Abstract
Although traumatic experiences increase risk for myriad mental health sequelae, most individuals who experience marked adverse events do not meet the criteria for psychiatric disorders or appear to sustain chronic injury or functional impairments. This chapter entails several of the critical aspects of psychosocial resilience and recovery in the context of distal and proximal trauma. First, we review the literature on posttraumatic well-being among peripartum women. Second, we consider therapeutic processes central to trauma recovery and survivors’ care preferences. Finally, we present information on the current state of knowledge regarding the application of empirically supported interventions for major depressive disorder (MDD), posttraumatic stress disorder (PTSD), and affect regulation difficulties to trauma-exposed peripartum women.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Peripartum Women
- Posttraumatic Stress Disorder (PTSD)
- Affect Regulation Difficulties
- Postpartum PTSD
- Peripartum Depression
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Resilience and Recovery
The construct of resilience within mental health is generally characterized as a biopsychosocially determined general capacity to maintain well-being despite stress exposure or a comprisal of factors that buffer against illness (see Fig. 8.1). For instance, following childhood trauma, MDD, PTSD, and chronic affect regulation difficulties have been repeatedly observed as potential sequelae. Yet, and often overlooked, the overwhelming majority of individuals who experience adversity do not meet diagnostic criteria for mental health disorders. Relatedly, recovery refers to the observation that many individuals who meet the criteria for posttrauma mental health diagnoses do not report persistent complaints. The more common pattern of resistance and recovery from trauma raises several questions. What individual or environmental characteristics are associated with increased ability to withstand stress exposure? Once diagnostic levels of symptoms and impairments are experienced, what naturalistic (i.e., nonintervention) factors are correlated with recovery? Do therapeutic interventions facilitate posttraumatic healing, and for which conditions?
2 Naturalistic Processes of Resilience and Recovery in Peripartum Women
2.1 Childhood Trauma
For peripartum women, their historical experiences of childhood abuse and neglect may have longstanding effects that impact their pregnancy and child-rearing in adulthood in ways which may increase the risks for intergenerational transmission of negative outcomes. Several of these adverse consequences are described elsewhere in this volume. The investigations described in this section focus on resilience-related findings from our translational program of research evaluating maternal and infant outcomes among women exposed to childhood maltreatment (CM).
The Maternal Anxiety during the Childbearing Years (MACY; Muzik, PI) study is a longitudinal investigation from pregnancy through 18 months postpartum. The research oversampled women endorsing CM (N = 214, including n = 145 with CM histories). During the study, women completed surveys and qualitative interviews. Mothers completed questionnaires at delivery, 4, 6, 12, 15, and 18 months postpartum and engaged in free play and structured sessions (at a 6 and 15 months postpartum visit) focused on interactions with their children.
To explore protective factors, our first study (Sexton et al. 2015) examined main and moderating effects of resilience as measured by the Connor-Davidson Resilience Scale (Connor and Davidson 2003) and childhood trauma severity on postpartum depression, PTSD, positive family functioning, and maternal self-confidence. Despite the high rates of CM in this sample, most mothers did not evidence PTSD (79.5% negative for diagnosis) or postpartum MDD (80.4% negative for diagnosis) at 4 months postpartum. Main effects were noted for CM severity and resilience on postpartum PTSD, MDD, and positive family functioning with trauma severity associated with poorer outcomes and resilience associated with better outcomes (i.e., decreased psychiatric risk and improved family support). Mothers endorsing higher levels of resilience were also more likely to report increased sense of parenting mastery.
Specific to moderating effects, the interaction of CM severity and resilience was associated with postpartum PTSD and MDD risk. When stratifying participants into quartiles of highest and lowest CM severity and resilience groups, we found an absence of PTSD in mothers with the lowest levels of CM, irrespective of resilience. However, for mothers with the highest levels of childhood abuse and neglect, the level of resilience was a major protective factor for the presence or absence of PTSD. Specifically, only 8% of those mothers with highest resilience and high CM exposure met PTSD criteria in contrast to 58% of mothers with lowest resilience and high CM. Similarly, among women in the highest resilience group, none met the criteria for MDD, irrespective of CM severity. But for women in the lowest resilience group, the level of resilience made a difference. In this low-resilience group, 25% of women with low levels of CM met diagnostic criteria for postpartum MDD compared to 68% of those with high levels of CM. These results suggest that resilience is critical for all mothers and is associated with improved family well-being, maternal competence, and reduction of PTSD and MDD risk. In addition, particularly for mothers with histories of childhood maltreatment, greater resilience may buffer against some of the common psychiatric outcomes associated with early trauma. This has particular clinical importance. CM histories, discussed elsewhere in this volume, are associated with adverse peripartum outcomes. Yet, resilience-enhancing interventions may offer a pathway to attenuate some deleterious effects associated with childhood trauma.
