Abstract
An accurate evaluation of acute pyelonephritis (APN) requires imaging of parenchymal involvement. When no predisposing conditions to complicated APN are found at US, noncomplicated APN is suspected, and CT or MRI should be performed. As patients with noncomplicated APN are mostly young women, gadolinium-enhanced (GE) MRI is preferred. Diffusion-weighted (DW) MRI might be quicker and cheaper than standard GE-MRI and is reliable for diagnosing or ruling out noncomplicated APN, due to the high diagnostic agreement with GE-MRI. However, GE-MRI is still mandatory for accurately staging APN within 48 h after diagnosis. DWI with ADC evaluation might be also useful in following therapeutic management of APN, without using ionizing radiation or contrast media.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute pyelonephritis (APN)
- Urinary tract infections (UTI)
- Gadolinium-enhanced magnetic resonance imaging (GE-MRI)
- Diffusion-weighted magnetic resonance imaging (DW-MRI)
- Apparent diffusion coefficient (ADC)
1 Background
Acute pyelonephritis (APN) is a non-specific suppurative inflammatory process due to hematogenous bacterial diffusion or secondary to ascending infection from the urinary bladder [1]. In fact, it is frequently associated with lower urinary tract infections (UTI) and involves all kidney structures, with E. coli as the most commonly found organism. UTI is more commonly seen in women [2].
Urinary tract infections accounted for two million emergency department visits in the USA in 2007 [3,4,5,6]. In that country acute pyelonephritis (APN) has an incidence as high as 250,000 cases per year, mostly in young women, and necessitates 200,000 hospitalizations every year [7,8,9]. There are very few data on the overall incidence of APN in Europe, being influenced by the type of sanitary system and the hospitalization policy; however, based on a previous surveillance on the referral area to our University Hospital, the gross incidence of hospitalized APN cases can be estimated as about 26.5 new cases per year per 100,000 inhabitants [10].
According to the British Medical Research Council Bacteriuria Committee [7], the definition of APN is clinical, based on a classic tetrad of high fever, costovertebral angle tenderness, signs or symptoms of lower UTI (leukocytosis, pyuria), and positive urinary cultures. As this definition does not discriminate between upper UTI with and without renal parenchymal involvement, other authors follow a “pathological” criterion, based upon the demonstration of kidney involvement by imaging techniques [8].
A general consensus is reached for the definition of “complicated” versus “noncomplicated” APN [9,10,11,12]. “Complicated” refers to the presence of systemic (any factor affecting the immune response, including diabetes, collagen disease, neoplasia, chemotherapy, HIV positivity, neuromuscular disease, hemoglobinopathies) or anatomical (any factor causing obstruction, including active stone disease, prostatic hypertrophy, kidney malformations, reflux nephropathy, polycystic kidney disease, and indwelling catheters) predisposing factors. “Noncomplicated” refers to their absence [10].
2 MRI and DW-MRI in the Workup of APN
In view of its low sensitivity for the presence of parenchymal lesions [13] but high sensitivity for obstructive lesions, conventional ultrasound (US) is used to identify the presence of anatomical or other predisposing factors for complicated APN, and further investigation is adopted based on US findings. In cases with a clinical suspicion of APN in which no predisposing condition is found at US, noncomplicated APN should be suspected, and a second-line imaging test has to be performed as well. Computed tomography (CT) or magnetic resonance imaging (MRI) examination allows precise definition of the inflammatory areas and evidence of abscesses [1, 14–15]. As patients with noncomplicated APN are mostly women of childbearing age, MR might be chosen as the preferred imaging technique, and CT should be performed only in the case of contraindications or logistical problems (i.e., long wait before the availability of an MRI) [16].
MRI, using a parallel imaging technique acquisition, is able to perform dynamic enhanced studies, with diagnostic accuracy comparable to CT [17]. It does not use ionizing radiation, and it is equipped with considerable contrast resolution. Between sequences performed in a basal setting, diffusion-weighted magnetic resonance imaging (DW-MRI) has recently gained particular interest [18]. It is realizable by analyzing the spin dephasing and signal loss caused by random motion along magnetic field gradients. The apparent diffusion coefficient (ADC), as a quantitative parameter calculated from the DW-MRI acquisition, combines the effects of capillary perfusion and water diffusion in the intracellular extravascular space.
