Abstract
Cognitive decline is a very common condition in advanced age with an enormous impact on health outcomes and patient’s trajectories. Despite this, cognitive performance is not systematically evaluated in older community dwellers and hospitalized patients, with the consequence of late diagnosis. This delay in diagnosis is particularly deleterious because cognitive impairment progresses to dementia which is not curable but associated to a number of geriatric syndromes and conditions associated with disability and mortality—falls, delirium, dysphagia, poor compliance, and adherence to treatment plans. The comprehensive geriatric assessment helps both for the early identification of cognitive impairment if not yet diagnosed and for improved clinical decision making in patients with advanced decline and dementia.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
By the end of the chapter, the reader will be able to
-
Define characteristics and burden of cognitive impairment in advanced age and recognize the multifactorial, continuum-like nature of cognitive impairment to dementia in advanced age as well as the challenges to the use of biomarkers and psychometric tests
-
Acknowledge the factors associated with adverse outcomes and clinical decision making in older patients with cognitive impairment and dementia
-
Provide the rationale for routine cognitive examination in older adults seeking for medical help due to other reasons than dementia
-
Extrapolate the impact of dementia and cognitive decline on diseases and different geriatric syndromes
1 Demographics, Definition, and Pathophysiology of Cognitive Decline
Cognitive decline—displaying as diminished orientation and/or ability to remember, judge, understand, and reason among several other cognitive abilities—is frequent in advanced age. Cognitive decline represents the phenotypical expression of age-related changes occurring in the “aging brain” within the process of senescence. In other words, age-related cognitive decline represents the expression of increased neuronal vulnerability due to senescence in the postmitotic structure of the brain (Drachman 1997; Drachman 2006). As for severe cognitive impairment the term dementia (from the Latin de, “out of”, and mens, “mind”) is used, this clinical entity is presented here in its main diagnostic and therapeutic features for didactic purposes. While the detailed description of each set of criteria is provided in the correspondent literature (extensively reviewed in Winblad et al. 2016), its presentation goes beyond the scope of this chapter. Diagnostic terms from dementia to what is considered its most common form, Alzheimer’s disease (AD), are based upon criteria (Table 7.1) currently under careful consideration for reliability and representativeness in old and very old age. These are difficult to apply in advanced age due to the heterogeneity of the aging process (see also Chapter 3) and the continuum from organ integrity to severe pathology typically evident along with aging.
Cognitive impairment due to age-related cognitive decline, from mild impairment to overt dementia, encompasses a range of neurological disorders characterized primarily, but not only, by loss of memory and orientation. For the diagnosis of dementia, presence of cognitive impairment in multiple domains and functional loss are required (Table 7.1); AD is considered the leading cause of dementia and its primary risk factor is advanced age. Once dementia is diagnosed in its mild and moderate stages, patients are overtly forgetful and disoriented, neglect their disorder, and are not able to judge its consequences. Later on, during the course of the disease, patients lose their ability to communicate, fail to recognize loved ones, become bedridden, and require continuous care, with 12–17 years’ living with disability (WHO 2016). Dementia is indeed known to increase mortality, but contributing factors are not well established, although some variables, such as being male, neuropsychiatric symptoms, comorbidity, and development of functional disability during follow-up, have been associated with a decrease in survival (http://www.who.int/mediacentre/factsheets/fs362/en/. Latest access August 15th, 2017).
As global life expectancy has reached 71.4 years (WHO 2016), the socioeconomic burden of cognitive impairment due to age-related decline will dramatically hit developing countries in the next years. Dementia alone is expected to reach over 130 million persons worldwide by 2050 (Winblad et al. 2016) with one-third of the oldest-old population being affected by mild cognitive impairment (MCI), considered to precede dementia (Petersen et al. 2015, Drachman 2006). Most importantly, this already impressive demographic burden is largely underestimated (Winblad et al. 2016) and cure against age-related cognitive decline including dementia is beyond our grasp. The extremely complex multifactorial pathophysiology of age-related cognitive impairment and dementia (Fig. 7.1) includes molecular biology of aging (Drachman 1997; Drachman 2006), mechanisms in part distinct from AD-related accepted ones (Pavlopoulos et al. 2013), and irreversible age-related changes of the postmitotic brain (Table 7.2).
