Abstract
In 2015 and 2016 there were 48 terrorist incidents resulting in 320 deaths and 1227 further casualties in Western Europe alone. The three largest of these incidents were Marauding Terrorist Firearms Attacks (MTFA), accounting for 82% of the total casualties in this period (258 deaths and 1011 casualties) with a median total number of casualties per incident of over 400. Prioritising medical care in the aftermath of these attacks, whilst being aware of tactical constraints, is essential in order to provide an optimal health response.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
7.1 Introduction
In 2015 and 2016 there were 48 terrorist incidents resulting in 320 deaths and 1227 further casualties in Western Europe alone. The three largest of these incidents were Marauding Terrorist Firearms Attacks (MTFA) , accounting for 82% of the total casualties in this period (258 deaths and 1011 casualties) with a median total number of casualties per incident of over 400. Prioritising medical care in the aftermath of these attacks, whilst being aware of tactical constraints, is essential in order to provide an optimal health response.
The health response to an MTFA has historically involved principles explained in the Major Incident Medical Management and Support (MIMMS) training manual [1]. The first casualty contact action in MIMMS is to identify the medical treatment priority of all patients, and in order to do so rapidly mandates that no treatment takes place until this phase is completed. This process is known as triage —a word derived from French ‘trier’ that literally means ‘to sort’, and has its origins in coffee bean selection and latterly to describe a process of prioritising casualties on the basis of their clinical acuity for medical treatment.
The London bombings on 7th July 2005 identified several key lessons for the pre-hospital health response to an MTFA. In response to the Coroner’s inquest a review of the triage system took place, resulting in changes to the MIMMS paradigm: primarily the requirement to undertake immediately life-saving interventions alongside the triage process and the use of a ‘two clinician’ triage system.
Triage systems need to be simple, and rapid, with reproducible results, whilst also allowing for a defined and limited number of immediate lifesaving interventions. This chapter will outline these processes.
7.2 History of Triage
The concept of medical triage was developed by Baron Dominique-Jean Larrey, Chief Surgeon of Napolean’s Imperial Guard (1766–1842) [2]. Larrey’s priority was to maintain fighting effectiveness, and therefore those with minor injuries received treatment first (to allow them to return to the battlefield), followed by the most severely injured.
The next major advancement in triage is attributed to British Naval Surgeon John Wilson (1834–1885), who declared that surgeons should concentrate their efforts on those with an immediate need for treatment and in whom intervention was likely to be successful, whilst deferring the care of those with minor wounds, and those whose wounds were probably fatal.
The term ‘triage’ was in widespread use during the First World War. A military war manual at the time observed: ‘It is often physically impossible to give speedy and thorough treatment to all patients. A single case, even if it urgently requires attention,—if this will absorb a long time,—may have to wait, for in that same time a dozen others, almost equally exigent, but requiring less time, might be cared for. The greatest good of the greatest number must be the rule’ [3].
The treatment priorities of triage have necessarily changed over time, but the underlying principle to give the right patient the right care at the right time remains extant.
7.2.1 Modern Day Triage
The MIMMS practical course and accompanying manual were written in the aftermath of the Musgrave Park Hospital bombing in 1991, and in recognition that healthcare professionals were inadequately prepared for a major incident. The backbone of MIMMS is the now well-known mnemonic ‘CSCATTT ’—a standard, systematic sequence of actions: Command, Safety, Communications, Assessment, Triage, Treatment, Transport [1]. Since its inception in 1994 the principles of MIMMS have been taught to a large number of healthcare professionals in the UK and overseas, and influenced major incident policy.
More recently adaptations to the system of triage have been made in response to the attacks in London in July 2005—these include recommendations for a two-person triage team to allow lifesaving intervention (application of tourniquets to control catastrophic haemorrhage) to be undertaken alongside assigning triage categories. The requirement for adequate supplies of immediate life-saving equipment was further highlighted following the Paris MTFA in November 2015: ‘the demand for tourniquets was so high that the mobile teams came back without their belts’ [4].
The United Kingdom’s National Ambulance Resilience Unit (NARU) was formed in 2011 to help strengthen national resilience and to improve patient outcomes in challenging pre-hospital environments, including the health response to MTFAs. NARU now provides national level guidance for the command and control, and management of incidents involving a large number of casualties [5].
Today there are numerous different triage systems in place around the world—this is likely to reflect both evolution in response to specific incidents, and the recognition that one triage system may not be applicable to all types of major incident.
