Abstract
Invasive tumor growth is associated with extensive remodeling of the surrounding extracellular matrix (ECM). Degradation of the original ECM scaffolds, which primarily consist of collagens, is key to the morbidity of the cancer as it leads to destruction of the original tissue and replacement with cancerous tissue. The degradation of collagen involves the cleavage of collagen fibers by extracellular proteases and the subsequent receptor-mediated internalization of large collagen fragments for lysosomal degradation. The extracellular cleavage reactions are typically mediated by matrix metalloproteinases (MMPs) that cleave the collagen strands at specific sites, thereby releasing defined collagen fragments. The intracellular collagen degradation pathway is primarily mediated by two endocytic receptors, uPARAP/Endo180 and the mannose receptor (MR), that bind collagen fragments at the cell surface and direct them to the lysosomes for complete proteolytic degradation. Macrophages and most mesenchymal cells can internalize collagen through the action of MR and uPARAP/Endo180, respectively. These receptors bind preferentially to cleaved collagen and cooperate with MMPs to degrade collagen fibers in a sequential process involving MMP-mediated collagen cleavage followed by receptor-mediated internalization of collagen fragments for lysosomal degradation. In vivo, MR-mediated collagen uptake has been suggested to be dominant in many situations with uPARAP/Endo180 playing a smaller role. In connection to cancer, uPARAP/Endo180 is often upregulated and mostly restricted to cancer-associated fibroblasts, and the action of uPARAP/Endo180 promotes tumor growth and counteracts the development of fibrosis. MR is expressed by M2 macrophages in healthy dermis and in solid tumors and mediates the efficient internalization of collagen. However, the direct functional consequences of this MR-mediated collagen degradation for cancer growth and invasion still need to be investigated.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
2.1 Collagen Degradation in Cancer
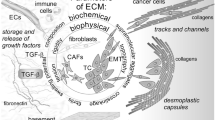
During the invasive growth of solid tumors, extensive remodeling of the surrounding extracellular matrix (ECM) occurs (Bonnans et al. 2014). The original ECM scaffolds, which primarily consist of collagens, are degraded, and this contributes to the destruction of the original tissue and replacement with cancerous tissue. The degradation of the ECM furthermore releases pro-tumorigenic growth factors embedded in the matrix (Kessenbrock et al. 2010), and the degradation of the basement membrane, a specialized sheetlike ECM structure, is considered a prerequisite for cancer invasion and metastasis to take place (Rowe and Weiss 2008). Within the last decade, several seminal papers have revealed that another critical consequence of the degradation of the original ECM follows from the fact that this process is accompanied by the excessive deposition of new matrix proteins (Cox and Erler 2011; Lu et al. 2012). These dynamics result in the generation of a novel ECM, which can have a very different composition, organization, and stiffness (Schedin and Keely 2011; Cox and Erler 2014; Bonnans et al. 2014). Often the deposited tumor-specific ECM is of increased stiffness and rich in collagen type I and sometimes also includes variants of matrix proteins that are not typically observed in adults (Schedin and Keely 2011; Cox and Erler 2011; Giblin and Midwood 2015). The altered tumor-specific ECM critically influences the biology of the tumor to ultimately promote tumor growth and metastasis (Joyce and Pollard 2009; Pyonteck et al. 2013; Pickup et al. 2014; Nagelkerke et al. 2015).
In connection to breast cancer, the ECM stiffness and orientation of the collagen fibers critically affect the prognosis of the patients (Conklin et al. 2011; Bredfeldt et al. 2014; Acerbi et al. 2015). The ECM stiffness is primarily determined by the density of deposited collagen and the degree of cross-linking mediated mainly by the enzyme LOX (Levental et al. 2009; Cox and Erler 2011). Furthermore, the density of normal breast tissue correlates strongly with the risk for development of breast cancer (Guo et al. 2001; Boyd et al. 2007). Interestingly, breast epithelial cells respond to increased ECM stiffness in vitro by losing polarity, by proliferating more, and by acquiring a phenotype in many ways resembling malignant transformation (Paszek et al. 2005; Levental et al. 2009).
Collagens are the main protein components of the ECM, although the ECM encompasses many other components including fibronectin, elastin, laminin, entactin, and proteoglycans (Lu et al. 2012). Collagen type I is the main fibrillar collagen of the ECM, and extremely large collagen type I deposits can be observed in connection to cancer (Provenzano et al. 2008; Lu et al. 2012). Collagen type IV is another critical collagen as it together with laminin is the predominant constituent of the basement membrane (Rowe and Weiss 2008). Only a limited number of secreted or cell membrane-anchored proteases can cleave ECM proteins, and the majority of these proteases belong to the matrix metalloproteinase (MMP) family (Kessenbrock et al. 2010). The activity of MMPs is usually low in tissues under steady-state conditions but increases dramatically under inflammatory conditions including cancer (Egeblad and Werb 2002; Madsen and Bugge 2015). The functional implications of MMPs in cancer have consequently been studied extensively, but broad-spectrum MMP inhibition for cancer treatment has, however, failed to show any effect on survival of the patients in clinical trials (reviewed by Coussens et al. 2002). The reason for this failure most likely relates to the fact that MMP functions are much more diverse than originally believed and not only pro-tumorigenic (Martin and Matrisian 2007; López-Otín et al. 2009; Decock et al. 2011). In addition to remodeling of the ECM, MMPs can also initiate signaling by releasing or activating growth factors (Egeblad and Werb 2002; Kessenbrock et al. 2010) or prevent downstream signaling processes by shedding signaling receptors from the cell surface (Sanderson et al. 2006; Atapattu et al. 2014). Furthermore, the understanding of the role of ECM in cancer progression has increased tremendously over the last decade, and we now know that the ECM is not just an inert physical barrier that needs to be degraded for the cancer cells to invade the surrounding tissue. Rather it provides the tumor cells with multiple cues that affect the biology and function of cancer cells, stromal cells, and infiltrating immune cells (Lu et al. 2011; Salmon et al. 2012; Pickup et al. 2014).
2.2 Extracellular Collagen Degradation
Collagen type I is the most abundant type of collagen and it is the main protein constituent of interstitial ECM. The extracellular cleavage of collagen type I is primarily mediated by MMP-1, MMP-2, MMP-8, MMP-13, and MMP-14 (Krane and Inada 2008; Fields 2013). In the specific case of osteoclast-mediated collagen degradation, the cysteine protease cathepsin K is responsible for the degradation that takes place in low-pH resorption pits formed between the bone surface and the cell (Saftig et al. 1998). MMP-mediated cleavage of collagen type I occurs at defined sites on the polypeptide chains, and the triple-helical collagen strands are especially susceptible to proteolytic cleavage after residue 775 of the α1- and α2-chain of type I collagen (Highberger et al. 1979; Fields 2013). This cleavage reaction results in the release of a large three quarter collagen fragment also designated TCA, and a small one quarter collagen fragment also designated TCB. The released one quarter and three quarter collagen fragments partially denature at physiological temperatures making the fragments susceptible to cleavage by other proteases such as the secreted gelatinases MMP-2 and MMP-9 (Hipps et al. 1991) and perhaps also the membrane-anchored serine protease fibroblast activation protein (FAP) (Park et al. 1999; Fan et al. 2015). The detailed molecular mechanisms of MMP-mediated cleavage of collagen have been thoroughly reviewed (Fields 2013). MMPs are upregulated in most solid cancers where they contribute to the cancer-associated collagen degradation (Egeblad and Werb 2002). The MMP-mediated remodeling of interstitial collagen is an essential part of invasive tumor growth, and degradation of collagen type IV, which is the main component of the basement membrane, is essential for the metastatic spread of the cancer (Tryggvason et al. 1987; Rowe and Weiss 2008). Both cancer cells and stromal cells can contribute to the increased levels of MMPs in the tumor microenvironment, but in many cases the stromal cells, such as fibroblasts and macrophages, appear to be the primary source of MMPs (Madsen and Bugge 2015).
The MMP-mediated cleavage of collagen is an extracellular event that has been the subject of numerous studies over the last 50 years, but interestingly an intracellular collagen degradation mechanism, which appears to be centrally engaged in collagen degradation as well, has received much less attention. This pathway involves receptor-mediated internalization of collagen for lysosomal degradation and cooperates with extracellular proteolysis for the complete degradation of insoluble collagen fibers. The rest of this book chapter will focus on this important part of the collagen degradation process.
