Abstract
In bone remodeling, a variety of mechanical and biochemical signaling occurs among osteoclasts and osteoblasts, which are responsible for bone resorption and formation, and osteocytes, which are believed to have a mechanosensing function. Biomechanics research incorporating mathematical modeling and computer simulations is being conducted in order to understand the functional adaptation of bone structure by remodeling that can be observed at a macroscopic level resulted from the complex interaction among these signals at molecular and cellular levels.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Bone remodeling
- Bone adaptation
- Osteocytes
- Mechanosensing
- Micro finite element analysis
- Computer simulations
1 Introduction
The details of intracellular signaling mechanisms and cell-cell interactions involved in the control of bone metabolism are gradually being clarified [1,2,3,4]. Moreover, a further development in biomechanics research [5,6,7] in order to understand the mechanical adaptation phenomenon, known as Wolff’s Law, is anticipated with advances in bone cell mechanobiology researches [8, 9]. However, while our understanding of the detailed mechanism at cellular and molecular levels increases, difficulties are still being faced in understanding the control dynamics of the bone remodeling system that occurs at the macroscopic level and emerges over the hierarchy of interaction between these elements due to the complexity involved.
Mathematical modeling and computational simulation research have recently garnered attention as means of comprehensively understanding the dynamics of complex systems [6, 10, 11]. The phenomenon by which the remodeling activity of osteoclasts and osteoblasts is regulated via the process of mechanical and biochemical signaling is not only temporally regulated but also spatially regulated, depending on the distance between and the location of cells. Moreover, in order to understand the functional adaptation phenomenon of bone as a result of remodeling, it is necessary to first understand the correlation between mechanical function and changes in bone morphology that arise from both the forces acting on bone and the deformation of the bone matrix. In other words, it is important to not only track the evolution of complex signaling but also to understand the relationship between bone structure and function and the deeply involved dynamic field.
2 From the Macroscopic Structure to the Microscopic Cellular Responses of Bone
2.1 Hierarchical Structure of Bone
Adaptive bone remodeling can be understood in terms of the relationship between forces and bone structure on a macroscopic level. However, remodeling occurs as a result of the coupling activity of osteoclasts and osteoblasts on a microscopic level. The relationship with osteocyte mechanosensing on a molecular level is also important. As shown in Fig. 1, cancellous bone is composed of a cancellous, trabecular network structure. A trabecular cross-section of this bone reveals a newly-formed lamellar bone matrix on the trabecular surface as a result of bone resorption and formation activity by osteoclasts and osteoblasts. Furthermore, osteocytes discretely present within the trabecular matrix form a dense network that extends to numerous cell processes.
2.2 Bone Remodeling Regulation by Mechanical Stimuli
Bone remodeling is thought to be regulated by the accumulation of microscopic damage, localized stress and strain, and mechanical stimuli such as the interstitial fluid flow within bone canaliculi into which cell processes extend [12, 13]. Furthermore, an experiment in which isolated osteocytes were loaded with localized mechanical stimuli demonstrated that the cell processes are particularly sensitive to mechanical stimuli [14]. The magnitude of macroscopic elastic strain that occurs in bone is usually no more than 0.1–0.2%, and even if such small deformation is directly applied to osteocytes and osteoblasts, cellular responses such as an influx of calcium ions or nitric oxide production are not observed. This suggests the presence of an amplification mechanism for mechanical stimuli on a microscopic cellular and/or molecular level.
Hierarchical structure of bone from the trabecular structure of cancellous bone, the osteocyte networks within bone matrix, to the osteocyte processes within the canaliculi (This figure was partially adapted from Ref. [26] with permission from Elsevier.)
2.3 The Mechanobiology of Osteocytes
The processes of osteocytes [9, 15, 16] that have garnered attention as mechanosensor cells of bone contain many actin filament bundles, the morphological characteristics of which are very interesting. It is conceivable that some kind of mechanosensing function exists on the scale of these cell processes. For example, the interstitial fluid flow within bone canaliculi places shear stress on the cell processes, while local linked structures between the walls of the bone canaliculi and the surface of the cell processes may act as a mechanism for transmitting mechanical signals (forces) by amplifying small deformation or stress of the membranes and internal cytoskeletal structure of cell processes [17]. Furthermore, responses to fluid shear stress by micro-patterned osteocyte networks have been observed [18], and models depicting the role of the primary cilia in the mechanosensing mechanism of osteocytes have been proposed [19, 20]. Thus, future detailed clarification of the mechanosensing mechanism of osteocytes is strongly required.
3 The Mathematical Modeling and Computational Biomechanics Approach
As shown in Fig. 1, it is not easy to explain the pattern formation of the trabecular structure in cancellous bone on the most macroscopic level based on the detailed mechanisms at a microscopic level. This is due to the size of the gap between the temporal and spatial hierarchy from molecular and cellular level to the tissue and organ level, even when the mechanosensing mechanism at the osteocyte level is elucidated in detail at the molecular level. Mathematical modeling with computational biomechanics is therefore a promising approach.
3.1 Classic Mathematical Models of Mechanical Adaptation by Bone Remodeling
Many phenomenological mathematical models of bone remodeling representing bone resorption and formation have been proposed to date, in which bone remodeling occurs by referring to the macroscopic mechanical state of bone, as typified by the mechanostat theory [21,22,23,24]. In contrast, we proposed a mathematical model in which local mechanical nonuniformity at the cell level appears to drive trabecular remodeling [25, 26]. The top left image in Fig. 1 shows the cancellous bone structure of the human proximal femur predicted by a large-scale computer simulation using this model [26]. It shows that the three-dimensional trabecular structure, which appears very similar to the actual structural pattern, can be predicted with an extremely simple local rule.
3.2 Mechanosensing and Communication of Osteocytes
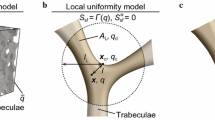
The bottom-up approach, in which knowledge obtained at the cellular and molecular levels is pieced together, is an important approach in regard to the above-mentioned phenomenological approach. The authors proposed a mathematical model of bone remodeling (Fig. 2a) in which the cell processes of osteocytes and the bone canalicular network are assumed to play an important role in mechanosensing and communication (Adachi et al. 2010; Kameo et al. 2011a). The trabeculae were first modeled as poroelastic media containing a bone lacuno-canalicular network, after which a mathematical model of bone remodeling was constructed from mechanosensing of fluid shear stress by osteocytes up to bone resorption and formation by osteoclasts and osteoblasts. As a result, shear stress placed on the surface of the cell processes due to the interstitial fluid flow associated with the dynamic deformation of the bone matrix was regarded as mechanical stimuli applied to osteocytes. We were thus able to demonstrate that trabecular morphology functionally adapts and changes to make the stress distribution on the trabecular surface uniform, i.e. to align the trabeculae in the direction of loading.
3.3 Flow Analysis Within Bone Canaliculi Using an Image-Based Model
Kamioka et al. visualized a detailed three-dimensional image (Fig. 2c) of the canaliculi and cell processes within the bone matrix using an ultra-high voltage electron microscope and electron tomography (Fig. 2b) [27]. They also analyzed the microscopic flow in the gaps surrounding the cell processes using the obtained digital image model (Fig. 2d). They found that interstitial fluid within the gaps exhibited a complex flow that depended greatly on location as a result of the irregular surfaces of the canalicular walls. This suggested that local force and deformation affect the cell processes. Furthermore, if it is revealed that the microscopic morphology and environment of the bone lacunae and canaliculi change as a result of various factors [28], this could lead to an understanding of changes in the microscopic mechanical environment surrounding osteocytes and changes in mechanosensing characteristics.

