Abstract
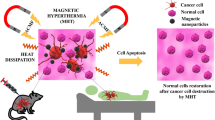
Magnetic hyperthermia (MHT) is heat dissipation in magnetic nanoparticles (MNPs) in an alternating magnetic field (AMF) of hundreds of kHz. This is an alternative method, non-invasive, and appears to be non-toxic compared to the usual methods – chemotherapy and radiotherapy used today in the therapy of malignant tumours – and with great future potential in cancer therapy. For the MHT to be effective in destroying tumour cells the temperature of biocompatible magnetic nanoparticles (Bio-MNPs) in the tumour must reach 42–43 °C, leading to local necrosis. There are many factors that increase the temperature of MNPs, depending on the nanoparticles’ size (NPs) and type, metals or oxides with metallic ions. In this chapter, I will discuss application of metal/oxide magnetic nanoparticles (Me/O-MNPs) in MHT as possible candidates for increasing the hyperthermic efficiency in cancer therapy. I will present the basic physical aspects of MHT, the magnetic properties of Me/O-MNPs with potential use in MHT, the results obtained in vitro and in vivo and future development trends of the MHT technique, such as superparamagnetic hyperthemia (SPMHT), proposed as alternative, non-invasive and non-toxic cancer therapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Metal/oxide magnetic nanoparticles
- Superparamagnetic hyperthermia
- In vitro/in vivo
- Cancer thermotherapy
1 Introduction
Magnetic hyperthermia (MHT) is today one of the most promising alternative methods, that is non-invasive and has low toxicity upon the living organism, and with a great future potential in cancer therapy (Gordon et al. 1979; Pankhurst et al. 2003; Ito et al. 2005a; Kawai et al. 2006; Gazeau et al. 2008; Kobayashi et al. 2014; Datta et al. 2015). The method relies on getting a higher temperature inside the tumor where the magnetic nanoparticles (MNPs) are found, ~43 °C respectively, compared to the normal temperature of the surrounding tissues, by using an external alternating magnetic field (AMF) (Rosensweig 2002; Pankhurst et al. 2003; Hergt et al. 2006). Local heating occurs through the Néel – Brown magnetic relaxation (Néel 1949; Brown 1963; Rosensweig 2002). The high temperatures destroy the tumour cells through apoptosis or even necrosis (up to 45–46 °C) (Prasad et al. 2007; Gazeau et al. 2008). Since Gordon et al. (1979) revealed for the first time in 1979, the hyperthermic magnetic effect on tumour cells through the use of MNPs coated with dextran exposed to an AMF, it has been considered that MHT with nanoparticles (NPs) can be a viable alternative method in cancer therapy compared to chemotherapy and radiotherapy (Gordon et al. 1979). Chemo- and radiotherapy used today to treat cancer are highly toxic, and in many advanced cases these are even inefficient. Therefore, finding an alternative method, which is non-invasive, with a reduced or no toxicity, and more efficient than the current methods is desirable. Even more, the importance of finding better alternatives for cancer therapy is emphasized by the high rates of cancer diagnosis in many European countries.Footnote 1 According to the World Health Organisation findings, cancer is the second leading cause of death globally with an expectancy of 70% increase in deaths over the next two decades.
By using a natural thermal effect instead of chemicals or radiations which are highly destructive for health cells, MHT has the advantage of a very low toxicity rate from the beginning. In addition, under the action of AMF, thermal effects occur only locally, inside only the tumour where are MNPs, and can be controlled by using MNPs without affecting the other surrounding healthy tissue. Moreover, AMF used in MHT has no negative biological effects on healthy tissues, as long as a certain threshold is not passed (Hergt and Dutz 2007). Some MNPs, such as magnetite, are well tolerated by the body (Lacava et al. 1999; Hilger et al. 2003; Naqvi et al. 2010). Furthermore, to eliminate the possible toxicity of the MNPs and to increase their affinity to the tumor cells, they are made biocompatible (Safarik and Safarikova 2002; Kobayashi et al. 2014) by various techniques used in bionanotechnology. Usually, these techniques are used for coating/covering the surface of NPs with a non-toxic organic layer (polymer, non-polymeric or different biological molecules) (Molday and MacKenzie 1982; Portet et al. 2001; Zhang et al. 2002; Berry et al. 2003; Mart et al. 2009; Guandong et al. 2010). Given all this, MHT with MNPs appears to be toxicity free.
However, following hyperthermic effect , MNPs can remain interstitial in the tumour area or in the bloodstream and can possibly migrate towards some organs (liver, spleen, etc.) (Johannsen et al. 2005). Regarding intracellular MNPs in the tumor, those can be eliminated naturally due to their reduced sizes (a few nanometers). These issues and others that can affect the toxicity and efficacy of thermotherapy are taken into account when studying the efficiency of the magnetic method.
Another important aspect of the MHT is finding the most suitable MNPs to get a maximum hyperthermic effect and a reduced toxicity. From this point of view, besides using ferrimagnetic nanoparticles (FiMNPs) of Fe3O4 and γ-Fe2O3 with Fe+2/Fe+3 metallic ions (MeIs), which seem to be most suitable, metallic ferromagnetic nanoparticles (Me-FeMNPs) of small sizes (only a few nm), such as Fe, Co, etc., are also considered for future use in superparamagnetic hyperthermia (SPMHT) . This would greatly increase the hyperthermic effect and ultimately, the efficiency of the method (Zeisbergera et al. 2007; Habib et al. 2008; Mehdaoui et al. 2010a, 2010b; Kappiyoor et al. 2010; McNerny et al. 2010; Wu et al. 2011).
Also, another aspect worthy of attention is the homogenous dispersion and accumulation of MNPs inside tumours. Moreover, if until now the more solid localized tumors were targeted through MHT, being easily accessible by injecting the biocompatible magnetic nanoparticles (Bio-MNPs) suspension directly in the tumour, with the current development of bionanotechnology , also the hidden and harder to reach tumours or extensively metastatic have started to be widely addressed. Through encapsulating NPs in liposomes (LPs) or coating them with a biocompatible layer (Bio-L) and then functionalising the surface (FS) of the NPs (FS-NPs) with molecules/bionanostructures and specific ligands with a high selectivity of tumor cells, and then administer them intravenously, these new techniques become viable alternatives (Shinkai and Ito 2004; Malhi et al. 2013; Le Renard et al. 2010; 2011). As a result of this type of thermotherapy by MHT there are also other advanced effects such as induced anti-tumor immunity (Kobayashi et al. 2014). Bioconjugation/biofunctionalisation the surface of nanoparticles (BioC/BioFS-NPs) with specific antibody (Ito et al. 2005a, b), or by encapsulating the drug/anti-tumor substances in cyclodextrins (CDs) (Fagui et al. 2011; Li et al. 2011; Nigam et al. 2011; Yallapu et al. 2011; Hayashi et al. 2014) with double action (thermal and biochemical) are current approaches in MHT. In vivo results so far have clearly demonstrated tumour regression following MHT therapy (Hergt et al. 1998; Ito et al. 2003a; Johannsen et al. 2005; Tanaka et al. 2005; Hilger et al. 2005) with promising future use in the clinical trial and as alternative method in cancer thermotherapy .
This chapter discusses the MHT with Me-MNPs (FeM) and O-MNPs (FiM) that contain MeIs, and presents some results obtained in vitro and in vivo about the possible use in therapy of malignant tumours. The physical principle of MHT, and in particular, of the SPMHT, which is the best method currently used for obtaining the magnetic hyperthermia effect with a maximum efficiency, will be discussed in detail further on. Also, other aspects of the MHT efficiency and real prospects of using this alternative method in the future cancer therapy will be further addressed.