2.3 Intracellular Collagen Degradation
The possibility that internalization of collagen for lysosomal degradation is a physiologically relevant collagenolytic pathway was suggested more than five decades ago based on electron microscopy evaluation of various tissues (Cullen 1972; Scherft and Heersche 1975; Garant 1976; Beertsen and Everts 1977). In these studies it was observed that in several locations and conditions, cells could display intracellular collagen-containing vacuoles. The intracellular collagen was in the form of crossbanded collagen fibrils strongly suggesting that it had been internalized from the extracellular space and did not represent newly synthesized collagen. These early electron microscopy-based studies on collagen internalization have been reviewed excellently (Everts et al. 1996).
Using ex vivo assays, the ability of cells to internalize collagen has been demonstrated, and these types of studies opened up the possibility to investigate the uptake mechanism in more detail. Upon internalization, collagen is routed to the lysosomes where especially cysteine proteases such as cathepsin B and cathepsin L complete the degradation process (Everts et al. 1985; van Noorden and Everts 1991; Creemers et al. 1998). Obvious candidate cell surface receptors for collagen binding were β1-integrins, which are central collagen receptors that support adhesion and migration on collagen surfaces (Mettouchi and Meneguzzi 2006; Leitinger and Hohenester 2007). β1-integrins are not classical endocytosis receptors, but in several papers they have been described to have an impact on the cellular internalization of collagen-coated fluorescent polystyrene beads mimicking the uptake of large collagen particles (Lee et al. 1996; Segal et al. 2001). More recently, many other studies on cellular collagen internalization have, however, indicated that a different family of collagen receptors is even more critical for efficient collagen internalization.
2.3.1 The Collagen Internalization Receptor uPARAP/Endo180
About 25 years ago, two independent research groups identified a cell surface receptor, which later turned out to be a novel collagen receptor (Isacke et al. 1990; Behrendt et al. 1993). This receptor was identified as a surface antigen on fibroblasts (Isacke et al. 1990) and as a receptor that could in certain cell types be enzymatically crosslinked to the urokinase receptor (uPAR) (Behrendt et al. 1993). Later on, protein purification, peptide sequencing, and cloning of the full-length cDNA encoding the proteins revealed that the two receptors were indeed the same protein (Behrendt et al. 2000; Sheikh et al. 2000). The receptor was named Endo180 or uPAR-associated protein (uPARAP) (alternative names are CD280 and MRC2) and was found to be an endocytic receptor belonging to the mannose family, which consists of four members: the mannose receptor (MR), uPARAP/Endo180, PLA2R, and DEC-205. All four receptors are constitutively active endocytosis receptors that can internalize their ligands and deliver them for lysosomal degradation whereas the receptors recycle back to the cell surface (East and Isacke 2002). The four receptors share a very similar protein domain composition that includes a fibronectin type II (FN-II) domain in the N-terminal part of the protein (Fig. 2.1a). FN-II domains are found in fibronectin and in MMP-2 and MMP-9, and here they mediate the binding to collagen type I (Bányai and Patthy 1991; Bányai et al. 1994). In line with this function of FN-II domains, solubilized collagen can be very efficiently internalized by cultured fibroblasts in a completely uPARAP/Endo180-dependent manner (Fig. 2.1b–c) (Engelholm et al. 2003; East et al. 2003; Kjøller et al. 2004; Madsen et al. 2011). So far collagens of type I, II, IV, V, and VI and gelatin have been tested and found to be ligands for uPARAP/Endo180 (Engelholm et al. 2003; East et al. 2003; Wienke et al. 2003), but no binding to other non-collagenous proteins including fibronectin, laminin, and vitronectin has been observed. It should, however, be noted that it has been demonstrated that fibronectin, when incorporated into a collagen matrix, can be internalized in a uPARAP/Endo180-dependent manner (Shi et al. 2010), probably reflecting the co-internalization of collagen and fibronectin. The collagen-binding capacity of uPARAP/Endo180 is contained within the three N-terminal domains, which include the FN-II domain (Wienke et al. 2003; Jürgensen et al. 2011; Jürgensen et al. 2014). In addition, the fourth protein domain, which is a calcium-dependent lectin-like (CTLD) domain, contributes to the binding to glycosylated collagen forms (Jürgensen et al. 2011).
uPARAP/Endo180 and the mannose receptor (MR) are endocytic collagen receptors. (a) Schematic representation of the domain composition of uPARAP/Endo180 and MR. uPARAP/Endo180 and MR share an identical domain composition staring with an N-terminal cysteine-rich domain (Cys-rich), followed by a fibronectin type II domain (FN-II), 8 C-type lectin-like domains (CTLDs), a transmembrane-spanning region, and a small cytoplasmic domain. (b and c) Fibroblasts internalize collagen in a uPARAP/Endo180-dependent manner. Cellular internalization of fluorescent collagen by wild-type (b) and uPARAP/Endo180-deficient fibroblasts (c) analyzed using confocal microscopy. Cells were incubated with Oregon Green-collagen IV (green) to allow endocytosis, followed by cell surface staining (red). The intracellular punctuate pattern of collagen indicates localization in endosomal/lysosomal compartments. Scale bar, 20 μm. (b and c) were adapted from Kjøller et al. (2004) with permission from Elsevier
Using single particle electron microscopy, a low-resolution three-dimensional structure of uPARAP/Endo180 has been solved (Rivera-Calzada et al. 2003; Boskovic et al. 2006). At neutral pH, the four N-terminal domains adopt a bent conformation, where the cysteine-rich (Cys-rich) domain contacts CTLD-2, but at pH 5.4 the receptor acquires a more extended conformation. This conformational change might relate to the ligand release mechanism of the receptor in the slightly acidic endosomes. Recently a high-resolution crystal structure of a truncated version of uPARAP/Endo180, consisting of the four N-terminal domains, has been solved (Paracuellos et al. 2015). This part of uPARAP/Endo180 forms a more open L-shaped structure that is unaffected by changes in pH, suggesting that the previously observed bent confirmation might instead involve an interaction between the N-terminal Cys-rich domain and CTLD-3 (Paracuellos et al. 2015).
In cellular assays in which fibroblasts are presented with solubilized forms of collagen, efficient and completely uPARAP/Endo180-dependent collagen internalization occurs. Furthermore, the uptake of solubilized collagen is independent of β1-integrin activity, which is in contrast to the reports on cellular uptake of collagen-coated beads (Madsen et al. 2011). The observed differences most likely reflect the different assay systems used. When fibroblasts are presented with an insoluble collagen matrix resembling native collagen fibers, uptake of collagen material occurs in a process that appears to be dependent on both uPARAP/Endo180 and β1-integrins (Shi et al. 2010). Strikingly, however, it has been demonstrated in another study that the conditioned media from uPARAP/Endo180-deficient fibroblasts cultured on a collagen matrix contain collagen fragments that correspond to the one quarter and three quarter fragments generated by MMP-mediated cleavage (Fig. 2.2a–b) (Madsen et al. 2007). In contrast, littermate wild-type fibroblasts have the ability to internalize and degrade the released collagen fragment, thereby leaving no large collagen fragments in the conditioned media. This strongly suggests that fibroblasts degrade collagen in a sequential process initiated by MMP-mediated cleavage of insoluble collagen fibers, followed by uPARAP/Endo180-mediated uptake of the released one quarter and three quarter collagen fragments. In accordance with these findings, biochemical analysis of the protein interaction between uPARAP/Endo180 and collagen revealed that collagen upon denaturation binds with an increased association rate to uPARAP/Endo180 (Leitinger and Hohenester 2007; Madsen et al. 2007; Jürgensen et al. 2011; Paracuellos et al. 2015). The one quarter and three quarter collagen fragments, which shift to a partially denatured state at 37 °C (Stark and Kühn 1968; Danielsen 1987), similarly show a more rapid binding to uPARAP/Endo180 compared to intact full-length collagen (Madsen et al. 2007). Consistently, MMP-generated collagen fragments are also internalized more efficiently than intact collagen (Fig. 2.2c–f).
