancies, the incidence grade 1–2 arthralgia is 5–17% with high-grade arthralgia in less than 1% of patients [5, 6, 11, 13]. The incidence of low-grade and high-grade myalgias in these same trials was <1.0–15% and less than 1%.
The incidence of arthralgia with ipilimumab therapy in a clinical trial of patients with advanced melanoma was 5.1% and <1% for low grade and high grade, respectively [5].
Autoimmune inflammatory myositis, PMR/GCA, vasculitis, and sarcoidosis are rare events occurring in less than 1% of patients.
12.10.4 Time to Presentation
Time to presentation has not been reported.
12.10.5 Management
There are no specific management guidelines for rheumatologic adverse events. Grade 1–2 musculoskeletal AEs including myalgias and arthralgias can be treated initially with nonsteroidal anti-inflammatory drugs. Synovitis and tenosynovitis have been treated symptomatically with bisphosphonates and sulfasalazine [89]. If this is not sufficient, systemic prednisone starting at 0.5 mg/kg or equivalent can be administered. Tapering of steroids should begin after relief of symptoms is attained. Laboratory studies including ESR and CRP should be obtained and trended to assess the degree of inflammation and treatment response.
For arthralgia specifically, it is reasonable to obtain a rheumatoid factor, anti-citrullinated antibody, antinuclear antibody, uric acid to assess for development of specific rheumatologic syndromes including rheumatoid arthritis, systemic lupus erythematosus, and gout. Referral to a rheumatologist is highly recommended with the development of an autoimmune musculoskeletal disorder or polyarticular arthritis with joint changes.
In the case of myalgia or myositis, serum creatinine kinase should be assessed to rule out inflammatory myositis or rhabdomyolysis. The mainstay of treatment for myositis is glucocorticoid therapy initiated with prednisone at a dose of 1 mg/kg per day followed by a slow taper. Inflammatory myopathy can occur in the setting of thyroid and adrenal dysfunction; therefore, these serologic tests should be evaluated.
12.10.6 Time to Resolution
Time to resolution has not been specifically reported.
12.11 Neurologic Toxicity
12.11.1 Clinical Presentation
Neurological irAEs are a rare heterogeneous toxicity class of ICI. A variety of neurologic syndromes have been described with anti-CTLA-4 mAbs such as Guillain-Barre´ syndrome (GBS) [98], aseptic meningitis [99], posterior reversible encephalopathy syndrome (PRES) [100], myasthenia gravis (MG)-type syndrome [101], mono- or polyneuropathy [102], inflammatory enteric neuropathy [103], limbic encephalitis , chronic inflammatory demyelinating polyneuropathy (CIDP) [101], and transverse myelitis [101]. Encephalitis associated with Hashimoto’s thyroiditis has also been described [89]. Limbic encephalitis [72], myasthenia gravis [93], peripheral neuropathy, and GBS have occurred in patients receiving PD-1 inhibition.
GBS presented as numbness and tingling in the hands and feet that rapidly ascended to loss of sensory and motor function of the limbs impairing gait. Clinical neurological examination revealed a loss of the deep tendon reflexes. Electromyography (EMG) was a diagnostic for a generalized motor and sensory demyelinating polyneuropathy. Cerebrospinal fluid (CSF) analysis showed an elevated protein level and IgG with the presence of oligoclonal bands in CSF and serum [98].
PRES presented as acute bilateral blindness with headache and generalized tonic-clonic seizure in a hospitalized patient with acute renal failure. MRI brain showed multiple bilateral symmetric alterations in the cortical and subcortical areas in the parieto-occipital region, frontal and temporal lobes, and cerebellar hemispheres [100].
MG presented with concurrent myositis. Initial symptoms included dysphagia, odynophagia, bilateral ptosis, fatigability/weakness of the proximal muscles in the setting of elevated acetylcholine receptor-binding Ab, acetylcholine receptor-modulating Ab, and anti-striated muscle Ab [101].