One facet of resilience, the ability to establish and solicit aid from social support networks, appears particularly protective against postpartum depression in at-risk women. Focusing on mothers with histories of CM, we evaluated the main and moderating effects of CM severity, social support, and income on postpartum depressive symptoms (Muzik et al. 2017). As may be expected, the severity of CM increased the risk of postpartum depression, while annual income and social support were inversely associated with symptoms. We observed a significant support-by-income interaction indicating that high social support mitigated the association between low income and depressive symptoms. Specifically, we found that mothers with high social support and low income reported significantly fewer symptoms than those mothers who also had low income but also experienced low social support. Most importantly, these low-income mothers with high social support were not significantly more symptomatic than high-income maternal peers with high social support. These results highlight the importance of close postpartum interpersonal relationships, particularly for those with limited financial resources.
We further investigated protective factors that may buffer against suicidal ideation (SI) among MACY-enrolled mothers with CM histories during the first 18 months postpartum (Muzik et al. 2016). Longitudinal trajectories indicated that 63% of mothers denied SI at all time points, and most mothers described only transient SI throughout this time frame. Specifically, at 4 months postpartum, resilience, financial resources, and being married or having a cohabitating partner reduced SI risk. At 6 months, the presence of family support was the primary protective factor against thoughts of self-harm. At 12 months, married or cohabitating mothers and those endorsing less trauma-specific shame demonstrated reduced risk of SI. At 15 months, resilience was associated with the presence or absence of SI, but only married/partnered status was predictive of the severity of thoughts. Finally, at 18 months, lower trauma-related shame was the only identified buffer against SI. Together, these results underscore the importance of understanding the interplay and variability of postpartum protective factors. Our findings suggest resilience and associated protective factors are not universal and constant safeguards but may fluctuate in importance depending on temporal changes in mother and infant development and interact with stressors (i.e., returning to work, loss of extended family support after early postpartum, increasing independence of the child, changes in sleeping and eating schedules) that may vary between parenting newborns and toddlers.
2.2 Peripartum Resilience to Adulthood Traumas
Psychological strain and morbidities secondary to myriad adulthood traumas are reviewed elsewhere in this volume and not further considered here. However, fewer investigations of resilience have been conducted and warrant attention.
In a study of peripartum resilience following Hurricane Katrina, Harville et al. (2010) found that older mothers, those in partnerships, and Caucasian women demonstrated increased peripartum resilience, whereas those who sustained a direct injury or illness demonstrated reduced well-being. Surprisingly, experiencing storm-related damage was correlated with report of increased resilience. Some possibilities may explain this finding. It may be the case that loss of property or other resources prompted mothers to engage social support networks and other resources that mitigated strain. Additionally, the immediacy of the stressor within a peripartum context may have increased the propensity of women to utilize active coping skills in response to burden.
In another study of proximal trauma, Hughes and Riches (2003) reviewed pertinent evidence specific to the clinical management of traumatic pregnancy loss. They report that, since the 1970s, close contact between parents and the deceased child has been recommended by care providers based on the belief this practice would assist mourning and reduce negative outcomes. However, in contrast to this philosophy, research found women who did not hold their babies following death were less likely to experience delivery- or miscarriage-related MDD or PTSD. Rather, the facilitation of social support engagement demonstrated improved resistance to psychiatric symptoms. The authors rightly note that for many women who experience pregnancy or child loss, parental autonomy, cultural practices, and personal preferences are paramount. Specifically, it may be the case that mothers elect to hold miscarried or stillborn children for important reasons even if it does increase their risk for psychiatric symptoms. In such cases, it is important to offer grieving parents control during this process. However, current evidence does not appear to justify this practice as a clinician-initiated recommendation for reducing adverse outcomes or facilitating healing. Together, the authors’ findings augment the importance of empirical assessment of routine clinical advice in order to limit potential for harming vulnerable populations.
