Abstract
Background
The number of adults in the USA with cognitive impairment is increasing; however, few studies report prevalence rates of undiagnosed cognitive impairment among older adults in primary care.
Objective
To determine the prevalence of undiagnosed cognitive impairment among adults ages 55 years and older in primary care settings and provide normative data for the Montreal Cognitive Assessment in this context.
Design
Single interview, observational study.
Participants
English-speaking adults ages 55 years and older without diagnoses of cognitive impairment recruited from primary care practices in New York City, NY, and Chicago, IL (n = 872).
Main Measures
Montreal Cognitive Assessment (MoCA). Undiagnosed cognitive impairment was defined by age and education adjusted z-scores more than 1.0 and 1.5 standard deviations below published norms, corresponding to mild or moderate to severe cognitive impairment, respectively.
Key Results
The mean age was 66.8 (8.0) years, 44.7% were male, 32.9% were Black or African-American, and 29.1% were Latinx. Undiagnosed cognitive impairment was identified in 20.8% of subjects (mild impairment, 10.5%; moderate-severe impairment, 10.3%). Impairment at any level of severity was associated in bivariate analyses with several patient characteristics, most notably for race and ethnicity (White, non-Latinx, 6.9% vs. Black, non-Latinx, 26.8%, Latinx, 28.2%, other race, 21.9%; p < 0.0001), place of birth (US 17.5% vs. non-US 30.7%, p < 0.0001), depression (33.1% vs. no depression, 18.1%; p < 0.0001), and impairment in activities of daily living (≥ 1 ADL impairment, 34.0% vs. no ADL impairment, 18.2%; p < 0.0001).
Conclusions
Undiagnosed cognitive impairment is common among urban dwelling older adults attending primary care practices, and was associated with several patient characteristics, including non-White race and ethnicity and depression. Normative data for the MoCA from this study may serve as a useful resource for studies of similar patient populations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The number of adults in the USA with mild cognitive impairment and dementia has been increasing with the growth of the elderly US population, even while the incidence of cognitive impairment declines.1,2 Current estimates indicate that 9% of all adult Americans and 19% of those aged 65 years and older have some form of cognitive impairment.2,3 Because mild cognitive impairment (MCI) is a risk factor for dementia, and because various and simple interventions may reduce the risk for cognitive decline or risk of harm among those with cognitive impairment,4,5,6,7,8 calls have been made for increased cognitive screening to improve the long-term management and care for these patients.9 Nevertheless, cognitive impairment frequently goes undetected in primary care settings,10,11,12 a problem attributed to various factors like inadequate training of providers.12,13 One study, for example, found that more than half of patients with dementia had not received a cognitive evaluation by their primary care physician.12 In addition to ruling out potentially reversible causes of cognitive decline, detecting cognitive decline in its earlier stages would allow clinicians to initiate early pharmacologic and lifestyle modifications to slow symptom progression and provide patients and caregivers sufficient time to seek counseling, enhance communication about symptoms and treatment decisions, identify surrogate decision-makers, and improve overall quality of life.12
Primary care is a logical venue for cognitive screening but there is little data on rates of cognitive impairment among older adults in primary care settings. Prevalence rates of MCI and dementia among middle-aged and older adults range widely and generally depend on the research focus and or clinical setting. For instance, epidemiological studies of community-dwelling adults over age 65 have reported rates of MCI as high as 24%14 whereas studies of adults with hypertension and diabetes report rates as high as 30%.15 However, there is scant data on rates of undiagnosed cognitive impairment in general primary care populations as most studies of MCI and dementia prevalence have been conducted in the context of specific chronic illnesses or more narrowly defined populations. European primary care studies that excluded persons with dementia have reported MCI rates of 31% among Spanish adults ages 50 and older with subjective cognitive complaints16 and 15 to 25% among German patients ages 75 years and older.17 In the USA, one study of cognitive functioning among primary care patients ages 55 and older in Chicago found that 36% had MCI.18
As attention is increasingly paid to cognitive impairment and potential interventions to mitigate it, a clearer picture of the prevalence of undiagnosed cognitive impairment in primary care could inform clinical leaders decisions about screening and or building the resources to manage cognitive impairment once identified. It could also affect clinicians’ clinical decision-making and diagnostic considerations. In this study, we sought to estimate the prevalence of undiagnosed cognitive impairment among adults aged 55 years and older in primary care using the Montreal Cognitive Assessment (MoCA), an instrument commonly used to screen for cognitive impairment, and to identify the patient characteristics associated with undiagnosed cognitive impairment. We also sought to provide normative data for the MoCA specifically for a primary care population.