Figure 7.1 displays the interconnectivity between the multiple features of the continuum from aging brain to dementia presented in Fig. 7.2 as well as the extreme complexity of this continuum’s context. The main age-related characteristics of the brain include structural, cellular, molecular, biochemical, and vascular changes reflecting impressively the known theories of the aging process itself—intrinsic and extrinsic—and are associated to cognition correlates (reviewed in detail in Drachman 2006): with advanced age, memory and fluid intelligence (the mixture of reaction time, channel capacity, and creativity) decrease, while crystallized intelligence (or wisdom, including vocabulary, past knowledge, and previously acquired skills) remains stable.
The multifactoriality of age-related cognitive decline.Different changes occur in a structurally and biomolecularly heterogeneous way from person to person. The consequence is a continuum from brain aging to dementia (Fig. 7.2) difficult to diagnose and treat according to standard diagnosis and therapy. Personalized, multidimensional management is necessary
Physiological changes associated with the aging of the brain explain not only memory loss but also impairment of other cognitive domains and neurological and neuropsychiatric systems. These cause motoric alterations, posture, balance and gait disorders, sleep disturbances, sensory decrements, personality changes, and mood disorders (Förstl et al. 2009). Furthermore, the characteristics of the aging brain are shared by those known to be typical of dementia in general and of AD in particular (Fig. 7.1). Despite this overlap, it is commonly accepted that AD is a distinct condition whose multiple pathophysiologic mechanisms are those displayed in the upper right section of Fig. 7.1 and include β-amyloid accumulation and neurotransmitter deficits, particularly deficits of cholinergic transmission. Both of the latter are the major targets of current drug treatments and clinical studies exploring new drug options; misfolded protein deposition in some regions of the brain is still considered the main histopathological marker of AD (Alzheimer et al 1995). To date, however, no cure exists against AD.
2 Geriatric Correlates of Cognitive Decline and Dementia: Underestimation, Risk Factors, Consequences
Beyond the traditional neurologic diagnostic algorithm and therapy of AD, this chapter aims at describing the approach to cognitive decline as a geriatric syndrome, highly challenging and with profound impact on the older ill adult.
First of all, cognitive impairment and dementia are not only underestimated but also diagnosed very late considering that the neurodegenerative changes associated with dementia (upper right corner of Fig. 7.1) may begin up to 30 years prior to symptom onset. Late diagnosis occurs because older patients tend to minimize their complaints, considering them part of “normal” aging, and also in part due to the concerns associated to a diagnosis of dementia—fear of limited own independence, management of finances, inheritance issues within the family, withdrawl of driving license, etc.Factors hindering prompt diagnosis of cognitive decline in advanced age:
-
Understanding of memory impairment as normal in advanced age
-
Lack of neurogeriatric education
-
Ageism
-
Fear of losing independence
Indeed, there are studies showing that cognitive decline is not systematically addressed in hospitalized patients, although it represents a major risk factor for geriatric syndrome development. From a geriatric perspective, the use of a Comprehensive Geriatric Assessment (CGA) foresees that the older person undergoes cognitive evaluation together with clinical, functional, and social examinations (Rubenstein 1984) (see also Chapter 26). By systematically including cognition among the domains explored in an older adult, problems related to poor detection of cognitive impairment and late diagnosis of dementia are overcome (Ellis 2011). Within the CGA, usually the Mini-Mental State Examination (MMSE) is used to screen multidomain cognitive performance (Folstein et al. 1975). However, as the MMSE is not easy to perform at general pactitioner (GP) settings (Folstein et al. 1975), many other tests are being implemented and validated including the clock-drawing test (Shulman et al. 2000). The evaluation of cognition can disclose a beginning deterioration and, even in the case of MCI diagnosis, it can pave the way to appropriate diagnosis. In case of suspected cognitive impairment at the CGA, comanagement with neurologist and performance of a broader test battery are highly recommended. However, the focus of the geriatric intervention will be on identification of all those factors able to influence and precipitate patient trajectories in advanced age (Tables 7.3 and 7.4).