(b–d were adapted from the Ref. [27] with permission from The Royal Society of Chemistry.)
Mathematical model of trabecular remodeling considering osteocyte mechanosensing and communication. a Force applied to bone causes bone matrix deformation. This results in a pressure gradient in the interstitial fluid within the bone canaliculi network, causing interstitial fluid flow. As a result of this flow, shear stress (force) acts on the surfaces of osteocyte processes, which are sensitive to mechanical stimuli. When osteocytes sense this shear force, signals are transmitted to the trabecular surfaces via intercellular communication, which regulates trabecular remodeling activity by osteoclasts and osteoblasts and results in changes in the trabecular structure of cancellous bone. b Using ultra-high voltage electron microscopy computed tomography scans, c we created an image-based model of the cell processes and canalicular walls, and d analyzed the microscopic flow of interstitial fluid.
4 Modeling Mechanosensing Osteocytes in Bone Adaptation
We previously proposed a mathematical model to represent bone cellular activities in response to mechanical loading based on the assumption that osteoclastic bone resorption and osteoblastic bone formation are regulated by mechanosensing osteocytes [5, 6, 29]. In this model, the process of trabecular bone remodeling consists of three parts: (i) cellular mechanosensing, (ii) intercellular signal transmission, and (iii) trabecular surface movement owing to remodeling, as shown in Fig. 3. A summary of each process is explained below by introducing some physiologically rational assumptions.Footnote 1

(This figure was reproduced from Ref. [29] with permission of Springer.)
Theoretical framework for trabecular bone remodeling considering the mechanical hierarchy from the microscopic level (\(\sim \)1 \(\upmu \)m) to the mesoscopic level (\(\sim \)100 \(\upmu \)m). The remodeling process consists of the following three parts: (i) cellular mechanosensing, (ii) intercellular signal transmission, and (iii) trabecular surface movement. The change in trabecular structure is caused by osteoclastic bone resorption and osteoblastic bone formation. Their remodeling activities are regulated by osteocytes in response to the interstitial fluid flow in canaliculi.
4.1 Cellular Mechanosensing
In the cellular mechanosensing process, osteocytes were assumed to be sensitive to fluid-induced shear stress acting on their cellular processes. For evaluating the shear stress, we adopted the microstructure model of Weinbaum et al. [12], which accounts for the interstitial fluid flow through a fiber matrix in an annular canaliculus. Using the fluid pressure gradient at the trabecular level, \(\nabla p\), the fluid-induced shear stress, \(\tau _p\), acting on the osteocyte processes aligned in direction \(\varvec{n}\) is given as:
where q is the ratio of the radius of the canaliculus \(r_c\) to that of the process \(r_p\), i.e., \(q=r_c/r_p\), \(I_1\) and \(K_1\) are the modified Bessel functions of the first order, and the other constants are defined in Weinbaum et al. [12].
Assuming the biochemical signal that osteocytes produce in response to the fluid-induced shear stress \(\tau _p\) is proportional to the shear force on their processes, the signal \(S_{OC}(\varvec{x})\) produced by the osteocytes per unit bone volume can be defined, using the volume fraction of the canaliculi oriented in direction \(\varvec{n}\), \(\rho _c(\varvec{n})\), introduced in Kameo et al. [30], as follows:
where \(\theta \) is the angle between the vector \(\varvec{n}\) and the \(x_3-\)axis in the arbitrary Cartesian coordinate system, \(\varphi \) is the angle between the \(x_1-\)axis and the projection of \(\varvec{n}\) onto the \(x_1 x_2-\)plane measured counterclockwise, \(\alpha \) is the mechanosensitivity of the osteocytes, and \(|\overline{\tau _p(\varvec{x},\varvec{n})}|\) is the time-averaged shear stress over the course of one day. For simplicity, we set \(\alpha =1\) for all of the osteocytes and assumed the isotropy of canalicular orientation, i.e., \(\rho _c(\varvec{n})=\phi /2\pi \), where \(\phi \) is the porosity of the trabeculae.

(This figure was reproduced from Ref. [29] with permission of Springer.)
Relationship between the rate of trabecular surface remodeling \(\dot{M}\) and the total stimulus \(S_{sf}\) that the trabecular surface cell receives from the neighboring osteocytes. This relationship is assumed to be represented by a piecewise sinusoidal function.
4.2 Intercellular Signal Transmission
The signals produced are modeled to be transmitted to the effector cells on the trabecular surface, such as osteoclasts and osteoblasts, through the intercellular network system of bone cells. With the use of a weight function w(l) that represents the decay in the signal intensity relative to the distance l, the total stimulus \(S_{sf}\) on the trabecular surface position \(\varvec{x}_{sf}\) is obtained in the following integral form:
where \(l=|\varvec{x}_{sf}-\varvec{x}|\), and distance \(l_L\) denotes the maximum distance for intercellular communication and determines the communication area \(\varOmega \). The total stimulus \(S_{sf}\) is a positive scalar function and is regarded as the driving force of trabecular bone remodeling.
4.3 Trabecular Surface Movement
In order to express the trabecular surface movement owing to remodeling, we introduced a piecewise sinusoidal function that describes the relationship between the rate of trabecular surface remodeling \(\dot{M}\) and the total stimulus on the trabecular surface \(S_{sf}\), as shown in Fig. 4. This empirical function indicates that bone resorption is initiated by stimuli below the remodeling equilibrium and that bone formation is initiated by stimuli exceeding the equilibrium. In this function, \(S_{sf}^U\) is the upper threshold for bone formation, \(S_{sf}^L\) is the lower threshold for bone resorption, \(S_{sf}^O\) is a stimulus at the remodeling equilibrium, and \(S_{sf}^Z\) is the width of the lazy zone. The maximum rates of resorption and formation are assumed to have the same absolute value \(\dot{M}_{max}\) in order to simplify the numerical algorithm, whereas, in reality, the formation rate of osteoblasts is much smaller than the resorption rate of osteoclasts. The level set method [31], which is a numerical technique for tracking the interfaces and shapes of materials, was employed to express trabecular surface movement in this simulation.
5 Adaptation of a Single Trabecula to a Bending Load
The individual trabecula has a characteristic morphology that is strut-like or plate-like in form depending on its position within cancellous bone. While it is certain that the morphology is associated with the mechanical environment, the determinant remains unclear. Therefore, we hypothesized that the trabecular morphology is influenced by a type of load such as a uniaxial or bending load, and demonstrated the reorientation of the strut-like trabecula under cyclic uniaxial loading [5, 6]. In the present study, we investigated the effects of a bending load on the changes in trabecular morphology [29]. By applying our mathematical model of bone remodeling to the three-dimensional voxel finite element model of a trabecula, we performed a bone remodeling simulation for a single trabecula subjected to a cyclic bending load.