Methods
Subjects and Settings
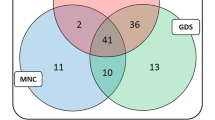
Data for this analysis were collected for a study to develop and validate machine learning models to support automated screening for cognitive impairment among older adults in primary care. We recruited patients from 5 primary care practices in the Mount Sinai Health Care System in New York City, NY, and Northwestern Memorial Hospital in Chicago, IL, from August 2020 through December 2021. These included three hospital-based teaching practices and two multi-provider faculty practices. Eligible patients were ages 55 years and older, English speaking, and able to provide informed consent in English. We excluded those with a diagnosis of MCI or dementia in the problem list or medical history of their electronic medical record. All study procedures were approved by the Institutional Review Boards of the Icahn School of Medicine at Mount Sinai and the Northwestern University Feinberg School of Medicine.
Recruitment, Interviews, and Data Collection
A list of potentially eligible patients was generated from the health systems’ electronic medical records, permission to recruit the patients was obtained from their primary care physicians, and a recruitment letter was mailed to a random selection of individuals. Research coordinators then contacted the individuals by telephone, described the study, and administered an eligibility screener. Approximately 9 months after beginning recruitment, we began oversampling White and Black male patients to achieve balanced representation by sex and race. Subjects meeting final eligibility criteria were then invited to participate in an in-person interview scheduled to immediately follow their upcoming primary care appointment. The 30-min interviews were conducted by trained research coordinators in an exam room to avoid distractions.
Measures
The primary measure was the MoCA total score. The MoCA is a widely used cognitive screener to detect MCI and dementia for clinical care and research.19,20,21,22 It consists of 12 tasks covering visuospatial/executive functioning, naming, memory, attention, language, delayed recall, and orientation. Scores range from 0 to 30. Raw scores were converted to age and education adjusted z-scores. We defined mild cognitive impairment and moderate to severe impairment as z-scores falling below 1.0 and 1.5 standard deviation (SD) of the mean of normative data, respectively,20 thresholds that are commonly applied in research and clinical care.23,24,25 Of note, diagnosis of MCI requires a subjective concern about cognition, like forgetfulness, in addition to neurocognitive assessment.26 We did not collect data on subjective cognitive complaints and MoCA threshold data presented in this paper indicate levels of impairment rather than clinical diagnoses. Results and interpretation of the MoCA assessment were provided to primary care providers upon the study participant’s request.
Data were also collected for variables that might be associated with performance on the MoCA, including age, education, race and ethnicity, English language proficiency (ELP), country of birth, depression, and physical functioning. ELP was assessed with a single item, “How would you describe your ability to speak and understand English?” with 6 response options ranging from very poor to excellent. Low ELP was defined as a response of very poor, poor, or fair. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9).27 We used an 8-item version of the PHQ that omitted a question about suicidal ideation and defined depression as a score of 10 or greater. Activities of daily living (ADLs) included bathing or showering, dressing, eating, getting in or out of bed or chair, walking, and toileting. Instrumental activities of daily living (IADLs) included ability to use a telephone, shop, prepare food, perform housekeeping chores, do laundry, use public transportation, self-manage medications, and handle finances. Impairments for each were indicated by difficulty performing or requiring assistance to perform the activity. Scores for ADL and IADL impairments were the sum of impairments for the 6 and 8 items of the measures, respectively.
Analysis
We report the mean scores on the MoCA and their standard deviations for all participants and stratified by age and level of education. Differences in mean MoCA scores across educational levels for each age group were tested with analysis of variance. We used the chi-square test to determine the univariate associations of patient characteristics with mild and moderate-severe impairment based on age and education-adjusted norms as z-scores 1.0–1.4 standard deviations and more than 1.5 standard deviations below the mean, respectively. We compared differences in the mean scores for each of the 7 domains of the MoCA by age group in linear regression analyses that adjusted for education level. Finally, we conducted a multivariable linear regression analysis of the association of participant characteristics, including age and education, with raw MoCA scores. All analyses were conducted in SAS, version 9.4 (SAS Institute, Cary, N.C.).
