Abstract
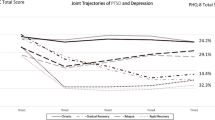
This chapter explores the prevalence, correlates, and consequences of posttraumatic stress disorder (PTSD) in World Trade Center (WTC) responders. Rates of WTC-related PTSD varied depending on when and how the assessments were conducted. In the Stony Brook cohort, 17% developed PTSD during the first 13 years after the accident; half had active illness 11–13 years later. Consistent with clinical and epidemiologic research, several studies found that PTSD was associated with medical conditions and impaired functioning. PTSD was also highly comorbid with depression, and comorbidity was associated with very poor outcomes. In the Stony Brook cohort, the majority of responders with comorbid PTSD and depression were out of the workforce (65.2%), diagnosed with a WTC medical condition (81.9%), and had impairments in life satisfaction (83.2%), relationships with friend (52.4%), and social support (63.1%). The data support the need for continued monitoring and treatment of both conditions.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Responders to the World Trade Center (WTC) disaster were exposed to emotional horrors and complex environmental toxins from gases and fine airborne particulate matter. The ~90,000 responders included trained first responders (e.g., police and firefighters) and inexperienced nontraditional responders, such as construction workers, electricians, and transportation and utility workers [1]. In the aftermath of the tower collapse, three large-scale health monitoring programs were funded by the National Institute of Occupational Safety and Health (NIOSH) : the Fire Department of the City of New York Medical Monitoring Program (FDNY-WTC-MMP) ; and the WTC Health Program (WTC-HP) established for police, other non-FDNY professionals, and nontraditional rescue/cleanup/recovery workers at five coordinated centers of excellence (Mount Sinai School of Medicine, Stony Brook University, Bellevue/New York University, Queens College, and Rutgers Robert Wood Johnson Medical School); and the WTC Health Registry (WTC-HR) which conducts longitudinal surveys of exposed civilians and responders.
The FDNY-WTC-MMP and WTC-HP provide ongoing assessments of both physical and mental health from direct physical examinations and self-report questionnaires and also treat WTC-related conditions. The WTC-HR collects survey data on physical and mental health. It is important to note that these programs are the first known health surveillance programs established after a toxic disaster that evaluate both physical and mental health, rather than solely focusing on physical outcomes.
This chapter focuses on posttraumatic stress disorder (PTSD) among responders. PTSD is a condition that can arise soon after a traumatic event (although symptoms may appear or become impairing after months or years have passed). The Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV) organized PTSD symptoms into three clusters: reexperiencing symptoms (e.g., intrusive recollections, nightmares, flashbacks), avoidance and numbing symptoms (e.g., avoiding reminders of the event, feeling detached, sense of foreshortened future), and hyperarousal symptoms (e.g., difficulty falling or staying asleep, irritability, difficulty concentrating, hypervigilance, exaggerated startle response). The diagnosis is made only when a sufficient number of symptoms in each category co-occur, last longer than a month, and interfere with a person’s functioning.
Because PTSD was the most common mental health condition being studied in disaster research, each of the three large-scale monitoring programs has assessed PTSD since 2002, when they were established. The assessment instrument used by all three programs is the Posttraumatic Symptom Checklist (PCL ), a 17-item self-report measure designed to assess the severity of the PTSD symptoms listed in DSM-IV [2] over the past month on a scale from 1 (not at all) to 5 (extremely). Scores can range from very low (17) to very high (85). Numerous WTC publications have described the prevalence of probable PTSD based on PCL cut points of either 44 or 50 or a proxy DSM-based PTSD measure created from the requisite number of moderate to severe symptoms in each of the three clusters (reexperiencing, avoidance, and hyperarousal).
Prevalence of PTSD in WTC Responders
The first paper on probable PTSD in WTC-HP responders examined more than 10,000 participants whose first monitoring visit occurred within 5 years of the attack [3]. Eleven percent met criteria for probable PTSD, a rate the authors described as similar to the rate in US veterans returning from Afghanistan. The rate is also almost three times higher than the rate of PTSD among men in the general population who reported being exposed to a traumatic event (4.1%; [4]). Stellman et al. also found that PTSD decreased across the 5 years of observation (2002–2006), but a study of FDNY using data from the same period of time found the reverse, namely, that the rate of probable PTSD increased during that period [5]. In addition to the early reports from the WTC-HP and FDNY programs, a number of reports on probable PTSD were published by the WTC-HR. The latter confirmed the high rate of PTSD in responders and also reported significantly more PTSD in nontraditional compared to police responders [6], a pattern also observed in WTC-HP participants [7]. Subsequently, Pietrzak et al. [8] conducted trajectory analyses using PCL data from WTC-HP responders’ three initial monitoring visits and found that 5.3% of police and 9.5% of nontraditional responders had chronically elevated symptom levels. The data from all three large monitoring programs were consistent in reporting that exposure severity, defined by variables such as death of colleagues, early arrival at the site (September 11 to September 12), injuries, and relatively long duration of work, was significantly associated with an increased rate of PTSD.