Inflammatory enteric neuropathy presented as severe refractory constipation [103]. Colonoscopy with biopsies was performed revealing prominent inflammatory infiltrates of mononuclear lymphocytes associated with the myenteric nervous system.
CIDP presented as proximal muscle weakness and intermittent numbness and tingling in the face and upper and lower extremities bilaterally. Initially symptoms were intermittent but then became constant [101]. Transverse myelitis presented as bilateral lower extremity weakness and paresthesias with intermittent urinary retention and fecal incontinence [101].
12.11.2 Grading
Due to the wide variety of neurological events described, please see the Common Terminology Criteria for Adverse Events (CTCAE) for specific grading.
12.11.3 Incidence
In a large phase III clinical trial of patients receiving ipilimumab in the adjuvant setting for high-risk melanoma, neurologic events occurred in 2.3% of patients [3] . Grade 3–5 neurologic AEs occur in less than 1%.
Neurologic AEs occur in less than 1% of patients treated with anti-PD-1 mAbs. One case of fatal limbic encephalitis has occurred with nivolumab [72].
12.11.4 Time to Presentation
Median time to presentation of neurologic AE with ipilimumab therapy was 13.1 weeks (8.3–77.3 weeks) [3]. Time to presentation for PD-1 -mediated neurologic complications has not been described.
12.11.5 Management
Withhold ICI in patients with new-onset grade 3 or 4 neurologic signs or symptoms. Thorough history and physical should be performed to evaluate infectious or other causes of moderate-to-severe neurologic deterioration. Evaluation should include neurologic consultation and brain imaging including MRI as soon as possible. Lumbar puncture can be helpful in evaluating infectious diseases, leptomeningeal metastatic disease, paraneoplastic syndromes, and inflammatory etiologies.
If other etiologies are ruled out, administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents for patients with grade 3 or 4 neurologic toxicity, followed by prolonged corticosteroid taper over at least 4 weeks. Permanently discontinue ICI for immune-mediated encephalitis , severe or life-threatening neurologic events defined as grade 3 or 4. Plasma exchange or IVIG may be considered for severe immune-mediated neurologic syndromes including GBS, MS, or CIPD, though limited data exists regarding the management of steroid-refractory neurologic irAEs [101].
12.11.6 Time to Resolution
Median time to resolution of ipilimumab-mediated neurologic toxicity was 8 weeks [3].
12.12 Renal Toxicity
12.12.1 Clinical Presentation
Acute renal failure due to immune-related nephritis has occurred rarely with ICI [104,105,106]. Minor fluctuations in serum creatinine can occur commonly through the duration of therapy. Immune-mediated nephritis is defined as renal dysfunction or serum creatinine 2–3 times above baseline increased creatinine, requirement for corticosteroids, and no clear alternate etiology [72]. The most typical clinical presentation is acute impairment of renal function seen by elevation in serum creatinine found on routine evaluation with or without an abnormal urinalysis.
Nephritis has been linked to either membranous lupus nephritis or more commonly acute interstitial granulomatous nephritis [105, 106]. Lupus nephritis has been described in a case report presenting with elevated serum creatinine, elevated urine protein excretion by spot urine protein-to-creatinine ratio, microscopic hematuria, elevated antinuclear antibodies (ANA) and anti-double-stranded DNA antibodies (dsDNA), and low complement (C3 and C4) levels. Kidney biopsy revealed extra-membranous and mesangial deposits of IgG, IgM, C3, and C1q [106].
Several cases of acute granulomatous interstitial nephritis have been described characterized by elevation in serum creatinine. Kidney biopsy revealed severe interstitial inflammation with edema or acute interstitial nephritis with tubular necrosis and non-necrotizing epithelioid granulomas [105]. There is lack of nephrotic range proteinuria, antinuclear antibodies, anti-double-stranded DNA antibodies, or microscopic hematuria. Kidney failure was preceded or accompanied with a rash in half of the cases. In one instance of ipilimumab-related renal failure, CT scan of the abdomen and pelvis revealed bilateral swelling of the renal cortices [104].