7.3 Principles of Triage
7.3.1 Triage: When?
Triage takes place day-to-day in most healthcare systems. In the UK this typically starts with the Ambulance Service call taker using a pre-defined set of questions to initiate the most suitable response. In order that the seriously unwell and injured are dealt with expediently and appropriately this system must be rapid, reliable, and reproducible. This sorting process (triage) continues at every step of the casualty’s journey in order that they receive the right healthcare, at the right facility, and at the right time—these are the fundamental principles of triage (Box 7.1).
Box 7.1 Fundamental principles of triage
-
Triage is a routine process in healthcare
-
It should be rapid, reliable, and reproducible (irrespective of the provider delivering it)
-
Effective triage results in the right patient receiving the correct healthcare at the most appropriate facility, at the right time.
In a major incident this process is even more important, as by definition it is a situation in which the number, type, or location of live casualties requires extraordinary resources. Therefore for optimal outcomes there must be a system in place that makes the best use of available resources.
The physiological state of casualties changes over time in response to both injury and interventions, triage must therefore be regularly repeated. In the major incident setting triage will occur numerous times; on first contact, before moving the casualty, in a casualty clearing station, prior to evacuation to hospital, and again on arrival at hospital.
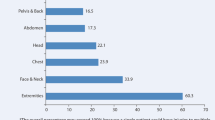
It is unrealistic to expect healthcare providers to do something in a major incident that they do not do regularly. Deliberate practice of triage should be supported by routine use (for example at any incident with a greater number of casualties than providers), and through major incident exercises. In recognition of this principle NARU have modified the UK civilian triage system to follow the day-to-day patient assessment paradigm of <C>ABC (Fig. 7.1).
7.3.2 Triage: Who?
Large-scale incidents, including MTFAs, have repeatedly shown to be disorganised, and it is likely that the first medical responders will be drawn into providing care to casualties that they first encounter (rather than initiating systematic triage). As soon as effective command, safety, communications, and scene assessment have taken place an effective triage system should be implemented. NARU guidance dictates the use of two-person triage teams to rapidly; triage casualties, apply triage labels, keep a casualty record, and perform a limited number of lifesaving interventions.
An underlying principle of triage is that it must be rapid, simple, and reproducible. A triage system should allow any pre-hospital provider to undertake primary triage; with appropriate training this could be extended to Fire and Rescue Service, Police, and military personnel.
Subsequent pre-hospital triage is likely to be undertaken by designated personnel, for example a Triage Officer. Utilising these specifically trained personnel may allow a more detailed casualty assessment, for example by including anatomical injury and mechanism of injury in decision-making. These more complex triage processes aim to increase sensitivity and specificity, and therefore reduce over and under-triage, in order to better categorise patients. However, this secondary triage is more time-consuming, and requires a higher level of clinical experience, it is therefore not suitable for the initial clinical assessment.
On arrival to hospital senior medical staff will use a combination of physiology, anatomical injury, and clinical acumen to further prioritise patients for medical treatment. The differentiation of primary triage and secondary triage is explicit in some systems, and in the UK is described using the ‘Triage Sieve’ and ‘Triage Sort’ respectively; these are further explained in the next section.
7.3.3 Triage Outcomes
The purpose of triage is to categorise casualties on the basis of their clinical acuity. Traditionally, irrespective of the system used, casualties are allocated to one of three categories corresponding to their urgency, this is summarised in Table 7.1.
The priority 4 or expectant category exists for casualties who, even with maximal medical attention are unlikely to survive. This category is implemented at the discretion of the overall operational “gold” commander and is reserved for exceptional situations.
Existing UK doctrine states priority one (immediate) patients require life-saving interventions immediately (for example decompression of a tension pneumothorax), priority two (urgent) patients require intervention within 4–6 h, and that priority three (delayed) patients can receive intervention after this time.
Historically triage systems have been validated against injury scores, aiming to predict those sustaining major trauma and convey them to the most appropriate hospital. However, it is well recognised that the injury severity score and need for life-saving intervention do not correlate, and within a MTFA or major incident setting the latter (the need for intervention) is the more appropriate measure [6, 7].
Although it is recognized internationally that the priority one (immediate) casualty is one whom requires a life-saving intervention, the definition of ‘life-saving intervention’ has only recently been defined. Expert consensus defined these as being interventions required within 1 h (Box 7.2) [8]. Whilst consensus exists for the priority one casualty, there is currently no good understanding of the timing requirements for the less urgent clinical categories, priorities two and three.
