Abstract
The urachus is a midline tubular structure that extends upwards from the dome of the bladder towards the umbilicus. It is a vestigial remnant of the connection between the early bladder and the fading allantois. The tubular urachus normally involutes before birth remaining as a fibrous band. Persistence of a (partially) patent urachus may give rise to various clinical problems in newborns, infants, children and even adults. Congenital urachal anomalies may present under 4 different forms with variable percentages and consequences.
Because urachal remnant diseases are uncommon (1/ 7500 autopsies) and manifest with non-specific abdominal or urinary symptoms, pre-surgical diagnosis is not always made. Imaging techniques, presently US and CT, will have an important role for the characterization and the follow-up of complicated urachal remnants of the sinus and cyst types. MR imaging is infrequently used due to lack of availability and duration of examination but provides significant information; its use will surely increase especially with the potential contribution of DWI. US will also be essential for the differential diagnosis of other umbilical anomalies and for the demonstration of rare tumors developing within the urachus.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 General Considerations
The urachus is a midline tubular structure that extends upwards from the dome of the bladder towards the umbilicus. It is a vestigial remnant of the connection between the early bladder and the fading allantois. The tubular urachus normally involutes before birth remaining as a fibrous band. Persistence of a (partially) patent urachus may give rise to various clinical problems in newborns, infants, children, and even adults. Congenital urachal anomalies may present under 4 different forms with variable percentages and consequences.
A first form, the commonest, is a completely patent urachus. It accounts for 50% of cases and is associated with several lower urinary tract anomalies, mainly the prune-belly syndrome and posterior urethral valves. The condition is easily recognized at birth due to urine leakage from the umbilicus. The patent urachus is visualized through retrograde voiding cystography. Management of this type of anomaly will be included in the global treatment of the underlying anomaly. A second anomaly, vesico-urachal diverticulum (3–5% of cases) will also be incidentally opacified during cystography. This anomaly lacks clinical significance. The two other congenital anomalies include an umbilical-urachal sinus (15%) and urachal cyst (30%). Part of the patients presenting these last 2 congenital anomalies will become symptomatic generally due to superinfection and enlargement of the urachus.
Because urachal remnant diseases are uncommon (1/7500 autopsies) and manifest with non-specific abdominal or urinary symptoms, pre-surgical diagnosis is not always achieved. Imaging techniques, presently US and CT, will have an important role for the characterization and the follow-up of complicated urachal remnants of the sinus and cyst types. MR imaging is infrequently used due to lack of availability and duration of examination but provides significant information; its use will surely increase especially with the potential contribution of DWI. US will also be essential for the differential diagnosis of other umbilical anomalies and for the demonstration of rare tumors developing within the urachus [1,2,3,4,5,6,7,8,9].
2 Complicated Urachal Sinus
Urachal sinus consists of a blind dilatation of the urachus at the umbilical end. The main symptom of a complicated sinus would be a (recurrent) pus discharge through the umbilicus associated with the palpation of a thickened cord on the midline below the umbilicus. This is typically a pathology occurring in early life or infancy but it does occur at any age.
On US, the fibrous cord connecting the umbilicus to the bladder will appear hypoechoic and thickened with sometimes increased flow on color Doppler. The thickened urachus will measure 3–4 mm diameter or more. The thickening may involve the entire urachal remnant cord or more commonly the part below the umbilicus on a few cm (Figs. 22.1 and 22.2). Color Doppler will demonstrate the surrounding inflammation. No other imaging will usually be necessary.
Infected urachal remnant—2-year-old girl. (a) US Sagittal scan a loculated mass extends from the umbilicus (U) towards the bladder representing a urachal remnant (Ur) abscess. (b) Color Doppler US—transverse scan below the umbilicus—massive peri-abscess hypervasularization corresponding to inflammatory response
The treatment will be mostly medical with antibiotics and the infection will resolve within a few weeks. The urachal remnant will return to a normal appearance. If necessary, the normalization can be followed up on US. As such no further treatment will be necessary [1, 7,8,9,10].
3 Complicated Urachal Cysts
A urachal cyst develops if the urachus remains patent in a localized segment somewhere between the umbilicus and the bladder. This occurs most commonly in the lower third of the urachus. Urachal cysts may be detected incidentally in asymptomatic patients. They will become symptomatic due to their rapid enlargement generally secondary to infection. Clinically the patient will complain of abdominal fullness or pain; he/she may present with lower urinary symptoms in relation with a secondary cystitis.