The development of echo-planar imaging (EPI), high-gradient amplitudes, multichannel coils, and parallel imaging has been helpful in increasing the applications of DW sequences. In particular, the introduction of parallel imaging, such as sensitivity encoding (SENSE), which allowed reduction in the echo-train length (TE) and the K-space filling time, led to considerably less motion artifacts at image acquisition, thus enabling high-quality DW images of the body to be acquired. Hence, DWI might be useful in differentiating APN, with the advantage of lower costs and execution times than gadolinium-enhanced MRI (GE-MRI). The following protocol is used at our institution.
3 MRI and DW-MRI Diagnosis of APN
Our study protocol is presented in Table 11.1. As summarized in Table 11.2, the MRI findings consistent with APN include:
At basal MRI:
-
Changes in renal volume (kidney enlargement, presumably due to edema from active infection) often associated with perinephric inflammatory fluid and stranding of the perinephric fat (Fig. 11.1a, b, c)
-
Alteration of corticomedullary delineation (reduced or absent) (Fig. 11.1d)
-
Focal or diffuse parenchymal signal alteration, with isointensity at T1-weighted sequences and slight hyperintensity at T2-weighted images or heavy hyperintensity at T2-weighted images in abscess
-
Hyperintensity at the DWI sequences with high b value and hypointensity in the same area on ADC maps, correlating with focal reduction of enhancement at T1-weighted sequences in the contrast-enhanced study (Fig. 11.2a, b)
(a) Axial SPAIR SENSE show right kidney enlargement due to edema. (b) Axial SPAIR SENSE show fat stranding around caudal right kidney pole. (c) Axial SPAIR SENSE show thin perirenal effusion. (d) Axial 3D FFE T1w Dixon show abnormal cortico medullary interface consistent in poor/absent delineation of cortical layer
After the administration of contrast medium (GE-MRI), on T1-weighted sequences:
-
Reduction of parenchymal contrast enhancement in the affected area. Multiple areas can readily be affected, and in most cases lesions are well-defined, wedge-shaped areas with their bases at the periphery and apexes toward the renal sinus, with the renal parenchyma sometimes demonstrating a striated appearance. These abnormalities indicate hypoperfusion secondary to arteriolar vasoconstriction and inflammatory response (Fig. 11.3a, b).
-
Abscessed areas, as fluid lesions delineated by a peripheral halo dilation of the collecting system (mild, moderate, marked) (Fig. 11.3c, d, e, f).
(a) Axial 3D FFE T1w enhanced Dixon show reduction of parenchymal contrast enhancement in the affected wedge shaped area. (b) Axial 3D FFE T1w enhanced Dixon show multiple fluid filled lesion in the affected area consistent with microabscess. (c, d) Coronal TE_100 T2w SENSE and Axial SPAIR T2w show well defined superior left pole mass with intermediate T2w signal and thickened periferal wall, consistent in macroabscess. (e, f) Axial DWI (b800) show marked hyperintensity of the mass with clear restricted diffusion in ADC map
4 Role of MRI and DW-MRI in the Diagnostic Algorithm
APN is a topic that has remained relatively neglected in terms of imaging research, and its diagnosis is still a challenge. None of the clinical signs or laboratory biochemical markers at presentation allow discrimination between a few small lesions and multifocal or abscessed ones [15]. Thus, imaging techniques are needed to assess the severity of kidney involvement and to plan the antibiotic therapy. Diagnostic imaging plays a role in looking for previous occult structural or functional abnormalities that may require intervention, to assess those patients at significant risk of more life-threatening complications as in diabetic, elderly, or immunosuppressed patients, to balance the severity of the infection, and to evaluate the extent of organ damage subsequent to a resolved acute infection. Second-line imaging tests (CT or MRI) should be systematically used to define the presence, extent, and type of parenchymal lesions and to reveal complications (such as abscess or perirenal fluid collections), in order to tailor interventions to the specific clinical contexts [19, 20].
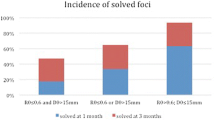
Our interest in APN originated from the observation of the increasing frequency of this disease and from the uncertain indications in the literature with regard to the opportunity to perform DW-MRI [21,22,23,24,25]. DWI provides information about the molecular translational motion of water, which can be affected by disease. This DW finding is probably secondary to compressive alterations due to edematous swelling and inflammatory parenchymal damage responsible for interstitial space reduction, with a resulting decrease in the diffusivity of water molecules. The degree of restricted diffusion is affected by various factors, including the type of pathogenic organism, the concentration of inflammatory cells and bacteria, the degree of viscosity, and the protein level [26–27]. ADC is a measure of the degree of molecular water motion. Lesions of high signal intensity on high-b-value images correspond to lesions of low signal intensity on the ADC map, and they represent restricted diffusion. Dealing with functional DW-MRI, in our series the mean ADC value was 2.38 ± 0.14 × 10−3 mm2 s−1, with a range of 1.99–2.76 × 10−3 mm2 s−1. In areas of affected parenchyma, ADC value in mm2/s was found to be consistently lower (mean 1.385; minimum 1.109, maximum 1.717) compared with healthy parenchyma (mean 2.383; minimum 1.989, maximum 2.763) (Fig. 4).