Box 7.2 Consensus definition of Priority One defining life-saving intervention (adapted from Ref. [8])
1 | Intubation for actual or impending airway obstruction. |
2 | Surgical airway for actual or impending airway obstruction. |
3 | Thoracostomy (needle/finger/tube). |
4 | Application of a chest seal (commercial/improvised). |
5 | Positive pressure ventilation for ventilatory inadequacy. |
6 | Application of a tourniquet for haemorrhage control. |
7 | Use of haemostatic agents for haemorrhage control. |
8 | Insertion of an intra-osseous device for resuscitation purposes. |
9 | Receiving uncross-matched blood. |
10 | Receiving ≥4 units of blood/blood products. |
11 | Administration of tranexamic acid. |
12 | Laparotomy for trauma. |
13 | Thoracotomy or pericardial window for trauma. |
14 | Surgery to gain proximal vascular control. |
15 | Interventional radiology for haemorrhage control. |
16 | Application of a pelvic binder. |
17 | ALS/ALS for a patient in a peri-arrest/cardiac arrest situation. |
18 | Neurosurgery for the evacuation of an intra-cranial haematoma. |
19 | Craniotomy/Burr hole insertion. |
20 | Spinal nursing for a C1-3 fracture. |
21 | Administration of a seizure-terminating medication. |
22 | Active/passive rewarming for initial core temp <32 °C. |
23 | Correction of low blood glucose. |
24 | Administration of chemical antidotes. |
7.4 Current Triage Systems
7.4.1 Primary Triage
There are multiple different triage systems in use internationally:
The UK currently employs the New Triage Sieve, commissioned by the National Ambulance Service Medical Directors Group in 2013 and delivered by the National Ambulance Resilience Unit (Fig. 7.1). The New Triage Sieve is an adaptation of the MIMMS triage sieve, and uses rapidly identifiable casualty characteristics and physiology to allocate priorities. The first action is to apply a tourniquet to catastrophic haemorrhage, this automatically makes a casualty P1. This is followed by identifying those with no injuries, signposted to a survivor reception centre and assigning the walking wounded P3 status. Subsequent assessment of airway, consciousness, respiratory rate, and circulation sieves casualties into dead, T1, and T2 categories. This system recognises that clinicians use the <C>ABC paradigm day-to-day, which starts with ‘catastrophic haemorrhage’ and therefore should use the same system during a major incident. This is in contrast to the UK military sieve, which starts by differentiating walking casualties as injured or not injured, followed by a similar assessment to that of the New Triage Sieve (Table 7.2).
The ‘Simple Triage And Rapid Treatment’ (START) triage system was developed in the US in 1983 and is designed for use by rescuers with basic first aid skills. START allocates priority categories, immediate, delayed, minor and dead, in a similar method to the UK military sieve—starting with identifying walking casualties. START includes an assessment of catastrophic haemorrhage, airway, breathing, circulation, and mental status—those that cannot obey commands are priority one ‘immediate’ (Table 7.2).
In 2001 the Care Flight triage system was introduced with the intent of standardising the initial health response to a major incident in Australia. This system is notably different to UK systems and START in that it does not require any physiological monitoring. Care Flight triage starts with assigning the walking casualties a delayed priority, followed by assessment of ability to obey commands, breathing, and radial pulse presence. The simplicity of this system means it is rapid, and suitable for casualties of all ages (Table 7.2).
A number of studies looking at triage tool performance both within a trauma registry and retrospectively following a major incident, have demonstrated that existing triage tools have poor performance at identifying those in need of a life-saving intervention [9, 10]. Within a civilian trauma registry dataset, all triage tools demonstrated poor sensitivity, corresponding to an inappropriately high rate of under-triage and thus failing to identify those in need of life-saving intervention. However, despite low sensitivity, all triage tools had in excess of 90% specificity, yielding a very low rate of over-triage [11].
7.4.2 Secondary Triage
Triage is a dynamic process, and as previously stated should be repeated at each stage of the casualty’s transition from scene to hospital. This process serves not only to alert the healthcare provider to subsequent deterioration, but also to assess any response from treatments already given.
Within both the UK military and civilian setting, a formal secondary triage assessment, using the Triage Sort is undertaken, again allocating the casualty to one of three categories. Existing major incident doctrine suggests that secondary triage should be performed when the situation permits.
Based on the Revised Trauma Triage Score, the Triage Sort uses a ranking system to provide an additional assessment of the casualty’s physiology. Unlike the Triage Sieve, this includes a systolic blood pressure measurement and an assessment of conscious level using the Glasgow Coma Scale (Fig. 7.2).