5.1 Voxel Finite Element Model of a Single Trabecula
A three-dimensional computational model of a single trabecula for simulating the morphological changes via bone remodeling was constructed as shown in Fig. 5. The region for analysis was \(a_1 \times a_2 \times a_3 = 0.8\,\text {mm} \times 1.6\,\text {mm} \times 1.2\,\text {mm}\), which was divided into \(20 \times 40 \times 30\) cubic voxel finite elements. A strut-like trabecula having a diameter of 240 \(\upmu \)m was placed at the center of the region along the direction of the \(x_3\)-axis. The trabecula was modeled as a poroelastic material with homogeneous and isotropic material properties (Table 1) [33, 34]. In order to impose external loadings, two parallel plates, each having a thickness of 40 \(\upmu \)m, were added to the upper and lower surfaces of the region for analysis. The shape of the plates did not change throughout the remodeling process, and the plates were assigned the same material properties as the trabeculae. As mechanical boundary conditions, a shear-free boundary condition was applied to the lower plate, and free leakage of interstitial fluid on the trabecular surfaces was assumed. A cyclic bending load, which was linearly distributed along the \(x_2\) direction \(\sigma = (2 \sigma _3 x_2/a_2) sin(2\pi f t)\) (\(f=1\) Hz), was imposed on the upper plate in the \(x_3\) direction for 1.0 s per day. In order to investigate the effects of the magnitude of the applied bending load on the trabecular morphology, the value of \(\sigma _3\) was determined as \(\sigma _3 = -0.10\,\text {and}\,-0.15\) MPa based on a previous remodeling simulation of cancellous bone [35]. The physiological parameters introduced in the remodeling model are as listed in Table 2 [8, 36,37,38]. With the exception of the parameters associated with the mechanical stimulus, i.e., \(S_{sf}^U\), \(S_{sf}^L\), \(S_{sf}^O\), and \(S_{sf}^Z\), which were determined arbitrarily, all of the parameter settings were based on experimental findings. Among the above four parameters, \(S_{sf}^Z\) representing a remodeling rate sensitivity to the stimulus near the remodeling equilibrium had a greater influence on the changes in bone volume [6]. Therefore, we performed trabecular remodeling simulations under two different settings of parameter \(S_{sf}^Z\), as listed in Table 2.

(This figure was reproduced from Ref. [29] with permission of Springer.)
Voxel finite element model of a single trabecula having a diameter of 240 m. A cyclic bending load, which was linearly distributed along the \(x_{2}\) direction, was applied to the upper plane along the \(x_{3}\) direction for 1.0 s per day.

(This figure was reproduced from Ref. [29] with permission of Springer.)
Changes in the trabecular morphology and average fluid-induced shear stresses in one day \(|\overline{\tau _p}|\) under a cyclic bending load when the width of the lazy zone \(S_{sf}^Z\) is 0.6 \(\upmu \)N. a \(\sigma _3 = -0.10 \) MPa and b \(\sigma _3 = -0.15\) MPa.
5.2 Results: Changes in Single Trabecular Morphology
Applying the proposed mathematical model of bone remodeling to the voxel finite element model of the trabecula, we investigated the morphological changes in a single trabecula subjected to an external cyclic bending load through remodeling simulations. Figures 6 and 7 show the distribution of the one-day average of the fluid-induced shear stress acting on the osteocyte processes \(|\overline{\tau _p}|\) at different stages of remodeling when the width of the lazy zone \(S_{sf}^Z\) is equal to 0.6 and 0.4 \(\upmu \)N, respectively. In both figures, part (a) corresponds to the results for the magnitude of bending load \(\sigma _3 = -0.10\) MPa, and part (b) corresponds to the results for \(\sigma _3 = -0.15\) MPa.

(This figure was reproduced from Ref. [29] with permission of Springer.)
Changes in the trabecular morphology and average fluid-induced shear stresses in one day \(|\overline{\tau _p}|\) under a cyclic bending load when the width of the lazy zone \(S_{sf}^Z\) is 0.4 \(\upmu \)N. a \(\sigma _3 = -0.10\) MPa and b \(\sigma _3 = -0.15\) MPa.
Under the loading condition of \(\sigma _3 = 0.10\) MPa, as shown in Fig. 6a, bone formation was promoted on all trabecular surfaces in the initial state owing to high fluid-induced shear stress. The bone formation along the \(x_2\) direction was dominant because the applied bending load was linearly distributed along the \(x_2\) direction. As a result, a plate-like trabecula, the dimension along the \(x_2\) direction of which is larger than that along the \(x_1\) direction, was formed after 10 days. Afterward, the morphology of the trabecula was almost unchanged, while a small cavity was formed close to the upper end.
The fluid-induced shear stress on the trabecular surfaces increases with the increase in magnitude of the applied bending load. When \(\sigma _3 = -0.15\) MPa, the remarkable bone formation for 10 days produced a plate-like trabecula with a larger width and thickness, as shown in Fig. 6b. After 20 days, unlike the case of \(\sigma _3 = -0.10\) MPa, when \(\sigma _3 = -0.15\) MPa significant bone resorption occurred around the central region of the trabecula near the neutral axis of bending because the fluid-induced shear stress decreased owing to the rapid bone formation along the \(x_2\) direction. As a result of subsequent bone resorption in the region, a branching structure was formed at the upper end of the plate-like trabecula.
Comparison of the changes in the trabecular morphology between the two different parameter settings of \(S_{sf}^Z\), as shown in Figs. 6 and 7, reveals that both remodeling processes are quite similar for the first 10 days. However, in the case of \(S_{sf}^Z = 0.4\) \(\upmu \)N, a comparatively large bone volume was lost owing to bone resorption around the central region of the plate-like trabecula. As shown in Fig. 7b, the plate-like trabecula split into two strut-like trabeculae under a large bending load.
5.3 Discussion
We demonstrated the morphological changes in a single trabecula under a cyclic bending load based on the remodeling model that incorporates cellular mechanosensing and intercellular signal transmission. As a result of remodeling simulations, a plate-like trabecula was formed after 10 days and the width and thickness increased with the increase in the magnitude of the bending load. The subsequent bone resorption around the central region of the trabecula contributed to the formation of a branching structure or split one plate-like trabecula into two strut-like trabeculae.
The trabeculae of cancellous bone in vivo are generally subjected to cyclic loading due to locomotion and maintenance of posture [12], which results in complex states of stress. The loading condition can be expressed as a superposition of multiple axial and bending loads in the simulation. Since the magnitude and the ratio of each load component are largely position-dependent in cancellous bone, we investigated the effects of uniaxial and bending loads separately in order to understand the basic and primary characteristics of trabecular bone remodeling. In a previous simulation study, we identified the formation of a strut-like trabecula aligned along the loading direction under pure uniaxial loading [5, 6]. In contrast, the results obtained in the present remodeling simulation reveal that the application of the bending loads influences not only the formation of the plate-like trabecula but also the change in trabecular topology. These results suggest the possibility that the characteristic trabecular morphology, such as a strut-like or plate-like form, is determined based on the local mechanical environment.