12.12.2 Grading
Acute kidney injury:
-
Grade 1: Creatinine level increase of >0.3 mg/dL; creatinine 1.5–2.0 times above baseline
-
Grade 2: Creatinine level 2–3 times above baseline
-
Grade 3: Creatinine greater than 3 times baseline or greater than 4.0 mg/dL; hospitalization indicated
-
Grade 4: Life-threatening consequences; dialysis indicated
-
Grade 5: Death
12.12.3 Incidence
The incidence of immune-mediated nephritis and renal failure with single-agent anti-CTLA-4 and anti-PD-1 mAbs is less than 1%. Immune-mediated nephritis and renal dysfunction occurred in 2.2% of patients receiving combined nivolumab and ipilimumab [72].
12.12.4 Time to Presentation
The time for renal disease to appear varied from 6 to 12 weeks in patients treated with ipilimumab therapy [105]. The median time to onset of nivolumab immune-mediated nephritis and renal dysfunction was 15 weeks [25]. The median time to onset of pembrolizumab immune-mediated nephritis was 5.1 months (range, 12 days to 12.8 months) [45].
12.12.5 Management
Kidney function should be evaluated prior to initiation and prior to each dose of ICI. Detection of any decreased renal function by laboratory evaluation should prompt closer monitoring. Urinalysis for detection of proteinuria and microscopic hematuria should be performed. It is very important to rule out other causes of renal failure including volume depletion, nephrotoxic medications, and urinary obstruction from malignancy. Nephrology consult is recommended. Quantitative evaluation of urine protein excretion should be performed with spot protein/creatinine ratio. Serum ANA, compliment levels, and dsDNA are recommended if lupus nephritis is suspected. Renal biopsy should be highly considered to differentiate etiologies.
Moderate (grade 2) or severe (grade 3) increased serum creatinine should be treated with corticosteroids at a dose of 0.5 to 1 mg/kg/day prednisone equivalents followed by corticosteroid taper. ICI should be withheld. If worsening or no improvement occurs, increase dose of corticosteroids to 1 to 2 mg/kg/day prednisone equivalents and permanently discontinue ICI.
For life-threatening (grade 4) increased serum creatinine, patients should present to the emergency room or be directly admitted for electrolyte management, emergent nephrology consultation, and consideration of dialysis. Permanently discontinue ICI, and administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper for at least 4 weeks.
12.12.6 Time to Resolution
Acute granulomatous interstitial nephritis resolved in most cases within 2–4 weeks of steroid treatment [105]. In patients who developed immune-mediated nephritis treated with nivolumab , high-dose corticosteroids were given for a median duration of 16 days (range, 1 day to 9.9 months). Complete resolution (defined as improved to baseline with completion of corticosteroids) occurred in 50% of patients [72]. Immune-mediated nephritis has not been well described with pembrolizumab therapy.
12.13 Other Toxicities
IrAEs can occur in any organ system with rarity. Immune-related pancreatitis leading to pancreatic insufficiency and diabetes mellitus has been reported [59, 107]. In general, it is not recommended to obtain baseline or serial amylase and lipase levels unless the patient is symptomatic. Asymptomatic elevations in amylase and lipase occur and do not necessitate treatment or cessation of ICI. Myocarditis and cardiomyopathy from takotsubo-like syndrome have been reported [108, 109].