Comparing DW-MRI with gadolinium-enhanced (GE) MRI for diagnostic accuracy in APN in 163 patients with noncomplicated APN, we found DWI-MRI achieving 95.2% sensitivity, 94.9% specificity, a 96.9% positive predictive value, a 92.3% negative predictive value, and 94.6% accuracy.
Several other reports noted the utility of non-enhanced MRI, particularly DWI, in the diagnosis of APN. Kuniyoshi et al. used non-enhanced MRI with DWI to detect foci in children with APN, showing high-intensity lesions as well [28]. In another study, 39 children (mean age, 5.7 years) with suspected APN underwent MRI, including DWI and gadolinium-enhanced T1-weighted imaging (Gd-T1-WI). The sensitivity and specificity of the DWI were 100% (32/32) and 93.5% (43/46), respectively [29].
The high diagnostic agreement between DW-MRI and GE-MRI provided an interesting starting point for gaining a new perspective on the diagnostic management of APN. In fact, DW-MRI of the kidney seems to be a feasible, rapid, and reliable method as quantification of ADC values can be useful in diagnosing noncomplicated APN. The high diagnostic agreement between GE-MRI and DW-MRI offers new perspectives in diagnostic management, enabling monitoring of APN in a short time without use of ionizing radiation or administration of paramagnetic contrast medium. We can assume the use of DW-MRI, together with the performance of the usual basal sequences T1 and T2, in the acute phase, possibly in the ED, affecting minimally (negligible time is required) the workflow of the MRI service, thus allowing a timely therapeutic approach.
Thereafter, in case of hospitalization, an exam with paramagnetic contrast as first examination should be systematically used to better define the presence, extent, and type of parenchymal lesions and to reveal complications (such as abscess or perirenal fluid collections), in order to tailor interventions to the specific clinical contexts [19, 20].
The subsequent checks, performed about every 3 weeks until complete resolution of the inflammatory process, may instead be programmed with DWI alone (Table 11.3).
Additionally, DW-MRI is an alternative to dynamic investigation in all cases where there are contraindications to administration of iodinated and/or paramagnetic contrast medium, such as those patients with renal insufficiency and pregnant or lactating women. Actually, the short duration of the examination and the easy response and reproducibility of ADC values allow a proper diagnostic evaluation even in uncooperative subjects or slightly sedated claustrophobic ones. Dealing with costs too, DW-MRI is an interesting tool for detecting noncomplicated APN, thanks to its inherent cost and its potential impact on the suitability and timeliness of treatment.
References
Craig WD, Brent JW, Travis MD (2008) From the archives of the AFIP, pyelonephritis: radiologic-pathologic review. Radiographics 28:255–276
Schappert SM, Rechtsteiner EA (2011) Ambulatory medical care utilization estimates for 2007. Vital Health Stat 13(169):1–38
Hooton TM, Stamm WE (1997) Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin N Am 11:551–581
Ramakrishnan K, Schedi DC (2005) Diagnosis and management of acute pyelonephritis in adults. Am Fam Physician 71:933–942
Georgi A, Reddy YNV, Gautam G (2012) Diagnosis of acute pyelonephritis with recent trends in management. Nephrol Dial Transplant 27:3391–3394
Ramzan MM, Sandstrom CK (2016) Core curriculum illustration: acute pyelonephritis. Emerg Radiol:1–3. https://doi.org/10.1007/s10140-016-1474-2
Medical Research Council Bacteriuria Committee (1979) Recommended terminology of urinary tract infection: a report by the members of Medical Research Council Bacteriuria committee. Br Med J 2:717–719
Talner LB, Davidson AJ, Lebowitz RL, Dalla Palma L, Goldman SM (1994) Acute pyelonephritis: can we agree on terminology? Radiology 192:297–305