Whether the plate-like form is maintained for long periods depends on the magnitude of the bending load and the cellular activities at the trabecular surface. Comparing Fig. 6a, b reveals that a large bending load causes remarkable bone loss in the neighborhood of the neutral axis of bending owing to insufficient mechanical stimuli to osteocytes. This structural change appears in a trabecular remodeling simulation based on the phenomenological rule that remodeling progresses toward a locally uniform state of equivalent stress [35]. On the other hand, the decrease in the width of the remodeling lazy zone \(S_{sf}^Z\) accelerated the expansion of the resorption cavity around the central region of the trabecula, as shown in Fig. 7a, b. The lazy zone is also introduced in the mechanostat model by Frost [21, 24] as the ‘adaptive window’ and represents the ability of the surface cells to detect changes in local stimuli. This means that reducing the span of \(S_{sf}^Z\) increases the cellular sensitivity to the mechanical stimuli. Considering the biological characteristics of the lazy zone, the simulation results can be interpreted as indicating that a plate-like trabecula is likely to be formed when the cellular response is comparatively stable with respect to the change in local mechanical stimuli.
The proposed remodeling model contains 11 parameters to describe the three processes of trabecular bone remodeling without considering the material properties of the trabecula listed in Table 2: five parameters for (i) cellular mechanosensing (\(r_p\), \(r_c\), \(A_1\), \(B_1\), and \(\gamma \)), one parameter for (ii) intercellular signal transmission (\(l_L\)), and five parameters for (iii) trabecular surface movement owing to remodeling (\(\dot{M}_{max}\), \(S_{sf}^U\), \(S_{sf}^L\), \(S_{sf}^O\), and \(S_{sf}^Z\)). Among these parameters, the five parameters for cellular mechanosensing do not essentially influence the trabecular bone architecture because we assumed that they are constant by ignoring the position dependence of the geometry and dimensions of canaliculi. In the modeling of intercellular signal transmission, as the maximum distance for intercellular communication \(l_L\) increases, the mechanical state of trabeculae within a more global area is reflected in the total stimulus on the trabecular surface \(S_{sf}\) and the bone volume fraction will increase due to the enlarged total stimulus. The maximum remodeling rate \(\dot{M}_{max}\) is the parameter governing only the rate of bone resorption and formation and has little influence on the trabecular bone architecture in the state of remodeling equilibrium. The roles of the remaining four parameters associated with the mechanical stimulus, \(S_{sf}^U\), \(S_{sf}^L\), \(S_{sf}^O\), and \(S_{sf}^Z\), has been discussed in Kameo et al. [6], which reported that the morphological changes in the trabeculae are more sensitive to the parameter set of \(S_{sf}^O\), and \(S_{sf}^Z\) than to that of \(S_{sf}^U\) and \(S_{sf}^L\).
In order to validate our results quantitatively, it is crucial to appropriately set the physiological parameters based on a comparison with experimental findings. Unfortunately, such a comparison has not yet been successfully performed because of the difficulty in observing a single trabecula in vivo under a controlled mechanical condition. However, if we can reconstruct the three-dimensional trabecular bone architecture at the entire bone scale in silico with the aid of high-resolution scanners [39, 40], the image-based finite element analysis would help us to investigate the state of stress in the region of interest and to clarify the relationship between the trabecular microstructure and the local mechanical environment. Although it cannot be quantitatively validated, our mathematical model of trabecular bone remodeling has potential for investigating how the well-organized three-dimensional architecture of cancellous bone is produced by complex metabolic activities of numerous bone cells. By incorporating the biochemical features of bone cells, such as the signaling cascade, in our remodeling model, the refined model will contribute not only to the elucidation of the mechanism of bone remodeling but also to future clinical applications.
6 Adaptation of Cancellous Bone Tissue
Cancellous bone is porous bone that is composed of strut-like or plate-like trabeculae forming a well-organized three-dimensional architecture.Footnote 2 The remodeling simulation proposed in Sect. 5 can represent the functional adaptation of a single trabecula under physiological cyclic loading. In this section, we focus on structural changes in cancellous bone comprising multiple trabeculae in order to validate our model in silico at a more macroscopic level. We combined our remodeling model with the voxel finite element method in order to demonstrate the changes in cancellous bone morphology in response to uniaxial or bending loads and compared the results with experimental findings and the results of the previous simulation based on the phenomenological law of bone transformation.

(This figure was reproduced from Ref. [32] with permission of Springer.)
Three-dimensional model of cancellous bone for simulation of trabecular remodeling. In the initial configuration, all of the trabeculae are randomly oriented. This model was subjected to two types of monotonically increasing loading through the upper plate: i uniaxial loading and ii bending loading
6.1 Voxel Finite Element Model of Cancellous Bone
For simulating the morphological changes in bone tissue caused by local bone remodeling at the trabecular level, a three-dimensional computational model of cancellous bone was constructed as shown in Fig. 8. The region for analysis was \(a_1 \times a_2 \times a_3 = 3.2\,\text {mm} \times 3.2\,\text {mm} \times 3.2\) mm and was divided into \(80 \times 80 \times 80\) cubic voxel finite elements having an edge size of 40 \(\upmu \)m. This sample size was determined based on previous remodeling simulations of cancellous bone [41, 42]. In order to create an isotropic and uniform porous structure as the starting point for the model of cancellous bone, several pieces of torus-like trabeculae having an outer diameter of 360 \(\upmu \)m and an inner diameter of 280 \(\upmu \)m were placed randomly throughout the entire region in order to yield a bone volume fraction BV/TV of 0.4, which is within the physiological range. The effectiveness of this method was proven through two-dimensional [43, 44] and three-dimensional remodeling simulations [26]. The trabecula was modeled as a poroelastic material [45,46,47] with homogeneous and isotropic material properties, as listed in Table 2 [33, 34]. Two 200 \(\upmu \)m-thick plates by which to apply external loads were added to the upper and lower surfaces of the analyzed region. These plates were assigned the same material properties as the trabeculae, and their shapes were not changed by remodeling. A shear-free boundary condition was applied to the lower plane, and free leakage of interstitial fluid over all trabecular surfaces was assumed. In order to investigate the effects of different loading patterns on trabecular adaptation, two types of monotonically increasing loads \(\sigma = \sigma _3(x_1, x_2)t\) were imposed on the upper plane in the \(x_3\) direction for 0.25 s per day, as shown in Fig. 8. One was (i) a uniaxial load \(\sigma _3 = -8\) MPa/s and the other was (ii) a bending load that was linearly distributed along the \(x_2\) direction from \(-12\) to 12 MPa/s, i.e., \(\sigma _3 = -24 x_2/a_2\) [MPa/s]. The settings of the physiological parameters used in the remodeling model presented in Sect. 4 are summarized in Table 3 [8, 36,37,38]. With the exception of our parameters associated with mechanical stimulus, \(S_{sf}^U\), \(S_{sf}^L\), \(S_{sf}^O\), and \(S_{sf}^Z\), which were determined arbitrarily, all of the parameter settings were based on experimental findings.
6.2 Results: Changes in Cancellous Bone Morphology
We used the mathematical model of trabecular bone remodeling to simulate the remodeling of a cube of cancellous bone over a 30-day period in order to investigate the mechanical adaptation to uniaxial or bending loads. Figure 9 shows the morphological changes in cancellous bone. Figure 9a presents the results for uniaxial loading, and Fig. 9b presents the results for bending loading. In both figures, the color indicates the one-day average of the fluid-induced shear stress acting on the osteocyte processes, which is a driving force of bone remodeling. Independent of the type of external loading, the morphology of the cancellous bone gradually changed over time and the remodeled trabeculae had approximately circular cross-sections, as shown in Fig. 9a, b.