12.14 Immune-Related Adverse Events and Outcomes
An association between the occurrence of irAEs and favorable response to ICI has been described [34]. For example, in one study, development of irAEs was linked with increased probability of achieving an objective response, and higher-grade irAEs were associated with deeper and more durable responses [105]. Cutaneous irAEs in particular have been associated with improved outcomes. In a large meta-analysis of several melanoma immunotherapies, vitiligo was associated with improved overall survival, better progression-free survival, reduction in risk of disease progression, and reduction in risk of death [34]. A retrospective cohort study also showed a progression-free survival benefit among melanoma, lung cancer, prostate cancer, and Merkel cell carcinoma patients treated with pembrolizumab who developed cutaneous irAEs, compared to patients with no cutaneous toxicity [36]. Notably, the connection between irAE and response to ICI is not completely defined, as other retrospective series have not shown improved overall survival or time to treatment failure in patients treated with checkpoint inhibitors that develop irAE, compared to patients without immune toxicity [62]. It is important to emphasize that the use of glucocorticoids for treatment of irAEs does not seem to negatively impact outcomes and treatment should not be withheld for this purpose [62].
12.15 Supportive Management During Glucocorticoid Therapy
The management of many irAEs requires prolonged use of steroids leaving patients at risk for opportunistic infections including Pneumocystis jiroveci. Prophylactic dosing of TMP/SMX, atovaquone, or pentamidine should be considered in patients treated with 20 mg of prednisone equivalent daily for at least 4 weeks, based on the National Comprehensive Cancer Network guidelines for the Prevention and Treatment of Cancer-Related Infections (Category 2B recommendation). Glucose should also be monitored carefully while on glucocorticoid therapy for steroid mediated hyperglycemia.
12.16 Summary
Immune checkpoint inhibition (ICI) is a new paradigm of targeted cancer therapeutics leading to meaningful outcomes in many diverse malignancies. Inhibitors of cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and programmed cell death-1 (PD-1) have shown clinically significant antitumor responses leading to approval in advanced melanoma, non-small cell lung cancer, Hodgkin’s lymphoma, head and neck, urothelial carcinoma, and renal cell carcinoma, with promising activity in many other tumor types. Though ICI is often well tolerated, a unique array of toxicities termed immune-related adverse events (irAEs) has been identified, which have the potential to be severe or even life-threatening in some patients. IrAEs are T-cell mediated and autoimmune in nature, challenging the oncologist to recognize and treat a new toxicity profile. IrAEs are reported in every organ system but most commonly affect the skin, liver, gastrointestinal tract, and endocrine system. There is currently no way to predict or prevent irAEs. Prompt recognition and management with supportive measures and/or immunosuppression is pivotal, often resulting in reversibility. The use of immunosuppression to treat irAEs has not been found to negatively impact outcomes.
References
Postow MA, Callahan MK, Wolchok JD. Immune checkpoint blockade in cancer therapy. J Clin Oncol. 2015;33(17):1974–82.
Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Eggermont AM, et al. Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2015;16(5):522–30.
Bertrand A, et al. Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med. 2015;13:211.
Robert C, et al. Pembrolizumab versus Ipilimumab in advanced Melanoma. N Engl J Med. 2015;372(26):2521–32.
Garon EB, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372(21):2018–28.
Herbst RS, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2015;387(10027):1540–50.
Reck M, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–33.
Chen R, et al. Phase II study of the efficacy and safety of pembrolizumab for relapsed/refractory classic Hodgkin lymphoma. J Clin Oncol. 2017;35(19):2125–32.
Bellmunt J, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015–26.
Le DT, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372(26):2509–20.
Borghaei H, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–39.
Brahmer J, et al. Nivolumab versus Docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–35.
Motzer RJ, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373(19):1803–13.
Ansell SM, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N Engl J Med. 2015;372(4):311–9.
Sharma P, et al. Nivolumab in metastatic urothelial carcinoma after platinum therapy (CheckMate 275): a multicentre, single-arm, phase 2 trial. Lancet Oncol. 2017;18(3):312–22.
Rosenberg JE, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387(10031):1909–20.
Rittmeyer A, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389(10066):255–65.
