Abstract
Background
Urachal cysts, part of the spectrum of congenital urachal anomalies, are typically extrinsic to the urinary bladder.
Objective
The purpose of this study is to present the salient imaging features of a pediatric series of unusual intravesical urachal cysts that protrude into the bladder lumen.
Materials and methods
Five children with intravesical urachal cysts depicted on imaging studies were retrospectively identified during a 6-year period at a children’s hospital. The clinical charts and findings on ultrasound (US) and voiding cystourethrogram (VCUG) were reviewed.
Results
In all five children, US revealed a thin-walled ovoid cystic structure containing anechoic fluid or echogenic debris and residing along the midline of the anterosuperior aspect of the urinary bladder protruding into the bladder lumen. Histological examination of the partial cystectomy specimen from one child revealed a cystic urachal remnant with intestinal mucosal lining and reactive lymphoid hyperplasia. The cysts in the four other children were managed conservatively without operative intervention.
Conclusion
The purpose of this report is to expand the spectrum of urachal remnant anomalies to include these newly recognized intravesical urachal cysts, which are characterized on US by the presence of a thin-walled cyst along the midline anterosuperior aspect of the urinary bladder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The spectrum of congenital urachal remnant anomalies occurs when the urachus remains patent in its entirety from the umbilicus to the bladder (patent urachus), when only the umbilical portion of the urachus remains open (umbilical urachal sinus), when only the vesical end of the urachus remains open (vesicourachal diverticulum) or when a cyst occurs along the course of the obliterated urachus and does not communicate with either the bladder lumen or the umbilicus (urachal cyst) [1, 2]. The traditional congenital urachal remnant classification is outlined in Table 1. Because urachal cysts do not communicate with the bladder lumen, they are traditionally described as extrinsic to the bladder [2–4]. We have recently observed five children with urachal cysts with an unusual imaging appearance: The cysts in these children arose from the anterosuperior bladder wall and ballooned into the bladder lumen. The purpose of this report is to expand the spectrum of urachal remnant anomalies to include these intravesical urachal cysts and describe their imaging appearance.
Material and methods
We identified five children with intravesical urachal cysts depicted on imaging studies during a 6-year period at a children’s hospital. An Institutional Review Board-approved retrospective review of all available relevant imaging studies was conducted by three board-certified pediatric radiologists to verify the findings, and the children’s clinical charts were also reviewed to determine the patients’ age at presentation, presenting signs or symptoms, sex, pertinent medical history, treatment and follow-up, if available.
Results
The five children included three girls and two boys with age at diagnosis of intravesical urachal cyst ranging from 7 months to 9 years. All five children underwent sonography and voiding cystourethrography was performed in two. Two children were imaged because of symptoms related to urinary tract infections, one had renal/bladder sonography performed for evaluation of a thrombocytopenia-absent radius-like syndrome, one had abdominal sonography for evaluation for biliary atresia, and the fifth had an abdominal sonogram for suspected appendicitis. There was no known history of urinary bladder instrumentation in any of the children prior to the diagnosis. One of the two children with urinary tract infection had a sibling with a typical extravesical urachal cyst.
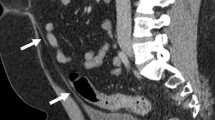
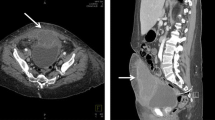
In all five children, US revealed a thin-walled ovoid cystic structure protruding intraluminally from the midline anterosuperior aspect of the urinary bladder wall. In two of the cases, there were both intramural and intraluminal components of the cyst (Fig. 1), while in three of the cases no intramural cystic component was discernible, and the cyst wall formed an acute angle with the bladder wall (Figs. 2, 3). In one of the two children undergoing voiding cystourethrography, this cystic structure was visible as a filling defect in the region of the dome of the bladder (Fig. 3).