Despite the fact that cognition is frequently negatively affected by inadequate clinical decisions and treatment plans (Campbell et al. 2016; Boccardi et al. 2017; Nørgaard et al. 2016; Ekdahl et al. 2016), it is not systematically addressed in hospitals (Mecocci et al. 2017) and up to 89% of older patients with a MMSE <24 might have been not diagnosed with cognitive impairment at the hospital admission occurred during the previous 12 months. However, proactive care targeting cognitive impairment might be extremely effective in very vulnerable multimorbid older patients, not only with respect to health outcomes, but also regarding quality of life and well-being. In addition, when progression of cognitive impairment and dementia is ascertained, patients and caregivers—the latter usually providing the largest part of the care to the cognitively impaired person—should be systematically allowed to be central authors of important decisions regarding prognosis of dementia, advanced care planning, and palliative, legal, and ethical issues (see Part VII and Part VIII).
For these reasons, and also for the socioeconomic impact of early recognizing cognitive decline up to very advanced age, cognition should be carefully considered when visiting older persons, especially those referring to the physicians for other reasons than cognitive impairment. In fact, while the sets of criteria to make a clinical diagnosis of dementia are under systematization since years (Table 7.1), diagnosis of MCI as the recognized prodromal stage of dementia (Albert et al. 2011) and its preceding phase, subjective cognitive impairment (SCI; Reisberg et al. 2008, “when the patient knows but the doctor does not know”), are highly challenging in older adults (the doctor does not ask, the patient does not complain and is not clearly ill). The continuum between cognitive integrity and dementia in advanced age (Fig. 7.2) is particularly challenging for the diagnosis of clinically significant cognitive impairment, since cutoff values, biomarkers, and neuropsychological assessments have limited significance and applicability in old-age subjects, particularly in the oldest old (Mattson et al. 2012).
3 Therapeutic and Management Challenges
As mentioned above, no cure is available against dementia, AD, MCI, and cognitive decline, as the latter occurs physiologically with increasing age, and the multifactoriality by nature of both conditions has impeded so far the identification of a single pathophysiological mechanism of dementia to be effectively targeted with drugs.
Nevertheless, symptomatic antidementia drugs such as acetylcholinesterase inhibitors (AChEIs) (donepezil, galantamine, and rivastigmine) and the N-methyl-d-aspartate (NMDA) receptor antagonist memantine have been developed in the last few decades; their use as well as the use of antipsychotics and sedatives need to occur in a very calibrated way (Boccardi et al. 2014). While antidementia drugs may delay nursing home placement alone or in combination and may reduce mortality for patients living in nursing homes and in the community (Gillette-Guyonnet et al. 2011; Rountree et al. 2013), decision making for therapeutical, including non-pharmacological options in older patients with dementia, is a major challenge for health practitioners, particularly in frail older patients with comorbidity and high mortality risk. There is a huge debate on the use of antidementia dugs (donepezil, galantamine, rivastigmine, and/or memantine) with respect to increase of survival in older community-dweller subjects with dementia and who are particularly frail (Riverol et al. 2011; Norstrom et al. 2011; Meguro et al. 2014; Gillette-Guyonnet et al. 2011; Schneider et al. 2014).
From a geriatric perspective, it is not surprising that data on effectiveness of antidementia drugs is conflicting. Antidementia drugs have been tested in randomized controlled trials (RCTs) typically excluding older multimorbid patients; however, these real-life patients are those who indeed are prescribed with drugs tested in the above-cited RCTs: in clinical experience, patients in need of antidementia treatment are very old, mostly women, suffering often from vascular comorbidities. Antidementia RCTs, in contrast, usually exclude very old, frail, multimorbid patients and include patients with dementia which might be not representative of the general population. In addition, the ameliorations shown in patients receiving treatment with respect to placebo in RCTs are based on non/patient-centered outcomes, such as prolongation of life (i.e., survival rather than disability-free life expectancy or healthy life expectancy) or mild score improvements at neuropsychological tests which clinical relevance might be questionable. In other words, there are no studies showing an undebated positive effect of a disease-modifying drug against AD neither using patient-centered endpoints such as quality of life and functionality. However, current antidementia remains a therapeutic option against dementia; research is urgently needed on the effect of therapeutic interventions—pharmacologic and non-pharmacologic—against dementia in oldest-old multimorbid patients, as these are the segments of the population most rapidly expanding (Boccardi et al. 2017; EU 2017).