Fibroblasts internalize MMP-generated collagen fragments in a uPARAP/Endo180-dependent manner. (a and b) uPARAP/Endo180 is indispensable for complete degradation of insoluble collagen fibers by fibroblasts. (a) Schematic overview of the experimental setup used for investigating the complete process of cellular collagen degradation. Fibroblasts were cultured for 5 days on top of an insoluble collagen matrix with a tracer of radiolabeled collagen included after which the cell culture supernatant was analyzed for the presence of collagen fragments. (b) SDS-PAGE and phosphorimager analysis shows that collagen fragments accumulate in the conditioned media of uPARAP/Endo180-deficient fibroblasts (lane 4). These fragments are cleared from the conditioned media by wild-type fibroblasts (lane 3). Intact collagen (lane 1) and MMP-13-generated collagen fragments (lane 2) are included for comparison. (e–f) MMP-generated collagen fragments are internalized more efficiently than intact collagen. Cellular internalization of MMP-13-cleaved (c and d) and intact (e and f) fluorescent collagen type I (green) by wild-type (c and e) or uPARAP/Endo180-deficient fibroblasts (d and f). A was adapted from Madsen et al. (2011), and (b–f) were adapted from Madsen et al. (2007)
The initial fragmentation of the insoluble collagen matrix is mainly mediated by MT1-MMP (Lee et al. 1996; Holmbeck et al. 1999; Ingvarsen et al. 2013), and this process is very likely facilitated by β1-integrin-mediated cellular interactions with the matrix (Segal et al. 2001; Hynes 2002; Shi et al. 2010). In addition, the membrane-anchored serine protease FAP can facilitate collagen internalization by participating in the further fragmentation of one quarter and three quarter collagen fragments (Fan et al. 2015). The internalized collagen fragments are finally routed to the lysosomes for complete degradation through the action of cysteine cathepsins (Kjøller et al. 2004; Mohamed and Sloane 2006; Madsen et al. 2007).
Altogether it is suggested that fibroblast-mediated collagen degradation occurs in a sequential process initiated by MMP-mediated cleavage of large insoluble collagen fibers followed by uPARAP/Endo180-mediated uptake of the released collagen fragments for lysosomal degradation (Fig. 2.3).
Collagen is degraded in a sequential process that requires receptor-mediated collagen internalization. Schematic representation of the collagen degradation process. The degradation process is initiated by proteolytic attack of insoluble collagen fibers to release defined soluble collagen fragments. This extracellular cleavage reaction is primarily mediated by the collagenolytic MMPs, such as MT1-MMP. The released collagen fragments bind to MR or uPARAP/Endo180 on the surface of M2 macrophages or fibroblast-like cells, respectively. The collagen fragments are internalized and routed to the lysosomes for complete degradation. Cysteine cathepsins are essential for the lysosomal degradation of collagen
2.3.2 The Collagen Internalization Receptor MR
uPARAP/Endo180 was initially identified as a novel fibroblast antigen, and in culture essentially all mesenchymal cells express uPARAP/Endo180. In addition to fibroblasts, this includes osteoblasts, chondrocytes, hepatic stellate cells, pancreatic stellate cells, glioma cells, and various sarcoma cell lines (Mousavi et al. 2005; Wagenaar-Miller et al. 2007; Mousavi et al. 2009; Huijbers et al. 2010; Madsen et al. 2011; Takahashi et al. 2011; Madsen et al. 2012; Ikenaga et al. 2012). uPARAP/Endo180 shows the highest degree of homology with the mannose receptor (MR, alternative names are CD206 and MRC1), which is a receptor that is primarily expressed by subsets of macrophages and by liver sinusoidal endothelial cells. MR has mainly been investigated as a receptor for certain pathogens and a potential key receptor involved in innate immunity. Based on the homology with uPARAP/Endo180, it was hypothesized that collagen could be a novel ligand for MR, and it has indeed been demonstrated that MR can bind and internalize collagens with efficiency and binding specificity very similar to that of uPARAP/Endo180 (Martinez-Pomares et al. 2006; Malovic et al. 2007; Jürgensen et al. 2011, 2014; Madsen et al. 2011). The collagen-binding capacity of MR is localized to the FN-II domain containing N-terminus (Napper et al. 2006; Jürgensen et al. 2014), and it has been suggested that multimerization of the receptor is required for efficient binding of collagen on the cell surface (Martinez-Pomares et al. 2006). In a direct comparison of the four receptors from this family, it has been shown that only uPARAP/Endo180 and MR possess the ability to bind and internalize collagen (Jürgensen et al. 2014). Although PLA2R and DEC-205 share a similar domain composition, including the presence of an FN-II domain, these two receptors are completely unable to internalize collagen (Jürgensen et al. 2014). The ability to bind collagen is mediated by a protruding ten-residue collagen-binding loop of the FN-II domain as well as adjacent protein domains, which probably affect either the multimerization of the receptor or the formation of a binding-active conformation (Jürgensen et al. 2014).
Using single particle electron microscopy, the N-terminal part of MR has been demonstrated to adopt a bent three-dimensional structure (Boskovic et al. 2006). Overall, the structure appears very similar to the structure of uPARAP/Endo180 (Rivera-Calzada et al. 2003; Boskovic et al. 2006) although the globular N-terminal part of MR involves two more CTLDs than observed for uPARAP/Endo180. Similar to uPARAP/Endo180, MR also adopts a different conformation at a lower pH corresponding to the endosomal environment (Boskovic et al. 2006).
2.4 Intracellular Collagen Degradation In Vivo
Most mesenchymal cells express uPARAP/Endo180 in vitro, and in vivo the expression of uPARAP/Endo180 is also restricted to certain mesenchymal cells. By Northern blotting and Western blotting of various tissues from mice, it has been shown that most tissues express uPARAP/Endo180, with especially high expression levels observed in the heart, lung, uterus, and bones (Wu et al. 1996; Madsen et al. 2013a). Very low expression levels are detected in the liver and brain. Histological analyses have demonstrated that uPARAP/Endo180 is expressed by mesenchymal cells of the developing and adult murine lung (Smith et al. 2008; Bundesmann et al. 2012) and in osteoblasts and chondrocytes of developing and adult bone (Engelholm et al. 2001; Howard et al. 2004; Wagenaar-Miller et al. 2007; Madsen et al. 2013a; Abdelgawad et al. 2014). In the skin, macrophages as well as fibroblasts, pericytes, and endothelial cells have been reported to express uPARAP/Endo180 (Sheikh et al. 2000; Honardoust et al. 2006). In human liver fibrosis and in mouse models of lung and liver fibrosis, uPARAP/Endo180 is upregulated and expressed by myofibroblasts (Madsen et al. 2012; Bundesmann et al. 2012). In mouse models of kidney fibrosis, uPARAP/Endo180 is expressed by myofibroblasts and a subset of macrophages (López-Guisa et al. 2012). In general, uPARAP/Endo180 is upregulated in conditions known to involve increased tissue remodeling, including bone development (Engelholm et al. 2001; Howard et al. 2004; Wagenaar-Miller et al. 2007), skin wound healing (Rohani et al. 2014), tissue fibrosis (Madsen et al. 2012; Bundesmann et al. 2012; López-Guisa et al. 2012), and in connection to cancer as described in detail later in this book chapter. In bone development, the importance of uPARAP/Endo180 became particularly clear when inactivating mutations in the MRC2 gene coding for uPARAP/Endo180 were identified as the underlying cause of a severe hereditary skeletal disorder in cattle known as crooked tail syndrome (CTS) (Fasquelle et al. 2009; Sartelet et al. 2012). In mice, uPARAP/Endo180 deficiency only results in a relatively mild skeletal phenotype (Wagenaar-Miller et al. 2007; Madsen et al. 2013a), but when combined with deficiency of the important extracellular collagenase MT1-MMP, severely impaired bone development is observed, and the mice only have a life span of up to 3 weeks (Wagenaar-Miller et al. 2007). So far, no human inactivating mutations of uPARAP/Endo180 have been reported although a single nucleotide polymorphism (SNP) in a regulatory region of the MRC2 gene has been found to associate with degenerative bony changes of the temporomandibular joint (Yamaguchi et al. 2014), and a SNP in exon 30 of MRC2 associates with the risk of recurrent disease for head and neck squamous carcinoma patients (Wu et al. 2009).
MR was first identified on Kupffer cells (Schlesinger et al. 1978) and later was also found to be expressed by many other types of tissue macrophages (Takahashi et al. 1998) and by subsets of dendritic cells (Linehan 2005; Burgdorf et al. 2006). In addition to macrophages, MR is expressed at high levels by sinusoidal endothelial cells in the liver and in lymph nodes (Takahashi et al. 1998; Malovic et al. 2007). Early studies of the function of the MR primarily focused on its potential role in the innate immune system as a receptor for certain pathogens due to the carbohydrate-binding properties of the receptor. However, subsequent littermate-controlled studies of MR knockout mice have failed to clearly demonstrate any significant changes in susceptibility to these pathogens (Lee et al. 2003; Swain et al. 2003).