(This figure was reproduced from Ref. [32] with permission of Springer.)
Changes of the cancellous bone morphology and average fluid-induced shear stresses in one day \(|\overline{\tau _p}|\) a under uniaxial loading and b under bending loading
The application of a uniaxial load (Fig. 9a) resulted in bone resorption on all cancellous bone surfaces for the first three days due to the low fluid-induced shear stress, leading to a decrease in the bone volume fraction. After this stage, bone formation began on the vertically oriented trabeculae exposed to greater fluid-induced shear stress, despite the preferential loss of the horizontal trabeculae. Successive remodeling gradually decreased the degree of trabecular connectivity, and the trabeculae in the cancellous bone reoriented parallel to the direction of loading by the end of the 30-day simulation.
The application of a bending load to cancellous bone produced significant bone erosion around the central region for analysis, which was close to the neutral axis of bending, during the first three days, as shown in Fig. 9b. During the period from three days to six days, large numbers of trabeculae were lost from this region due to insufficient mechanical stimuli to osteocytes, while bone deposition occurred in the sides of the cancellous bone cube. After 30 days, the cancellous bone architecture reached a state of remodeling equilibrium in which the trabeculae around the central region were essentially absorbed and the remaining trabeculae aligned parallel to the direction of loading. This sequence of bone remodeling resulted in a locally inhomogeneous trabecular pattern within the cancellous bone cube.
6.3 Results: Distributions of Equivalent Stress
The spatial distributions of the mechanical quantities of the trabeculae are important determinants of the cancellous bone morphology in the state of remodeling equilibrium. The previously proposed mathematical model for bone remodeling assumed several mechanical quantities to be mechanical stimuli regulating the remodeling process [48]. In order to investigate the relationship between the cancellous bone architecture and the mechanical environment at the trabecular level, we focused on the distribution of von Mises equivalent stress \(\sigma _{eq}\) under the maximum load in one day as a typical mechanical quantity. We introduced the deviation of equivalent stress defined as
where Mean(\(\sigma _{eq}\)) denotes the mean value of \(\sigma _{eq}\) in the cancellous bone included in the region for analysis.
The distributions of the volume fractions corresponding to the deviation of equivalent stress \(\overline{\sigma _{eq}}\) are shown in Fig. 10. Figure 10a shows the distributions under uniaxial loading, and Fig. 10b shows the distribution under bending loading. The mean value and the standard deviation (s.d.) of the equivalent stress at different stages of remodeling are listed in Table 4. The initial distributions were asymmetric with respect to the mean value under both types of loading, although there was a slight difference in their kurtosis values. Their distributions shifted to nearly symmetrical bell-shaped curves as bone remodeling progressed. As shown in Table 4, the standard deviation of the equivalent stress decreased by 32% during the 30-day simulation regardless of the type of loading, whereas the mean value increased in both cases.

(This figure was reproduced from Ref. [32] with permission of Springer.)
Distributions of the volume fraction corresponding to the deviation of equivalent stress \(\overline{\sigma _{eq}}\) a under uniaxial loading and b under bending loading
6.4 Discussion
The process by which the cancellous bone architecture adapts to the mechanical environment has a hierarchy from the microscopic cellular level to the macroscopic tissue level. The apparent changes in the density and orientation of cancellous bone result from bone remodeling on the surfaces of the individual trabeculae, and the changes in trabecular morphology are caused by the metabolic activities of numerous bone cells. In the present study, we represented this hierarchical regulatory process in a mathematical model and demonstrated the structural changes in cancellous bone during uniaxial or bending loading in silico. Previous simulation models of the adaptation of the trabecular microstructure have assumed that remodeling is driven by mechanical stimuli, such as stress and strain, at the trabecular level (e.g., [23]). In contrast to these models, the proposed model considers the interstitial fluid flow, which acts directly on the osteocyte processes within the bone matrix, to be the most important stimulus. This simulation method should enable elucidation of the processes by which normal or pathological trabecular architecture develops in response to mechanical conditions at the cellular level.
The simulation results obtained herein indicated that subjecting cancellous bone with randomly arranged trabeculae to external loading resulted in alignment of the trabeculae parallel to the direction of loading and a well-organized architecture specific to the type of external loading, as shown in Fig. 9. Such reorientation of the trabeculae is a reasonable phenomenon from the viewpoint of functional adaptation and agrees qualitatively with in-vivo experimental observations of cancellous bone architecture under controlled mechanical conditions [49,50,51]. Comparing the cancellous bone morphology in the remodeling equilibrium state between the two loading conditions, as shown in Fig. 9a, b, shows that the trabecular pattern is more inhomogeneous under bending loading due to loss of bone around the central region for analysis, which corresponds to the neutral axis of bending. Although in-vivo experimental studies have not yet succeeded in confirming this phenomenon, a trabecular remodeling simulation based on the phenomenological rule that remodeling progresses toward a locally uniform state of equivalent stress suggested a similar pattern [35]. Under all types of loading, the trabeculae in the remodeling equilibrium state had approximately circular cross-sections because cylindrical trabecular morphology uniformizes the interstitial fluid velocity. The characteristic cross-sectional shape agrees with the anatomical observations of cancellous bone and was first represented by our original remodeling model. These results indicate that our mathematical model for trabecular bone remodeling can successfully predict the macroscopic changes in cancellous bone architecture based on the microscopic cellular activities.
The distributions of the mechanical quantities at the trabecular level are generally non-uniform due to the complexity of cancellous bone architecture. However, as shown in Table 4, the standard deviation of the equivalent stress decreased during the 30-day simulation under both uniaxial and bending loadings. This suggests that our remodeling model with osteocytes as the mechanosensors can represent the phenomenological law of bone transformation toward a locally uniform state of stress or strain at the trabecular level. The physical meaning of our mathematical model is that bone remodeling is driven by the gradient of interstitial fluid pressure (see Eqs. (1) and (2)) rather than by the hydrostatic pressure itself. This means that the balance of bone resorption and formation is assumed to be regulated by local differences in the mechanical conditions experienced by the trabeculae. In this sense, our model differs distinctly from the previous models in which remodeling was designed to obtain the global reference value of a particular mechanical quantity [23, 52] but is analogous to the model for remodeling caused by the local nonuniformity of equivalent stress [25]. Since the latter model, despite its basis on the phenomenological rule, can successfully describe a three-dimensional trabecular pattern similar to that in the actual human proximal femur [26], it seems reasonable to suppose that bone remodeling is influenced by the local distribution of certain mechanical quantities in the trabeculae rather than by the magnitude of stress or strain.
In our mathematical model, complex three-dimensional architectures of the lacuno-lanalicular porosity and the osteocyte network are ignored for simplicity even though they have a strong anisotropy. The effects of the microstructure on the osteocytic mechanotransduction via interstitial fluid flow can be represented in our simulation by using an anisotropic permeability tensor in the poroelastic analysis and considering the orientation dependence of the volume fraction of the canaliculi \(\rho _c(\varvec{n})\) [30]. In addition, our mathematical model is limited by the assumption of an empirical relationship between the rate of trabecular surface remodeling \(\dot{M}\) and the total stimulus on the trabecular surface \(S_{sf}\), which can be regarded as an index of local fluid pressure gradient. Despite these limitations, our mathematical model has the advantage of being able to investigate the effects of cellular mechanosensing and intercellular communication on the structural changes in cancellous bone. This trabecular remodeling simulation will definitely contribute to elucidating the mechanism of bone functional adaptation as a result of cellular activities. Future incorporation of the signaling cascade of bone cells into the mathematical model will make our simulation model a powerful tool for such clinical applications as the prediction of the effects of drugs targeting specific bone cells and the expected course of bone disease.