2.3 Peripartum Resilience and Recovery in Non-trauma Research
Within non-trauma populations, studies have primarily examined the role of social support as a mechanism to inhibit the development of postpartum MDD. In a synthesis of the literature, Robertson et al. (2004) concluded that maternal perceptions of available emotional and practical support were associated with reduced probability of developing MDD postpartum. In addition to reducing depression risk, Leahy-Warren et al. (2012) further demonstrated that social support was positively associated with maternal self-efficacy in first-time mothers. The consistency with which interpersonal relationships appear associated with positive outcomes is likely exceptionally relevant for traumatized women although consideration of other potential factors associated with peripartum resistance to mental health concerns remains warranted.
While several factors associated with postpartum resilience have been identified, features associated with postpartum recovery from depressive symptoms exhibited during pregnancy have been more elusive, and longitudinal research remains scant. Gotlib et al. (1991) prospectively assessed 730 women from pregnancy through early postpartum on a number of factors: age, marital duration, stress, severity of depressive symptoms during pregnancy, bonding in the family of origin, coping strategies, and negative attitudes. Regression analyses did not confirm relationships between any of the variables under investigation and recovery from depressive symptoms. Similarly, Andersson et al. (2006) examined maternal age, economic resources, partnership status, alcohol and nicotine use, parity, obesity, and prenatal health difficulties and similarly did not identify factors apart from history of psychiatric disorders prior to pregnancy as predictive of depression and anxiety trajectories from pregnancy to postpartum.
In a separate longitudinal research study with pregnant women (Sexton et al. 2012), we observed 39% of women experiencing significant depressive symptoms at 32 weeks of pregnancy did not exhibit clinically significant symptoms at 12 weeks postpartum. We examined demographic factors, medication and psychotherapy utilization, prenatal exercise behaviors, history of depression, history of negative life events, family and partner support, adequacy of resources, and domestic division of labor as potential predictors of symptom course. Of the factors investigated, prenatal exercise, fewer depressive symptoms in pregnancy, and cohabitation with a partner were related to recovery from depressive symptoms at the postpartum assessment. While this sample was not drawn from a study emphasizing trauma history, a lifetime history of negative event exposure was not associated with reduced likelihood of recovery. Among multiparous mothers, a history of past postpartum depression, but not lifetime depression history, differentiated between those with transient and persisting complaints. Together, results suggest continued research is warranted to further discern factors associated with postpartum mental health recovery in those with prenatal symptoms. The finding that exercise behaviors are associated with improved mental health outcomes may be helpful to investigate further empirically given that most pregnant women experiencing symptoms do not engage in medication or therapy services but may consider other wellness recommendations from care providers.
3 Treatment Interventions to Promote Recovery and Resilience
When peripartum women present for therapeutic interventions, proximal and distal traumas often critically influence care. Several of the following chapters detail treatments developed specifically for pregnant, grieving, and postpartum women with histories of adversity and are beyond the scope of this chapter. Here, we will broadly consider salient intervention issues and processes that may emerge when working with traumatized clients, preferences articulated by survivors, and postpartum translations of empirically supported interventions for common posttraumatic presentations.
3.1 Therapeutic Issues, Processes, and Survivor Preferences
For many providers, facilitating recovery with traumatized women is simultaneously rewarding and challenging. Trauma survivors often present to care at various stages of healing with characteristics that may influence the therapeutic relationship and content. Not uncommonly, clients may be mistrustful of therapists or others they perceive as authorities, particularly if their trauma involves a perpetrator in a position of power. Likewise, clients may find themselves triggered when clinician characteristics are similar to stimuli present during traumatic events. For instance, rape survivors may be initially anxious about working with male therapists if their perpetrator was a male or otherwise physically or experientially similar. Others may display strong emotions of fear, anger, shame, and disgust. Concurrently, they may note a numbing of positive emotions and incapability to feel warmth and attachment to others. Some may have processed their trauma in such a way that solidifies negative cognitions about being responsible for their own injuries, that others are generally dangerous, and that they are not capable of recovery. During and after pregnancy, these beliefs can extend to perceptions that they are not “up to the challenge” of parenting, that they are harming their fetus or child with their inability to manage stress, or that others will not help when they need support. Oftentimes, survivors articulate difficulties with communicating effectively with tendencies toward aggressive or passive interactions that limit their ability to have their needs met. The use of Socratic questioning and motivational interviewing strategies may be particularly beneficial for “rolling with resistance,” providing affirming support, facilitating understanding, and developing rapport.