A few studies evaluated the long-term prevalence of probable PTSD more than a decade after 9/11. Cone et al. [9] analyzed data from police enrolled in the WTC-HR and found that 11% had probable PTSD at 10–11-year follow-up, half of whom also had PTSD at earlier time points. Thus, even more than a decade after 9/11, in men who were previously considered “a healthy worker” cohort and indeed were screened for resilience prior to entry into the police academy, the rate of long-term, probable PTSD was more than double that of an unselected sample of men in the general population who reported trauma exposure.
To date, only four studies of WTC-PTSD in responders have been based on actual clinical diagnostic interviews rather than the PCL. A clinical interview allows a professional rater to probe for all DSM-IV criteria, symptoms, duration, and impairment. Two studies administered the Clinician-Administered PTSD Scale [10], which is considered the gold standard for assessment of PTSD. The first study assessed mental health relief workers 6–8 months after 9/11; 6.4% met developed WTC-related PTSD [11]. The second was a longitudinal study of utility workers that reported a decline in PTSD from 15% in 2002 to 5% in 2008 [12]. The Diagnostic Interview Schedule was administered to a large sample of retired firefighters 5–6 years after 9/11; 7% of the sample had active PTSD [13]. The fourth study was conducted at the Stony Brook WTC-HP and involved an assessment of ~3500 responders in 2012–2014 using the Structured Clinical Interview for DSM-IV (SCID ; [14]). Eighteen percent developed WTC-PTSD during that period, and 10% had current PTSD at the time of interview. Consistent with the PCL findings, the rates were higher in nontraditional than police responders and were significantly associated with severity of exposure (early arrival, longer hours of work, exposure to the dust cloud).
Comorbidity of PTSD and Physical Health
A large number of studies have shown strong reciprocal and longitudinal associations of PTSD with several aspects of physical health , particularly respiratory (e.g., [7, 15]) and gastrointestinal [16, 17] conditions. The Stony Brook studies in particular [7, 15] showed that PTSD was not just a correlate but was a significant driver of lower respiratory symptoms, with new onsets being twice as common and recovery being half as common in responders with PTSD at their previous visit compared to responders free from PTSD. This finding was consistent with evidence of a biological pathway between these conditions. As shown in Fig. 1, the pathway also includes poor health behaviors, such as smoking and substance abuse.
Pathways between PTSD and lower respiratory symptoms. Modified from Vaccarino and Bremner [26]
Indeed, it is important to note that PTSD has consistently been tied to neurohormonal dysregulation in stress response systems (e.g., [18]), including sympathetic hyperactivity [19] and altered hypothalamic-pituitary-adrenal (HPA) axis functioning [18]. The latter has been reflected in low peripheral cortisol at rest, increased suppression during pharmacological challenge paradigm, and increased cortisol reactivity following cognitive challenge. Dysfunction in both sympathetic and HPA systems is known to be associated with increased levels of pro-inflammatory cytokines (e.g., interleukin-1 and interleukin-6) (e.g., [20]). Of note, immunologic dysregulation has been documented across several studies of PTSD. These inflammatory processes in turn may contribute to medical comorbidities, including respiratory illnesses, as observed in the Stony Brook responder cohort [15].
In addition to associations between PTSD and physical health, a recent study showed that PTSD, especially the reexperiencing symptom cluster, was also predictive of cognitive impairment 14 years after 9/11 [21]. Recent studies of veterans have also shown associations between PTSD and cognitive impairment, but a large proportion of veteran samples has comorbid traumatic brain injuries, making it difficult to disentangle the effects of PTSD from those of traumatic brain injury. While the results from the Stony Brook study need to be replicated, if confirmed, they suggest that the consequences of persistent PTSD reach beyond the medical symptoms that have been the focus of most of the WTC research to date. They also raise questions about potential changes in the brain resulting from chronic and persistent PTSD.