2 Principle of Magnetic Hyperthermia
2.1 Hyperthermia with Magnetic Nanoparticles
MHT consists in increasing the temperature environment (physical or biological) that contains a magnetic material, metal (FeM) or oxides (generally based on irons) with MeIs (FiM), under the action of an external AMF. In the case of a biological environment, when aiming at destroying tumour cells by using hyperthermic effect (more than the normal value of ~37 °C), the goal is to increase the tissue’s temperature at target values of 42–43 °C.
The magnetic effects that can lead to heating the magnetic material (FeM or FiM) located in an external AMF are: (i) eddy currents that occur through electromagnetic induction in metallic magnetic materials, (ii) magnetic hysteresis, (iii) magnetic relaxation and (iv) magnetic resonance (ferro- or ferrimagnetic). In the case of MNPS, because they are very small (10−7 to 10−9 m) and generally isolated from each other in a suspension, turbionari currents (i) are negligible, even in conductive MNPs (Fe, Ni, Co, etc.).
In addition, for obtaining MHT, the AMFs are used at a frequency of tens – hundreds of kHz. Having in view that the magnetic resonance in a fero- or ferrimagnetic material (FeM when NPs are metals or FiM when NPs are metal oxides) is achieved at much higher frequencies (hundreds of MHz – tens of GHz), MHT can not be generated by magnetic resonance (iv). Only the hysteresis effect (ii) (Pankhurst et al. 2003) and the magnetic relaxation (iii) (Néel 1949; Brown 1963) may produce heat to the material.
Magnetic hysteresis (ii) (Fig. 10.1a is obtained, in general, in the case of large MNPs, that have a structure of magnetic domains (Fig. 10.1b).
Power dissipation per unit of material volume in AMF can be expressed by the formula (Pankhurst et al. 2003)
where f is the frequency of AFM with H magnitude and M is the magnetization of the material. Basically, this power is the surface S of hysteresis loop (Fig. 10.1a) which gives the power dissipated during a hysteresis loop, on a period of time t(t = 1/f) of the magnetic field multiplied by frequency (P = μ 0 fS). When the sample is comprised of MNPs the specific power dissipation is used (Habib et al. 2008)
where ρ is the density of the sample (nanoparticles system). For small amounts of material, such as NPs, it is customary the use of the expression of specific power dissipated in W/g (see Sect. 10.2.2). The loss power in NPs in the form of heat (Q), will lead to their heating. When the MNPs are found in a biological tissue (after previously being made biocompatible with the enviroment), as a result of applying AMF to obtain a temperature increase of the tissue compared to normal value (ex. ~37 °C), the MNPs suffer hyperthermic effect.
However, it was found that the practical use of MHT as an effect of magnetic hysteresis has some drawbacks (Pankhurst et al. 2003). Mainly for getting an efficient heating of a tissue is needed to increases its temperature in a short time and also to reach the necessary value in a MHT. This requires that the hysteresis loop to be as broad and saturaturated as possible, which implies the existence of high fields for magnetization and magnetic saturation . This is hard to have at frequencies of hundreds of kHz. Also, NPs should be large enough and be structured as magnetic domains in order to have a pronounced hysteresis, and/or to have a large magnetic anisotropy. Using large MNPs raises many aspects of the biological toxicity or biocompatibility and transportation at cellular and intracellular level.
Recent research results have shown that MHT would be more effective if instead of large NPs (average diameter of tens of nm), with magnetic domains structure, its would use NPs that are smaller, single-domain and superparamagnetic, with a (mean) diameters in the ~5–25 nm range. In this case, it was found that MNPs can achieve higher power dissipation than using hysteresis losses (Pankhurst et al. 2003; Hergt et al. 1998), and in addition, their toxicity should be lower, due their smaller size. Moreover, small MNPs should be more effective in intracellular therapy (Fortin et al. 2008).
The main feature of MNPs, FeM or FiM, that have a superparamagnetic (SPM) behavior is the lack of hysteresis (Fig. 10.2a). Their magnetization is done by a function of Langevin type (Jacobs and Bean 1963). At the same time, the magnetic domains structure is missing, NPs having a single-domain (Fig. 10.2b) magnetized spontaneously to saturation. In this case, the spontaneous magnetization \( \left({\overrightarrow{M}}_{\mathrm{s}}\right) \) is not stable, but fluctuates along a direction, called the easy magnetization axis (e.m.a.) under the action of thermal activation, a process known as magnetic relaxation, respectively, in this case superparamagnetic relaxation (Néel 1949; Bean and Livingston 1959). The 180° magnetization reversal and the magnetic moment of nanoparticle \( \left(\overrightarrow{m}\right) \) which has volume V, respectively
are done in the Néel magnetic relaxation time (Néel 1949; Aharoni 1964), which has the formula
where KV is the energy barrier for the magnetic moment of NPs, k B T is the thermal energy and τ 0 is a time constant (10−9 s Back et al. 1998). In Eq. 10.4 K is the magnetocrystalline anisotropy constant, which in the simplest case is considered uniaxial, and k B is the Boltzmann constant.
This process of superparamagnetic relaxation in an external AMF leads to a dissipation of energy in the form of heat. Thus, they heat up. This magnetic relaxation effect (iii) in superparamagnetic nanoparticles (SPMNPs) is used in MHT and appears to be more appropriate than the effect given by hysteresis (ii) both in terms of increased power dissipation obtained but also of lower toxicity, due to using smaller nanoparticles. According to some researchers in the field, the SPMHT is considered the future cancer therapy method, more efficient and with almost no toxicity compared with chemo- and radiotherapy, which are used today in treatment of cancer and have a high toxicity and in many cases are inefficient.
2.2 Superparamagnetic Hyperthermia
In an harmonic AMF with amplitude H 0 and frequency f, power (volumetric) dissipated is given by (Rosensweig 2002)
where χ″ is the component of complex magnetic suspectivity, called the loss component. This component is found (Shliomis 1974) as having the form of the Debye equation
where χ 0 is magnetic susceptibility of echilibrum, τ is magnetic relaxation time and ω = 2πf is pulsation.
When NPs are found in colloidal suspensions, magnetic relaxation can occur by two mechanisms, Néel and Brown, and relaxation time will be given by (Néel 1949; Brown 1963; Aharoni 1964)
where τ N is given by Eq. 10.4 and τ B is (Brown 1963)
In Eq. 10.8 η it is the viscosity coefficient of the fluid in which the NPs are dispersed and V h is the hydrodynamic volume of the NPs (Fig. 10.3), which in a spherical nanoparticles approximation model (Fig. 10.3a have the expression
In Eq. 10.9 D is the diameter of the NPs (Fig. 10.3a) and δ is the thickness of the biocompatible coating (Fig. 10.3b), such as dextran, liposomes, cyclodextrins, polymers, etc., depending on biomedical application (Veiseh et al. 2010).
(a) The core-shell model of compatible nanoparticles; (b) (color online) Illustration depicting the assembly of polymers onto the surface of magnetic nanoparticle cores (Reprinted from Veiseh et al. 2010, Copyright (2010), with permission from Elsevier)
Considering Eq. 10.6, the loss power by magnetic relaxation in fluid (Eq. 10.5) will have the formula
In many cases, NPs in biological environments are fixed, or thickness of the Bio-L is quite thick, so the condition is achieved τ B ≫ τ N, and relaxation time τ is reduced to τ N (τ = τ N). This approximation takes place in most practical cases. In this case, the loss power occurs only through Néel relaxation process, as by rotation of the magnetic moments within the MNPs under the action of the AMF.
In the case of different NPs, to be able to compare results, specific loss power is used (Eq. 10.2)
where δ is the density of NPs (δ = m/V, m is the mass).