A 9-year-old girl undergoing abdominal sonography for suspected appendicitis with incidentally discovered intravesical urachal cyst. Transverse (a) and longitudinal (b) sonographic images of the bladder demonstrate a thin-walled cyst (asterisk) along the midline anterosuperior bladder wall with intramural and intraluminal components
A 7-month-old boy with a thrombocytopenia-absent radius-like syndrome and incidentally identified intravesical urachal cyst. Transverse (a) and longitudinal (b) sonographic images of the urinary bladder demonstrate a thin-walled ovoid cyst (asterisk) arising from the anterosuperior bladder wall and protruding into the bladder lumen
A 6-year-old boy who presented with hematuria and dysuria and was found to have an intravesical urachal cyst. Transverse (a) and longitudinal (b) sonographic images of the urinary bladder demonstrate a cystic structure (asterisk) with a small amount of internal echogenic debris protruding intraluminally from the midline anterosuperior bladder wall. An oblique image from a voiding cystourethrogram (c) demonstrates a smoothly marginated, rounded filling defect (arrow) protruding intraluminally from the midline anterosuperior bladder wall
One child underwent partial cystectomy for hematuria and dysuria attributed to the urachal cyst. Histological examination of the specimen revealed a cystic urachal remnant with abundant reactive lymphoid hyperplasia and a wall lined with transitional epithelium and foci of intestinal-type epithelium (Fig. 4). This child developed an immediate postoperative urinary tract infection but was without clinical signs or symptoms referable to the urinary tract for the subsequent 3 years of follow-up. The remaining four children were managed conservatively. Two of them were lost to follow-up, while the other two were without clinical signs or symptoms referable to the urinary tract during one-and-a-half and two-and-a-half years of follow-up, respectively. In one of these children, follow-up US exams showed no change in the intravesical urachal cyst during a 4-month period. There was no recorded follow-up imaging obtained in the other children.
Histopathological section of the urachal cyst demonstrates abundant reactive lymphoid tissue (asterisk) in the wall of the cyst and transitional epithelium and foci of intestinal mucosa (arrow) lining the interior wall of the cyst (bottom of image). The cyst sits within the bladder wall with bladder mucosa above and cyst lumen below. H & E, 40x. Image courtesy of Deborah Kearney, MD, Houston, TX
Discussion
The urachus is an embryological remnant of the cloaca and the allantois. As the urinary bladder descends into the pelvis during development, the urachus elongates in the midline extraperitoneal space as a tubular structure from the apex of the bladder to the umbilicus. Typically, the lumen of the urachus obliterates, leaving a cord-like remnant. Urachal anomalies arise from failure of obliteration of the lumen.
The spectrum of urachal remnant anomalies includes patent urachus, umbilical urachal sinus, vesicourachal diverticulum and urachal cysts (Table 1). We suggest that the spectrum of anomalies be expanded to include this peculiar type of urachal cyst that balloons into the bladder lumen, and propose the term intravesical urachal cyst to describe this anomaly. True urachal remnant anomalies must be distinguished from the hypoechoic urachal remnant seen along the prevesical space or anterosuperior bladder wall in nearly all children [3–5]. Ozbek et al. [3] reported that 9% of urachal remnants in children have a “significant protrusion” into the urinary bladder lumen, but did not report the frequency of a cyst-like appearance with an acute angle interface with the bladder wall. Leicher-Düber [6] reported the existence of fusiform urachal remnants that cause an impression on the ventral bladder wall, but did not describe an intravesical location of the remnants. Yagishita et al. [7] reported the histopathological findings in a case of an urachal cyst protruding in the bladder lumen and four additional cases of urachal cysts with intravesical development in a review of the Japanese medical literature, but the imaging features were not detailed.