Massard C, et al. Safety and efficacy of durvalumab (MEDI4736), an anti-programmed cell death Ligand-1 immune checkpoint inhibitor, in patients with advanced urothelial bladder cancer. J Clin Oncol. 2016;34(26):3119–25.
Gulley JL, et al. Avelumab for patients with previously treated metastatic or recurrent non-small-cell lung cancer (JAVELIN solid tumor): dose-expansion cohort of a multicentre, open-label, phase 1b trial. Lancet Oncol. 2017;18(5):599–610.
Hamanishi J, et al. Safety and antitumor activity of anti-PD-1 antibody, Nivolumab, in patients with platinum-resistant ovarian cancer. J Clin Oncol. 2015;33(34):4015–22.
Nghiem PT, et al. PD-1 blockade with pembrolizumab in advanced Merkel-cell carcinoma. N Engl J Med. 2016;374(26):2542–52.
Johnson DB, et al. Ipilimumab therapy in patients with advanced melanoma and preexisting autoimmune disorders. JAMA Oncol. 2016;2(2):234–40.
Robert C, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372(4):320–30.
Weber JS, Antonia SJ, Topalian SL, Schadendorf D, Larkin JMG, Sznol M, Liu H, Waxman I, Robert C. Safety profile of nivolumab (NIVO) in patients with advanced melanoma: a pooled analysis. J Clin Oncol. 2015;33(15 suppl):9018.
Larkin J, Hodi FS, Wolchok JD. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373(13):1270–1.
The National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) v4.0.; Available from: http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf.
Jaber SH, et al. Skin reactions in a subset of patients with stage IV melanoma treated with anti-cytotoxic T-lymphocyte antigen 4 monoclonal antibody as a single agent. Arch Dermatol. 2006;142(2):166–72.
Lacouture ME, et al. Ipilimumab in patients with cancer and the management of dermatologic adverse events. J Am Acad Dermatol. 2014;71(1):161–9.
Hwang SJ, et al. Bullous pemphigoid, an autoantibody-mediated disease, is a novel immune-related adverse event in patients treated with anti-programmed cell death 1 antibodies. Melanoma Res. 2016;26(4):413–6.
Joseph RW, et al. Lichenoid dermatitis in three patients with metastatic melanoma treated with anti-PD-1 therapy. Cancer Immunol Res. 2015;3(1):18–22.
Naidoo J, et al. Autoimmune bullous skin disorders with immune checkpoint inhibitors targeting PD-1 and PD-L1. Cancer Immunol Res. 2016;4(5):383–9.
Nayar N, Briscoe K, Fernandez Penas P. Toxic epidermal necrolysis-like reaction with severe satellite cell necrosis associated with nivolumab in a patient with ipilimumab refractory metastatic melanoma. J Immunother. 2016;39(3):149–52.
Teulings HE, et al. Vitiligo-like depigmentation in patients with stage III–IV melanoma receiving immunotherapy and its association with survival: a systematic review and meta-analysis. J Clin Oncol. 2015;33(7):773–81.
Fecher LA, et al. Ipilimumab and its toxicities: a multidisciplinary approach. Oncologist. 2013;18(6):733–43.
Sanlorenzo M, et al. Pembrolizumab cutaneous adverse events and their association with disease progression. JAMA Dermatol. 2015;151(11):1206–12.
Rizvi NA, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257–65.
Larkin J, et al. Efficacy and safety of nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433–40.
Yervoy® [Package insert]. 2013 [cited 2016 April]. Available from: http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=2265ef30-253e-11df-8a39-0800200c9a66.
Weber JS, Kahler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30(21):2691–7.
Naidoo J, et al. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol. 2015;26(12):2375–91.
Kim KW, et al. Ipilimumab-associated colitis: CT findings. AJR Am J Roentgenol. 2013;200(5):W468–74.
Beck KE, et al. Enterocolitis in patients with cancer after antibody blockade of cytotoxic T-lymphocyte-associated antigen 4. J Clin Oncol. 2006;24(15):2283–9.
