Abstract
Objectives: Arterial hypertension is among the leading risks for mortality. This burden requires in hypertensive patients the use of single, double or more antihypertensive drugs. The relationship between intracranial pressure (ICP) and arterial blood pressure is complex and still under debate. The impact of antihypertensive drugs on ICP is unknown. We wanted to understand whether the use of antihypertensive drugs has a significant influence on ICP and cerebrospinal fluid (CSF)/brain related parameters.
Materials and methods:In a cohort of 95 patients with suspected normal pressure hydrocephalus, we prospectively collected drug details according to the Anatomical Therapeutic Chemical (ATC) classification. Lumbar infusion studies were performed. Using ICM+ software, we calculated at baseline and plateau ICP and pulse amplitude, resistance to CSF outflow, elastance, and pressure in the sagittal sinus and CSF production rate. We studied the influence of the administration of 1, 2, 3 or more antihypertensive drugs on ICP-derived parameters. We compared the data using Student’s and Mann–Whitney tests or Chi-squared and Fisher’s exact test.
Results: Elastance is significantly higher in patients with at least one antihypertensive drug compared with patients without medication. On the contrary, pressure volume index (PVI) is significantly decreased in patients with antihypertensive drugs compared with patients not on these medications. However, the number of antihypertensive drugs does not seem to influence other ICP parameters.
Conclusions: Patients on antihypertensive drugs seem to have a stiffer brain than those not on them.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
The interaction between intracranial pressure (ICP) and arterial blood pressure (ABP) is complex and still ill-understood. Hypertension, i.e., high ABP, has no symptoms, but if not treated it can damage the kidneys, heart, and brain, with an increased risk of renal failure, myocardial infarction, and stroke. In that respect, hypertension is among the leading risks for mortality. Hence, lowering ABP reduces the risk, in particular, of stroke. Hence, antihypertensive drugs must influence directly or indirectly not only brain biomechanical characteristics but also ICP.
This burden of hypertension requires the use of one, two or more antihypertensive drugs. These drugs are classified by the Anatomical Therapeutic Chemical (ATC) system. This is an international system [1] that defines a drug as part of different groups according to the organ or system on which they act and their therapeutic, pharmacological, and chemical properties. Drugs are classified in groups at five different levels. The drugs are divided into 14 main groups (the first level, which is an alphabetic letter), with pharmacological/therapeutic subgroups (second level). The third and fourth levels are used to identify pharmacological subgroups when that is considered more appropriate than therapeutic or chemical subgroups. Examples of the main groups: A alimentary tract and nutrition, B blood and blood forming organs, C cardiovascular system, D dermatologicals, etc.… With regard to antihypertensive drugs, the most common medications are angiotensin-converting enzyme (ATC C09A), angiotensin-2 receptor blockers (ATC C09C), calcium channel blockers (ATC C08), diuretics (ATC C03), and beta-blockers (ATC C07).
We hypothesize that the use of one or several antihypertensive drugs might influence ICP and brain biomechanical characteristics.
Materials and Methods
Study Population
Our analysis was carried out in a prospective cohort of 95 patients with suspected normal pressure hydrocephalus. We collected drug details according to the ATC classification. Thus, we classified patients according to the number of antihypertensive drugs they take to compare the potential effects of these treatments on ICP and brain characteristics.
Infusion Studies
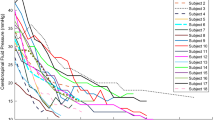
Lumbar infusion studies were performed for every patient [2]. Using ICM+ software we analyzed nine parameters of cerebral hydrodynamics: baseline and plateau ICP, baseline and plateau of pulse amplitude, resistance to CSF outflow and an estimation of elastance, pressure volume index (PVI), pressure in the sagittal sinus (PSS), and CSF production rate.
Statistical Analysis
We studied the influence of antihypertensive drugs on the mean value of all nine parameters. For our statistical analysis, we made two comparisons. The first one was between patients with 0–2 antihypertensive drugs and patients with 3 or 4 antihypertensive drugs. The second one was between patients without treatment and patients with at least one antihypertensive drug. Quantitative values were compared using Student’s test or Mann–Whitney test and qualitative values were compared using Chi-squared test or Fisher’s exact test.
Results
Characteristics of the population are detailed in Table 1. Comparative overview shows that the two subpopulations have similar characteristics according to age, gender, and mean arterial blood pressure. Parameters of 84 patients with 0, 1 or 2 antihypertensive drugs were compared with parameters of 11 patients with 3 or 4 antihypertensive drugs. The number of antihypertensive drugs does not seem to be associated with ICP parameters (Table 2, left panel).
However, the presence of at least one antihypertensive drug is significantly associated with an increased estimation of brain elastance compared with patients not taking antihypertensive drugs (0.16 ± 0.01 vs 0.26 ± 0.003, p = 0.0017). Unsurprisingly, the PVI parameter is significantly decreased in the same group (13.24 ± 1 vs 17.8 ± 0.9, p = 0.021).
The PSS is significantly increased in patients with at least one antihypertensive drug compared with those not taking antihypertensive drugs (2.42 ± 1.5 vs 4.3 ± 0.8, p < 0.0001 respectively).
Conclusion
Our study reveals that brain stiffness is associated with the use of antihypertensive drugs through elastance, PVI, and PSS markers. Arterial stiffness is emerging as an important risk marker for pathological brain aging and dementia through its associations with cerebral small vessel disease, stroke, β-amyloid deposition, brain atrophy, and cognitive impairment [3]. Indeed, arterial stiffness provides an important link between systemic hypertension and dementia, because it serves as the driving force behind the effects of hypertension on the microvasculature of the brain. Brain stiffness probably provides an indirect expression of arterial stiffness. One hypothesis could be that the use of antihypertensive drugs is probably an indirect marker of an altered microcirculation. Our data reinforce the concept that vascular diseases participate in brain alteration. We plan to further explore the influence of other drugs on ICP and CSF/brain biomechanics.
References
Word Health Organization. WHOCC – structure and principles. Collaboration Centre for Drug Statistics Methodology. 2011 [accessed 8 Nov 2016]. http://www.whocc.no/atc/structure_and_principles/.
Czosnyka M, Czosnyka Z, Momjian S, Pickard JD. Cerebrospinal fluid dynamics. Physiol Meas. 2004;25:R1–27. PII: S0967-3334(04)70217-8.
Hughes TM, Craft S, Lopez OL. Review of the potential role of arterial stiffness in the pathogenesis of Alzheimer’s disease. Neurodegener Dis Manag. 2015;5(2):121–35.
Conflicts of interest statement
We declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this paper
Cite this paper
Rouzaud-Laborde, C., Lafitte, P., Balardy, L., Czosnyka, Z., Schmidt, E.A. (2018). ICP and Antihypertensive Drugs. In: Heldt, T. (eds) Intracranial Pressure & Neuromonitoring XVI. Acta Neurochirurgica Supplement, vol 126. Springer, Cham. https://doi.org/10.1007/978-3-319-65798-1_34
Download citation
DOI: https://doi.org/10.1007/978-3-319-65798-1_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65797-4
Online ISBN: 978-3-319-65798-1
eBook Packages: MedicineMedicine (R0)