The most common complication of an urachal cyst is infection. Although the risk of malignant transformation of an urachal remnant anomaly in children is very low, adults presenting with symptomatic urachal anomalies require more extensive surgical intervention and have a much higher incidence of malignancy [8]. In a study by Ashley et al. [9], 51% of symptomatic urachal anomalies identified in adults were malignant. Although surgical excision is the traditional management of symptomatic urachal anomalies, Lipskar et al. [10] suggest that nonoperative management of even symptomatic urachal cysts in children may be reasonable if serial US demonstrates spontaneous involution of infected urachal cysts after initial adequate drainage. While one of our cases of intravesical presented with hematuria, the risk of developing complicating infection or neoplasia is unknown.
One limitation of our study is the lack of histological confirmation of the presumed diagnosis in four of the five children. The urachal remnant in our series that was surgically excised had a lining consisting of both transitional epithelium and foci of intestinal-type epithelium on histological examination. Although urachal remnants are classically lined by transitional epithelium, up to 25% of urachal anomalies examined histologically have alternative linings, including colonic, small intestinal or squamous epithelium. The clinical significance of the presence of alternative linings is uncertain [8]. The US findings in the other children were very similar and considered consistent with an urachal remnant anomaly, and surgical excision could not be justified in the absence of complications requiring operative intervention. The absence of solid elements alleviated concern for a neoplastic or proliferative tumor such as rhabdomyosarcoma, neuroblastoma, leiomyoma or inflammatory pseudotumor. The intravesical location excluded the possibility of an omphalomesenteric duct cyst that can mimic extravesical midline periumbilical urachal cysts. The natural history of these intravesical urachal cysts could not be defined due to the lack of availability of long-term follow-up imaging studies. Also, the prevalence could not be established as a systematic review of the bladder in children undergoing bladder imaging studies was not conducted. The cases identified were encountered during the course of routine clinical practice.
Conclusion
We report a case series of intravesical urachal cysts and propose that the spectrum of urachal remnant anomalies be expanded to include this previously neglected anomaly. Intravesical urachal cysts are characterized on US by the presence of a thin-walled cyst protruding intraluminally from the midline anterosuperior aspect of the wall of the urinary bladder. Although these may be managed conservatively without surgical intervention if discovered incidentally, the potential risk for superinfection or malignant transformation as reported for other urachal remant anomalies is unclear.
References
Saddler TW (1995) Langman’s medical embryology. Williams and Wilkins, Baltimore
Yu JS, Kim KW, Lee HJ et al (2001) Urachal remnant diseases: spectrum of CT and US findings. Radiographics 21:451–461
Ozbek SS, Pourbagher MA, Pourbagher A (2001) Urachal remnants in asymptomatic children: gray-scale and color doppler sonographic findings. J Clin Ultrasound 29:218–222
Cacciarelli AA, Kass EJ, Yang SS (1990) Urachal remnants: sonographic demonstration in children. Radiology 174:473–475
Zieger B, Sokol B, Rohrschneider W et al (1998) Sonomorphology and involution of the normal urachus in asymptomatic newborns. Pediatr Radiol 28:156–161
Leicher-Düber A, Schumacher R (1991) Urachal remnants in asymptomatic children: sonographic morphology. Pediatr Radiol 21:200–202
Yagishita H, Nagayama T, Zean Z et al (2001) A case of asymptomatic urachal cyst in autopsy – histopathological study of urachal cyst and review of the literature of 99 cases during a 10 year period in Japan. Hinyokika Kiyo 47:849–852
Upadhyay V, Kukkady A (2003) Urachal remnants: an enigma. Eur J Pediatr Surg 13:372–376
Ashley RA, Inman BA, Routh JC et al (2007) Urachal anomalies: a longitudinal study of urachal remnants in children and adults. J Urol 178:1615–1618
Lipskar AM, Glick RD, Rosen NG et al (2010) Nonoperative management of symptomatic urachal anomalies. J Pediatr Surg 45:1016–1019
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Metwalli, Z.A., Guillerman, R.P., Mehollin-Ray, A.R. et al. Imaging features of intravesical urachal cysts in children. Pediatr Radiol 43, 978–982 (2013). https://doi.org/10.1007/s00247-013-2628-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2628-y