Instead, the first study reporting the generation of MR knockout mice revealed increased serum levels of several glycoproteins including seven lysosomal hydrolases and the carboxy-terminal propeptide domains of collagen types I and III in MR-deficient mice (Lee et al. 2002). MR-deficient mice also have a significantly reduced ability to clear denatured collagen from the circulation (Malovic et al. 2007). In subsets of dendritic cells, MR probably contributes to the cross presentation of certain glycosylated antigens (Burgdorf et al. 2006), and interestingly the MR-mediated uptake of these antigens can be inhibited by collagen fragments (Burgdorf et al. 2010).
Still, the study of MR as a collagen internalization receptor involved in ECM turnover is in its infancy, and future in vivo studies addressing the role of MR in tissue remodeling processes are therefore a high priority. However, as described in detail in the section below, a recent study strongly suggests that MR-mediated collagen internalization could be an important function of M2 macrophages in the dermis and in tumors of mice (Madsen and Bugge 2013; Madsen et al. 2013b).
2.4.1 Imaging Collagen Internalization In Vivo
As outlined earlier in this book chapter, in vitro studies have clearly shown that cells can internalize collagen for lysosomal degradation in a uPARAP/Endo180- or MR-dependent manner. Furthermore, in vivo studies have revealed phenotypes of uPARAP/Endo180-deficient animals consistent with a role of this receptor in collagen remodeling processes. However, many aspects related to the mechanism of collagen internalization in vivo are still uncovered, although some answers have been provided by a recent study utilizing a novel confocal microscopy assay to analyze the cellular uptake of collagen in the skin of mice (Madsen et al. 2013b). In this study fluorescent collagen was introduced into the connective tissue of the skin of mice where it immediately polymerized to form insoluble collagen fibers indistinguishable from endogenous collagen fibers. The turnover of these collagen fibers could be visualized using two-photon or confocal microscopy analysis of the intact tissue. The study revealed that fluorescent collagen or collagen degradation fragments are efficiently internalized by various cells in the dermis (Fig. 2.4a). By combining the assay with transgenic mice expressing cell lineage-specific fluorescent reporter proteins or with whole-mount immunostaining, it was demonstrated that several cell types are capable of internalizing collagen, including fibroblasts and Cx3Cr1-positive macrophages, but that M2-like macrophages are the dominant collagen-internalizing cell population (Fig. 2.4b). These cells are positive for the pan-macrophage marker F4/80 and for the M2-macrophage markers Fizz1 and MR. Collagen internalization by these M2-like macrophages is mediated by MR as demonstrated by the lack of collagen internalization in MR-deficient mice (Madsen et al. 2013b). M2-polarized macrophages are cells proposed to play an important role in tissue remodeling and repair processes, but this has mainly been ascribed to their ability to stimulate ECM synthesis (Ingman et al. 2006) and to dampen inflammatory reactions (Gordon and Martinez 2010; Vasievich and Huang 2011). Internalization of collagen, and potentially other ECM proteins, is likely to be another important way by which these cells promote tissue remodeling. Since tumor-associated macrophages (TAMs) often acquire an M2-polarized phenotype (Biswas et al. 2013), it has been suggested that TAMs play an important role for the collagen degradation that occurs in connection to solid tumor growth and invasion (Madsen and Bugge 2013). Recently we have indeed been able to demonstrate, using a similar confocal microscopy-based assay, that in solid tumors of mice, M2-polarized TAMs are the dominant collagen internalizing cells (Madsen et al. unpublished). These collagen-internalizing TAMs are very abundant in the tumors and internalize collagen in an MR-dependent manner (Madsen et al. unpublished).
M2 macrophages of the dermis internalize high levels of collagen. (a) Image of the dermis from collagen-injected Cx3cr1-GFP;Col1a1-GFP double transgenic mice. Fluorescent collagen (white) and dextran (red) were introduced into the dermis of transgenic reporter mice expressing GFP in Cx3cr1-positive monocytes and Col1a1-positive fibroblast (green). 24 h later the dermis was excised and the fresh tissue was imaged using confocal microscopy. Several cell population display intracellular collagen-containing vesicles, but certain cells that were not monocytes or fibroblasts internalized very high levels of collagen and dextran (white arrow). Scale bar, 20 μm. (b) High-level collagen-internalizing cells of the dermis express the M2-macrophage marker Fizz-1. Fluorescent collagen (white) and dextran (red) were introduced into the dermis of mice, and 20 h later the dermis was excised and whole mount stained for Fizz-1 (green). Adapted from Madsen et al. (2013b)
2.4.2 Intracellular Collagen Degradation in Cancer
In most tissues, resting or quiescent fibroblasts express no or very low levels of uPARAP/Endo180, whereas activated myofibroblasts in connection to cancer are uPARAP/Endo180 positive (Fig. 2.5a–b) (Schnack Nielsen et al. 2002; Curino et al. 2005; Sulek et al. 2007; Kogianni et al. 2009; Melander et al. 2015). Such uPARAP/Endo180-positive cancer-associated fibroblasts (CAFs) have been demonstrated in all studied carcinomas, including breast cancer, prostate cancer, and head and neck squamous cell carcinoma. In osteosarcomas and gliomas, the cancer cells themselves often express uPARAP/Endo180 (Huijbers et al. 2010; Takahashi et al. 2011; Engelholm et al. 2016), and in a small subset of breast tumors with a basal-like subtype, the cancer cells are also uPARAP/Endo180 positive (Wienke et al. 2007). In prostate cancer specimens, an upregulation of uPARAP/Endo180 has been demonstrated, with expression suggested to be both on cancer cells and stromal cells (Kogianni et al. 2009). In addition to these descriptive studies, a few studies have demonstrated the direct functional implications of uPARAP/Endo180 for tumor growth. First of all, a study by Curino et al. has investigated the effects of uPARAP/Endo180 deficiency in a genetic mouse model of breast cancer. In this model, the tumors of uPARAP/Endo180 knockout mice are smaller than the tumors of littermate uPARAP/Endo180-expressing mice, and strikingly the uPARAP/Endo180-deficient mice display highly increased levels of intratumoral collagen (Fig. 2.5c–g) (Curino et al. 2005). When collagen internalization by ex vivo explants from these tumors was assayed, it was observed that fibroblasts from uPARAP/Endo180-deficient tumors lack the ability to internalize collagen. In another study it has been demonstrated that MCF-7 breast cancer cells transfected with uPARAP/Endo180 have a growth advantage over cells transfected with an internalization-deficient mutant when inoculated into immunocompromised mice (Wienke et al. 2007). Using antibody-mediated neutralization of uPARAP/Endo180, it has recently been demonstrated that uPARAP/Endo180 expressed by sarcoma cells in mice contributes to the severe bone degradation that accompanies the tumor progression (Engelholm et al. 2016). Altogether these studies demonstrate that uPARAP/Endo180 affects ECM remodeling associated with tumor progression and influences tumor growth and associated skeletal morbidities.