The formula found (10.11) determines the temperature of heating nanoparticles (∆T), considering the adiabatic system, when entire energy (power) is transformed into heat (Q) in a time period ∆t,
and
respectively, where c is the specific heat of NPs. In studies of magnetic hyperthermia often one will use the heating rate (speed)
which is more suggestive.
3 Superparamagnetic Hypethermia in Cancer Thermotherapy
3.1 Factors That Can Influence the Efficiency of Superparamagnetic Hyperthermia
Given the loss power (Eq. 10.10) and specific loss power (Eq. 10.11) and heating rate (Eq. 10.14), we see that these observables depend on many factors, both specific magnetic nanoparticles (type, size, shape and distribution of MNPs, magnetic anisotropy, magnetic susceptibility, surface thickness of Bio-NPs, interactions between NPs, which can form agglomerates) and suspension in which nanoparticles are dispersed (the concentration of NPs suspension, the viscosity of the fluid, the density of suspension) and an external magnetic field (external magnetic field amplitude and frequency, harmonic AC). In addition, when the suspension of NPs is introduced in a physiological environment (tissue, tumour, blood, fluid, etc.), depending on the biomedical/pharmaceutical application, we must take into account the characteristics of this environment, the interaction with Bio-NPs and the possibility of movement or no movement (fixing) of NPs. All these factors should be considered when the maximum efficiency of the MHT application is pursued.
However, some of these can be considered critic parameters, such as the size of NPs. Besides thess, it quite critical is the magnetic anisotropy of MNPs that can change the power dissipation and heating rate, in order to get a maximum hyperthermic effect, with direct repercussions on the size of NPs to be used in MHT.
To get a clearer picture of the influence these parameters have on the MHT, Fig. 10.4 shows different curves of heating rates ΔT/Δt (Eq. 10.14) for different O-MNPs with Fe2+, Fe3+ and Co2+ metal ions (FiM nanostructures of Fe3O4 (magnetite), γ-Fe2O3 (maghemite), CoFe2O4 (cobalt ferrite) and Ba ferrite) dispersed in teradecane (carrier liquid) (Rosensweig 2002). The heating rates of these nanosystems presents a maximum for each of the values of diameters (sizes) of the NPs, in range of 3–12 nm, bigger being at Fe3O4 and γ-Fe2O3. From the diagrams we can see that a small change in the NPs diameter leads to a high decreases of heating rate (ex. curves 3 and 4). This shows that the diameter of NPs is a critical measure in obtaining the maximum heating rate. Also, magnetic anisotropy of NPs changes significantly the maximum positions (the size of NPs where the maximum is obtained), that are obtained at slightly lower diameters when the magnetic anisotropy is high. For example, this can be observed in the case of barium and cobalt ferrite (curves 1 and 2) compared to magnetite and maghemite (curves 2 and 4). The curves were recorded in the magnetic field H = 71.6 kA/m (H = B/μ 0, B = 0.09 T) and the frequency f of 300 kHz, and the dispersion environment of the NPs had the following characteristics: the volume fraction of the NPs in liquid (ϕ) is 7.1% and the viscosity coefficient of liquid (η) is 0.00235 kgm−1 s−1).
Comparative heating rates for various magnetic solids. 1 Barium ferrite, 2 Cobalt ferrite, 3 Magnetite, 4 Maghemite. ϕ = 0.071, η = 0.00235 kg m−1 s−1, f = 300 kHz, B = 0.09 T, δ = 2 nm (Reprinted from Rosensweig 2002, © (2002), with permission from Elsevier)
In Fig. 10.5 we can properly seen (in a 3D representation) the influence of the external magnetic field (amplitude H and frequency f) and of the mean diameter (<D>) of MNPs (taking into account a distribution of size of NPs in a real dispersion) on the specific loss power (SLP) (Eq. 10.11), in the case of Co ferrite NPs and in the absence of relaxation Brown (when the viscosity of the fluid is high or NPs are fixed), and when the magnetic susceptibility of equilibrium (χ 0) is constant (Caizer 2010). For the magnetic field were considered the following values of 10–30 kA/m and the variable parameters, frequency (f) and mean diameter (<D>) in the ranges of 100–500 kHz, and 4–7 nm, respectively. The study was done in a biological tissue without cellular damage by magnetic field (amplitude and frequency) (Hergt and Dutz 2007)
(Color online) 3D SLP for cobalt ferrite nanoparticles as a function of f and <D>; (a) 10 kAm−1 and (b) 30 kAm−1 (Reprinted from Caizer 2010, © (2010), with permission from West University Publising House)
One such study done with a professional software, optimizes MHT (finding the conditions to specify the highest specific loss power for a particular nanosystem) study required both prior to the experiments in vitro and in vivo, and during these tests.
The purpose of my study is the possible future use of Co ferrite NPs encapsulated in LPs, with a SPM behavior in an external magnetic field of up to 150 kA/m (Fig. 10.6), in the therapy of malignant tumors. The curve was recorded for concentrations of 20 mg/ml of liposomal suspension of nanoparticles (magnetoliposomes in distilled water). Due to the LPs sizes (>100 nm), Brown relaxation (Eq. 10.8) has been neglected, losses taking place during Néel relaxation processes (Eq. 10.4), in the low field of 10–30 kA/m. An important finding of this study is that the high specific loss power is achieved at a lower mean diameter of Co ferrite NPs. This result leads to the idea that these NPs that would be suitable for use in intracellular therapy (Jordan et al. 1999a; Fortin et al. 2008) of hyperthermia may destroy tumour cells more effectively within them.
(Color online) magnetisation of CoFe2O4 nanoparticles encapsulated in liposomes (Reprinted from Caizer 2010, © (2010), with permission from West University Publising House)
An excellent review, where the influence of other parameters on the SPMHT can be observed, is found in Gazeau et al. (2008). For example, the viscosity of fluid or the large dispersion of the MNPs that always exists in a real nanosystems, can substantially affect the SPMHT (Rosensweig 2002). In the case of the large dispersion of NPs we must consider the distribution function of the sizes (diameters) of nanoparticles. Experimentally, in most cases, it was found that the nanoparticle size distribution can be approximated by a lognormal function (Bacri et al. 1986; O’Grady and Bradbury 1994; Caizer 2003)
where D is the diameter of the NPs (Fig. 10.3) (in spherical nanoparticles approximation, for example) and d and σ are the distribution parameters. In this case, the mean diameter of the NPs will be (Baker et al. 2006)
Given such ditribution , and the Eqs. 10.10 and 10.11, mean specific loss power in this case is calculated by formula
In order to have a small influence of the NPs sizes over the power dissipated, is important to aims at achieving this by various methods used in obtaining nanoparticle systems with more narrow distributions. However, in real terms this condition often is difficult, and the formula (10.18) should be applied for assessing the correct loss power.
3.2 Superparamagnetic Hyperthermia with Metal Magnetic Nanoparticles
While aiming at increasing the loss power in a short time in a system of MNPs and given the theoretical and experimental results regarding the SPMHT, and other results and recent studies (Baker et al. 2006; Lee et al. 2007; Ondeck et al. 2009; Purushotham and Ramanujan 2010), an alternative route is considered in order to achieve the desired results. In order to reduce the side effects of toxicity on normal cells surrounding the tumour cells targeted through MHT, the use of metallic superparamagnetic nanoparticles (Me-SPMNPs) is used instead of those oxides that are limited (Kappiyoor et al. 2010).