It is important to recognize that most of the symptoms that present in the context of depression, PTSD, and affect dysregulation often represent behaviors that were functional at the time the trauma occurred and developed for the purposes of assisting with the prevention of further harm or coping during taxing stressors. For instance, emotional numbing may have originated as a coping strategy to reduce emotional pain when situations could not be physically avoided. However, when these tendencies persist, individuals may find themselves limited in their behavioral and emotional engagement.
Fostering a clinical environment in which survivors feel autonomous, supported, safe, understood, and validated is paramount. For many clients, the therapeutic relationship may be their first disclosure of trauma. Normalizing experiences and matching clients’ pace are key to developing trusting and safe relationships. Some may have decided to disclose to others and perceived disclosures as supportive interactions that bolster well-being. Others may have had a history of disclosure experiences that were harmful. For example, those experiencing sexual trauma in the military frequently describe an initial assault followed by secondary stress when attempting to disclose their attack. They may describe being disbelieved, threatened, or minimized during these occasions. In the context of interpersonal violence, many describe receiving questions from social supports such as “why didn’t you just leave?,” which often appear accusatory. Beyond direct personal experiences, cultural norms influence trauma responding. Rape survivors may conclude that they are to blame for their attack and that it happened to them “for a reason,” beliefs that are often societally reinforced. Clients are often particularly attuned to the verbal and nonverbal signals provided by therapists during disclosure encounters. As such, it is particularly important that we examine our own potential biases and are thoughtful in our responses to difficult clinical content.
Recognizing the importance of autonomy and choices of survivors, we (Muzik et al. 2013) solicited treatment preferences of mothers with histories of CM. A subset of mothers enrolled in the MACY study engaged in qualitative interviews. Mothers identified ten factors that may facilitate readiness to enter care: respectful and trusting communication, staff diversity, team approaches to care, availability of a range of care options, accessible and coordinated physical and mental health services, flexible hours, incorporation and welcoming of children and family in care, attention to expansion of social supports, holistic approaches to care, and inspiring and discrete clinic names. Structural and interpersonal adaptions of care to meet the preferences of peripartum women may help resolve ambivalence about seeking care and facilitate entry into recovery interventions.
Many clients present with trauma or developmental experiences that involve marked interpersonal boundary violations. Interventions may focus on facilitating clients’ skills with the establishment of limits in their lives and healthy methods of giving and receiving power. It is further paramount to develop healthy exchanges within treatment sessions. The use of physical touch, dual relationships, or extended visits outside of those typically offered within the framework of the intervention can be particularly hazardous when working with those with trauma histories. Some providers elect to use self-disclosure of their own trauma histories, often to encourage the perception that they can be trusted or fully appreciate clients’ struggles. This may be consistent with peer support models of care, in which care by a “similar other” is explicitly solicited, as well as with some treatment paradigms. Yet, in therapeutic environments involving traumatized patients, ethical caution and consideration of potential adverse outcomes are critical. For instance, many clients report having a previous care provider who disclosed his or her own survivor history. Although some may perceive this as helpful for reducing reluctance to disclose, self-disclosure may result in clinically unintended consequences. Patients with previous providers who disclosed often remark treatment subsequently “became about them, not about me,” feeling embarrassed about experiencing distress when perceiving their providers’ experiences as “more severe,” or attempting to step into a caretaking role. Some report feeling more incompetent as their therapist seemed to be managing stress fine while they “felt like a mess.” Thorough consideration of balancing boundaries and flexibility within intervention environments and utilization of professional consultation can be particularly helpful to reduce the likelihood of inadvertently harming clients.