uPARAP/Endo180-mediated collagen remodeling promotes tumor growth. uPARAP/Endo180 is upregulated in human breast cancer (a and b). (a) Immunohistochemical analysis of uPARAP/Endo180 in invasive ductal breast carcinoma specimens demonstrates upregulation of uPARAP/Endo180 (brown) with expression restricted to the stromal cells of the tumor (St). uPARAP/Endo180-positive fibroblast-like cells show a punctuated staining pattern (arrow) indicative of a localization in intracellular vesicles (b). Intratumoral collagen accumulates in uPARAP/Endo180-deficient mice in a genetic mouse model of breast cancer. Transgenic PymT mice that are predisposed to develop breast cancer were crossed with uPARAP/Endo180-deficient mice. (c and d) Immunohistochemical analysis of collagen type I reveals large accumulations of collagen type I (brown) in tumors of uPARAP/Endo180-deficient mice (d) compared to tumors of littermate uPARAP/Endo180-expressing mice (c). Scale bar, 500 μm. (e) Histomorphometric quantification of collagen type I in the tumors of uPARAP/Endo180-expressing mice (white bar) and littermate uPARAP/Endo180-deficient mice (black bar). (f and g) uPARAP/Endo180 promotes breast tumor growth. Scatter plots illustrate the cumulative tumor burden of uPARAP/Endo180-expressing mice (open circles) and uPARAP/Endo180-deficient mice (filled circles) at 95 (f) and 105 (g) days of age. (a) and (b) were adapted from Schnack Nielsen et al. (2002) with permission from John Wiley and Sons, and C-G were adapted from Curino et al. (2005) with permission from Rockefeller University Press
Historically, MR has been studied as a receptor involved in the innate immune response, and its importance in vivo as a collagen internalization receptor with a potential role in tumor growth and invasion still remains to be addressed. In recent years, MR has been given a lot of attention as a marker for M2-polarized macrophages (Gordon and Martinez 2010). M1 macrophages, also known as classically activated macrophages, develop when exposed to the pro-inflammatory cytokine interferon-gamma (IFN-γ) and tumor necrosis factor alpha (TNFα), whereas M2 macrophages, also known as alternatively activated macrophages, develop in response to interleukin-4 (IL-4) and IL-13 (Gordon and Martinez 2010; Wang and Joyce 2010). M2 macrophages are anti-inflammatory macrophages that are often engaged in tissue remodeling processes such as wound healing (Martinez et al. 2009). In connection to cancer, it has been proposed that M2 macrophages have pro-tumorigenic functions through their ability to promote tumor-associated angiogenesis and their ability to stimulate cancer cell migration and invasion (Noy and Pollard 2014). M2 macrophages also have immunosuppressive functions and can contribute to a tumor microenvironment, which helps the tumor cells evade a T-cell response directed against them (Vasievich and Huang 2011; Noy and Pollard 2014). At this point, the role of MR expressed by M2 macrophages for tumor growth and invasion still remains to be directly investigated. However, the recent demonstration of MR as a critical receptor for macrophage-mediated collagen uptake in the skin and in tumors of mice (Madsen et al. 2013b; Madsen et al. unpublished) renders it highly probable that MR could play an important role for tumor-associated collagen remodeling and thereby critically affect tumor growth (Fig. 2.6). Future studies will reveal the importance of MR-mediated collagen degradation in cancer and in connection to other pathological conditions and indicate whether therapeutic targeting of MR could form the basis of novel cancer treatments.
Tumor-infiltrating fibroblasts and M2 macrophages promote collagen degradation. Simplified schematic representation of a tumor consisting of cancer cells, collagen, fibroblasts, and M2 macrophages. In connection to invasive tumor growth, fibroblasts and M2 macrophage contribute to the tumor-associated ECM remodeling. Fibroblasts and M2 macrophages can internalize collagen fragments for lysosomal degradation through the action of uPARAP/Endo180 and MR, respectively
References
Abdelgawad ME, Søe K, Andersen TL, Merrild DMH, Christiansen P, Kjærsgaard-Andersen P, Delaisse J-M (2014) Does collagen trigger the recruitment of osteoblasts into vacated bone resorption lacunae during bone remodeling? Bone 67:181–188. doi:10.1016/j.bone.2014.07.012
Acerbi I, Cassereau L, Dean I, Shi Q, Au A, Park C, Chen YY, Liphardt J, Hwang ES, Weaver VM (2015) Human breast cancer invasion and aggression correlates with ECM stiffening and immune cell infiltration. Integr Biol 7:1120–1134. doi:10.1039/C5IB00040H
Atapattu L, Lackmann M, Janes PW (2014) The role of proteases in regulating Eph/ephrin signaling. Cell Adh Migr 8:294–307. doi:10.4161/19336918.2014.970026
Bányai L, Patthy L (1991) Evidence for the involvement of type II domains in collagen binding by 72 kDa type IV procollagenase. FEBS Lett 282:23–25
Bányai L, Tordai H, Patthy L (1994) The gelatin-binding site of human 72 kDa type IV collagenase (gelatinase A). Biochem J 298(Pt 2):403–407
Beertsen W, Everts V (1977) The site of remodeling of collagen in the periodontal ligament of the mouse incisor. Anat Rec 189:479–497. doi:10.1002/ar.1091890308
Behrendt N, Rønne E, Danø K (1993) A novel, specific pro-urokinase complex on monocyte-like cells, detected by transglutaminase-catalyzed cross-linking. FEBS Lett 336:394–396
Behrendt N, Jensen ON, Engelholm LH, Mørtz E, Mann M, Danø K (2000) A urokinase receptor-associated protein with specific collagen binding properties. J Biol Chem 275:1993–2002
Biswas SK, Allavena P, Mantovani A (2013) Tumor-associated macrophages: functional diversity, clinical significance, and open questions. Semin Immunopathol 35:585–600
Bonnans C, Chou J, Werb Z (2014) Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol 15:786–801. doi:10.1038/nrm3904
Boskovic J, Arnold JN, Stilion R, Gordon S, Sim RB, Rivera-Calzada A, Wienke D, Isacke CM, Martinez-Pomares L, Llorca O (2006) Structural model for the mannose receptor family uncovered by electron microscopy of Endo180 and the mannose receptor. J Biol Chem 281:8780–8787. doi:10.1074/jbc.M513277200
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S, Yaffe MJ (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356:227–236. doi:10.1056/NEJMoa062790
Bredfeldt JS, Liu Y, Conklin MW, Keely PJ, Mackie TR, Eliceiri KW (2014) Automated quantification of aligned collagen for human breast carcinoma prognosis. J Pathol Inform 5:28. doi:10.4103/2153-3539.139707
Bundesmann MM, Wagner TE, Chow Y-H, Altemeier WA, Steinbach T, Schnapp LM (2012) Role of urokinase plasminogen activator receptor-associated protein in mouse lung. Am J Respir Cell Mol Biol 46:233–239. doi:10.1165/rcmb.2010-0485OC
Burgdorf S, Lukacs-Kornek V, Kurts C (2006) The mannose receptor mediates uptake of soluble but not of cell-associated antigen for cross-presentation. J Immunol 176:6770–6776. doi:10.4049/jimmunol.176.11.6770
Burgdorf S, Schuette V, Semmling V, Hochheiser K, Lukacs-Kornek V, Knolle PA, Kurts C (2010) Steady-state cross-presentation of OVA is mannose receptor-dependent but inhibitable by collagen fragments. Proc Natl Acad Sci USA 107:E48–E49.; author reply E50–1. doi:10.1073/pnas.1000598107
Conklin MW, Eickhoff JC, Riching KM, Pehlke CA, Eliceiri KW, Provenzano PP, Friedl A, Keely PJ (2011) Aligned collagen is a prognostic signature for survival in human breast carcinoma. Am J Pathol 178:1221–1232. doi:10.1016/j.ajpath.2010.11.076
Coussens LM, Fingleton B, Matrisian LM (2002) Matrix metalloproteinase inhibitors and cancer: trials and tribulations. Science 295:2387–2392. doi:10.1126/science.1067100