Results
Research coordinators attempted to call 3815 potentially eligible persons and reached 2894 (75.9%) by telephone. Of these, 1737 (60.0%) declined to be scheduled for an interview, 208 (7.2%) were ineligible because of inability to complete the screening in English, and 949 (32.8%) agreed to study participation. Signed consent was provided by 918 individuals; 872 (30.1%) completed the in-person interview.
The mean age of study participants was 66.8 years, 44.7% were male, 32.9% Black or African-American, and 29.1% were Latinx (Table 1). Educational attainment was broadly distributed, with more than half reporting some college (37.8%) or graduate education (19.5%). One quarter (25.2%) were born outside the USA. Depression was identified among 16.3% of participants and 17.0% had one or more impairments of activities of daily living.
Montreal Cognitive Assessment Scores
The mean unadjusted value for scores on the MoCA was 21.8 (4.5) (median 22, range 7–30) and the distribution of MoCA scores is shown in the Fig. 1. Table 2 displays the MoCA scores stratified by age and education level. MoCA scores did not differ across age groups for the whole sample, but declined significantly within educational strata, most notably for individuals with fewer than 12 years of education (MoCA scores for ages 55–59 years, 18.5 [3.5]; ages 60–64 years, 17.9 [3.8]; ages 65–69 years, 18.5 [4.0]; ages 70–74 years, 17.2 [4.3]; ages 75–79, 14.9 [3.5]; 80 and older, 16.0 [3.8]; p = 0.02). Performance on some of the individual domains of the MoCA also declined with increasing age, when adjusting for education, specifically, visuospatial/executive functioning, naming, and delayed recall (Table 3).
Rates of Undiagnosed Cognitive Impairment and Associations with Participant Characteristics
The rate of undiagnosed cognitive impairment based on age and education adjusted MoCA z-scores below 1.0 SD of the norm was 20.8%; 10.5% had z-scores between 1.0 and 1.4 SD below the norm, and 10.3% were 1.5 SD below the norm (Table 4). There were statistically significant differences in the rates of any undiagnosed cognitive impairment and moderate to severe cognitive impairment across all participant characteristics tested, with the exception of age. For any cognitive impairment, the largest differences were observed for ethnicity (e.g., Latinx vs. non-Latinx White, 28.2% vs. 6.9%), education (e.g., < 12 years vs. graduate education, 25.9% vs. 12.9%), non-US born vs. US born (30.7% vs. 17.5%), low vs. high English language proficiency (32.8% vs. 19.9%), depression vs. no depression (33.1% vs. 18.1%), any ADL impairment vs. no impairment (34.0% vs. 18.2%), and any IADL impairment vs. no impairment (28.0% vs. 17.3%). Similar patterns were observed for the associations of participant characteristics with moderate to severe cognitive impairment.
In a multivariable linear regression model, several participant characteristics were significantly associated with worse performance on the MoCA (Table 5), including age ≥ 75 years (β − 2.06 [0.34], p < 0.0001), non-Latinx Black race (β − 3.10 [0.36], p < 0.0001), Latinx ethnicity (β − 2.62 [0.40], p < 0.0001), other race/ethnicity (β − 2.51 [0.52], p < 0.0001), less than high school education (β − 2.06 [0.44], p < 0.0001), high school education without college (β − 4.58 [0.46], p < 0.0001), low English language proficiency (β − 1.80 [0.49], p = 0.0003), and depression (β − 1.15 [0.35], p = 0.001).