In summary, the treatment of dementia is highly challenging because dementia among older community dwellers and hospitalized patients is underdiagnosed and undertreated; furthermore, treatment options available are symptomatic and have been or are being tested in patients: old-old male more than female, without substantial vascular morbidity—substantially different from those receiving prescription of antidementia in real life—oldest-old female with major cardiovascular comorbidity.
Age-Related Cognitive Decline and Dementia: A Synthetic Guide for Undergraduates and Residents in Geriatrics—Part I, General Considerations
-
The number of patients in general and acute wards who also have some form of cognitive impairment is high and rising. Around a quarter of hospital beds accommodate someone with dementia, with the percentage rising to around 40% for patients over the age of 80, which share will rise to 12% of the European population by 2050 (EU Report 2017).
-
Old-old and oldest-old adults are likely to suffer from some sort of cognitive decline, but due to the (1) heterogeneity and complexity of aging, (2) the continuum between aging and pathology in advanced age, and (3) the fact that mildly cognitively impaired older adults don’t complain and doctors don’t ask, cognitive impairment is poorly diagnosed, prevented, and treated.
-
Old-old and oldest-old adults with and without cognitive impairment suffer from multimorbidity often including vascular pathology and disability and are at high risk of delirium, falls, and poor compliance with treatment and institutionalization. Investigation targeted the geriatric instability syndrome.
-
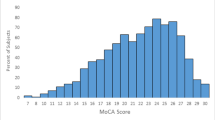
Expect older adults with cognitive impairment. Ask targeted for forgetfulness. If the patient is cooperative, take your time to perform a screening such as the Short Portable Mental Status Questionnaire (see also Part VI, Chapter 1) or the Mini-Mental State Examination (http://www.dementiatoday.com/wp-content/uploads/2012/06/MiniMentalStateExamination.pdf). Although cutoffs for psychometric screenings must be used carefully especially in advanced age, do consider further assessments by a MMSE score of 24/30 for persons with lower and of 27/30 for persons with higher education. Do consider to perform the clock-drawing test or the Montreal Cognitive Assessment (MoCA) (www.mocatest.org). Train on the performance of both. If the older patient scores poorly, (1) do refer to broader neuropsychology and comanage with neurologist; (2) take your time for adequate history collection with the caregiver; (3) investigate on medication, comorbidities, and other potentially reversible causes; (4) inform patients and/or caregivers on ethical issues, prognosis, power of lifestyle, and vascular preventive strategies; and (5) comanage with the neurologist and carefully consider the indication for medication with antidementia.
-
If you are not sure why your newly admitted hospitalized older patient is confused, do target the differential diagnosis between delirium and dementia: talk to accompanying person or caregiver and screen for delirium using for instance the 4 ‘A’ test (MacLullich, www.the4at.com). Do consider, respectively, for delirium and dementia (1) subacute vs. the insidious symptomatic; (2) changing vs. clear consciousness; and (3) frequent vs. stage-dependent presence of hallucinations and alteration of concentration, orientation, sleep, and psychomotor activity.
Age-Related Cognitive Decline and Dementia: A Synthetic Guide for Undergraduates and Residents in Geriatrics—Part II, the ABC of Clinical Decision Making Regarding Cognition in Older Patients
-
A.
Is the patient cognitively impaired?
Address orientation for person and situation by asking name, birthdate, address, and reason for seeking medical advice (rather than abruptly examining spatial and temporal orientation or recall of three objects). Encourage caregiver presence, and, if the visit takes place under caregiver’s initiative, interview separately. Ask patient respectfully about presence of forgetfulness. Ask politely to perform some evaluation. Ensure that patient has his/her eyeglasses, slept, and ate/drank well before the test. Perform the clock-drawing test after training and performing under supervision. Avoid pressure of time. If you are trained enough and have time for appropriate examination, consider MMSE or MoCA performance. Encourage the patient to give his/her best, without providing feedback. When scoring the neuropsychological tests, do acknowledge your level of experience and run-in effect. Ask for advice. Do score upon consideration of social background, years of education, therapeutic drug plan, presence of current stress factors (disease, loss of a family member, fatigue), depressive symptoms, extrapyramidal signs, sensory (patient does not hear and see well, suboptimal hearing, and visual correction) and motor impairment (tremor, rigidity), absence of cutoff values with advancing age, loss of predictive value of biomarkers, and assessments with advancing age. Mark on your protocols if some of the domains could not be tested and score consequently (i.e., MMSE score achieved on a total of 28 points, instead of 30 if the patient could not write the sentence and redraw the figure).