In addition to notable content of the therapy session, provider self-care is a fundamental aspect of delivering trauma interventions. Vicarious strain from hearing multiple trauma accounts and the energy expended working with survivors has long been associated with compassion fatigue. Colleague support can be especially beneficial. Interventions such as dialectical behavior therapy specifically incorporate the use of consultation teams to promote sustained motivation, peer provider support, advice, and model fidelity. Many other interventions and practices have case conference meetings or other formats for support and skill development that can buffer against provider strain. For many, consideration of work-life balance and engagement in enjoyable and meaningful activities can help bolster coping reserves. While some providers may manage clinical loads entirely comprised of trauma-related care, others elect to balance the percentage of trauma cases they see with engagement of other types of care or clinical activities. Clinicians are also not immune to many of the traumas their patients have experienced. Those that find they have sufficiently processed their own trauma or are managing their own life stress well may feel more prepared to be fully present and effective with clients.
3.2 Peripartum Applications of Empirically Supported Interventions Targeting Depression, PTSD, and Affect Dysregulation
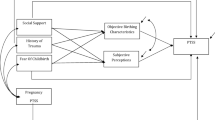
When posttrauma symptoms are present, certain mental health complaints are more likely sequelae of trauma (see Fig. 8.2) with depression, PTSD, and chronic difficulties with affect regulation among those most frequently encountered. Empirically supported interventions for these specific outcomes are extant, and several have been adapted or evaluated for use with peripartum populations.
3.3 Clinical Interventions for Peripartum Depression
Interpersonal therapy (IPT) is among the most well-researched cognitive behavioral interventions for peripartum depression with over 25 years of empirical investigation supporting its use with this population. As previously discussed, perceived and utilized social supports are paramount to resilience and recovery among both peripartum women and survivors of trauma. Further, in cases in which trauma occurs developmentally early, attachment to early caregivers is often disrupted. Theoretically, this framework considers disrupted attachments, unfulfilling interpersonal interactions, and role changes which increase the propensity to experience negative emotions. IPT is a time-limited (16 sessions or fewer) approach to care that augments social functioning through selection of a central focus area: role transitions, interpersonal disputes, or grief and role deficits. In a 2003 study, Spinelli and Endicott (2003) found 60% of depressed pregnant women treated with IPT met recovery criteria in contrast with 15% of women assigned to a parenting education control group. O’Hara et al. (2000) demonstrated similar results for women treated postpartum, finding that mothers engaged in IPT demonstrated recovery rates nearly three times higher than waitlist controls. In addition to symptom reduction, engagement in the intervention was associated with increased postpartum and social adjustment. Importantly, IPT appears not only effective at reducing peripartum depression but has also been successfully used to prevent the development of postpartum MDD (Zlotnick et al. 2006).
Cognitive behavioral therapies (CBT) targeting mood changes through the modification of negative thoughts or behaviors have also demonstrated effectiveness in the treatment or prevention of peripartum depression. In a meta-analysis of 37 intervention studies, Sockol et al. (2011) concluded IPT and CBT were both valuable psychotherapies for the treatment of peripartum depression. Further, therapies delivered individually were superior to those offered in group formats, and effect sizes were larger for treatments utilizing an IPT versus CBT framework.
Recently, peripartum sleep has garnered attention as a buffer against depression and anxiety. Insomnia and nightmares have long been associated with the development, maintenance, and recovery from MDD and PTSD in general populations. Several changes during pregnancy (i.e., increased awakenings due to pain, changes in recommended sleep position, nocturia) and postpartum (i.e., breastfeeding, infant wake cycles) provide new threats to peripartum women’s ability to obtain sufficient sleep. To concurrently target sleep and mood, Swanson et al. (2013) conducted an open pilot translation of cognitive behavioral therapy for insomnia incorporating postpartum-specific modifications for mothers with depression. Adaptations included solicitation of partner support to assist with nighttime feedings, psychoeducation regarding regulation of infant sleep cycles, and the associations between sleep and postpartum mood, permissibility of brief naps, and flexibility in treatment scheduling hours. Though further examination is warranted, the authors preliminarily report posttreatment increases in sleep efficiency and sleep quality and reductions in total time awake at night, mood symptoms, insomnia severity, and fatigue.