Me-MNPs that are FeM would bring additional benefits in SPMHT compared to the oxides, primarily by strong increase in power dissipated due to the high magnetic moment (Eq. 10.3) and the high susceptibility of FeMNPs, which can be tens – hundreds of times higher than the FiM oxides (ferrites). In addition, the magnetic anisotropy of FeM metals such as Fe, Co, brings other advantages due its generally higher values than iron-based FiM oxides, such as Fe3O4 or γ-Fe2O3, the most suitable and used in experiments of SPMHT. This makes the maximum power dissipated in SPMHT (Eq. 10.10) to be achieved at smaller sizes of NPs, which makes FeM more suitable for use in therapy of intracellular magnetic hyperthermia (Fortin et al. 2008). Me-FeMNPs are smaller than FiM oxides, and thus will have less effect on cell toxicity. Moreover, smaller NPs can easily get inside cells by active transportation mechanisms, making them more efficient in terms of effects of MHT. In addition, even using various biocompatible surfactants the hydrodynamic volume (diameter) (Fig. 10.3 and Eq. 10.9) will be smaller, thus facilitating both relaxation mechanisms in MHT and transportation mechanisms of biocompatible NPs to the target biological tissue.
The result shown in Fig. 10.7 is very suggestive in this regard. It can be observed very clearly that the loss power in Me-FeMNPs of Fe or Co is noticeably higher than in the case of O-FiMNPs of Fe3O4 or γ-Fe2O3. In addition, the diameter of Me-MNPs where can achieve the maximum power is approx. two times lower than that of the O-MNPs, being about 10 nm, aspect benefit for SPMHT. Another important issue when using Me-FeMNPs in SPMHT is also their usage as metal alloys, which gives the possibility of obtaining a magnetic anisotropy adjustable depending on the concentration of one or other of the chemicals used (ex. FeCo). This allows a modification of Me-MNPs size in a fairly wide range without the power dissipation having to change too much, which is great for SPMHT.
(Color online) volumetric power loss for various magnetic materials at 300 kHz and 50 mT ac field in aqueous dispersion with 10% particle concentration (Reprinted from Habib et al. 2008, with the permission of AIP Publishing)
In addition, the limitation imposed by Eq. 10.15 could be easily met in Me-FeMNPs by the real possibility of using a magnetic field with amplitude or frequency reduced, and that will lead to the same hyperthermic effect as when iron O-MNPs are used.
Given the above advantages, preparation of colloidal suspensions of Me-FeMNPs based on Fe and Co, and their use in SPMHT, has already caught scientist’s attention (Zhang et al. 2003; Mendoza-Resendez et al. 2004; Hutten et al. 2005; Hergt et al. 2006; Zeisbergera et al. 2007; Habib et al. 2008; Mehdaoui et al. 2010a, b; Kappiyoor et al. 2010; McNerny et al. 2010; Wu et al. 2011).
In Fig. 10.8 I have a 3D computational result of a study that we did in the case of Me-MNPs of Fe as a possible use of their SPMHT. The study was aimed at finding optimal diameter of the NPs (considered as spherical) that gives the highest specific loss power, starting from simulating real conditions (considering the iron magnetic characteristics, a magnetic packing fraction (volumetric) of 10%, and NPs fixed in the future tissue (neglecting the Brown relaxation processes)). The result is surprising, because one can get a fairly high specific power dissipation even at low H and f (i.e., H < 40 kA/m and f < 100 kHz), making these MNPs very suitable for SPMHT.
Similar results were obtained by other authors. Mehdaoui et al. (2010a) reported MHT for iron FeMNPs with cubic shape and sizes of 11 nm and 16 nm, where they obtained a specific loss power (SAR – specific absortion rate) of 1,690 W/g in a magnetic field of 66 mT (~53 kA/m). This power exceeds that one reported in other nanosystems. In Fig. 10.9 SAR is shown for the two samples studied.
Magnetic field dependence of SAR at 300 kHz for the two samples (Reprinted from Mehdaoui et al. 2010a, Copyright (2010), with permission from Elsevier)
However, reduced biocompatibility compared to NPs of the iron oxide is a major issue when it comes to their use in SPMHT in tumors. If the problem of biocompatibility and stability of suspensions of Me-MNPs in aqueous solution will be solved the Me-FeMNPs would be used successfully in SPMHT instead of O-FiMNPs ones, this leading to greater efficiency of the hyperthermic method. The problem of biocompatibility and using oxide/metal NPs in MHT studies in vitro and in vivo will be discussed in the next section.
In this respect, a first step in reducing the toxicity of Me-FeMNPs on healthy tissues could be done by reducing from the start their concentrations in the tissue, respectively the volume fraction of magnetic material in suspension. Because of this there is an additional reserve of loss power that would be obtained in the case of Me-MNPs, compared with the oxide ones. Depending on the application targeted for using MHT, it is beyond doubt that we must find the most suitable organic compounds, in order to obtain a good biocompatibility of Me-MNPs, so they can then be used in SPMHT.
Overall, it is observed that FiMNPs of iron oxide, such as Fe3O4 and γ-Fe2O3, are regarded today as the most suitable for use in MHT. A special attention should be paid to nanoparticle-based metallic iron, e.g. Fe or Co metal, that increases the power dissipated. In a good biocompatible that can be achieved, they could be used successfully and with high efficiency in SPMHT of tumours.
3.3 Biocompatibility of Magnetic Nanoparticles for Cancer Therapy by Magnetic Hyperthermia
One of the most important issues in the application of MHT is avoiding possible toxicity on healthy tissue, which can be caused by the MHT or mostly by the used MNPs. Damage to healthy tissue by a magnetic field can be avoided by using AMF with low amplitudes and frequencies, so that the conditions in Eq. 10.15 are respected. Also, the temperature achieved by the magnetic field must be maintained at around ~43 °C with the effect of inducing apoptosis and necrosis in the tumour tissue, this being controlled by external electronic devices. Only in some cases, the temperature of localized tumors may be slightly higher in the tumor (44–46 °C), healthy tissue being unaffected, warming taking place only on the tumour in which there are MNPs.
It only remains that the NPs that mediate hyperthermia to be biocompatible with the tissues where they are to be introduced. In this direction, since the question of using MNPs in MHT, various methods/techniques were developed for making Bio-MNPs using different agents (polymeric, no-polymeric, biological molecules) coating/covering surface nanoparticles (surfacted, BioC, BioFS, etc.) or encapsulating NPs in different mebranes/biological nanostructures, creating hybrid bionanostructures core-shell (magnetic core and biocompatible biological shell (Molday and MacKenzie 1982; Portet et al. 2001; Safarik and Safarikova 2002; Zhang et al. 2002; Berry et al. 2003; Mart et al. 2009; Guandong et al. 2010 Kobayashi et al. 2014). A synthesis of these and highlighting MNPs used in MHT was made recently by Kobayashi et al. (2014). In Table 10.1 these are summarized (with permission from Kobayashi et al. 2014).
Current trends are in favour of BioC of the surface of MNPs with different specific molecular nanostructures, antibodies or by inducing through MHT an immune response to specific proteins to stimulate the antitumoral immunity (heat shock protein (HSP) – mediated antitumor Immunity), which would make MHT possible even in tumour metastasis (Schlesinger 1990; Ito et al. 2005a). In Fig. 10.10 the BioC of LPs containing magnetite NPs with antibody G250 for targeting active tumor cells is shown.