-
B.
If the patient is cognitively impaired, do consider severity according to functions and comanage with neurologist, neurogeriatrician, speech therapist, physiotherapist, and other specialists and health practitioners according to disease type (AD, vascular dementia, frontotemporal dementia, mixed dementia, AD-Parkinson dementia, pseudodementia, etc.) and severity (MCI and mild dementia vs. moderate and severe dementia). Focus on judgment abilities, multimorbidity, multidimensional prognosis, and shared decision making. Upon severity—the continuum from brain aging to MCI to severe dementia—shift your decisions from primary to secondary prevention strategies using a combination of the following:
-
1.
Lifestyle strategies including balanced nutrition (encourage adherence to Mediterranean-like diets), regular physical training, structured cognitive exercise, leisure activities, and hobbies supporting well-being and quality of life
-
2.
Medication reconciliation targeting polypharmacy, aggressive antihypertensive treatment, anticholinergics, and sedatives
-
3.
Management of comorbidities such as depression; Parkinson’s disease; and cardiovascular disease to prevent heart-brain syndrome
-
4.
Drug strategies against dementia to maintain functional level and slower progression considering that in advanced age common side effects of these drugs (vertigo, somnolence, gastrointestinal symptoms) might overcome the benefits
-
5.
Drug strategies against neuropsychiatric symptoms, preferably citalopram as antidepressant and risperidone/quetiapine as neuroleptics, considering that side effects like extrapyramidal symptoms and hypokinesia can be extremely impairing in advanced age
-
6.
Music, dance therapy, reality orientation therapy, and organized arts activities for cognitively impaired older subjects
-
7.
Addressing of caregiver burden including information on supporting associations, daycare options, etc.
-
8.
Information on ethic, legal issues, advanced care planning, and palliative options including adapted management of chronic pain
-
9.
Prevention of falls, immobility, decubitus, and delirium
-
1.
-
C.
Adopt multidimensional strategies but personalize them. Do consider that most of the above-cited actions are not as time expensive as usually considered but will exert extremely positive effects on patient’s and caregiver’s quality of life. Do not apply the same counseling to every patient in the same way. At the socioeconomic level, do consider that better care is always cheaper at the end.
References
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Carrillo MC, Thies B, Phelps CH. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
Alzheimer A, Stelzmann RA, Schnitzlein HN, Murtagh FR. An English translation of Alzheimer’s 1907 paper, “Uber eine eigenartige Erkankung der Hirnrinde”. Clin Anat. 1995;8(6):429–31.
Boccardi V, Baroni M, Paolacci L, Ercolani S, Longo A, Giordano M, Ruggiero C, Mecocci P. Anticholinergic burden and functional status in older people with cognitive impairment: results from the regal project. J Nutr Health Aging. 2017;21(4):389–96.
Boccardi V, Comanducci C, Baroni M, Mecocci P. Of Energy and Entropy: The Ineluctable Impact of Aging in Old Age Dementia. Int J Mol Sci. 2017;18(12).
Drachman DA. Aging and the brain: a new frontier. Ann Neurol. 1997;42:819–28.
Drachman DA. Aging of the brain, entropy, and Alzheimer disease. Neurology. 2006;67(8):1340–52.
Drachman DA. Rethinking Alzheimer's disease: the role of age-related changes. Curr Neurol Neurosci Rep. 2007;7(4):265–8.
Drachman DA. Nature or nurture: education and the trajectory of declining brain function with age and Alzheimer disease. Neurology. 2008;70(19 Pt 2):1725–7.
Ekdahl AW, Odzakovic E, Hellström I. Living unnoticed: cognitive impairment in older people with multimorbidity. J Nutr Health Aging. 2016;20(3):275–9.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Förstl H, Perneczky R, Karenberg A, Diehl-Schmid J, Lautenschlager NT. Personality in old age. Nervenarzt. 2009;80(11):1275–82.
Gillette-Guyonnet S, Andrieu S, Nourhashemi F, Gardette V, Coley N, Cantet C, Gauthier S, Ousset PJ, Vellas B, REAL.FR Study Group. Long-term progression of Alzheimer’s disease in patients under antidementia drugs. Alzheimers Dement. 2011;7(6):579–92.