The findings on PTSD in WTC responders have been consistent with 50 years of research showing that mental ill health is associated with disability, physical morbidity, and even mortality. Thus, treating PTSD in WTC responders and survivors is a priority for WTC health programs as well as society more generally. The most commonly prescribed medications are antidepressants, and the most common forms of psychotherapy are psychoeducation, exposure therapy, and cognitive behavioral therapy. However, it has been estimated that the majority of individuals with PTSD either improve slowly or fail to improve after various medication and psychotherapy trials. Thus, in light of the protracted nature of PTSD, the need for care remains a continuing challenge.
Comorbidity of PTSD and Major Depression
Many clinical- and population-based studies have shown that PTSD and major depressive disorder are significantly comorbid and that this is particularly true for chronic PTSD , as shown in several WTC PCL-based studies (e.g., [9, 22, 23]) and diagnosis-based research [14]. In the Stony Brook study of 3504 responders, 204 responders met diagnostic criteria for both current DSM-IV PTSD and current major depressive disorder (MDD) 11–13 years after 9/11. This represented almost half (47.7%) of responders with either one of these disorders (N = 428; odds ratio = 1.42; 95% confidence interval = 1.43–1.53; p = 0.000). For the remainder of the chapter, we explore whether responders with current comorbid PTSD/MDD were significantly more disadvantaged with regard to their health and quality of life than responders with single or with no current disorder.
Specifically, we compared three groups: responders with current DSM-IV PTSD/MDD, responders with either PTSD or MDD , and responders with neither condition (Table 1). We first compared them on demographic characteristics. In the three-way comparison, the groups were similar in age at the time of 9/11 but differed significantly on sex, occupational and marital status, and police versus nontraditional responder status. That is, the comorbid PTSD/MDD group contained the largest proportion of women, unmarried and unemployed responders, and those coming from nontraditional occupations, while the group with neither condition contained the fewest responders who were female, unmarried, out of the workforce, or in the nontraditional responder category. The single-disorder group fell in between. Of note, two-thirds of responders with PTSD/MDD were out of the workforce compared to ~50% in the single-disorder group and one-quarter in the group having neither disorder. The two-way comparisons of responders in the PTSD/MDD versus single-disorder groups indicated a trend for those with both disorders to be older (p = 0.057) and not in the workforce (p = 0.052).
Regarding WTC experiences, we analyzed two key exposures and two key health effects. With regard to exposures, the three groups did not differ significantly on dust cloud exposure. However, three-quarters of responders with single and with comorbid PTSD/MDD lost colleagues and friends when the towers collapsed compared to two-thirds of responders with neither disorder (p = 0.002). In terms of WTC health effects, responders with neither PTSD nor MDD were the least, and comorbid PTSD/MDD responders the most, likely to have current lower respiratory symptoms and to report that they were told by a doctor that they have a WTC-related condition. In the no-disorder group, 44.2% reported that they were diagnosed with a WTC-related condition. In contrast, among responders with comorbid PTSD/MDD, 81.9% reported such a diagnosis. In the single-disorder group, the figure was 68.3% (p value for the two-way comparison = 0.003).
We next examined health-related quality of life (self-rated health as poor or very poor on a five-point scale) and impairments in life satisfaction, relationships with friends, and adequacy of social support. The latter three domains were determined from the Range of Impaired Functioning Tool (RIFT) developed by Leon et al. [24]. These domains represent interviewer ratings made after a series of probes on a five-point scale from very positive to very negative. Impairment scores for each scale were dichotomized as follows: life satisfaction (fair/poor/very poor versus good/very good), impaired friendships (mild/moderate/severe impairment versus satisfactory/non-impaired friendships), and social support (fair/poor social network involvement versus good/very good).
As shown in Table 1, each of the three-way comparisons was highly significant, with the no-disorder group having the lowest and the comorbid group the highest percent reporting poor subjective health and rated as having impairment in each domain. Indeed, four out of five comorbid responders had impaired life satisfaction, and two out of three had inadequate social support. The rank ordering across the three groups was particularly striking. The two-way comparison further indicated that significantly more comorbid responders had poor subjective health ratings and impaired functioning compared to responders with a single disorder (p ≤ 0.001).
Conclusion
WTC experiences have taken an enduring toll on responders. Fortunately, there are programs in place to monitor and treat their physical and mental health conditions. Comorbid PTSD/MDD has proven to be a particularly severe mental health outcome, having an adverse association with not just physical health but also quality of life. One surprising finding was that although nontraditional responders are at increased risk of long-term PTSD and MDD, there was no difference by responder status in the rate of comorbid PTSD/MDD. In general, the findings from the published literature and from this secondary analysis of comorbid PTSD/MDD 11–13 years after 9/11 showed that half of responders with long-term PTSD also had comorbid MDD and comorbidity was associated with multiple forms of impairment many years after 9/11, including being out of the workforce and having poor life satisfaction. These results confirm earlier findings based on the PCL [23] and support the need for continued screening and treatment of both PTSD and MDD and comorbid PTSD/MDD.