Discussion
This study reports scores on the Montreal Cognitive Assessment and rates of undiagnosed cognitive impairment in a large sample of adults ages 55 years and older in primary care. We found that 10.5% of participants had mild cognitive impairment and 10.3% had moderate to severe cognitive impairment based on MoCA scores of ≥ 1.0 and ≥ 1.5 standard deviations below age and education adjusted norms, respectively, for an overall rate of undiagnosed cognitive impairment of 20.8%. The results of this study provide a view of undiagnosed cognitive impairment in US primary care settings and are within the range of prevalence estimates reported from epidemiological studies and primary care–based studies elsewhere.3,8 The prevalence rates are lower than the rates observed in other studies, which have included populations at elevated risk of cognitive impairment, such as those with subjective cognitive complaints.18,28
The results of this study are notable for the high prevalence of moderate to severe cognitive impairment in the absence of formal diagnoses of cognitive impairment. With one in ten patients having unrecognized moderate to severe cognitive impairment, primary care physicians may be missing opportunities to address potentially reversible causes of cognitive impairment, slow the progression of cognitive decline, and/or reduce risks for these patients through counseling, modification of medication regimens, or the introduction of home-based supports.9 Although advocacy organizations, public health entities, and professional societies have called for routine cognitive impairment screening,3,9,29 the practice remains controversial as the United States Preventive Services Task Force (USPSTF) concluded in 2014, and again in 2020, that “the balance of benefits and harms of screening for cognitive impairment [among adults 65 years and older] cannot be determined.”30 The lack of a USPSTF endorsement may contribute to low rates of cognitive impairment screening. One community-based epidemiological study found that only half of older adults with dementia had undergone a cognitive evaluation12 even though Medicare reimburses for screening and a visit to develop a plan of care. Other factors may also contribute to low screening rates, such as competing priorities, clinician knowledge and attitudes, and resource constraints.10 Improving rates of screening will require consideration of all these factors as well as better integration of screening into clinical workflow. Newer technologies, such as mobile and web-based applications, may facilitate the latter.31
High rates of depression among participants with moderate or severe cognitive impairment was another notable finding of this study. Participants with depression were more than twice as likely as those without it to have moderate or severe cognitive impairment. The association of cognitive impairment with depression is well established, with depression occurring in some cases as a consequence of cognitive impairment, and in other cases cognitive dysfunction occurring as a result of depression.28,32,33,34,35 The findings of this study bring this issue into sharp focus because depression is common among older adults in primary care (16% in this cohort), and highlights the importance of screening for depression as part of the work up of persons with cognitive impairment.
Ethnoculturally diverse, minoritized study participants (e.g., non-Latinx Black American, Latinx) were considerably more likely to have undiagnosed cognitive impairment based on MoCA scores. Specifically, the results of univariate analyses revealed that Latinx participants were four times more likely to demonstrate cognitive impairment on the MoCA compared to their non-Latinx White counterparts. Moreover, the association of ethnocultural status with MoCA scores was among the strongest effects observed in multivariable analysis. Although one large epidemiological study found declining rates of cognitive impairment among Black and Latinx persons relative to non-Latinx White persons,36 other research, including studies conducted in clinical settings and in the community, indicate higher rates of cognitive impairment in these populations, consistent with our findings.18,37 A number of factors could explain the inequities observed in our study sample, including greater burden of chronic illnesses associated with cognitive impairment (e.g., diabetes, hypertension, and cardiovascular disease),38,39 adverse social determinants of health,40,41 the effects of sociocultural factors on test performance (e.g., quality of education, acculturation, linguistic factors),42,43 and/or potential limitations to the construct validity of the MoCA with ethnoculturally diverse populations.
Study Strengths and Limitations
Strengths of this study include its large sample of adults in primary care, its racial and ethnic diversity, and use of the MoCA, a widely used, well-validated screening tool for MCI and dementia. Some limitations of the study may affect interpretation and generalizability of study findings. We may have excluded some patients who had dementia or cognitive impairment on their electronic medical record problem list because it was considered but did not represent a final diagnosis. Excluding such individuals could have led to underestimation of the rate of undiagnosed cognitive impairment. Alternatively, some clinicians may have suspected cognitive impairment but not documented it, which would result in an overestimation. The net effect of these competing possibilities is unknown. Clinical staff without training in use of the MoCA might observe different performance by patients on the assessment than if it were administered by an individual trained according to the standards of its administration, such as the research coordinators who administered it in our study. We were unable to account for some factors that may contribute to the presence and/or severity of cognitive impairment, such as comorbidities, medications, and more granular sociocultural factors known to impact cognitive test performance. Additionally, English language proficiency (ELP) was measured subjectively, and patients with low ELP may have performed better on the MoCA if they were tested in their native language. Generalizability of study findings to other study populations may be limited without such data. Study participants were recruited from two urban academic healthcare systems, which may further limit generalizability, although we included both hospital- and community-based primary care practices. The MoCA is a screening tool, and although it has high sensitivity and specificity for MCI and dementia, we did not perform comprehensive neuropsychological evaluation to confirm the identified cases of cognitive impairment.