Antibody-conjugated magnetoliposomes (AMLs) for active targeting. Magnetite nanoparticles were wrapped in a neutral liposome, and a G250 antibody was covalently linked to the liposomal surface (Reprinted from Ito et al. 2005a, Copyright (2005) The Society for Biotechnology Japan, with permission from Elsevier)
Another way, which I have in mind as a possible biocompatibilization of MNPs for cancer therapy through MHT, is through the use of CDs. We can use CDs to decorate the surface of NPs, which could lead to increase in the overall efficiency of the method while minimizing cell toxicity (Fagui et al. 2011; Li et al. 2011; Nigam et al. 2011; Yallapu et al. 2011; Hayashi et al. 2014; Caizer 2014). CDs are fully biocompatible (are natural polysaccharides) being used today in pharmacy and medicine to deliver controlled release drug carriers (Pradhan et al. 2007; Bellia et al. 2009). These form the toroidal cavity guest host for the drugs that can be encapsulated in hydrophobic cavities. CDs are well dispersed in an aqueous solution. Of these, γ-CDs are most stable in aqueous solution and are more suitable for bioconjugation surface of MNPs using chemical agents.
In a recent study, the specific absorption rate in biocompatible Fe3O4 NPs monodispersed in an aqueous solution, suitable for MHT, is still being shown (Caizer 2014). The some results are presents below (republished with permission from CCL-IOP Publishing).
“Data used in calculations, according to the formulas in Sect. 10.2, are given in Table 10.2. I considered two cases: (i) Fe3O4 encapsulated in LPs and (ii) Fe3O4 bioconjugated with CDs, strategy currently used in research on targeted therapy.
When the NPs are encapsulated in LPs (i), Brown relaxation time becomes much higher than the Néel relaxation time (τ B(167 × 103 ns) ≫ τ N(122 ns)), and the relaxation time will be: τ = τ N/(1 + τ N/τ B) ≅ τ N (see Sect. 10.2.2). In this case the SAR diagram obtained is similar to that in Fig. 10.5, these being determined only by the Néel dissipation processes.
The results for Fe3O4-CDs are shown in Fig. 10.11 for two values of the magnetic field, considering biological accessibility limit, Hf ≤ 5 × 109 Am−1 Hz (Hergt and Dutz 2007). In this case, two magnetic relaxation processes contribute to the SAR, both Néel and Brown, for magnetic diameters greater than 15 nm. Néel relaxation processes become dominant with the increasing frequency to the upper limit at the ~15.5–17 nm. At lower frequencies, such as 150 kHz, contributions to the SAR of the Néel and Brown relaxation processes become comparable and at the frequency of 100 kHz, Brown relaxation prevail, especially in large diameters. When the magnetic field reaches to 20 kA/m (Fig. 10.11b), the highest maximum of SAR increases significantly from ~15 W/g to about ~38 W/g, at the biological limit, for the 17 nm diameter. In this case, the SAR still remains high (~30 W/g) for D > 22 nm, due to Brown relaxation.
(Color online) 3D diagram of SAR until the biological limit in the case of Fe3O4 nanoparticles bioconjugated with CDs, for magnetic field amplitude of (a) 10 kA/m and (b) 20 kA/m (Caizer 2014) (CCL 2014, IOP Publishing. Reproduced by permission of CCL-IOP Publishing)
In conclusion, the 3D study allowed us to optimize SPMHT, in order to apply it in practice: by finding the most suitable bionanoparticles, as material and size, and also as magnetic field parameters (f, H), in order to obtain the highest SAR within the biological accepted limit.”
3.4 Main Results Obtained in Cancer Therapy by Using Superparamagnetic Hyperthermia
The results obtained so far, both in vitro and in vivo, have demonstrated to viability of the MHT method (Ito et al. 2003a; Johannsen et al. 2005; Tanaka et al. 2005; Hilger et al. 2005).
For example, Johannsen et al. (2005) demonstrated an in vivo experiment for treatment of prostate cancer done by means of MHT, using a magnetic fluid. In experiment 48 mice were used which had induced prostate cancer. The mice were injected once with a ferrofluid in the tumour, after which they were subjected to two MHT treatments. Ferrofluid was injected into the tumor at a rate of 0.5 ml/cm3. It was performed with a ferrofluid of magnetite particles in water, which were surfacted with aminosilane, having a mean diameter of 15 nm and a concentration in water of 120 mg/ml. The MHT treatment was made by applying a magnetic field with an amplitude between 0 and 18 kA/m, at a frequency of 100 kHz. The obtained results showed that the magnetic fluid hiperthermia (MFH) treatment leads to inhibition of tumour growth by 44–51%.
Other experiments (Jordan et al. 1999b; Ito et al. 2003a; 2004; Ito et al. 2003b; Hilger et al. 2005; Sunderland et al. 2006; Baldi et al. 2007; Johannsen et al. 2007a) emphasize the viability of the MHT method and the possibility of applying them successfully in the not too distant future for the treatment of various cancers. Ito et al. (2003a) showed the complete regression of mammary carcinoma by repeating MHT with magnetite nanoparticles.
A synthesis of tumour regression results obtained by applying MHT and the conditions used are shown in Fig. 10.12 and in the text of Figure (Gazeau et al. 2008) based on the works of authors: Ito et al. (2003a, 2005a) and Kawai et al. (2006) for Fig. 10.12a; Jordan et al. (2006) for Fig. 10.12b. Important results have been obtained at animals with breast cancer, prostate cancer, brain cancer, renal cancer and melanoma.
(Color online) examples of tumor regression following magnetic hyperthermia. (a) Complete regression of mouse mammary carcinoma by frequent repeated hyperthermia using magnetic cationic liposomes. (i) Magnetite nanoparticles were embedded into cationic liposomes (MCLs) and injected directly into 15-mm tumors, which were induced subcutaneously in mice. (ii) Alternating magnetic field (AMF) of frequency 118 kHz was generated by a horizontal coil, where the mouse was placed. (iii) Temperatures in the rectum and at the surface of the tumor were recorded with an optical fiber probe during AMF exposure. For each irradiation AMF, the tumor was heated to 45 °C for 30 min by controlling the AMF intensity. (iv) The therapeutic effect of tumor irradiation. MCLs were injected directly into 15-mm diameter tumors (2 mg magnetite). Tumors were irradiated for 30 min, repetitively (one to six rounds). Compared with control (blue lines), the tumor growth was stopped after AMF irradiation (red lines). Each line represent a single tumor (n = 5 for both control and treated mice). After repeated hyperthermia, complete regression of the tumor was observed. (v) Percentage of survival for the same group of mice. Control mice: full circles; treated mice: open circles. All the treated mice survived for 120 days after treatment, with no regrowth of the tumor (Adapted with permission from Ito et al. 2003a, 2005a; Kawai et al. 2006). (b) Effect of magnetic hyperthermia on rat malignant glioma. (i) Tumors were induced by implantation of rat glioma RG-2-cells into the brains of rats and were visualized by MRI (T1-weighted MR image). (ii) Magnetic nanoparticles with two different coatings and sizes were administered in to the tumors by stereotactic injection (20 μl at 2 mol/l iron concentration). AMF (100 kHz, 0–18 kA/m) was generated using an applicator system (MFH 12-TS®, MagForce Nanotechnology, Germany). Temperature into the tumor was measured using a fiber optic thermometry device. Although the rectum temperature did not increase by more than 1 °C, tumors injected were heated up to 45 °C (10 °C increase). (iii) Prussian blue staining of the tumor after thermotherapy treatment: the injection of the aminosilane-coated particles led to the formation of stable deposit into the tumor: the nanoparticles (in blue) were still distributed throughout the tumor after treatment. (iv) Effect of treatment temperature on the survival rate after thermotherapy (one round, 30 min). Intratumoral temperature greater than 43 °C significantly increased the lifespan of tumor-bearing rats compared with nontreated controls (survival fraction null at days 8–13, data not shown). The gain of survival was correlated with the intratumoral temperature (Adapted with permission from Jordan et al. 2006). MCL magnetic cationic liposomes. (Republished with permission of Future Medicine Ltd., from Gazeau et al. 2008; permission conveyed through Copyright Clearance Center, Inc)
In the most advanced MHT state reached today even in the preclinical phase (clinical trial) (in Germany) (Gazeau et al. 2008) for non-invasive treatment of prostate cancer (Johannsen et al. 2007a, b, c) and glioblastoma (Maier-Hauff et al. 2007; Jordan and Maier-Hauff 2007) by intratumoral injection of suspension of Bio-MNPs and control by computed tomography (CT) and medical resonance imaging (MRI), with good results. These treatments, when applicable, are combined with radiation therapy to increase the effectiveness of irreversible destruction of malignant tumours.