3.4 Clinical Interventions for PTSD
A strong literature supports the efficacy of psychotherapy for PTSD, most notably prolonged exposure (PE; Foa et al. 2007) and cognitive processing therapy (CPT; Resick and Schnicke 1993), each of which was initially developed for use with survivors of sexual trauma but are well validated for use following interpersonal violence experienced throughout the lifespan, combat trauma, accidents, and other types of trauma. PE is based on emotional processing theory, a conceptualization of posttraumatic reactions that includes feared trauma-related stimuli generalizing to other stimuli through avoidance. PE focuses on disaffirming these maladaptive fear structures through habituation across exposure to feared stimuli. PE is therefore an exposure-based therapy that incorporates imaginal exposure, for reprocessing the trauma memory, and in vivo exposure, to overcome avoidance of real-world situations and stimuli and promote engagement in valued areas. There is also a processing component to facilitate changes in trauma-related cognitions through these exposure tasks. CPT, also a cognitive behavioral treatment, is grounded in social cognitive theory, which asserts that distorted posttrauma thoughts have an effect on emotions and behaviors. This theory suggests that new information is processed in accordance with existing schemas or that schemas are changed to accommodate new information. Over-accommodation may occur in such a way that schemas about oneself, others, and the world are negatively altered to maintain a sense of control and safety. CPT focuses on the identification, examination, and alteration of maladaptive beliefs maintaining PTSD symptoms, with special attention to how the traumatic event has impacted the individual in the domains of safety, intimacy, power and control, esteem, and trust. Through modifying cognitions, behavioral approach rather than avoidance is facilitated.
Meta-analyses and review articles have identified significant reductions in PTSD symptoms (Bradley et al. 2005), including large effect sizes posttreatment and medium-to-large effect sizes at follow-up compared to controls, with similar effects across both PE and CPT (Powers et al. 2010). Among samples of women, both CPT and PE have been demonstrated as effective (Dossa and Hatem 2012; Resick et al. 2002), with either no differences in effectiveness or treatment completion between men and women or demonstrating better outcomes for women (Mouilso et al. 2015; Walter et al. 2014).
Whereas some common pharmacological treatments for anxiety may have risks for use during pregnancy, evidence indicates psychotherapy is preferred over medication by most pregnant women, and exposure-based treatments are considered safe for use during pregnancy (Arch et al. 2012). Arch et al.’s (2012) review of the literature indicates untreated anxiety disorders likely pose greater risk than even the most intense exposure-based treatments, such as PE, for pregnant women. Both PE and CPT include components that target posttrauma cognitions and appraisals, including those that may affect the woman’s relationship to her infant, across broad themes such as safety (of the infant and the woman herself) and trust (of medical professionals, of other caregivers, or of herself as a caregiver) (Ayers et al. 2007).
The extant research on trauma-focused treatments during pregnancy has consisted of case studies. Although larger-scale research is lacking, results are encouraging. Ayers et al. (2007) reviewed the literature and suggested that although the same treatments are likely to be effective in postnatal PTSD, when a traumatic birth is the index trauma, there may be unique aspects to the presentation such that women may avoid sexual activity, develop a fear of childbirth, have difficulty bonding to the child, or become anxiously attached to the child. They described two case studies on the use of trauma-focused treatment related to traumatic birth which indicate that these treatments can be effective and tailored to the individual, taking into account the woman’s emotions (such as fear or shame) and cognitive reactions to the traumatic event. Another case study of exposure-based PTSD treatment during pregnancy demonstrated effective reduction in treatment without any harm to the mother, developing fetus, or infant (Twohig and O’Donohue 2007). Although limited in scope, these studies suggest exposure-based PTSD treatment during pregnancy is likely safe and effective.
The literature to date has yielded several recommendations for implementing trauma-focused treatment during pregnancy. Turton et al. (2001) advocate referral to treatment when symptoms are demonstrated and, even prophylactically during subsequent pregnancies, as during this time a resurgence of symptoms may occur. Twohig and O’Donohue (2007) advise that when beginning exposure-based treatment with a pregnant woman, the provider should inform the patient of the limited data on trauma-focused treatments during pregnancy as well as the general effectiveness of such treatments and consult with the patient’s physician both prior to initiating treatment and throughout treatment should any health issues arise. Finally, Arch et al. (2012) offer suggestions as to how interoceptive exposure tasks can be modified for use during pregnancy, such as monitoring the pregnant woman’s heart rate when breathing may be affected. Consultation with the patient’s physician as exposure tasks are determined is recommended.