Knopman DS, Beiser A, Machulda MM, Fields J, Roberts RO, Pankratz VS, Aakre J, Cha RH, Rocca WA, Mielke MM, Boeve BF, Devine S, Ivnik RJ, Au R, Auerbach S, Wolf PA, Seshadri S, Petersen RC. Spectrum of cognition short of dementia: Framingham Heart Study and Mayo Clinic Study of Aging. Neurology. 2015;85(19):1712–21.
Mattsson N, Rosén E, Hansson O, Andreasen N, Parnetti L, Jonsson M, Herukka SK, van der Flier WM, Blankenstein MA, Ewers M, Rich K, Kaiser E, Verbeek MM, Olde Rikkert M, Tsolaki M, Mulugeta E, Aarsland D, Visser PJ, Schröder J, Marcusson J, de Leon M, Hampel H, Scheltens P, Wallin A, Eriksdotter-Jönhagen M, Minthon L, Winblad B, Blennow K, Zetterberg H. Age and diagnostic performance of Alzheimer disease CSF biomarkers. Neurology. 2012;78(7):468–76.
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34(7):939–44.
Meguro K, Ouchi Y, Akanuma K, Meguro M, Kasai M. Donepezil can improve daily activities and promote rehabilitation for severe Alzheimer’s patients in long-term care health facilities. BMC Neurol. 2014;14:243.
Nørgaard A, Jensen-Dahm C, Gasse C, Hansen HV, Waldemar G. Time trends in antipsychotic drug use in patients with dementia: a nationwide study. J Alzheimers Dis. 2016;49(1):211–20.
Pavlopoulos E, Jones S, Kosmidis S, Close M, Kim C, Kovalerchik O, Small SA, Kandel ER. Molecular mechanism for age-related memory loss: the histone-binding protein RbAp48. Sci Transl Med. 2013;5(200):200ra115.
Polidori MC, Schulz RJ. Nutritional contributions to dementia prevention: main issues on antioxidant micronutrients. Genes Nutr. 2014;9(2):382.
Reisberg B, Prichep L, Mosconi L, John ER, Glodzik-Sobanska L, Boksay I, Monteiro I, Torossian C, Vedvyas A, Ashraf N, Jamil IA, de Leon MJ. The pre-mild cognitive impairment, subjective cognitive impairment stage of Alzheimer’s disease. Alzheimers Dement. 2008;4(1 Suppl 1):S98–S108.
Riverol M, López OL. Biomarkers in Alzheimer’s disease. Front Neurol. 2011;2:46.
Rountree SD, Atri A, Lopez OL, Doody RS. Effectiveness of antidementia drugs in delaying Alzheimer’s disease progression. Alzheimers Dement. 2013;9(3):338–45.
Rubenstein LZ. Geriatric imperative: geriatric assessment programs. J Med Soc N J. 1984;81(8):651–4.
Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. 2000;15(6):548–61.
Winblad B, Amouyel P, Andrieu S, Ballard C, Brayne C, Brodaty H, Cedazo-Minguez A, Dubois B, Edvardsson D, Feldman H, Fratiglioni L, Frisoni GB, Gauthier S, Georges J, Graff C, Iqbal K, Jessen F, Johansson G, Jönsson L, Kivipelto M, Knapp M, Mangialasche F, Melis R, Nordberg A, Rikkert MO, Qiu C, Sakmar TP, Scheltens P, Schneider LS, Sperling R, Tjernberg LO, Waldemar G, Wimo A, Zetterberg H. Defeating Alzheimer's disease and other dementias: a priority for European science and society. Lancet Neurol. 2016;15(5):455–532.
Further reading can be accessed online at https://doi.org/10.1007/978-3-319-61997-2_7
Further reading can be accessed online at https://doi.org/10.1007/978-3-319-61997-2_7
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Polidori, M.C., Nelles, G., Senin, U., Mecocci, P. (2018). Cognitive Decline. In: Roller-Wirnsberger, R., Singler, K., Polidori, M. (eds) Learning Geriatric Medicine. Practical Issues in Geriatrics. Springer, Cham. https://doi.org/10.1007/978-3-319-61997-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-61997-2_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61996-5
Online ISBN: 978-3-319-61997-2
eBook Packages: MedicineMedicine (R0)