Cox TR, Erler JT (2011) Remodeling and homeostasis of the extracellular matrix: implications for fibrotic diseases and cancer. Dis Model Mech 4:165–178. doi:10.1242/dmm.004077
Cox TR, Erler JT (2014) Molecular pathways: connecting fibrosis and solid tumor metastasis. Clin Cancer Res 20:3637–3643. doi:10.1158/1078-0432.CCR-13-1059
Creemers LB, Hoeben KA, Jansen DC, Buttle DJ, Beertsen W, Everts V (1998) Participation of intracellular cysteine proteinases, in particular cathepsin B, in degradation of collagen in periosteal tissue explants. Matrix Biol 16:575–584
Cullen JC (1972) Intracellular collagen in experimental arthritis in rats. J Bone Joint Surg Br 54:351–359
Curino AC, Engelholm LH, Yamada SS, Holmbeck K, Lund LR, Molinolo AA, Behrendt N, Nielsen BS, Bugge TH (2005) Intracellular collagen degradation mediated by uPARAP/Endo180 is a major pathway of extracellular matrix turnover during malignancy. J Cell Biol 169:977–985. doi:10.1083/jcb.200411153
Danielsen CC (1987) Thermal stability of human-fibroblast-collagenase-cleavage products of type-I and type-III collagens. Biochem J 247:725–729
Decock J, Thirkettle S, Wagstaff L, Edwards DR (2011) Matrix metalloproteinases: protective roles in cancer. J Cell Mol Med 15:1254–1265. doi:10.1111/j.1582-4934.2011.01302.x
East L, Isacke CM (2002) The mannose receptor family. Biochim Biophys Acta 1572:364–386
East L, McCarthy A, Wienke D, Sturge J, Ashworth A, Isacke CM (2003) A targeted deletion in the endocytic receptor gene Endo180 results in a defect in collagen uptake. EMBO Rep 4:710–716. doi:10.1038/sj.embor.embor882
Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2:161–174. doi:10.1038/nrc745
Engelholm LH, Nielsen BS, Netzel-Arnett S, Solberg H, Chen XD, Lopez Garcia JM, Lopez-Otin C, Young MF, Birkedal-Hansen H, Danø K, Lund LR, Behrendt N, Bugge TH (2001) The urokinase plasminogen activator receptor-associated protein/endo180 is coexpressed with its interaction partners urokinase plasminogen activator receptor and matrix metalloprotease-13 during osteogenesis. Lab Invest 81:1403–1414
Engelholm LH, List K, Netzel-Arnett S, Cukierman E, Mitola DJ, Aaronson H, Kjøller L, Larsen JK, Yamada KM, Strickland DK, Holmbeck K, Danø K, Birkedal-Hansen H, Behrendt N, Bugge TH (2003) uPARAP/Endo180 is essential for cellular uptake of collagen and promotes fibroblast collagen adhesion. J Cell Biol 160:1009–1015. doi:10.1083/jcb.200211091
Engelholm LH, Melander MC, Hald A, Persson M, Madsen DH, Jürgensen HJ, Johansson K, Nielsen C, Nørregaard KS, Ingvarsen SZ, Kjaer A, Trovik CS, Laerum OD, Bugge TH, Eide J, Behrendt N (2016) Targeting a novel bone degradation pathway in primary bone cancer by inactivation of the collagen receptor uPARAP/Endo180. J Pathol 238:120–133. doi:10.1002/path.4661
Everts V, Beertsen W, Tigchelaar-Gutter W (1985) The digestion of phagocytosed collagen is inhibited by the proteinase inhibitors leupeptin and E-64. Coll Relat Res 5:315–336
Everts V, van der Zee E, Creemers L, Beertsen W (1996) Phagocytosis and intracellular digestion of collagen, its role in turnover and remodelling. Histochem J 28:229–245
Fan M-H, Zhu Q, Li H-H, Ra H-J, Majumdar S, Gulick DL, Jerome JA, Madsen DH, Christofidou-Solomidou M, Speicher DW, Bachovchin WW, Feghali-Bostwick C, Puré E (2015) Fibroblast activation protein (FAP) accelerates collagen degradation and clearance from lung in mice. J Biol Chem 291:8070–8089. doi:10.1074/jbc.M115.701433
Fasquelle C, Sartelet A, Li W, Dive M, Tamma N, Michaux C, Druet T, Huijbers IJ, Isacke CM, Coppieters W, Georges M, Charlier C (2009) Balancing selection of a frame-shift mutation in the MRC2 gene accounts for the outbreak of the Crooked Tail Syndrome in Belgian Blue Cattle. PLoS Genet 5:e1000666. doi:10.1371/journal.pgen.1000666
Fields GB (2013) Interstitial collagen catabolism. J Biol Chem 288:8785–8793. doi:10.1074/jbc.R113.451211
Garant PR (1976) Collagen resorption by fibroblasts. A theory of fibroblastic maintenance of the periodontal ligament. J Periodontol 47:380–390. doi:10.1902/jop.1976.47.7.380
Giblin SP, Midwood KS (2015) Tenascin-C: Form versus function. Cell Adh Migr 9:48–82. doi:10.4161/19336918.2014.987587
Gordon S, Martinez FO (2010) Alternative activation of macrophages: mechanism and functions. Immunity 32:593–604. doi:10.1016/j.immuni.2010.05.007
Guo YP, Martin LJ, Hanna W, Banerjee D, Miller N, Fishell E, Khokha R, Boyd NF (2001) Growth factors and stromal matrix proteins associated with mammographic densities. Cancer Epidemiol Biomarkers Prev 10:243–248
Highberger JH, Corbett C, Gross J (1979) Isolation and characterization of a peptide containing the site of cleavage of the chick skin collagen alpha 1[I] chain by animal collagenases. Biochem Biophys Res Commun 89:202–208
Hipps DS, Hembry RM, Docherty AJ, Reynolds JJ, Murphy G (1991) Purification and characterization of human 72-kDa gelatinase (type IV collagenase). Use of immunolocalisation to demonstrate the non-coordinate regulation of the 72-kDa and 95-kDa gelatinases by human fibroblasts. Biol Chem Hoppe Seyler 372:287–296
Holmbeck K, Bianco P, Caterina J, Yamada S, Kromer M, Kuznetsov SA, Mankani M, Gehron Robey P, Poole AR, Pidoux I, Ward JM, Birkedal-Hansen H (1999) MT1-MMP-deficient mice develop dwarfism, osteopenia, arthritis, and connective tissue disease due to inadequate collagen turnover. Cell 99:81–92. doi:10.1016/S0092-8674(00)80064-1
Honardoust HA, Jiang G, Koivisti L, Wienke D, Isacke CM, Larjava H, Häkkinen L (2006) Expression of Endo180 is spatially and temporally regulated during wound healing. Histopathology 49:634–648. doi:10.1111/j.1365-2559.2006.02559.x
Howard MJ, Chambers MG, Mason RM, Isacke CM (2004) Distribution of Endo180 receptor and ligand in developing articular cartilage. Osteoarthritis Cartilage 12:74–82
Huijbers IJ, Iravani M, Popov S, Robertson D, Al-Sarraj S, Jones C, Isacke CM (2010) A role for fibrillar collagen deposition and the collagen internalization receptor endo180 in glioma invasion. PLoS One 5:e9808. doi:10.1371/journal.pone.0009808
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110:673–687
Ikenaga N, Ohuchida K, Mizumoto K, Akagawa S, Fujiwara K, Eguchi D, Kozono S, Ohtsuka T, Takahata S, Tanaka M (2012) Pancreatic cancer cells enhance the ability of collagen internalization during epithelial-mesenchymal transition. PLoS One 7:e40434. doi:10.1371/journal.pone.0040434
Ingman WV, Wyckoff J, Gouon-Evans V, Condeelis J, Pollard JW (2006) Macrophages promote collagen fibrillogenesis around terminal end buds of the developing mammary gland. Dev Dyn 235:3222–3229. doi:10.1002/dvdy.20972
Ingvarsen S, Porse A, Erpicum C, Maertens L, Jürgensen HJ, Madsen DH, Melander MC, Gardsvoll H, Hoyer-Hansen G, Noel A, Holmbeck K, Engelholm LH, Behrendt N (2013) Targeting a single function of the multifunctional matrix metalloprotease MT1-MMP Impact on Lymphangiogenesis. J Biol Chem 288:10195–10204
Isacke CM, van der Geer P, Hunter T, Trowbridge IS (1990) p180, a novel recycling transmembrane glycoprotein with restricted cell type expression. Mol Cell Biol 10:2606–2618
Joyce JA, Pollard JW (2009) Microenvironmental regulation of metastasis. Nat Rev Cancer 9:239–252. doi:10.1038/nrc2618
Jürgensen HJ, Madsen DH, Ingvarsen S, Melander MC, Gårdsvoll H, Patthy L, Engelholm LH, Behrendt N (2011) A novel functional role of collagen glycosylation: interaction with the endocytic collagen receptor uPARAP/ENDO180. J Biol Chem 286:32736–32748
Jürgensen HJ, Johansson K, Madsen DH, Porse A, Melander MC, Sørensen KR, Nielsen C, Bugge TH, Behrendt N, Engelholm LH (2014) Complex determinants in specific members of the mannose receptor family govern collagen endocytosis. J Biol Chem 289:7935–7947