Opdivo® [package insert]. 2015 [cited 2016 April]. Available from: http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f570b9c4-6846-4de2-abfa-4d0a4ae4e394.
Keytruda® [package insert]. 2015 [cited 2016 April]. Available from: http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=9333c79b-d487-4538-a9f0-71b91a02b287.
Weber J, et al. A randomized, double-blind, placebo-controlled, phase II study comparing the tolerability and efficacy of ipilimumab administered with or without prophylactic budesonide in patients with unresectable stage III or IV melanoma. Clin Cancer Res. 2009;15(17):5591–8.
Weber JS, et al. Patterns of onset and resolution of immune-related adverse events of special interest with ipilimumab: detailed safety analysis from a phase 3 trial in patients with advanced melanoma. Cancer. 2013;119(9):1675–82.
O’Day S, Weber JS, Wolchok JD, et al. Effectiveness of treatment guidance on diarrhea and colitis across ipilimumab studies. J Clin Oncol. 2011; 28:554–8554.
Johnston RL, et al. Cytotoxic T-lymphocyte-associated antigen 4 antibody-induced colitis and its management with infliximab. Dig Dis Sci. 2009;54(11):2538–40.
Ravi S, et al. Ipilimumab administration for advanced melanoma in patients with pre-existing hepatitis B or C infection: a multicenter, retrospective case series. J Immunother Cancer. 2014;2(1):33.
Chmiel KD, et al. Resolution of severe ipilimumab-induced hepatitis after antithymocyte globulin therapy. J Clin Oncol. 2011;29(9):e237–40.
Nishino M, et al. Anti-PD-1-related pneumonitis during cancer immunotherapy. N Engl J Med. 2015;373(3):288–90.
Kwon ED, et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2014;15(7):700–12.
Larkin J, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373(1):23–34.
Postow MA, et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 2015;372(21):2006–17.
Weber JS, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375–84.
Abdel-Rahman O, Fouad M. Risk of pneumonitis in cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Ther Adv Respir Dis. 2016;10(3):183–93.
Spain L, Diem S, Larkin J. Management of toxicities of immune checkpoint inhibitors. Cancer Treat Rev. 2016;44:51–60.
Hofmann L, et al. Cutaneous, gastrointestinal, hepatic, endocrine, and renal side-effects of anti-PD-1 therapy. Eur J Cancer. 2016;60:190–209.
Corsello SM, et al. Endocrine side effects induced by immune checkpoint inhibitors. J Clin Endocrinol Metab. 2013;98(4):1361–75.
Ribas A, et al. Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trial. Lancet Oncol. 2015;16(8):908–18.
Horvat TZ, et al. Immune-related adverse events, need for systemic immunosuppression, and effects on survival and time to treatment failure in patients with melanoma treated with Ipilimumab at Memorial Sloan Kettering Cancer Center. J Clin Oncol. 2015;33(28):3193–8.
Eigentler TK, et al. Diagnosis, monitoring and management of immune-related adverse drug reactions of anti-PD-1 antibody therapy. Cancer Treat Rev. 2016;45:7–18.
Ryder M, et al. Endocrine-related adverse events following ipilimumab in patients with advanced melanoma: a comprehensive retrospective review from a single institution. Endocr Relat Cancer. 2014;21(2):371–81.
Dillard T, et al. Anti-CTLA-4 antibody therapy associated autoimmune hypophysitis: serious immune related adverse events across a spectrum of cancer subtypes. Pituitary. 2010;13(1):29–38.
Blansfield JA, et al. Cytotoxic T-lymphocyte-associated antigen-4 blockage can induce autoimmune hypophysitis in patients with metastatic melanoma and renal cancer. J Immunother. 2005;28(6):593–8.