Whilst the aim of the Triage Sort is to further refine the triage decision, evidence from military studies suggest that it is no better than existing primary triage methods at predicting the priority one ‘immediate’ casualty [12].
The use of senior clinicians’ gestalt can be considered an additional form of secondary triage; not only has it been used in the past, but in addition, features as the final step in the Triage Sort. Methodologically however, it is not a protocolled assessment and is not only dependent on the resources available at the incident, but also the experiences of the clinician involved. Whilst difficult to quantify what is essentially a qualitative process, Israeli experience of senior clinician gestalt demonstrated only 50% sensitivity for predicting severe injury [13].
7.4.3 Casualty Labeling
Once a casualty has had a triage category assigned, there is a need to both differentiate their category from others and to identify that they have been triaged. The labeling system used needs to be dynamic to changes in the casualty’s condition, be easily attached to the casualty, weather-proof, and ideally allow unique numbering as well as an area for concise medical notes.
The cruciform card and the Smart Tag system (commonly used in UK civilian and military settings respectively) both allow re-folding of the same card to change a triage category, while also including space for brief medical notes as well as a unique numbering system.
Not all methods of triage labeling include a label for the priority four, expectant category. If the expectant category has been authorized by the senior Gold command, those performing triage must be aware of their local procedure of how to identify such casualties.
7.5 Triage Systems Research
There is increasing evidence to demonstrate that existing triage tools have poor performance at predicting those in need of a life-saving intervention, the priority one (immediate) patient [9, 14]. The development of an effective triage method is therefore an important research priority in improving trauma care during a major incident.
In an ideal setting, like any diagnostic test, the triage method utilised will have both 100% sensitivity and specificity. However in practice, the optimal performance of a triage tool lies in the balance between sensitivity and specificity, correlating with rates of over and under-triage. Whilst an over-triage rate of 65% was tolerated following the London 7/7 bombings [15], this level of over-triage may well overwhelm a more rural setting with fewer healthcare facilities immediately available.
Guidance currently exists for measuring the performance of field triage, a process that utilises a combination of anatomical, mechanism, physiological and clinician gestalt assessments. For the field triage process, both the American College of Surgeons (ACS) and the Centers for Disease Control (CDC) suggest that tolerable thresholds are a rate of 5% under-triage and 35% over-triage. For the major incident setting, the ACS simply state that both under and over-triage should be kept to a minimum [16, 17].
The New Triage Sieve adopted by the UK follows the <C>ABC paradigm (Fig. 7.1). A review of patients presenting to the Royal London Hospital following the 7/7 London bombings demonstrated only three patients with injuries that would be consistent with requiring tourniquet application [18]. Although it was noted at the coroners inquest that make shift tourniquets were used by police who enter the scenes in the early phases [19]. In comparison, the experience from the 2015 Paris MTFA clearly supports this addition to the New Triage Sieve [4]. The likely requirement for controlling catastrophic haemorrhage will be dependent on the mechanism of the major incident (e.g. London 7/7 vs Paris MTFA) and the injuries sustained. It is unlikely to be required in all major incidents, but the concept of a simple life-saving intervention (if required) incorporated within a triage algorithm is sensible and is unlikely to grossly delay the triage process.
Work within the UK military has been undertaken to identify the optimum physiological thresholds for identifying those in need of life-saving intervention [20]. Derived specifically for this purpose, the physiological parameters within the Modified Physiological Triage Tool (MPTT) have been optimised to predict the need for life-saving intervention. Within both a military and civilian environment this has the greatest sensitivity at identifying the priority one patient. However this comes at the expense of a high rate of over-triage, although within a civilian setting this was found to be comparable to that observed following 7/7.
An initially high level of over-triage should be accepted at a major incident, as without this, large numbers of genuine priority one patients are likely to be missed. Once the casualty has been removed from the ‘front line’ of the incident, to a more permissive area, a secondary triage process, which yields a reduced rate of over-triage can be undertaken in order to refine the casualty’s category.
The existing method of secondary triage, the Triage Sort , performs poorly in this role, further research is required to optimize the secondary triage process. Early military studies have shown that the use of the Shock Index (HR/SBP) shows improved performance over the Triage Sort at predicting the need for life-saving intervention [12]. From UK civilian studies it is observed that the groups most frequently under-triaged are those sustaining injuries to the thoracic region. By using a combination of physiological and anatomical assessments, similar to that observed in the field triage process, it is likely that the secondary triage process can be improved considerably.