Kessenbrock K, Plaks V, Werb Z (2010) Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141:52–67. doi:10.1016/j.cell.2010.03.015
Kjøller L, Engelholm LH, Høyer-Hansen M, Danø K, Bugge TH, Behrendt N (2004) uPARAP/endo180 directs lysosomal delivery and degradation of collagen IV. Exp Cell Res 293:106–116
Kogianni G, Walker MM, Waxman J, Sturge J (2009) Endo180 expression with cofunctional partners MT1-MMP and uPAR-uPA is correlated with prostate cancer progression. Eur J Cancer 45:685–693. doi:10.1016/j.ejca.2008.11.023
Krane SM, Inada M (2008) Matrix metalloproteinases and bone. Bone 43:7–18. doi:10.1016/j.bone.2008.03.020
Lee W, Sodek J, McCulloch CA (1996) Role of integrins in regulation of collagen phagocytosis by human fibroblasts. J Cell Physiol 168:695–704. doi:10.1002/(SICI)1097-4652(199609)168:3<695::AID-JCP22>3.0.CO;2-X
Lee SJ, Evers S, Roeder D, Parlow AF, Risteli J, Risteli L, Lee YC, Feizi T, Langen H, Nussenzweig MC (2002) Mannose receptor-mediated regulation of serum glycoprotein homeostasis. Science 295:1898–1901. doi:10.1126/science.1069540
Lee SJ, Zheng N-Y, Clavijo M, Nussenzweig MC (2003) Normal host defense during systemic candidiasis in mannose receptor-deficient mice. Infect Immun 71:437–445
Leitinger B, Hohenester E (2007) Mammalian collagen receptors. Matrix Biol 26:146–155. doi:10.1016/j.matbio.2006.10.007
Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, Fong SFT, Csiszar K, Giaccia A, Weninger W, Yamauchi M, Gasser DL, Weaver VM (2009) Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell 139:891–906. doi:10.1016/j.cell.2009.10.027
Linehan SA (2005) The mannose receptor is expressed by subsets of APC in non-lymphoid organs. BMC Immunol 6:4. doi:10.1186/1471-2172-6-4
López-Guisa JM, Cai X, Collins SJ, Yamaguchi I, Okamura DM, Bugge TH, Isacke CM, Emson CL, Turner SM, Shankland SJ, Eddy AA (2012) Mannose receptor 2 attenuates renal fibrosis. J Am Soc Nephrol 23:236–251. doi:10.1681/ASN.2011030310
López-Otín C, Palavalli LH, Samuels Y (2009) Protective roles of matrix metalloproteinases: from mouse models to human cancer. Cell Cycle 8:3657–3662
Lu P, Takai K, Weaver VM, Werb Z (2011) Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb Perspect Biol 3:a005058. doi:10.1101/cshperspect.a005058
Lu P, Weaver VM, Werb Z (2012) The extracellular matrix: a dynamic niche in cancer progression. J Cell Biol 196:395–406. doi:10.1083/jcb.201102147
Madsen DH, Bugge TH (2013) Imaging collagen degradation in vivo highlights a key role for M2-polarized macrophages in extracellular matrix degradation. Oncoimmunology 2:e27127
Madsen DH, Bugge TH (2015) The source of matrix-degrading enzymes in human cancer: problems of research reproducibility and possible solutions. J Cell Biol 209:195–198. doi:10.1083/jcb.201501034
Madsen DH, Engelholm LH, Ingvarsen S, Hillig T, Wagenaar-Miller RA, Kjøller L, Gårdsvoll H, Høyer-Hansen G, Holmbeck K, Bugge TH, Behrendt N (2007) Extracellular collagenases and the endocytic receptor, urokinase plasminogen activator receptor-associated protein/endo180, cooperate in fibroblast-mediated collagen degradation. J Biol Chem 282:27037–27045. doi:10.1074/jbc.M701088200
Madsen DH, Ingvarsen S, Jürgensen HJ, Melander MC, Kjøller L, Moyer A, Honoré C, Madsen CA, Garred P, Burgdorf S, Bugge TH, Behrendt N, Engelholm LH (2011) The non-phagocytic route of collagen uptake: a distinct degradation pathway. J Biol Chem 286:26996–27010
Madsen DH, Jürgensen HJ, Ingvarsen S, Melander MC, Vainer B, Egerod KL, Hald A, Rønø B, Madsen CA, Bugge TH, Engelholm LH, Behrendt N (2012) Endocytic collagen degradation: a novel mechanism involved in protection against liver fibrosis. J Pathol 227:94–105
Madsen DH, Jürgensen HJ, Ingvarsen S, Melander MC, Albrechtsen R, Hald A, Holmbeck K, Bugge TH, Behrendt N, Engelholm LH (2013a) Differential actions of the endocytic collagen receptor uPARAP/Endo180 and the collagenase MMP-2 in bone homeostasis. PLoS One 8:e71261. doi:10.1371/journal.pone.0071261
Madsen DH, Leonard D, Masedunskas A, Moyer A, Jürgensen HJ, Peters DE, Amornphimoltham P, Selvaraj A, Yamada SS, Brenner DA, Burgdorf S, Engelholm LH, Behrendt N, Holmbeck K, Weigert R, Bugge TH (2013b) M2-like macrophages are responsible for collagen degradation through a mannose receptor-mediated pathway. J Cell Biol 202:951–966
Malovic I, Sørensen KK, Elvevold KH, Nedredal GI, Paulsen S, Erofeev A V, Smedsrød BH, McCourt PAG (2007) The mannose receptor on murine liver sinusoidal endothelial cells is the main denatured collagen clearance receptor. Hepatology 45:1454–1461. doi:10.1002/hep.21639
Martin MD, Matrisian LM (2007) The other side of MMPs: protective roles in tumor progression. Cancer Metastasis Rev 26:717–724. doi:10.1007/s10555-007-9089-4
Martinez FO, Helming L, Gordon S (2009) Alternative activation of macrophages: an immunologic functional perspective. Annu Rev Immunol 27:451–483. doi:10.1146/annurev.immunol.021908.132532
Martinez-Pomares L, Wienke D, Stillion R, McKenzie EJ, Arnold JN, Harris J, McGreal E, Sim RB, Isacke CM, Gordon S (2006) Carbohydrate-independent recognition of collagens by the macrophage mannose receptor. Eur J Immunol 36:1074–1082. doi:10.1002/eji.200535685
Melander MC, Jürgensen HJ, Madsen DH, Engelholm LH, Behrendt N (2015) The collagen receptor uPARAP/Endo180 in tissue degradation and cancer (Review). Int J Oncol 47:1177–1188. doi:10.3892/ijo.2015.3120
Mettouchi A, Meneguzzi G (2006) Distinct roles of beta1 integrins during angiogenesis. Eur J Cell Biol 85:243–247. doi:10.1016/j.ejcb.2005.09.010
Mohamed MM, Sloane BF (2006) Cysteine cathepsins: multifunctional enzymes in cancer. Nat Rev Cancer 6:764–775. doi:10.1038/nrc1949
Mousavi SA, Sato M, Sporstøl M, Smedsrød B, Berg T, Kojima N, Senoo H (2005) Uptake of denatured collagen into hepatic stellate cells: evidence for the involvement of urokinase plasminogen activator receptor-associated protein/Endo180. Biochem J 387:39–46. doi:10.1042/BJ20040966
Mousavi SA, Fønhus MS, Berg T (2009) Up-regulation of uPARAP/Endo180 during culture activation of rat hepatic stellate cells and its presence in hepatic stellate cell lines from different species. BMC Cell Biol 10:39. doi:10.1186/1471-2121-10-39
Nagelkerke A, Bussink J, Rowan AE, Span PN (2015) The mechanical microenvironment in cancer: how physics affects tumours. Semin Cancer Biol 35:62–70. doi:10.1016/j.semcancer.2015.09.001
Napper CE, Drickamer K, Taylor ME (2006) Collagen binding by the mannose receptor mediated through the fibronectin type II domain. Biochem J 395:579–586. doi:10.1042/BJ20052027
Noy R, Pollard JW (2014) Tumor-associated macrophages: from mechanisms to therapy. Immunity 41:49–61. doi:10.1016/j.immuni.2014.06.010
Paracuellos P, Briggs DC, Carafoli F, Lončar T, Hohenester E (2015) Insights into collagen uptake by C-type mannose receptors from the crystal structure of Endo180 domains 1–4. Structure 23:2133–2142. doi:10.1016/j.str.2015.09.004
Park JE, Lenter MC, Zimmermann RN, Garin-Chesa P, Old LJ, Rettig WJ (1999) Fibroblast activation protein, a dual specificity serine protease expressed in reactive human tumor stromal fibroblasts. J Biol Chem 274:36505–36512
Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, Gefen A, Reinhart-King CA, Margulies SS, Dembo M, Boettiger D, Hammer DA, Weaver VM (2005) Tensional homeostasis and the malignant phenotype. Cancer Cell 8:241–254. doi:10.1016/j.ccr.2005.08.010
Pickup MW, Mouw JK, Weaver VM (2014) The extracellular matrix modulates the hallmarks of cancer. EMBO Rep 15:1243–1253. doi:10.15252/embr.201439246