3.5 Affect Regulation and Borderline Personality Disorder Intervention
Many women with trauma histories present for treatment with complicated diagnostic pictures and severe symptoms of chronic affect dysregulation and environmental reactivity, including borderline personality disorder (BPD), a diagnosis that includes symptoms such as chronic suicidal ideation and self-injury. Dialectical behavior therapy (DBT; Linehan 1993) is an intensive treatment for BPD and emotional dysregulation and includes the teaching of skills such as mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness with attention to factors that alleviate dysfunctional behaviors. DBT is typically conducted with a combination of participation in a weekly skills group, weekly individual psychotherapy, and phone coaching, generally for 6 months to a year. Several studies have demonstrated the efficacy of DBT for treatment engagement and in behavioral changes, such as a decrease in suicide attempts and depressive symptoms (see Lynch et al. 2007, for a review). Combined DBT and PE intervention for individuals with PTSD who would benefit from additional skills before beginning trauma-focused treatment has been recently evaluated. The integrated intervention has been found to reduce PTSD symptoms as well as suicidal ideation, depression, anxiety, shame, dissociation, and trauma-related guilt cognitions among women (Harned et al. 2012). Although no known studies have examined the peripartum use of DBT or DBT with PE, Apter-Danon and Candilis-Huisman (2005) assert treatment for BPD should be implemented as early in pregnancy or postpartum as possible. The authors identify pregnancy as a prime point for intervention among women with BPD, given the consequences of poor self-care on the woman and the developing fetus’ health and the fact that the impending birth of a child may be a highly motivating factor for treatment. The authors recommend treatment that incorporates the infant after birth to address infant emotion dysregulation and enhance maternal responsivity.
Conclusions
Resilience and recovery following adversity are the most common posttrauma trajectories. Peripartum social support is one of the most salient identified factors for promoting wellness during and after pregnancy. When clinically relevant difficulties do occur, particular therapeutic processes and interpersonal strategies may promote engagement and recovery. Several interventions that are developed to address depression, PTSD, and affect regulation complaints appear well suited for use in peripartum.
References
Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M (2006) Depression and anxiety during pregnancy and six months postpartum: a follow-up study. Acta Obstet Gynecol Scand 85:937–944
Apter-Danon G, Candilis-Huisman D (2005) A challenge for perinatal psychiatry: therapeutic management of maternal borderline personality disorder and their very young infants. Clin Neuropsychiatr 2:302–314
Arch JJ, Dimidjian S, Chessick CA (2012) Are exposure-based cognitive behavioral therapies safe during pregnancy? Arch Womens Ment Health 15:445–457
Ayers S, McKenzie-McHarg K, Eagle A (2007) Cognitive behaviour therapy for postnatal post-traumatic stress disorder: case studies. J Psychosom Obstet Gynaecol 28:177–184
Bradley R, Greene J, Russ E, Dutra L, Westen D (2005) A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatr 162:214–227
Connor M, Davidson JR (2003) Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 18:76–82
Dossa NI, Hatem M (2012) Cognitive-behavioral therapy versus other PTSD psychotherapies as treatment for women victims of war-related violence: a systematic review. Sci World J 2012:1–9
Foa EB, Hembree EA, Rothbaum BO (2007) Prolonged exposure therapy for PTSD: emotional processing of traumatic experiences, therapist guide (treatments that work). Oxford University, New York, NY
Gotlib IH, Whiffen VE, Wallace PM, Mount JH (1991) Prospective investigation of postpartum depression: factors involved in onset and recovery. J Abnorm Psychol 100:122–132
Harned M, Korslund K, Foa E, Linehan M (2012) Treating PTSD in suicidal and self-injuring women with borderline personality disorder: development and preliminary evaluation of a dialectical behavior therapy prolonged exposure protocol. Behav Res Ther 50:381–386