A thin walled cyst with echo-free fluid content will be the usual appearance in incidental asymptomatic urachal cysts. The cyst being typically located on the midline, above the bladder. This particular type of congenital urachal remnant is a different entity from the urachal remnant that can appear as a nodular nubbin on the top of the bladder, within its wall. Especially, since this latter type of remnant may sometimes present a confusing protruding cystic appearance within the bladder [7, 8, 10].
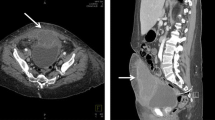
Superinfected urachal cysts will manifest on US as a thick wall cystic mass with echogenic or heterogeneous content (Fig. 22.3a,b). The wall may appear hypervascularized on color Doppler as the surrounding tissues and the wall may become inflamed. Similar findings will be demonstrated on CE-CT or MR imaging (Fig. 22.3c–e). A thick wall cyst enhancing after contrast injection will be demonstrated. Inflamed surrounding tissues may show enhancement as well and determine irregular boundaries. Rarely the cyst may rupture rendering the diagnosis more difficult.
Infected urachal cyst in a 5-year-old girl. (a) US—Sagittal scan showing a distended urachal remnant (Ur) cyst filled with echogenic material and extending from the bladder (B) towards the umbilicus. (b) US—Transverse scan below the umbilicus. The infected cyst appears round and located anteriorly just behind the abdominal wall (Ur urachal remnant cyst). (c) MR imaging—T2-weighted sequence—It demonstrates the infected cysts, lying on the dome of the bladder. (d) MR imaging—T1-weighted after Gd injection. Enhancement of the wall of the cyst and surrounding inflammatory tissues. (e) MR imaging DWI—Striking hypersignal of the abscess
The differential diagnosis of an infected urachal sinus includes all potentially infected cysts of the abdomen especially those developing around the midline such as Meckel’s diverticulum, mesenteric cyst, lymphangioma, or duplication cyst. A connecting tract from the cyst to the umbilicus (or to the bladder) is a clue for a urachal remnant [1].
The treatment is controversial. In young infants, it will be mainly medical; surgery being reserved for unfavorable evolution or recurrence. The treatment would more often be surgical in older children, as excision of the infected cyst is performed to prevent reinfection (30% of reinfection rate). Furthermore, some authors have reported the increased risk of tumoral development in unresected or incompletely resected urachal remnant (see below). As mentioned, this remains controversial [1, 3, 11, 12].
4 Other Umbilical Anomalies
Various other umbilical anomalies need to be considered whenever a urachal remnant is suspected. The pathologies may be self-limited to the umbilicus or the “tip of an iceberg,” as part of the anomaly extends within the abdomen.
4.1 Localized Anomaly
Omphalitis is defined as erythema and edema of the umbilical region with or without discharge from the abdomen. An umbilical granuloma may develop after the cord separation when the epithelialization has been incomplete. The granulation tissue may overgrow and form a granuloma. Both entities do not require imaging and will be treated medically.
Rarely, an abscess may develop and masquerade as urachal remnant; imaging will demonstrate the limited localized lesion (Fig. 22.4).
4.2 Umbilical Anomaly as a Sign of a Deeper Intraabdominal Pathology
Umbilical discharge may be a common symptom to different entities. As mentioned already, it can correspond to the discharge of a patent or inflamed urachal remnant as well as associated with omphalitis. Another etiology for umbilical discharge or inflammation is vitelline duct remnant. Meckel’s diverticulum is the most common type of vitelline duct remnant, but does not present usually umbilical symptoms (See also Chap. 11). On the contrary, a patent vitelline duct that represents only 2% of duct remnants does manifest with umbilical symptoms. In such condition, feces will appear in the umbilicus and will facilitate the diagnosis. Fistulography may be performed in case of uncertain diagnosis. It will show the connection to the digestive tract.
Vitelline sinus or a vitelline cyst is also part of the panel of anomalies of vitelline duct remnants; they are also connected to the umbilicus; they may become infected and can cause umbilical inflammation. US may be performed to demonstrate the cyst type; the sinus may be more difficult to demonstrate. CT may be performed in ambiguous cases.
All symptomatic vitelline duct anomalies need to be excised.
An umbilical hernia develops when the umbilical ring fails to close after the cord separation. A protrusion will then appear at the umbilicus. It may contain just fat or some bowel loops. Umbilical hernia rarely incarcerates and the natural history is towards spontaneous resolution. Imaging is rarely necessary (see also Chap. 29) [4, 13].