7 Mathematical Modeling of Spatiotemporal Dynamics at Microscopic Level
After mechanosensing by osteocytes, the remodeling activity of osteoclasts and osteoblasts is regulated by interactions between mechanical signals and intercellular biochemical signaling. These phenomena are not only regulated temporally (Fig. 11a) but may also be regulated spatially (Fig. 11b), for example through intercellular communication that depends on the distance between and location of cells and the diffusion of signaling molecules. Thus, simultaneously considering the spatiotemporal evolution of mechanical and physical fields, such as the deformation of bone matrix, the fluid flow within bone canaliculi, and the diffusion of signaling molecules, while incorporating morphological changes by bone remodeling, in addition to the conventional systems-biology approach that primarily describes their time evolution, is important.
Modeling and simulation of the temporal and spatial development of bone remodeling. Bone remodeling is understood as a a temporal evolution as a result of osteoclast and osteoblast coupling. b However, it is important to understand bone remodeling in terms of the system dynamics, which include spatiotemporal development, such as intercellular interactions via signaling and the diffusion of signaling molecules
7.1 Remodeling of Trabeculae and Osteons
The trabeculae in cancellous bone and osteons in cortical bone are recognized as bone remodeling units [53]. Here, we propose a model to directly describe the activity of cell groups referred to as remodeling packets at the microscopic structural level. The resorption pit on the trabecular surface in cancellous bone and the cutting cone of the Haversian canals present in the osteons in cortical bone are considered as individual units. The coupling of osteoclasts and osteoblasts in these remodeling units was mathematically modeled, and their activities were merged into a mathematical model for bone remodeling by taking into account both signaling mechanisms and mechanosensing mechanisms.
7.2 An Example of Osteoclast Differentiation Signals
Here, we develop a mathematical model of signals related to bone resorption with the receptor activator of nuclear factor \(\kappa \)B ligand (RANKL) as an example. As shown in Fig. 11a, b, RANKL expressed by osteoblasts and osteocytes is a ligand of RANK, which is expressed on the cell surface of osteoclast progenitors, and promotes differentiation into osteoclasts. Meanwhile, osteoprotegerin (OPG), which is secreted by osteoblasts and osteocytes, suppresses differentiation into osteoclasts by forming an OPG-RANKL complex. An example of this system is that dependent on spatial distance and time, such as the display of RANKL on the cell surface and/or its diffusion into the surroundings. Furthermore, by including the diffusion of OPG with its inhibitory function, the system dynamics are likely to be more complex.
7.3 Mathematical Modeling of Signaling Molecules in Bone Remodeling
We develop a model for bone remodeling in which mechanical stimuli to osteocytes activate cellular remodeling activities. First, assuming that osteocytes within the bone matrix can sense mechanical stimuli, the amount of mechanical stimuli \(S_{ocy}(\varvec{x})\) sensed by osteocytes is estimated based on the stress \(\sigma _{eq}(\varvec{x})\) within the bone matrix at location \(\varvec{x}\) (Adachi et al. 2009b, 2010). Next, we consider that the stimuli \(S_{ocy}(\varvec{x})\) sensed by osteocytes is transmitted to the trabecular and Haversian canal surfaces while decaying depending on the distance, then mechanical stimuli on their surfaces are evaluated as surface stimuli \(S_{sf}(\varvec{x},t)\). Assuming that the expression of OPG and RANKL, signal molecules associated with differentiation into osteoclasts, \(\phi _{OPG}(\varvec{x},t)\) and \(\phi _{RANKL}(\varvec{x},t)\), depends on \(S_{sf}(\varvec{x})\), we evaluate the concentrations of OPG and RANKL using an evolution equation:
in which the subscripts \((i, j) =\) (RANKL, OPG) or (OPG, RANKL). The first term on the right hand side of Eq. (5) represents the production of each signal molecule, and the amount of production is described by a function of the surface stimuli \(S_{sf}(\varvec{x})\). Here, the constant \(K_i\) represents the activation coefficient, whereas \(\beta \) represents the maximum level of expression. The second term represents the decrease due to inactivation by the binding of RANKL and OPG (with a constant \(k_{on}\)), whereas the third term represents the decrease due to the degradation of each molecule (with a constant \(k_{deg}\)). The fourth term represents the diffusion of each molecule within the bone marrow with a diffusion coefficient \(D_i\).
When the concentration of RANKL, \(\phi _{RANKL}\), becomes higher than the threshold \(C_{dif}\) shown in Fig. 11a, we consider this to indicate that new bone resorption will start on the trabecular surface and Haversian canal surface. Moreover, bone resorption and formation are considered to be controlled by the mechanical stimulation thresholds, \(S_{ocl}\) and \(S_{obl}\), shown in Fig. 11a. Based on this assumption, we determine the rate (speed) of remodeling on the trabecular surface and Haversian canal surface, and express the morphological changes in bone by bone resorption and formation.
8 Computer Simulations of Trabecular and Osteonal Remodeling
8.1 Trabecular Remodeling Simulation
We construct a model of an initial single trabecula (Fig. 12a) with a simple shape. The entire volume region for analysis is a 400 \(\upmu \)m \(\times \) 1,000 \(\upmu \)m \(\times \) 1,000 \(\upmu \)m rectangular solid, which is discretized using 10 \(\upmu \)m-voxel finite elements. The cylindrical trabecula with a radius of 80 \(\upmu \)m is tilted 30\(^{\circ }\) on the z-axis and is positioned in the center. A rigid plate is then positioned on the upper and lower surfaces and a uniform compression stress of \(\sigma _0=-0.2\) MPa is applied in the direction of the z-axis to the surface of the upper rigid plate as a boundary condition. Displacement perpendicular to the lower rigid plate was constrained.
Figure 12b, c show the changes in trabecular morphology and the amount of surface stimuli \(S_{sf}\) by remodeling. In their initial state, osteoclasts are randomly located on the trabecular surface. The results of the remodeling simulation confirmed that the morphology of the obliquely oriented trabecula changes to the direction along the compressive loading direction. This is because bone formation and resorption occur repeatedly in regions in which the surface stimulation \(S_{sf}\) are large (red) and small (blue), respectively, as shown in Fig. 12b, c.
8.2 Osteonal Remodeling Simulation
Figure 12c shows a model of the cutting cone in the Haversian canal of an osteon. The entire volume of analysis is a rectangular solid (600 \(\upmu \)m \(\times \) 600 \(\upmu \)m \(\times \) 2,000 \(\upmu \)m) that is regularly discretized using 10 \(\upmu \)m-voxel finite elements. A cylindrical Haversian canal having a radius of 80 \(\upmu \)m and a length of 300 \(\upmu \)m was positioned parallel to the z-axis under the top surface, and a hemispherical cutting cone was positioned. The displacement in the z-direction at the bottom surface was constrained, whereas the lateral surfaces were not. A uniform compression stress, \(\sigma _0=-0.2\) MPa, was then applied to the top surface.