Conclusion
In conclusion, we identified high rates of undiagnosed mild and moderate to severe cognitive impairment in primary care practices of two large urban healthcare systems, and found markedly higher rates for Black and Latinx patients than for non-Latinx White patients. These findings also demonstrate that better integration of cognitive impairment screening is needed in primary care to ensure that patients with impairment are identified and appropriately evaluated, treated, and supported. We also provide normative data for the MoCA by age and education that may serve as a useful resource for studies of similar patient populations.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Langa KM, Larson EB, Crimmins EM, et al. A Comparison of the Prevalence of Dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177(1):51-58.
2022 Alzheimer's disease facts and figures. Alzheimers Dement. 2022;18(4):700-789.
Alzheimer's Disease Association. 2022 Alzheimer's Disease Facts and Figures. 2022. Accessed March 13, 2019. https://www.alz.org/media/Documents/alzheimers-facts-and-figures-2022-r.pdf
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303-8.
Lopez OL, Jagust WJ, DeKosky ST, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Arch Neurol. 2003;60(10):1385-9.
Gauthier S, Reisberg B, Zaudig M, et al. Mild cognitive impairment. Lancet. 2006;367(9518):1262-70.
Feldman HH, Jacova C. Mild cognitive impairment. Am J Geriatr Psychiatry. 2005;13(8):645-55.
Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148(6):427-34.
Morley JE, Morris JC, Berg-Weger M, et al. Brain health: the importance of recognizing cognitive impairment: an IAGG consensus conference. J Am Med Dir Assoc. 2015;16(9):731-9.
Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23(4):306-14.
Chodosh J, Petitti DB, Elliott M, et al. Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc. 2004;52(7):1051-9.
Kotagal V, Langa KM, Plassman BL, et al. Factors associated with cognitive evaluations in the United States. Neurology. 2015;84(1):64-71.
Sabbagh MN, Boada M, Borson S, et al. Early Detection of Mild Cognitive Impairment (MCI) in Primary Care. J Prev Alzheimers Dis. 2020;7(3):165-170.
Petersen RC, Roberts RO, Knopman DS, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66(12):1447-55.
Qin J, He Z, Wu L, et al. Prevalence of mild cognitive impairment in patients with hypertension: a systematic review and meta-analysis. Hypertens Res. 2021;44(10):1251-1260.
Juncos-Rabadán O, Pereiro AX, Facal D, et al. Prevalence and correlates of mild cognitive impairment in adults aged over 50 years with subjective cognitive complaints in primary care centers. Geriatr Gerontol Int. 2014;14(3):667-673.
Luck T, Riedel-Heller SG, Kaduszkiewicz H, et al. Mild cognitive impairment in general practice: age-specific prevalence and correlate results from the German study on ageing, cognition and dementia in primary care patients. Dement Geriatr Cogn Disord. 2007;24(4):307-16.
Lovett RM, Curtis LM, Persell SD, et al. Cognitive impairment no dementia and associations with health literacy, self-management skills, and functional health status. Patient Educ Couns. 2020;103(9):1805-1811.
Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695-9.
Rossetti HC, Lacritz LH, Cullum CM, Weiner MF. Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample. Neurology. 2011;77(13):1272-5.
Davis DH, Creavin ST, Yip JL, Noel-Storr AH, Brayne C, Cullum S. Montreal Cognitive Assessment for the diagnosis of Alzheimer's disease and other dementias. Cochrane Database Syst Rev. 2015;(10):CD010775.
Freitas S, Simoes MR, Alves L, Santana I. Montreal cognitive assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord. 2013;27(1):37-43.
Trittschuh EH, Crane PK, Larson EB, et al. Effects of varying diagnostic criteria on prevalence of mild cognitive impairment in a community based sample. J Alzheimers Dis. 2011;25(1):163-73.
Jak AJ, Preis SR, Beiser AS, et al. Neuropsychological Criteria for Mild Cognitive Impairment and Dementia Risk in the Framingham Heart Study. J Int Neuropsychol Soc. 2016;22(9):937-943.