Juszczak A, et al. Ipilimumab: a novel immunomodulating therapy causing autoimmune hypophysitis: a case report and review. Eur J Endocrinol. 2012;167(1):1–5.
van den Eertwegh AJ, et al. Combined immunotherapy with granulocyte-macrophage colony-stimulating factor-transduced allogeneic prostate cancer cells and ipilimumab in patients with metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13(5):509–17.
Madan RA, et al. Ipilimumab and a poxviral vaccine targeting prostate-specific antigen in metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13(5):501–8.
Min L, Vaidya A, Becker C. Association of ipilimumab therapy for advanced melanoma with secondary adrenal insufficiency: a case series. Endocr Pract. 2012;18(3):351–5.
Mahzari M, et al. Immune checkpoint inhibitor therapy associated hypophysitis. Clin Med Insights Endocrinol Diabetes. 2015;8:21–8.
Albarel F, et al. Long-term follow-up of ipilimumab-induced hypophysitis, a common adverse event of the anti-CTLA-4 antibody in melanoma. Eur J Endocrinol. 2015;172(2):195–204.
Marlier J, et al. Ipilimumab, not just another anti-cancer therapy: hypophysitis as side effect illustrated by four case-reports. Endocrine. 2014;47(3):878–83.
Faje AT, et al. Ipilimumab-induced hypophysitis: a detailed longitudinal analysis in a large cohort of patients with metastatic melanoma. J Clin Endocrinol Metab. 2014;99(11):4078–85.
Della Vittoria Scarpati G, et al. Ipilimumab in the treatment of metastatic melanoma: management of adverse events. Onco Targets Ther. 2014;7:203–9.
Grossman AB. Clinical review#: the diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010;95(11):4855–63.
Arafah BM. Medical management of hypopituitarism in patients with pituitary adenomas. Pituitary. 2002;5(2):109–17.
Downey SG, et al. Prognostic factors related to clinical response in patients with metastatic melanoma treated by CTL-associated antigen-4 blockade. Clin Cancer Res. 2007;13(22 Pt 1):6681–8.
Caturegli P, et al. Autoimmune hypophysitis. Endocr Rev. 2005;26(5):599–614.
Gordon IO, et al. Immune-mediated red cell aplasia after anti-CTLA-4 immunotherapy for metastatic melanoma. Cancer Immunol Immunother. 2009;58(8):1351–3.
Akhtari M, et al. Neutropenia in a patient treated with ipilimumab (anti-CTLA-4 antibody). J Immunother. 2009;32(3):322–4.
Delyon J, Mateus C, Lambert T. Hemophilia a induced by ipilimumab. N Engl J Med. 2011;365(18):1747–8.
Ahmad S, et al. Ipilimumab-induced thrombocytopenia in a patient with metastatic melanoma. J Oncol Pharm Pract. 2012;18(2):287–92.
Hahn L, Pepple KL. Bilateral neuroretinitis and anterior uveitis following ipilimumab treatment for metastatic melanoma. J Ophthalmic Inflamm Infect. 2016;6(1):14.
Papavasileiou E, et al. Ipilimumab-induced ocular and orbital inflammation-a case series and review of the literature. Ocul Immunol Inflamm. 2016;24(2):140–6.
Abu Samra K, et al. A case of bilateral uveitis and papillitis in a patient treated with pembrolizumab. Eur J Ophthalmol. 2016;26(3):e46–8.
de Velasco G, Bermas B, Choueiri TK. Autoimmune arthropathy and uveitis as complications of programmed death 1 inhibitor treatment. Arthritis Rheumatol. 2016;68(2):556–7.
Tarhini A. Immune-mediated adverse events associated with ipilimumab ctla-4 blockade therapy: the underlying mechanisms and clinical management. Scientifica (Cairo). 2013;2013:857519.
Chan MM, et al. Arthritis and tenosynovitis associated with the anti-PD1 antibody pembrolizumab in metastatic melanoma. J Immunother. 2015;38(1):37–9.