Figure 12d shows the changes in morphology of the Haversian canal within the osteon by remodeling. As the initial surface cells, osteoclasts were originally located on the cutting cone, whereas lining cells were located elsewhere. As shown in Fig. 12d, bone was resorbed by osteoclasts at the tip of the cutting cone, after which osteoblasts formed bone. The osteon was observed to extend in the direction of principal stress.
Morphological changes by remodeling of a single trabecula and a single osteon under uniaxial compressive loading. a Initial trabecular morphology and boundary conditions. b Distribution of surface cells associated with changes in trabecular morphology and c temporal changes in the surface mechanical stimuli. d Initial morphology of an osteon and a Haversian canal. e Extension of the Haversian canal and changes in surface cell distribution as a result of osteonal remodeling
9 Conclusion
In silico experiments of bone remodeling have made it possible to observe morphological changes in bone microstructure as a result of remodeling as well as the spatiotemporal dynamics of osteoclasts and osteoblasts, which were difficult to experimentally observe in vivo. We expect that mathematical modeling and computer simulations of bone remodeling will function as a framework for allowing the discovery of numerous new findings in bone metabolism. Moreover, mathematical modeling and computer simulations of bone remodeling will play an important role in clarifying the behavior of this complex system. We also anticipate that these approaches will be used to elucidate the mechanisms of bone diseases, in which bone morphology and mechanics are closely related, and to predict changes in bone morphology associated with bone metabolic changes caused by therapeutic agents.
References
L.F. Bonewald, M.L. Johnson, Osteocytes, mechanosensing and wnt signaling. Bone 42(4), 606–615 (2008)
T. Nakashima, M. Hayashi, T. Fukunaga, K. Kurata, M. Oh-Hora, J.Q. Feng, L.F. Bonewald, T. Kodama, A. Wutz, E.F. Wagner, J.M. Penninger, H. Takayanagi, Evidence for osteocyte regulation of bone homeostasis through rankl expression. Nat. Med. 17(10), 1231–1234 (2011)
A. Mochizuki, M. Takami, Y. Miyamoto, T. Nakamaki, S. Tomoyasu, Y. Kadono, S. Tanaka, T. Inoue, R. Kamijo, Cell adhesion signaling regulates rank expression in osteoclast precursors. PLoS ONE 7(11), e48795 (2012)
C.A. O’Brien, T. Nakashima, H. Takayanagi, Osteocyte control of osteoclastogenesis. Bone 54(2), 258–263 (2012)
T. Adachi, Y. Kameo, M. Hojo, Trabecular bone remodelling simulation considering osteocytic response to fluid-induced shear stress. Philos. Trans. Royal Soc. a-Math. Phys. Eng. Sci. 368(1920), 2669–2682 (2010)
Y. Kameo, T. Adachi, M. Hojo, Effects of loading frequency on the functional adaptation of trabeculae predicted by bone remodeling simulation. J. Mech. Behav. Biomed. Mater. 4(6), 900–908 (2011)
F.A. Schulte, A. Zwahlen, F.M. Lambers, G. Kuhn, D. Ruffoni, D. Betts, D.J. Webster, R. Muller, Strain-adaptive in silico modeling of bone adaptation a computer simulation validated by in vivo micro-computed tomography data. Bone 52(1), 485–492 (2013)
T. Adachi, Y. Aonuma, K. Taira, M. Hojo, H. Kamioka, Asymmetric intercellular communication between bone cells: propagation of the calcium signaling. Biochem. Biophys. Res. Commun. 389(3), 495–500 (2009)
L.F. Bonewald, The amazing osteocyte. J. Bone Miner. Res. 26(2), 229–238 (2011)
P. Pivonka, J. Zimak, D.W. Smith, B.S. Gardiner, C.R. Dunstan, N.A. Sims, T.J. Martin, G.R. Mundy, Model structure and control of bone remodeling: a theoretical study. Bone 43(2), 249–263 (2008)
P. Pivonka, J. Zimak, D.W. Smith, B.S. Gardiner, C.R. Dunstan, N.A. Sims, T.J. Martin, G.R. Mundy, Theoretical investigation of the role of the rank-rankl-opg system in bone remodeling. J. Theor. Biol. 262(2), 306–316 (2010)
S. Weinbaum, S.C. Cowin, Y. Zeng, A model for the excitation of osteocytes by mechanical loading-induced bone fluid shear stresses. J. Biomech. 27(3), 339–360 (1994)
J. KleinNulend, C.M. Semeins, N.E. Ajubi, P.J. Nijweide, E.H. Burger, Pulsating fluid flow increases nitric oxide (no) synthesis by osteocytes but not periosteal fibroblasts - correlation with prostaglandin upregulation. Biochem. Biophys. Res. Commun. 217(2), 640–648 (1995)
T. Adachi, Y. Aonuma, M. Tanaka, M. Hojo, T. Takano-Yamamoto, H. Kamioka, Calcium response in single osteocytes to locally applied mechanical stimulus: differences in cell process and cell body. J. Biomech. 42(12), 1989–1995 (2009)
R.Y. Kwon, D.R. Meays, A.S. Meilan, J. Jones, R. Miramontes, N. Kardos, J.C. Yeh, J.A. Frangos, Skeletal adaptation to intramedullary pressure-induced interstitial fluid flow is enhanced in mice subjected to targeted osteocyte ablation. Plos One 7(3) (2012)
J. Klein-Nulend, A.D. Bakker, R.G. Bacabac, A. Vatsa, S. Weinbaum, Mechanosensation and transduction in osteocytes. Bone 54(2), 182–90 (2013)
Y.F. Han, S.C. Cowin, M.B. Schaffler, S. Weinbaum, Mechanotransduction and strain amplification in osteocyte cell processes. Proc. Natl. Acad. Sci. U.S.A. 101(47), 16689–16694 (2004)
X.L. Lu, B. Huo, M. Park, X.E. Guo, Calcium response in osteocytic networks under steady and oscillatory fluid flow. Bone 51(3), 466–473 (2012)
R.Y. Kwon, S. Temiyasathit, P. Tummala, C.C. Quah, C.R. Jacobs, Primary cilium-dependent mechanosensing is mediated by adenylyl cyclase 6 and cyclic amp in bone cells. FASEB J. 24(8), 2859–2868 (2010)
S. Temiyasathit, W.J. Tang, P. Leucht, C.T. Anderson, S.D. Monica, A.B. Castillo, J.A. Helms, T. Stearns, C.R. Jacobs, Mechanosensing by the primary cilium: deletion of kif3a reduces bone formation due to loading. Plos One 7(3), e33368 (2012)
H.M. Frost, Bone mass and the mechanostat - a proposal. Anat. Rec. 219(1), 1–9 (1987)
H.M. Frost, Defining osteopenias and osteoporoses: Another view (with insights from a new paradigm). Bone 20(5), 385–391 (1997)
R. Huiskes, R. Ruimerman, G.H. van Lenthe, J.D. Janssen, Effects of mechanical forces on maintenance and adaptation of form in trabecular bone. Nature 405(6787), 704–706 (2000)