Busse A, Hensel A, Gühne U, Angermeyer MC, Riedel-Heller SG. Mild cognitive impairment: long-term course of four clinical subtypes. Neurology. 2006;67(12):2176-85.
Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):270-279.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-13.
Ismail Z, Elbayoumi H, Fischer CE, et al. Prevalence of Depression in Patients With Mild Cognitive Impairment: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2017;74(1):58-67.
U.S. Department of Health and Human Services. National Plan to Address Alzheimer’s Disease: 2018 Update. Accessed March 19, 2018. https://aspe.hhs.gov/system/files/pdf/259581/NatPlan2018.pdf
Owens DK, Davidson KW, Krist AH, et al. Screening for Cognitive Impairment in Older Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323(8):757-763.
Athilingam P, Visovsky C, Elliott AF, Rogal PJ. Cognitive screening in persons with chronic diseases in primary care: challenges and recommendations for practice. Am J Alzheimers Dis Other Demen. 2015;30(6):547-58.
van Reekum R, Simard M, Clarke D, Binns MA, Conn D. Late-life depression as a possible predictor of dementia: cross-sectional and short-term follow-up results. Am J Geriatr Psychiatry. 1999;7(2):151-9.
Butters MA, Whyte EM, Nebes RD, et al. The nature and determinants of neuropsychological functioning in late-life depression. Arch Gen Psychiatry. 2004;61(6):587-95.
Nebes RD, Butters MA, Mulsant BH, et al. Decreased working memory and processing speed mediate cognitive impairment in geriatric depression. Psychol Med. 2000;30(3):679-91.
Blair M, Coleman K, Jesso S, et al. Depressive Symptoms Negatively Impact Montreal Cognitive Assessment Performance: A Memory Clinic Experience. Can J Neurol Sci. 2016;43(4):513-7.
Sheffield KM, Peek MK. Changes in the prevalence of cognitive impairment among older Americans, 1993-2004: overall trends and differences by race/ethnicity. Am J Epidemiol. 2011;174(3):274-83.
Sloan FA, Wang J. Disparities among older adults in measures of cognitive function by race or ethnicity. J Gerontol B Psychol Sci Soc Sci. 2005;60(5):P242-50.
Cheng YJ, Kanaya AM, Araneta MRG, et al. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011-2016. JAMA. 2019;322(24):2389-2398.
Khatib R, Glowacki N, Lauffenburger J, Siddiqi A. Race/Ethnic Differences in Atherosclerotic Cardiovascular Disease Risk Factors Among Patients With Hypertension: Analysis From 143 Primary Care Clinics. Am J Hypertens. 2021;34(9):948-955.
Cockerham WC, Hamby BW, Oates GR. The Social Determinants of Chronic Disease. Am J Prev Med. 2017;52(1S1):S5-S12.
Rotblatt LJ, Aiken-Morgan AT, Marsiske M, Horgas AL, Thomas KR. Do Associations Between Vascular Risk and Mild Cognitive Impairment Vary by Race? J Aging Health. 2021:898264320984357.
Rivera Mindt M, Byrd D, Saez P, Manly J. Increasing culturally competent neuropsychological services for ethnic minority populations: a call to action. Clin Neuropsychol. 2010;24(3):429-53.
Rivera Mindt M, Arentoft, A., Coulehan, K., Summers, A. C., Tureson, K., Aghvinian, M., & Byrd, D. A. Considerations for the neuropsychological evaluation of culturally/linguistically diverse older adults. The Handbook on the Neuropsychology of Aging and Dementia (2nd ed). Springer Science + Business Media; 2019.
Acknowledgements
The project described was supported by Award Number R01AG066471 from the National Institute Aging of the National Institutes of Health.
Funding
This work was supported by grant R01AG066471 from the National Institute for Aging.
Author information
Authors and Affiliations
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Federman, A.D., Becker, J.H., Mindt, M.R. et al. Rates of Undiagnosed Cognitive Impairment and Performance on the Montreal Cognitive Assessment Among Older Adults in Primary Care. J GEN INTERN MED 38, 2511–2518 (2023). https://doi.org/10.1007/s11606-023-08102-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08102-w