Although many results attest to the viability of the method of SPMHT, there are many aspects still to be clarified before this method can be applied clinically, with maximum effectiveness against tumors (complete destruction and irreversibly against tumors) without side effects and without a longer need for radiotherapy . Concerning the characteristics of the magnetic field, things are quite clear, and in terms of MNPs best suited for hyperthermia, it is still necessary here to optimize. The current efforts of researchers in the field are focused heavily on bionanostructures from the surface of MNPs, which give them specific properties for targeting tumor cells and are mediators of MHT. Furthermore, the suspension of suitable Bio-MNPs must be injected into the blood vessel of hidden tumours, inaccessible from the outside. All these could result in future MHT in advanced stages of cancer, metastases, or even cancer detection in early stages (Levy et al. 2010). In addition, it is considered that MHT method combining with others, such as chimioterapy, genetherapy, micro-RNA (Yin et al. 2014) etc., lead to an increase in efficiency of destroying tumorus cells.
4 Conclusions
MHT, and in particular, SPMHT based on temperature increase in a tissue at ~43 °C by Néel – Brown relaxation in SPMNPs that are biocompatible and injected inside, it has a great potential for future use in cancer therapy. According to the results obtained so far in vitro and in vivo, and recently even in clinical trial in the treatment of prostate cancer and glioblastoma, the chances of using MHT in the not so far future are promising. SPMHT is a advanced stage of the alternative cancer therapy, non-invasive and with very low toxicity compared to chemotherapy and radiotherapy, which are highly toxic and sometimes in advanced stages of cancer are ineffective. SPMHT efficiency depends on: (i) using SPMNPs best suited for this experiment (type, size, size distribution, magnetic anisotropy, etc.), (ii) AMF parameters and how to apply it on tumours (amplitude, frequency, time of exposure, temperature control, etc.), (iii) biological nanostructures coating of SPMNPs to make them biocompatible with the tissue and increase their affinity to targeted tumor cells. A future perspective of increasing the loss power in specific tumours in a short time and reduce the side effects on healthy cells, is also an avantage resulting from using SPMNPs of FeM metals instead of FiM oxides. While the first two issues (i) and (ii) are well developed and addressed in the contemporary research, the third issue (iii) has high development potential.
Future advances in bionanotehnology and finding chemical agents most suitable for coating the MNPs with high specificity and affinity for different target tumors, opens real prospects for the SPMHT method to become, in the not too distant future, an alternative method, non-invasive, the most effective in cancer therapy.
Notes
- 1.
World Cancer Research Fund International, Data for Cancer Frequency by Country, accessed at http://www.wcrf.org/int/cancer-facts-figures/data-cancer-frequency-country.
Abbreviations
- AMF:
-
Alternating magnetic field
- BioC:
-
Bioconjugation
- BioFS:
-
Biofunctionalised surface
- BioFS-NPs:
-
Nanoparticles with biofunctionased surface
- Bio-L:
-
Biocompatible layer
- Bio-MNPs:
-
Biocompatible magnetic nanoparticles
- CDs:
-
Cyclodextrins
- FeM:
-
Ferromagnetic
- FeMNPs:
-
Ferromagnetic nanoparticles
- FiM:
-
Ferrimagnetic
- FiMNPs:
-
Ferrimagnetic nanoparticles
- FS:
-
Functionalised surface
- FS-NPs:
-
Nanoparticles with functionalised surface
- LPs:
-
Liposomes
- MeIs:
-
Metallic ions
- Me-MNPs:
-
Matallic magnetic nanoparticles
- Me-FeMNPs:
-
Metallic ferromagnetic nanoparticles
- Me-SPMNPs:
-
Metallic superparamagnetic nanoparticles
- MFHT:
-
Magnetic fluid hyperthermia
- MHT:
-
Magnetic hyperthermia
- MNPs:
-
Magnetic nanoparticles
- NPs:
-
Nanoparticles
- O-FiMNPs:
-
Oxide ferrimagnetic nanoparticles
- O-MNPs:
-
Oxide magnetic nanoparticles
- SAR:
-
Specific absortion rate
- SPM:
-
Superparamagnetic
- SPMHT:
-
Superparamagnetic hiperthermia
- SPMNPs:
-
Superparmagnetic nanoparticles
References
Aharoni A. Thermal agitation of single domain particles. Phys Rev A. 1964;135:447–9.
Back CH, Weller D, Heidmann J, Mauri D, Guarisco D, Garwin EL, Siegmann HC. Magnetization reversal in ultrashort magnetic field pulses. Phys Rev Lett. 1998;81:3251.
Bacri JC, Perzinski R, Salin D, Cabuil V, Massart R. Magnetic colloidal properties of ionic ferrofluids. J Magn Magn Mater. 1986;62:36–46.
Baker I, Zeng Q, Li W, Sullivan CR. Heat deposition in iron oxide and iron nanoparticles for localized hyperthermia. J Appl Phys. 2006;99:08H106–08H106-3.
Baldi G, Bonacchi D, Innocenti C, Lorenzi G, Sangregorio C. Cobalt ferrite nanoparticles: the control of the particle size and surface state and their effects on magnetic properties. J Magn Magn Mater. 2007;311:10–16.
Bean CP, Livingston LD. Superparamagnetism. J Appl Phys. 1959;30:S120–9.
Bellia F, La Mendola D, Pedone C, Rizzarelli E, Saviano M, Vecchio G. Selectively functionalized cyclodextrins and their metal complexes. Chem Soc Rev. 2009;38:2756–81.
Berry CC, Wells S, Charles S, Curtis ASG. Dextran and albumin derivatised iron oxide nanoparticles: influence on fibroblasts in vitro. Biomaterials. 2003;24:4551–7.
Brown WF Jr. Thermal fluctuations of a single-domain particle. Phys Rev. 1963;130:1677–86.
Caizer C. T2 law for magnetite-based ferrofluids. J Phys Condens Matter. 2003;15:765–76.
Caizer C. Nano-biomagnetism. West University of Timisoara, Timisoara; 2010
Caizer C. Computational study on superparamagnetic hyperthermia with biocompatible SPIONs to destroy the cancer cells. J Phys Conf Ser. 2014;521:012015–4.
Datta NR, Ordóńez SG, Gaipl US, Paulides MM, Crezee H, Gellermann J, Marder D, Puric E, Bodis S. Local hyperthermia combined with radiotherapy and-/or chemotherapy: recent advances and promises for the future. Cancer Treat Rev. 2015;41:742–53.
Fagui A, Dalmas F, Lorthioir C, Wintgens V, Volet G, Amiel C. Well-defined core-shell nanoparticles containing cyclodextrin in the shell: a comprehensive study. Polymer. 2011;52:3752–61.
Fortin JP, Gazeau F, Wilhelm C. Intracellular heating of living cells through Néel relaxation of magnetic nanoparticles. Eur Biophys J. 2008;37:223–8.
Gazeau F, Lévy M, Wilhelm C. Optimizing magnetic nanoparticle design for nanothermotherapy. Nanomedicine. 2008;3:831–44.
Gordon RT, Hines JR, Gordon D. Intracellular hyperthermia. A biophysical approach to cancer treatment via intracellular temperature and biophysical alterations. Med Hypotheses. 1979;5:83–102.