Since the bombings in Japan in 1945, a number of toxic disasters have occurred, ranging from the gas leak at Bhopal primarily from methyl isocyanate (1984), to the vast radiation contamination from the explosion at the Chernobyl nuclear power plant (1986), to the sarin attack on the Tokyo subway (1995), and to the triple disaster in Fukushima which led to the evacuation of 220,000 residents living in the 20–30 km area near the Daiichi plants (2011). Each event had both physical and mental health consequences. Yet only after the WTC attacks were both physical and mental health evaluated concurrently. After the Fukushima radiation disaster, self-report health questionnaires were mailed to evacuees and other affected populations, and self-report mental health and lifestyle questionnaires were also posted. But they were done as separate mailings. After the three nuclear power plant accidents (Three Mile Island, Chernobyl, Fukushima), the consensus reports issued by the major international radiation agencies all concluded that the biggest public health impact of these events was on mental health. Yet in spite of the 1948 World Health Organization statement that health encompasses physical, mental, and social well-being, and in spite of the research findings on mental health after these large-scale toxic disasters, mental health was not viewed as a direct effect and hence did not fall within the purview of health monitoring and research programs, even as a risk factor. It is well established that mental and physical health are two sides of the same coin, each influencing the other, with mental health in some instances serving as the driver of physical morbidity and mortality. The fact that the WTC monitoring programs assess and offer treatment for both aspects of health has been a momentous step forward.
Since the first epidemiologic evidence on PTSD [25], the chronicity of PTSD has been well known. Furthermore, the original study by Kessler, the National Comorbidity Survey, showed that respondents with a history of untreated PTSD had a longer course of illness than those who had sought treatment. PTSD is one of the most difficult disorders to treat effectively, in part because of its complexity and in part because of its comorbidity with other disorders, including depression described in this chapter but also substance abuse and other anxiety disorders. Nonetheless, some treatments, such as exposure therapy and antidepressants, are effective for some individuals. Although treatment often proceeds by trial and error, it is reasonable to hope that an effective treatment can be found for responders with PTSD, even if initiated long after its onset. Short of that, long-term support from clinical staff in programs such as the Stony Brook WTC-HP and certification of PTSD and depression, which allows for treatment without charge to the responders, minimize the sense of isolation and unhappiness that arise in individuals with chronic mental disorders.
Abbreviations
- DSM-IV:
-
Diagnostic and Statistical Manual of Mental Disorders 4th edition
- FDNY-WTC-MMP:
-
Fire Department of the City of New York World Trade Center Medical Monitoring Program
- MDD:
-
Major depressive disorder
- NIOSH:
-
National Institute of Occupational Safety and Health
- PCL:
-
Posttraumatic Symptom Checklist
- PTSD:
-
Posttraumatic stress disorder
- RIFT:
-
Range of Impaired Functioning Tool
- SCID:
-
Structured Clinical Interview for DSM-IV
- WTC:
-
World Trade Center
- WTC-HP:
-
World Trade Center Health Program
- WTC-HR:
-
World Trade Center Health Registry
References
Dasaro CR, Holden WL, Berman KD, Crane MA, Kaplan JR, Lucchini RG, et al. Cohort profile: World Trade Center Health Program general responder cohort. Int J Epidemiol. 201510.1093/ije/dyv099. Epub.
Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34(8):669–73.
Stellman JM, Smith RP, Katz CL, Sharma V, Charney DS, Herbert R, et al. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect. 2008;116(9):1248–53.
Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25(3):456–65.
Berninger A, Webber MP, Cohen HW, Gustave J, Lee R, Niles JK, et al. Trends of elevated PTSD risk in firefighters exposed to the World Trade Center disaster: 2001–2005. Public Health Rep. 2010;125(4):556–66.
Perrin MA, DiGrande L, Wheeler K, Thorpe L, Farfel M, Brackbill R. Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers. Am J Psychiatry. 2007;164(9):1385–94.
Luft BJ, Schechter C, Kotov R, Broihier J, Reissman D, Guerrera K, et al. Exposure, probable PTSD and lower respiratory illness among World Trade Center rescue, recovery and clean-up workers. Psychol Med. 2012;42(5):1069–79.
Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, et al. Trajectories of PTSD risk and resilience in World Trade Center responders: an 8-year prospective cohort study. Psychol Med. 2014;44(1):205–19.
Cone JE, Li J, Kornblith E, Gocheva V, Stellman SD, Shaikh A, Schwarzer R, et al. Chronic probable PTSD in police responders in the world trade center health registry ten to eleven years after 9/11. Am J Ind Med. 2015;58(5):483–93.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8(1):75–90.
Zimering R, Gulliver SB, Knight J, Munroe J, Keane TM. Posttraumatic stress disorder in disaster relief workers following direct and indirect trauma exposure to Ground Zero. J Trauma Stress. 2006;19(4):553–7.
Cukor J, Wyka K, Mello B, Olden M, Jayasinghe N, Roberts J, et al. The longitudinal course of PTSD among disaster workers deployed to the World Trade Center following the attacks of September 11th. J Trauma Stress. 2011;24(5):506–14.
Chiu S, Webber MP, Zeig-Owens R, Gustave J, Lee R, Kelly KJ, et al. Performance characteristics of the PTSD Checklist in retired firefighters exposed to the World Trade Center disaster. Ann Clin Psychiatry. 2011;23(2):95–104.
Bromet EJ, Hobbs MJ, Clouston SA, Gonzalez A, Kotov R, Luft BJ. DSM-IV post-traumatic stress disorder among World Trade Center responders 11–13 years after the disaster of 11 September 2001 (9/11). Psychol Med. 2016;46(4):771–83.
Kotov R, Bromet EJ, Schechter C, Broihier J, Feder A, Friedman-Jimenez G, et al. Posttraumatic stress disorder and the risk of respiratory problems in World Trade Center responders: longitudinal test of a pathway. Psychosom Med. 2015;77(4):438–48.
Litcher-Kelly L, Lam Y, Broihier JA, Brand DL, Banker SV, Kotov R, et al. Longitudinal study of the impact of psychological distress symptoms on new-onset upper gastrointestinal symptoms in World Trade Center responders. Psychosom Med. 2014;76(9):686–93.
Wisnivesky JP, Teitelbaum SL, Todd AC, Boffetta P, Crane M, Crowley L, et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet. 2011;378(9794):888–97.
Yehuda R. Status of glucocorticoid alterations in post-traumatic stress disorder. Ann N Y Acad Sci. 2009;1179:56–69.
Pole N. The psychophysiology of posttraumatic stress disorder: a meta-analysis. Psychol Bull. 2007;133(5):725–46.
Spitzer C, Barnow S, Völzke H, Wallaschofski H, John U, Freyberger HJ, et al. Association of posttraumatic stress disorder with low-grade elevation of C-reactive protein: evidence from the general population. J Psychiatr Res. 2010;44(1):15–21.
Clouston SA, Kotov R, Pietrzak RH, Luft BJ, Gonzalez A, Richards M, et al. Cognitive impairment among World Trade Center responders: Long-term implications of re-experiencing the 9/11 terrorist attacks. Alzheimers Dement (Amsterdam). 2016;19(4):67–75.
Bowler RM, Kornblith ES, Li J, Adams SW, Gocheva VV, Schwarzer R, et al. Police officers who responded to 9/11: comorbidity of PTSD, depression, and anxiety 10–11 years later. Am J Ind Med. 2016;59(6):425–36.
Caramanica K, Brackbill RM, Liao T, Stellman SD. Comorbidity of 9/11-related PTSD and depression in the World Trade Center Health Registry 10–11 years postdisaster. J Trauma Stress. 2014;27(6):680–8.
Leon AC, Solomon DA, Mueller TI, Turvey CL, Endicott J, Keller MB. The range of impaired functioning tool (LIFE-RIFT): a brief measure of functional impairment. Psychol Med. 1999;29(4):869–78.
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–60.
Vaccarino V, Bremner JD. Traumatic stress is heartbreaking. Biol Psychiatry. 2013;74(11):790–2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Bromet, E.J., Kotov, R., Luft, B.J. (2018). Long-Term PTSD and Comorbidity with Depression Among World Trade Center Responders. In: Szema, A. (eds) World Trade Center Pulmonary Diseases and Multi-Organ System Manifestations. Springer, Cham. https://doi.org/10.1007/978-3-319-59372-2_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-59372-2_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59371-5
Online ISBN: 978-3-319-59372-2
eBook Packages: MedicineMedicine (R0)