Providing a modified two-tiered triage approach like this to a major incident will reduce the overall over-triage rate of an incident and reduce the critical mortality that has previously been associated with over-triage.
7.6 Summary
The concept of triage in clinical practice arose from the contingencies and demands of armed conflict. In modern times triage is practiced routinely in most healthcare settings, and exceptionally in response to major incidents and MTFAs. If simple and effective to use, regularly exercised and widely understood, triage systems ensure the optimal care of a group of casualties in times of limited resources. Triage systems should continue to be developed in response to evolving threats in order to fulfill the underlying principle—to give the right patient the right care, at the right time, and in the right place.
References
Mackway-Jones K. In: Mackway-Jones K, editor. Major incident medical management and support: the practical approach at the scene. 3rd ed. Chichester: Wiley-Blackwell; 2012.
Iserson KV, Moskop JC. Triage in medicine, part I: concept, history, and types. Ann Emerg Med. 2007;49(3):275–81.
Keen WW. The treatment of war wounds. Philadelphia: WB Saunders; 1917.
Hirsch M, Carli P, Nizard R, Riou B, Baroudjian B, Baubet T, et al. The medical response to multisite terrorist attacks in Paris. Lancet. 2015;386(10012):2535–8.
National Ambulance Service Command and Control Guidance. National Ambulance Resilience Unit. V1.2. October 2015. Available at: https://naru.org.uk/document-category/naru-publications/. Accessed 6 Jan 2017.
Baxt WG, Upenieks V. The lack of full correlation between the Injury Severity Score and the resource needs of injured patients. Ann Emerg Med. 1990;19(12):1396–400.
Wallis L, Carley S, Hodgetts CT. A procedure based alternative to the injury severity score for major incident triage of children: results of a Delphi consensus process. Emerg Med J. 2006;23(4):291–5.
Vassallo J, Smith JE, Bruijns SR, Wallis LA. Major incident triage: a consensus based definition of the essential life-saving interventions during the definitive care phase of a major incident. Emerg Med J. 2016;47(9):1898–902.
Challen K, Walter D. Major incident triage: comparative validation using data from 7th July bombings. Injury. 2013;44(5):629–33.
Garner A, Lee A, Harrison K, Schultz CH. Comparative analysis of multiple-casualty incident triage algorithms. Ann Emerg Med. 2001;38(5):541–8.
Smith JE, Vassallo J. Major incident triage: the civilian validation of the modified physiological triage tool. Emerg Med J. 2016;33(12):908.
Vassallo J, Horne S, Ball S, Smith JE. Usefulness of the Shock Index as a secondary triage tool. J R Army Med Corps. 2015;161(1):53–7.
Ashkenazi I, Kessel B, Khashan T, Haspel J, Oren M, Olsha O, Alfici R. Precision of in-hospital triage in mass-casualty incidents after terror attacks. Prehosp Disaster Med. 2006;21(1):20–3.
Vassallo J, Horne S, Ball S, Whitley J. UK Triage the validation of a new tool to counter an evolving threat. Injury. 2014;45(12):2071–5.
Aylwin CJ, König TC, Brennan NW, Shirley PJ, Davies G, Walsh MS, Brohi K. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. 2006;368(9554):2219–25.
American College of Surgeons. Resources for optimal care of the injured patient 2014. Chicago: American College of Surgeons, Committee on Trauma; 2014.
Sasser SM, Hunt RC, Sullivent EE, Wald MM, Mitchko J, Jurkovich GJ, et al. Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage. MMWR Recomm Rep. 2009;58:1–35.
Challen KHE. Comparative validation of major incident triage systems. MRes Thesis. University of Manchester; 2008.
Transcripts from coroners inquest into 7 July 2005. National archives. http://webarchive.nationalarchives.gov.uk/20120216072438/http://7julyinquests.independent.gov.uk/hearing_transcripts/19102010pm.htm. Accessed 20 Feb 2017.
Vassallo J, Beavis J, Smith JE, et al. Major incident triage: derivation and comparative analysis of the Modified Physiological Triage Tool (MPTT). Injury. 2017;48(5):992–9. https://doi.org/10.1016/j.injury.2017.01.038.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Barnard, E., Vassallo, J. (2017). Triage. In: Breeze, J., Penn-Barwell, J., Keene, D., O'Reilly, D., Jeyanathan, J., Mahoney, P. (eds) Ballistic Trauma. Springer, Cham. https://doi.org/10.1007/978-3-319-61364-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-61364-2_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61363-5
Online ISBN: 978-3-319-61364-2
eBook Packages: MedicineMedicine (R0)