Guandong Z, Yifeng L, Baker I. Surface engineering of core/shell iron/iron oxide nanoparticles from microemulsions for hyperthermia. Mater Sci Eng C. 2010;30:92–7.
Habib AH, Ondeck CL, Chaudhary P, Bockstaller MR, McHenry ME. Evaluation of iron-cobalt/ferrite core-shell nanoparticles for cancer thermotherapy. J Appl Phys. 2008;103:07A307–07A307-3.
Hayashi K, Nakamura M, Miki H, Ozaki S, Abe M, Matsumoto T, Sakamoto W, Yogo T, Ishimura K. Magnetically responsive smart nanoparticles for cancer treatment with a combination of magnetic hyperthermia and remote-control drug release. Theranostics. 2014;4:834–44.
Hergt R, Dutz S. Magnetic particle hyperthermia – biophysical limitations of a visionary tumour therapy. J Magn Magn Mater. 2007;311:187–92.
Hergt R, Andra W, d’Ambly C, Hilger I, Kaiser W, Richter U, Schmidt H. Physical limits of hyperthermia using magnetite fine particles. IEEE Trans Magn. 1998;34:3745–54.
Hergt R, Dutz S, Muller R, Zeisberger M. Magnetic particle hyperthermia: nanoparticle magnetism and materials development for cancer therapy. J Phys Condens Matter. 2006;18:S2919–34.
Hilger I, Fruhauf S, Linss W, Hiergeist R, Andra W, Hergt R, Kaiser WA. Cytotoxicity of selected magnetic fluids on human adenocarcinoma cells. J Magn Magn Mater. 2003;261:7–12.
Hilger I, Hergt R, Kaiser WA. Towards breast cancer treatment by magnetic heating. J Magn Magn Mater. 2005;293:314–9.
Hutten A, Sudfeld D, Ennen I, Reiss G, Wojczykowski K, Jutzi P. Ferromagnetic FeCo nanoparticles for biotechnology. J Magn Magn Mater. 2005;293:93–101.
Ito A, Tanaka K, Honda H, Abe S, Yamaguchi H, Kobayaschi T. Complete regression of mouse mammary carcinoma with a size greater than 15 mm by frequent repeated hyperthermia using magnetite nanoparticles. J Biosci Bioeng. 2003a;96:364–9.
Ito A, Matsuoka F, Honda H, Kobayashi T. Heat shock protein 70 gene therapy combined with hyperthermia using magnetic nanoparticles. Cancer Gene Ther. 2003b;10:918–25.
Ito A, Kuga Y, Honda H, Kikkawa H, Horiuchi A, Watanabe Y, Kobayashi T. Magnetite nanoparticle-loaded anti-HER2 immunoliposomes for combination of antibody therapy with hyperthermia. Cancer Lett. 2004;212:167–75.
Ito A, Shinkai M, Honda H, Kobayashi T. Medical application of functionalized magnetic nanoparticles. J Biosci Bioeng. 2005a;100:1–11.
Ito A, Ino K, Kobayashi T, Honda H. The effect of RGD peptide-conjugated magnetite cationic liposomes on cell growth and cell sheet harvesting. Biomaterials. 2005b;26:6185–93.
Jacobs IS, Bean CP. Fine particles, thin films and exchange anisotropy. In: Rado GT, Suhl H, editors. Magnetism, vol. III. New York: Academic; 1963. p. 271–350.
Johannsen M, Thiesen B, Jordan A, Taymoorian K, Gneveckow U, Waldofner N. Magnetic fluid hyperthermia (MFH) reduces prostate cancer growth in the orthotopic Dunning R3327 rat model. Prostate. 2005;64:283–92.
Johannsen M, Gneveckow U, Thiesen B, Taymoorian K, Cho CH, Waldofner N, Scholz R, Jordan A, Loening SA, Wust P. Thermotherapy of prostate cancer using magnetic nanoparticles: feasibility, imaging, and three-dimensional temperature distribution. Eur Urol. 2007a;52:1653–62.
Johannsen M, Gneveckow U, Taymoorian K, Thiesen B, Waldöfner N, Scholz R, Jung K, Jordan A, Wust P, Loening SA. Morbidity and quality of life during thermotherapy using magnetic nanoparticles in locally recurrent prostate cancer: results of a prospective phase I trial. Int J Hyperth. 2007b;23:315–23.
Johannsen M, Gneveckow U, Taymoorian K, Cho CH, Thiesen B, Scholz R, Waldöfner N, Loening SA, Wust P, Jordan A. Thermal therapy of prostate cancer using magnetic nanoparticles. Actas Urol Esp. 2007c;31:660–7.
Jordan A, Maier-Hauff K. Magnetic nanoparticles for intracranial thermotherapy. J Nanosci Nanotechnol. 2007;7:4604–6.
Jordan A, Scholz R, Wust P, Schirra H, Schiestel T, Schmidt H, Felix RJ. Endocytosis of dextran and silan-coated magnetite nanoparticles and the effect of intracellular hyperthermia on human mammary carcinoma cells in vitro. J Magn Magn Mater. 1999a;194:185–96.
Jordan A, Scholz R, Wust P, Fähling H, Felix R. Magnetic fluid hyperthermia (MFH): cancer treatment with AC magnetic field induced excitation of biocompatible superparamagnetic nanoparticles. J Magn Magn Mater. 1999b;201:413–9.
Jordan A, Scholz R, Maier-Hauff K, Landeghem FKH, Waldoefner N, Teichgraeber U, Pinkernelle J, Bruhn H, Neumann F, Thiesen B, Deimling A, Felix R. The effect of thermotherapy using magnetic nanoparticles on rat malignant glioma. J Neuro-Oncol. 2006;78:7–14.
Kappiyoor R, Liangruksa M, Ganguly R, Puri IK. The effects of magnetic nanoparticle properties on magnetic fluid hyperthermia. J Appl Phys. 2010;108:094702.
Kawai N, Ito A, Nakahara Y, Honda H, Kobayashi T, Futakuchi M, Shirai T, Tozawa K, Kohri K. Complete regression of experimental prostate cancer in nude mice by repeated hyperthermia using magnetite cationic liposomes and a newly developed solenoid containing a ferrite core. Prostate. 2006;66:718–27.
Kobayashi T, Kakimi K, Nakayama E, Jimbow K. Antitumor immunity by magnetic nanoparticle-mediated hyperthermia. Nanomedicine. 2014;9:1715–26.
Lacava ZGM, Azevedo RB, Martins EV, Lacava LM, Freitas MLL, Garcia VAP, Rebula CA, Lemos APC, Sousa MH, Tourinho FA, Da Silva MF, Morais PC. Biological effects of magnetic fluids: toxicity studies. J Magn Magn Mater. 1999;201:431–4.
Le Renard PE, Jordan O, Faes A, Petri-Fink A, Hofmann H, Rufenacht D, Bosman F, Buchegger F, Doelker E. The in vivo performance of magnetic particle-loaded injectable, in situ gelling, carriers for the delivery of local hyperthermia. Biomaterials. 2010;31:691–705.
Le Renard PE, Lortz R, Senatore C, Rapin JP, Buchegger F, Petri-Fink A, Hofmann H, Doelker E, Jordan O. Magnetic and in vitro heating properties of implants formed in situ from injectable formulations and containing superparamagnetic iron oxide nanoparticles (SPIONs) embedded in silica microparticles for magnetically induced local hyperthermia. J Magn Magn Mater. 2011;323:1054–63.