Dyer RB (1997) CT of renal inflammatory disease. Invited commentary. Radiographics 17:867–868
De Pascale A, Piccoli GB, Priola SM et al (2013) Diffusion-weighted magnetic resonance imaging: new perspectives in the diagnostic pathway of non-complicated acute pyelonephritis. Eur Radiol 23(11):3077–3086. https://doi.org/10.1007/s00330-013-2906-y
Soulen MC, Fishman EK, Goldman SM, Gatewood OM (1989) Sequelae of acute renal infection: CT evaluation. Radiology 173:423–426
Webb JAW (1987) The role of imaging in adult acute urinary tract infection. Eur Radiol 7:837–843
Parenti GC, Passari A (2001) Pielonefrite acuta: ruolo della diagnostica per immagini. Radiol Med 101:251–254
Majd M, Nussbaum Blask AR, Markle BM et al (2001) Acute pyelonephritis: comparison of diagnosis with 99mTc-DMSA, SPECT, spiral CT, MR imaging, and power Doppler US in an experimental pig model. Radiology 218:101–108. Diffusion-weighted magnetic resonance imaging: new perspectives in the diagnostic pathway of non-complicated acute pyelonephritis
Piccoli GB, Consiglio V, Deagostini MC et al (2011) The clinical and imaging presentation of acute “non complicated” pyelonephritis, a new profile for an ancient disease. BMC Nephrol 12:68–78
Martina MC, Campanino PP, Caraffo F et al (2010) Dynamic magnetic resonance imaging in acute pyelonephritis. Radiol Med 115:287–300
Nikken JJ, Krestin GP (2007) MRI of the kidney: state of the art. Eur Radiol 17:2780–2793
Hagmann P, Jonasson L, Maeder P, Thiran JP, Wedeen VJ, Meuli R (2006) Understanding diffusion MR imaging technique. Radiographics 26:S205–S223
Kawashima A, Sandler CM, Goldman SM (2000) Imaging in acute renal infection. BJU Int 86:70–79
Johansen TE (2004) The role of imaging in urinary tract infections. World J Urol 22:392–398
Muller MF, Prasad PV, Bimmler D, Kaiser A, Edelman RR (1994) Functional imaging of the kidney by means of measurement of the apparent diffusion coefficient. Radiology 193:711–715
Chow LC, Bammer R, Moseley ME, Sommer FG (2003) Single breath-hold diffusion-weighted imaging of the abdomen. J Magn Reson Imaging 18:377–382
Thoeny HC, De Keyzer F, Oyen RH, Peeters RR (2005) Diffusionweighted MR imaging of kidneys in healthy volunteers and patients with parenchymal diseases: initial experience. Radiology 235:911–917
Xu Y, Wang X, Jiang X (2007) Relationship between the renal apparent diffusion coefficient and glomerular filtration rate: preliminary experience. J Magn Reson Imaging 26:678–681
Carbone SF, Gaggioli E, Ricci V, Mazzei F, Mazzei MA, Volterrani L (2007) Diffusion-weighted magnetic resonance imaging in the evaluation of renal function: a preliminary study. Radiol Med 112:1201–1210
Fanning NF, Laffan EE, Shroff MM (2006) Serial diffusion-weighted MRI correlates with clinical course and treatment response in children with intracranial pus collections. Pediatr Radiol 36:26–37
Aoyagi J, Odaka J, Kuroiwa Y, Nakashima N, Ito T, Saito T, Kanai T, Yamagata T, Momoi MY (2014) Utility of non-enhanced magnetic resonance imaging to detect acute pyelonephritis. Pediatr Int 56(3):e4–e6. https://doi.org/10.1111/ped.12312
Kuniyoshi Y, Kamura A, Yasuda A, Tashiro M (2011) Acute pyelonephritis diagnosed by diffusion-weighted whole body imaging with background signal suppression: three case reports. J Jpn Pediatr Soc 115:1919–1925
Vivier P-H et al (2014) MRI and suspected acute pyelonephritis in children: comparison of diffusion-weighted imaging with gadolinium-enhanced T1-weighted imaging. Eur Radiol 24:19–25
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Veltri, A., De Pascale, A., Gned, D. (2018). MRI and DW-MRI of Acute Pyelonephritis (APN). In: Tonolini, M. (eds) Imaging and Intervention in Urinary Tract Infections and Urosepsis. Springer, Cham. https://doi.org/10.1007/978-3-319-68276-1_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-68276-1_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-68275-4
Online ISBN: 978-3-319-68276-1
eBook Packages: MedicineMedicine (R0)