H.M. Frost, Bone’ s mechanostat: a 2003 update. Anat. Rec. Part A 275A(2), 1081–1101 (2003)
T. Adachi, Y. Tomita, H. Sakaue, M. Tanaka, Simulation of trabecular surface remodeling based on local stress nonuniformity. Jsme Int. J. Ser. C-Mech. Syst. Mach. Elem. Manuf. 40(4), 782–792 (1997)
K. Tsubota, Y. Suzuki, T. Yamada, M. Hojo, A. Makinouchi, T. Adachi, Computer simulation of trablecular remodeling in human proximal femur using large-scale voxel fe models: Approach to understanding wolff’s law. J. Biomech. 42(8), 1088–1094 (2009)
H. Kamioka, Y. Kameo, Y. Imai, A.D. Bakker, R.G. Bacabac, N. Yamada, A. Takaoka, T. Yamashiro, T. Adachi, J. Klein-Nulend, Microscale fluid flow analysis in a human osteocyte canaliculus using a realistic high-resolution image-based three-dimensional model. Integr. Biol. 4(10), 1198–1206 (2012)
D. Sharma, C. Ciani, P.A.R. Marin, J.D. Levy, S.B. Doty, S.P. Fritton, Alterations in the osteocyte lacunar-canalicular microenvironment due to estrogen deficiency. Bone 51(3), 488–497 (2012)
Y. Kameo, T. Adachi, Modeling trabecular bone adaptation to local bending load regulated by mechanosensing osteocytes. Acta Mech. 225(10), 2833–2840 (2014)
Y. Kameo, T. Adachi, N. Sato, M. Hojo, Estimation of bone permeability considering the morphology of lacuno-canalicular porosity. J. Mech. Behav. Biomed. Mater. 3(3), 240–248 (2010)
S. Osher, J.A. Sethian, Fronts propagating with curvature-dependent speed - algorithms based on hamilton-jacobi formulations. J. Comput. Phys. 79(1), 12–49 (1988)
Y. Kameo, T. Adachi, Interstitial fluid flow in canaliculi as a mechanical stimulus for cancellous bone remodeling: in silico validation. Biomech. Model. Mechanobiol. 13(4), 851–860 (2014)
T. Beno, Y.J. Yoon, S.C. Cowin, S.P. Fritton, Estimation of bone permeability using accurate microstructural measurements. J. Biomech. 39(13), 2378–2387 (2006)
T.H. Smit, J.M. Huyghe, S.C. Cowin, Estimation of the poroelastic parameters of cortical bone. J. Biomech. 35(6), 829–835 (2002)
K. Tsubota, T. Adachi, Spatial and temporal regulation of cancellous bone structure: characterization of a rate equation of trabecular surface remodeling. Med. Eng. Phys. 27(4), 305–311 (2005)
L.D. You, S. Weinbaum, S.C. Cowin, M.B. Schaffler, Ultrastructure of the osteocyte process and its pericellular matrix. Anat. Rec. Part a-Discov. Mol. Cell. Evol. Biol. 278A(2), 505–513 (2004)
Z.F. Jaworski, E. Lok, Rate of osteoclastic bone erosion in haversian remodeling sites of adult dogs rib. Calcif. Tissue Res. 10(2), 103–112 (1972)
B. Huo, X.L. Lu, C.T. Hung, K.D. Costa, Q.B. Xu, G.M. Whitesides, X.E. Guo, Fluid flow induced calcium response in bone cell network. Cell. Mol. Bioeng. 1(1), 58–66 (2008)
S. Majumdar, M. Kothari, P. Augat, D.C. Newitt, T.M. Link, J.C. Lin, T. Lang, Y. Lu, H.K. Genant, High-resolution magnetic resonance imaging: Three-dimensional trabecular bone architecture and biomechanical properties. Bone 22(5), 445–454 (1998)
R. Muller, T. Hildebrand, P. Ruegsegger, Noninvasive bone-biopsy - a new method to analyze and display the 3-dimensional structure of trabecular bone. Phys. Med. Biol. 39(1), 145–164 (1994)
T. Adachi, K. Tsubota, Y. Tomita, S.J. Hollister, Trabecular surface remodeling simulation for cancellous bone using microstructural voxel finite element models. J. Biomech. Eng.-Trans. ASME 123(5), 403–409 (2001)
R. Ruimerman, P. Hilbers, B. van Rietbergen, R. Huiskes, A theoretical framework for strain-related trabecular bone maintenance and adaptation. J. Biomech. 38(4), 931–941 (2005)
K. Tsubota, T. Adachi, Y. Tomita, Functional adaptation of cancellous bone in human proximal femur predicted by trabecular surface remodeling simulation toward uniform stress state. J. Biomech. 35(12), 1541–1551 (2002)
I.G. Jang, I.Y. Kim, Computational study of wolff’s law with trabecular architecture in the human proximal femur using topology optimization. J. Biomech. 41(11), 2353–2361 (2008)
S.C. Cowin, Bone poroelasticity. J. Biomech. 32(3), 217–238 (1999)
Y. Kameo, T. Adachi, M. Hojo, Transient response of fluid pressure in a poroelastic material under uniaxial cyclic loading. J. Mech. Phys. Solids 56(5), 1794–1805 (2008)
Y. Kameo, T. Adachi, M. Hojo, Fluid pressure response in poroelastic materials subjected to cyclic loading. J. Mech. Phys. Solids 57(11), 1815–1827 (2009)
F.A. Gerhard, D.J. Webster, G.H. van Lenthe, R. Muller, In silico biology of bone modelling and remodelling: adaptation. Philos. Trans. R. Soc. a-Math. Phys. Eng. Sci. 367(1895), 2011–2030 (2009)
S.A. Goldstein, L.S. Matthews, J.L. Kuhn, S.J. Hollister, Trabecular bone remodeling - an experimental-model. J. Biomech. 24, 135–150 (1991)
R.E. Guldberg, N.J. Caldwell, X.E. Guo, R.W. Goulet, S.J. Hollister, S.A. Goldstein, Mechanical stimulation of tissue repair in the hydraulic bone chamber. J. Bone Miner. Res. 12(8), 1295–1302 (1997)
R.E. Guldberg, M. Richards, N.J. Caldwell, C.L. Kuelske, S.A. Goldstein, Trabecular bone adaptation to variations in porous-coated implant topology. J. Biomech. 30(2), 147–153 (1997)
L.M. McNamara, P.J. Prendergast, Bone remodelling algorithms incorporating both strain and microdamage stimuli. J. Biomech. 40(6), 1381–1391 (2007)
A.M. Parfitt, Osteonal and hemi-osteonal remodeling - the spatial and temporal framework for signal traffic in adult human bone. J. Cell. Biochem. 55(3), 273–286 (1994)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 CISM International Centre for Mechanical Sciences
About this chapter
Cite this chapter
Adachi, T., Kameo, Y. (2018). Computational Biomechanics of Bone Adaptation by Remodeling. In: Pivonka, P. (eds) Multiscale Mechanobiology of Bone Remodeling and Adaptation. CISM International Centre for Mechanical Sciences, vol 578. Springer, Cham. https://doi.org/10.1007/978-3-319-58845-2_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-58845-2_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58843-8
Online ISBN: 978-3-319-58845-2
eBook Packages: EngineeringEngineering (R0)