Lee SW, Bae S, Takemura Y, Shim I-B, Kim TM, Kim J, Lee HJ, Zurn S, Kim CS. Self-heating characteristics of cobalt ferrite nanoparticles for hyperthermia application. J Magn Magn Mater. 2007;310:2868–70.
Levy A, Dayan A, Ben-David M, Gannot I. A new thermography-based approach to early detection of cancer utilizing magnetic nanoparticles theory simulation and in vitro validation. Nanomedicine. 2010;6:786–96.
Li R, Liu S, Zhao J, Otsuka H, Takahara A. Preparation of superparamagnetic β-cyclodextrin-functionalized composite nanoparticles with core–shell structures. Polym Bull. 2011;66:1125–36.
Maier-Hauff K, Rothe R, Scholz R, Gneveckow U, Wust P, Thiesen B, Feussner A, Deimling A, Waldoefner N, Felix R, Jordan A. Intracranial thermotherapy using magnetic nanoparticles combined with external beam radiotherapy: results of a feasibility study on patients with glioblastoma multiforme. J Neuro-Oncol. 2007;81:53–60.
Malhi S, Dixit K, Sohi H, Shegokar R. Expedition of liposomes to intracellular targets in solid tumors after intravenous administration. J Pharm Investig. 2013;43:75–87.
Mart RJ, Liem KP, Webb SJ. Creating functional vesicle assemblies from vesicles and nanoparticles. Pharm Res. 2009;26:1701–10.
McNerny KL, Kim Y, Laughlin DE, McHenry ME. Chemical synthesis of monodisperse γγ-Fe–Ni magnetic nanoparticles with tunable curie temperatures for self-regulated hyperthermia. J Appl Phys. 2010;107:09A312–4.
Mehdaoui B, Meffre A, Lacroix LM, Carrey J, Lachaize S, Gougeon M, Respaud M, Chaudret B. Large specific absorption rates in the magnetic hyperthermia properties of metallic iron nanocubes. J Magn Magn Mater. 2010a;322:L49–52.
Mehdaoui B, Meffre A, Lacroix LM, Carrey J, Lachaize S, Respaud M, Gougeon M, Chaudret B. Magnetic anisotropy determination and magnetic hyperthermia properties of small Fe nanoparticles in the superparamagnetic regime. J Appl Phys. 2010b;107:09A324.
Mendoza-Resendez R, Bomati-Miguel O, Morales MP, Bonville P, Serna CJ. Microstructural characterization of ellipsoidal iron metal nanoparticles. Nanotechnology. 2004;15:S254–8.
Molday RS, MacKenzie D. Immunospecific ferromagnetic iron-dextran reagents for the labeling and magnetic separation of cells. J Immunol Methods. 1982;52:353–67.
Naqvi S, Samim M, Abdin MZ, Ahmed FJ, Maitra AN, Prashant CK, Dinda AK. Concentration-dependent toxicity of iron oxide nanoparticles mediated by increased oxidative stress. Int J Nanomedicine. 2010;5:983–9.
Néel L. Théorie du traînage magnétique des ferromagnétiques en grains fins avec application aux terres cuites. Ann Geophys. 1949;5:99–136.
Nigam S, Barick KC, Bahadur D. Development of citrate-stabilized Fe3O4 nanoparticles: conjugation and release of doxorubicin for therapeutic application. J Magn Magn Mater. 2011;323:237–43.
O’Grady K, Bradbury A. Particle size analysis in ferrofluids. J Magn Magn Mater. 1994;39:91–4.
Ondeck CL, Habib AH, Ohodnicki P, Miller K, Sawyer CA. Theory of magnetic fluid heating with an alternating magnetic field with temperature dependent materials properties for self-regulated heating. J Appl Phys. 2009;105:07B324–07B324-3.
Pankhurst QA, Connolly J, Jones SK, Dobson J. Applications of magnetic nano-particles in biomedicine. J Phys D Appl Phys. 2003;36:R167–81.
Portet D, Denizot B, Rump E, Lejeune JJ, Jallet P. Nonpolymeric coatings of iron oxide colloids for biological use as magnetic resonance imaging contrast agents. J Colloid Interface Sci. 2001;238:37–42.
Pradhan P, Giri J, Samanta G, Sarma HD, Mishra KP, Bellare J, Banerjee R, Bahadur D. Comparative evaluation of heating ability and biocompatibility of different ferrite-based magnetic fluids for hyperthermia application. J Biomed Mater Res B Appl Biomater. 2007;81B:12–22.
Prasad NK, Rathinasamy K, Panda D, Bahadur D. Mechanism of cell death induced by magnetic hyperthermia with nanoparticles of γ-Mn x Fe2–x O3 synthesized by a single step process. J Mater Chem. 2007;17:5042–51.
Purushotham S, Ramanujan RV. Modeling the performance of magnetic nanoparticles in multimodal cancer therapy. J Appl Phys. 2010;107:114701–114701-9.
Rosensweig RE. Heating magnetic fluid with alternating magnetic field. J Magn Magn Mater. 2002;252:370–4.
Safarik I, Safarikova M. Magnetic nanoparticles and biosciences. Monatchefte Chem. 2002;133:737–59.
Schlesinger MJ. Heat shock proteins. J Biol Chem. 1990;265:12111–4.
Shinkai M, Ito A. Functional magnetic particles for medical application. Adv Biochem Eng Biotechnol. 2004;91:191–220.
Shliomis MI. Magnetic fluids. Sov Phys Usp. 1974;17:153–69.
Sunderland CJ, Steiert M, Talmadge JE, Derfus AM, Barry SE. Targeted nanoparticles for detecting and treating cancer. Drug Dev Res. 2006;67:70–93.
Tanaka K, Ito A, Kobayashi T, Kawamura T, Shimada S, Matsumoto K, Saida T, Honda H. Intratumoral injection of immature dendritic cells enhances antitumor effect of hyperthermia using magnetic nanoparticles. Int J Cancer. 2005;116:624–33.
Veiseh O, Gunn JW, Zhang M. Design and fabrication of magnetic nanoparticles for targeted drug delivery and imaging. Adv Drug Deliv Rev. 2010;62:284–304.
Wu SY, Yang KC, Tseng CL, Chen JC, Lin FH. Silica-modified Fe-doped calcium sulfide nanoparticles for in vitro and in vivo cancer hyperthermia. J Nanopart Res. 2011;13:1139–49.
Yallapu MM, Othman SF, Curtis ET, Gupta BK, Jaggi M, Chauhan SC. Multi-functional magnetic nanoparticles for magnetic resonance imaging and cancer therapy. Biomaterials. 2011;32:1890–905.
Yin PT, Shah BP, Lee K-B. Combined magnetic nanoparticle-based microRNA and hyperthermia therapy to enhance apoptosis in brain cancer cells. Small. 2014;10:4106–12.
Zeisbergera M, Dutza S, Muller R, Hergt R, Matoussevitch N, Bonnemann H. Metallic cobalt nanoparticles for heating applications. J Magn Magn Mater. 2007;311:224–7.
Zhang Y, Kohler N, Zhang M. Surface modification of superparamagnetic magnetite nanoparticles and their intracellular uptake. Biomaterials. 2002;23:1553–61.
Zhang XX, Wen GH, Xiao G, Sun S. Magnetic relaxation of diluted and self-assembled cobalt nanocrystals. J Magn Magn Mater. 2003;261:21–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Caizer, C. (2017). Magnetic Hyperthermia-Using Magnetic Metal/Oxide Nanoparticles with Potential in Cancer Therapy. In: Rai, Ph.D, M., Shegokar, Ph.D, R. (eds) Metal Nanoparticles in Pharma. Springer, Cham. https://doi.org/10.1007/978-3-319-63790-7_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-63790-7_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63789-1
Online ISBN: 978-3-319-63790-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)