Harville EW, Xiong X, Buekens P, Pridjian G, Elkind-Hirsch K (2010) Resilience after hurricane Katrina among pregnant and postpartum women. Womens Health Issues 20:20–27
Hughes P, Riches S (2003) Psychological aspects of perinatal loss. Curr Opin Obstet Gynecol 15:107–111
Leahy-Warren P, McCarthy G, Corcoran P (2012) First-time mothers: social support, maternal parental self-efficacy and postnatal depression. J Clin Nurs 21:388–397
Linehan MM (1993) Cognitive behavioral treatment of borderline personality disorder. Guilford Press, New York
Lynch TR, Trost WT, Salsman N, Linehan MM (2007) Dialectical behavior therapy for borderline personality disorder. Annu Rev Clin Psychol 3:181–205
Mouilso ER, Tuerk PW, Schnurr PP, Rauch SA (2015) Addressing the gender gap: prolonged exposure for PTSD in veterans. Psychol Serv 13(3):308–316. doi:10.1037/ser0000040
Muzik M, Ads M, Bonham C, Rosenblum K, Broderick A, Kirk R (2013) Perspectives on trauma-informed care from mothers with a history of childhood maltreatment: a qualitative study. Child Abuse Negl 37:1215–1224
Muzik M, Brier Z, Menke R, Davis MT, Sexton MB (2016) Longitudinal suicidal ideation across 18-months postpartum in mothers with childhood maltreatment histories: temporal trajectories and predictors of risk. J Affect Disord 204:138–145
Muzik M, Umarji R, Sexton MB, Davis MT (2017) Social support buffers the relationships between childhood maltreatment severity, economic adversity and postpartum depressive symptoms. Matern Child Health J 21:1018–1025
O’Hara MW, Stuart S, Gorman LL, Wenzel A (2000) Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 57:1039–1045
Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB (2010) A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clin Psychol Rev 30:635–641
Resick PA, Schnicke MK (1993) Cognitive processing therapy for sexual assault victims: a treatment manual. Sage Publications, Newbury Park
Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA (2002) A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J Consult Clin Psychol 70:867–879
Robertson E, Grace S, Wallington T, Stewart DE (2004) Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry 26:289–295
Sexton MB, Flynn HA, Lancaster C, Marcus S, McDonough S et al (2012) Predictors of recovery from prenatal depressive symptoms from pregnancy through postpartum. J Womens Ment Health 21:43–49
Sexton MB, Hamilton L, McGinnis EW, Rosenblum KL, Muzik M (2015) The roles of resilience and childhood trauma history: main and moderating effects on postpartum maternal mental health and functioning. J Affect Disord 174:562–568
Sockol LE, Epperson CN, Barber JP (2011) A meta-analysis of treatments for perinatal depression. Clin Psychol Rev 31:839–849
Spinelli MB, Endicott J (2003) Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatr 160:555–562
Swanson LM, Flynn H, Adams-Mundy JD, Armitage R, Arnedt JT (2013) An open pilot of cognitive-behavioral therapy for insomnia in women with postpartum depression. Behav Sleep Med 11:297–307
Turton P, Hughes P, Evans CDH, Fainman D (2001) Incidence, correlates, and predictors of posttraumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 178:556–560
Twohig MP, O’Donohue WT (2007) Treatment of posttraumatic stress disorder with exposure therapy during late term pregnancy. Clin Case Stud 6:525–535
Walter KH, Varkovitzky RL, Owens GP, Lewis J, Chard KM (2014) Cognitive processing therapy for veterans with posttraumatic stress disorder: a cross-sectional and longitudinal comparison between outpatient and residential PTSD treatment. J Consult Clin Psychol 82:551–561
Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P (2006) A preventative intervention for pregnant women on public assistance at risk for postpartum depression. Am J Psychiatr 163:1443–1445
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Sexton, M.B., Bennett, D.C., Muzik, M., Rosenblum, K.L. (2018). Resilience, Recovery, and Therapeutic Interventions for Peripartum Women with Histories of Trauma. In: Muzik, M., Rosenblum, K. (eds) Motherhood in the Face of Trauma. Integrating Psychiatry and Primary Care. Springer, Cham. https://doi.org/10.1007/978-3-319-65724-0_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-65724-0_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65722-6
Online ISBN: 978-3-319-65724-0
eBook Packages: MedicineMedicine (R0)