Hunter G, Voll C, Robinson CA. Autoimmune inflammatory myopathy after treatment with ipilimumab. Can J Neurol Sci. 2009;36(4):518–20.
Vallet H, et al. Pembrolizumab-induced necrotic myositis in a patient with metastatic melanoma. Ann Oncol. 2016;27(7):1352–3.
Andersen R, et al. Late development of splenic sarcoidosis-like lesions in a patient with metastatic melanoma and long-lasting clinical response to ipilimumab. Oncoimmunology. 2014;3(8):e954506.
Brahmer JR, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–65.
Berthod G, et al. Pulmonary sarcoid-like granulomatosis induced by ipilimumab. J Clin Oncol. 2012;30(17):e156–9.
Eckert A, et al. Anti-CTLA4 monoclonal antibody induced sarcoidosis in a metastatic melanoma patient. Dermatology. 2009;218(1):69–70.
van den Brom RR, et al. Rapid granulomatosis with polyangiitis induced by immune checkpoint inhibition. Rheumatology (Oxford). 2016;55(6):1143–5.
Goldstein BL, Gedmintas L, Todd DJ. Drug-associated polymyalgia rheumatica/giant cell arteritis occurring in two patients after treatment with ipilimumab, an antagonist of ctla-4. Arthritis Rheumatol. 2014;66(3):768–9.
Wilgenhof S, Neyns B. Anti-CTLA-4 antibody-induced Guillain-Barre syndrome in a melanoma patient. Ann Oncol. 2011;22(4):991–3.
Yang JC, et al. Ipilimumab (anti-CTLA4 antibody) causes regression of metastatic renal cell cancer associated with enteritis and hypophysitis. J Immunother. 2007;30(8):825–30.
Maur M, et al. Posterior reversible encephalopathy syndrome during ipilimumab therapy for malignant melanoma. J Clin Oncol. 2012;30(6):e76–8.
Liao B, et al. Atypical neurological complications of ipilimumab therapy in patients with metastatic melanoma. Neuro Oncol. 2014;16(4):589–93.
Thaipisuttikul I, Chapman P, Avila EK. Peripheral neuropathy associated with ipilimumab: a report of 2 cases. J Immunother. 2015;38(2):77–9.
Bhatia S, et al. Inflammatory enteric neuropathy with severe constipation after ipilimumab treatment for melanoma: a case report. J Immunother. 2009;32(2):203–5.
Forde PM, et al. Ipilimumab-induced immune-related renal failure--a case report. Anticancer Res. 2012;32(10):4607–8.
Izzedine H, et al. Kidney injuries related to ipilimumab. Investig New Drugs. 2014;32(4):769–73.
Fadel F, El Karoui K, Knebelmann B. Anti-CTLA4 antibody-induced lupus nephritis. N Engl J Med. 2009;361(2):211–2.
Di Giacomo AM, et al. Therapeutic efficacy of ipilimumab, an anti-CTLA-4 monoclonal antibody, in patients with metastatic melanoma unresponsive to prior systemic treatments: clinical and immunological evidence from three patient cases. Cancer Immunol Immunother. 2009;58(8):1297–306.
Geisler BP, et al. Apical ballooning and cardiomyopathy in a melanoma patient treated with ipilimumab: a case of takotsubo-like syndrome. J Immunother Cancer. 2015;3:4.
Mehta A, et al. Myocarditis as an immune-related adverse event with ipilimumab/nivolumab combination therapy for metastatic melanoma. Melanoma Res. 2016;26(3):319–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Sammons, S., McNamara, M., Salama, A.K.S., Crawford, J. (2018). Immune Checkpoint Inhibition. In: Dicato, M., Van Cutsem, E. (eds) Side Effects of Medical Cancer Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-70253-7_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-70253-7_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-70252-0
Online ISBN: 978-3-319-70253-7
eBook Packages: MedicineMedicine (R0)