5 Tumors Developing in Urachal Remnants
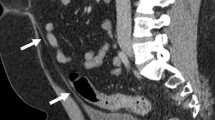
Very rarely urachal tumors develop in the urachus during childhood. Case reports of different types of tumors have been reported, both benign and malignant. Among others, benign teratoma, mucinous tumor, giant cell tumor, rhabdomyosarcoma (Fig. 22.5) or yolk sac tumor. Rupture of urachal tumors has been exceedingly rarely reported. Exceptionally as well, a tumor may develop within the umbilicus itself (e.g., duplication cyst) [12, 14,15,16].
Imaging rater CE-CT than US, or whenever available MR imaging will provide clues for the diagnosis of the tumoral nature of the mass rather than a complex inflamed urachal remnant. It will also help to determine the extension of the tumor.
Noteworthy, the relation between urachal remnants and carcinoma developing in adults is controversial. Urachal carcinoma accounts for few than 1% of bladder neoplasms (in adults). No convincing association has been established between urachal remnants in childhood and later urachal carcinoma. Therefore, it has been recommended that patients with asymptomatic umbilical remnants and patients under 1 year should not undergo surgical resection unless symptoms are recurrent [5, 12, 14,15,16].
Conclusion
Urachal remnants complications should always be included in the differential diagnosis of acute abdominal pain especially in young children. US is useful for their demonstration and for the differential diagnosis. CE-CT and MR imaging may provide additional information.
References
Yu J, Kim KW, Lee HL, et al. Urachal remnant diseases: spectrum of CT and US findings. Radiographics. 2001;21:451–61.
Choi YJ, Kim JM, Ahn SY, et al. Urachal anomalies in children: a single center experience. Yonsei Med J. 2006;47:782–6.
Naiditch JA, Radhakrishnan J, Chin AC. Current diagnosis and management of urachal anomalies. J Pediatr Surg. 2013;48:2148–52.
O’Donell KA, Glick PL, Caty MG. Pediatric umbilical problem. Pediatr Clin N Am. 1998;45:791–9.
Chouchan M, Cuckow P, Humphries PD. Utility of diffusion weighted imaging in the pre-surgical diagnosis of an infected urachal cyst. Pediatr Radiol. 2011;41:125–8.
Galati V, Donovan B, Ramji F, et al. Management of urachal remnants in early childhood. J Urol. 2008;180:1824–7.
Cilento BG, Bauer SB, Retik AB, et al. Urachal anomalies: defining the best diagnostic modality. Urology. 1998;52:120–2.
Widni EE, Hollwarth ME, Haxhija EQ. The impact of preoperative US on the correct diagnosis of urachal remnants in children. J Pediatr Surg. 2010;45:1433–7.
Copp HL, Wong IY, Krishnan C, et al. Clinical presentation and urachal remnant pathology: implications for treatment. J Urol. 2009;182:1921–4.
Metwalli ZA, Guillerman RP, Mehollin-Ray AR, et al. Imaging features of intravesical urachal cyst in children. Pediatr Radiol. 2013;43:978–82.
Stopak JK, Azarow KS, Abdessalam SF, et al. Trends in surgical management of urachal anomalies. J Pediatr Surg. 2015;50:1334–7.
Sato H, Furuta S, Tsuji S, et al. The current strategy for urachal remnants. Pediatr Surg Int. 2015;31:581–7.
Abdulhai SA, Glenn IC, Ponsky TA. Incarcerated pediatric hernias. Surg Clin N Am. 2016;97:129–45.
Gleason JM, Bowlin PR, Bagli DJ, et al. A comprehensive review of pediatric urachal anomalies and predictive analysis for adult urachal carcinoma. J Urol. 2015;193:632–6.
Sumer TL, Ramanathan S, Padura M. Urachal yolk sac tumor with rupture in a child. J Pediatr Hematol Oncol. 2017;39:e82–4.
Cheik-Helard A, Irtan S, Orbah D. Urachal RMS with poor outcome. J Pediatr Surg. 2015;50:1329–33.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Avni, F.E. (2018). Complicated Urachal Remnants. In: E. Avni, F., Petit, P. (eds) Imaging Acute Abdomen in Children. Springer, Cham. https://doi.org/10.1007/978-3-319-63700-6_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-63700-6_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63699-3
Online ISBN: 978-3-319-63700-6
eBook Packages: MedicineMedicine (R0)