Provenzano PP, Inman DR, Eliceiri KW, Knittel JG, Yan L, Rueden CT, White JG, Keely PJ (2008) Collagen density promotes mammary tumor initiation and progression. BMC Med 6:11. doi:10.1186/1741-7015-6-11
Pyonteck SM, Akkari L, Schuhmacher AJ, Bowman RL, Sevenich L, Quail DF, Olson OC, Quick ML, Huse JT, Teijeiro V, Setty M, Leslie CS, Oei Y, Pedraza A, Zhang J, Brennan CW, Sutton JC, Holland EC, Daniel D, Joyce JA (2013) CSF-1R inhibition alters macrophage polarization and blocks glioma progression. Nat Med 19:1264–1272. doi:10.1038/nm.3337
Rivera-Calzada A, Robertson D, MacFadyen JR, Boskovic J, Isacke CM, Llorca O (2003) Three-dimensional interplay among the ligand-binding domains of the urokinase-plasminogen-activator-receptor-associated protein, Endo180. EMBO Rep 4:807–812. doi:10.1038/sj.embor.embor898
Rohani MG, Chow Y-H, Razumova M V, Ash S, Hung CF, Schnapp LM (2014) uPARAP function in cutaneous wound repair. PLoS One 9:e92660. doi:10.1371/journal.pone.0092660
Rowe RG, Weiss SJ (2008) Breaching the basement membrane: who, when and how? Trends Cell Biol 18:560–574
Saftig P, Hunziker E, Wehmeyer O, Jones S, Boyde A, Rommerskirch W, Moritz JD, Schu P, von Figura K (1998) Impaired osteoclastic bone resorption leads to osteopetrosis in cathepsin-K-deficient mice. Proc Natl Acad Sci USA 95:13453–13458
Salmon H, Franciszkiewicz K, Damotte D, Dieu-Nosjean M-C, Validire P, Trautmann A, Mami-Chouaib F, Donnadieu E (2012) Matrix architecture defines the preferential localization and migration of T cells into the stroma of human lung tumors. J Clin Invest 122:899–910. doi:10.1172/JCI45817
Sanderson MP, Dempsey PJ, Dunbar AJ (2006) Control of ErbB signaling through metalloprotease mediated ectodomain shedding of EGF-like factors. Growth Factors 24:121–136. doi:10.1080/08977190600634373
Sartelet A, Klingbeil P, Franklin CK, Fasquelle C, Géron S, Isacke CM, Georges M, Charlier C (2012) Allelic heterogeneity of crooked tail syndrome: result of balancing selection? Anim Genet 43:604–607. doi:10.1111/j.1365-2052.2011.02311.x
Schedin P, Keely PJ (2011) Mammary gland ECM remodeling, stiffness, and mechanosignaling in normal development and tumor progression. Cold Spring Harb Perspect Biol 3:a003228. doi:10.1101/cshperspect.a003228
Scherft JP, Heersche JN (1975) Accumulation of collagen-containing vacuoles in osteoblasts after administration of colchicine. Cell Tissue Res 157:353–365
Schlesinger PH, Doebber TW, Mandell BF, White R, DeSchryver C, Rodman JS, Miller MJ, Stahl P (1978) Plasma clearance of glycoproteins with terminal mannose and N-acetylglucosamine by liver non-parenchymal cells. Studies with beta-glucuronidase, N-acetyl-beta-D-glucosaminidase, ribonuclease B and agalacto-orosomucoid. Biochem J 176:103–109
Schnack Nielsen B, Rank F, Engelholm LH, Holm A, Danø K, Behrendt N (2002) Urokinase receptor-associated protein (uPARAP) is expressed in connection with malignant as well as benign lesions of the human breast and occurs in specific populations of stromal cells. Int J Cancer 98:656–664
Segal G, Lee W, Arora P, McKee M, Downey G, McCulloch C (2001) Involvement of actin filaments and integrins in the binding step in collagen phagocytosis by human fibroblasts. J Cell Sci 114:119–129
Sheikh H, Yarwood H, Ashworth A, Isacke CM (2000) Endo180, an endocytic recycling glycoprotein related to the macrophage mannose receptor is expressed on fibroblasts, endothelial cells and macrophages and functions as a lectin receptor. J Cell Sci 113(Pt 6):1021–1032
Shi F, Harman J, Fujiwara K, Sottile J (2010) Collagen I matrix turnover is regulated by fibronectin polymerization. Am J Physiol Cell Physiol 298:C1265–C1275. doi:10.1152/ajpcell.00341.2009
Smith L, Wagner TE, Huizar I, Schnapp LM (2008) uPARAP expression during murine lung development. Gene Expr Patterns 8:486–493. doi:10.1016/j.gep.2008.06.006
Stark M, Kühn K (1968) The properties of molecular fragments obtained on treating calfskin collagen with collagenase from clostridium histolyticum. Eur J Biochem 6:534–541
Sulek J, Wagenaar-Miller RA, Shireman J, Molinolo A, Madsen DH, Engelholm LH, Behrendt N, Bugge TH (2007) Increased expression of the collagen internalization receptor uPARAP/Endo180 in the stroma of head and neck cancer. J Histochem Cytochem 55:347–353
Swain SD, Lee SJ, Nussenzweig MC, Harmsen AG (2003) Absence of the macrophage mannose receptor in mice does not increase susceptibility to Pneumocystis carinii infection in vivo. Infect Immun 71:6213–6221
Takahashi K, Donovan MJ, Rogers RA, Ezekowitz RA (1998) Distribution of murine mannose receptor expression from early embryogenesis through to adulthood. Cell Tissue Res 292:311–323
Takahashi S, Yamada-Okabe H, Hamada K, Ohta S, Kawase T, Yoshida K, Toda M (2011) Downregulation of uPARAP mediates cytoskeletal rearrangements and decreases invasion and migration properties in glioma cells. J Neurooncol 103:267–276. doi:10.1007/s11060-010-0398-z
Tryggvason K, Höyhtyä M, Salo T (1987) Proteolytic degradation of extracellular matrix in tumor invasion. Biochim Biophys Acta 907:191–217. doi:10.1016/0304-419X(87)90006-0
van Noorden CJ, Everts V (1991) Selective inhibition of cysteine proteinases by Z-Phe-AlaCH2F suppresses digestion of collagen by fibroblasts and osteoclasts. Biochem Biophys Res Commun 178:178–184
Vasievich EA, Huang L (2011) The suppressive tumor microenvironment: a challenge in cancer immunotherapy. Mol Pharm 8:635–641
Wagenaar-Miller RA, Engelholm LH, Gavard J, Yamada SS, Gutkind JS, Behrendt N, Bugge TH, Holmbeck K (2007) Complementary roles of intracellular and pericellular collagen degradation pathways in vivo. Mol Cell Biol 27:6309–6322. doi:10.1128/MCB.00291-07
Wang H-W, Joyce JA (2010) Alternative activation of tumor-associated macrophages by IL-4: priming for protumoral functions. Cell Cycle 9:4824–4835
Wienke D, MacFadyen JR, Isacke CM (2003) Identification and characterization of the endocytic transmembrane glycoprotein Endo180 as a novel collagen receptor. Mol Biol Cell 14:3592–3604. doi:10.1091/mbc.E02-12-0814
Wienke D, Davies GC, Johnson DA, Sturge J, Lambros MBK, Savage K, Elsheikh SE, Green AR, Ellis IO, Robertson D, Reis-Filho JS, Isacke CM (2007) The collagen receptor Endo180 (CD280) Is expressed on basal-like breast tumor cells and promotes tumor growth in vivo. Cancer Res 67:10230–10240. doi:10.1158/0008-5472.CAN-06-3496
Wu K, Yuan J, Lasky LA (1996) Characterization of a novel member of the macrophage mannose receptor type C lectin family. J Biol Chem 271:21323–21330
Wu X, Spitz MR, Lee JJ, Lippman SM, Ye Y, Yang H, Khuri FR, Kim E, Gu J, Lotan R, Hong WK (2009) Novel susceptibility loci for second primary tumors/recurrence in head and neck cancer patients: large-scale evaluation of genetic variants. Cancer Prev Res (Phila) 2:617–624. doi:10.1158/1940-6207.CAPR-09-0025
Yamaguchi T, Nakaoka H, Yamamoto K, Fujikawa T, Kim Y-I, Yano K, Haga S, Katayama K, Shibusawa T, Park SB, Maki K, Kimura R, Inoue I (2014) Genome-wide association study of degenerative bony changes of the temporomandibular joint. Oral Dis 20:409–415. doi:10.1111/odi.12141
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Kuczek, D.E., Hübbe, M.L., Madsen, D.H. (2017). Internalization of Collagen: An Important Matrix Turnover Pathway in Cancer. In: Brekken, R., Stupack, D. (eds) Extracellular Matrix in Tumor Biology. Biology of Extracellular Matrix. Springer, Cham. https://doi.org/10.1007/978-3-319-60907-2_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-60907-2_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-60906-5
Online ISBN: 978-3-319-60907-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)