Abstract
Psychosocial stress has been consistently linked with alterations in immune, endocrine, and metabolic function, and growing evidence indicates that psychosocial stressors—including noise, poverty, and exposure to violence—may alter human susceptibility to environmental chemical exposures. As a result, there is a growing need for methods to disentangle patterns in chemical and non-chemical exposures and to quantify their independent and interacting effects on health.
Here, a framework is presented for integrating psychosocial stressors into a traditional risk assessment approach, with attention to exposure assessment for non-chemical stressors and to statistical methods for incorporation of very disparate exposures into a risk assessment. Finally, an illustrative case example is presented, to demonstrate an approach for incorporating a psychosocial stressor (here, exposure to violence, a key stressor in urban U.S. communities) into a cumulative risk assessment aiming to quantify air pollution effects on health.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction/Framework
1.1 Psychosocial Stressors in Mixtures Analysis and Cumulative Risk Assessment
The rapidly growing interest in characterizing the combined effects of chemical and non-chemical stressors on health outcomes and in cumulative risk assessment has stemmed from a few key observations. First, significant chemical and non-chemical stressors are often spatially or demographically correlated, clustered in lower-income communities near highways or industrial corridors (Bullard 1993). Second, there is growing epidemiological and toxicological evidence that chronic psychological stress (oftentimes driven by poverty, exposure to violence, and other community-scale non-chemical stressors) may alter individuals’ susceptibility to environmental pollution (Clougherty et al. 2007, 2010a, 2014; Clougherty and Kubzansky 2010; Virgolini et al. 2006). This heightened susceptibility may be mediated through a suite of immune, endocrine, and metabolic changes that occur under chronic stress, a condition collectively referred to as allostatic load (McEwen 1998). Together, these observations suggest that the most pollution-exposed communities also may be the most susceptible (Lipfert 2004). Thus, disentangling the effects of chemical and non-chemical exposures and identifying their potential for greater than additive effects are increasingly becoming research and policy priorities, recognized as critical toward identifying and protecting susceptible populations as well as reducing health disparities (U.S. EPA 2003). While numerous non-chemical stressors may either cause harm directly or increase vulnerability to harm by other stressors, the focus of this chapter is on the role of psychosocial stressors in cumulative risk assessments for physical or chemical environmental exposures.
A cumulative risk assessment may be motivated by observed disease patterns (effects-based risk assessment), interest in a specific set of exposures present in a given community (stressor-based risk assessment), or a defined subpopulation of concern within a community (receptor-based risk assessment). Although this third category is likely to overlap procedurally with either an effects-based or stressor-based assessment, given the nature of cumulative risk assessments, it would include a more explicit characterization of the community including elements such as demographics, geographic boundaries, and health. For any of these applications, psychosocial stressors may be hypothesized either to directly influence health outcomes or to modify health response to chemical/physical exposures. The issues at hand in accurately characterizing psychosocial stressors and their potential role in cumulative risk assessment apply equally to any assessment type, including such significant questions as:
-
How does cumulative risk assessment integrate insight from epidemiology, given that (1) toxicological evidence may not fully capture human psychosocial stressors, (2) epidemiological evidence is currently lacking for the vast majority of chemicals, and (3) the vast majority of chemicals also do not currently have toxicological data sufficient for traditional risk assessment processes? Relatedly, can either toxicology or epidemiology adequately inform the distribution of stressors or vulnerability in a population, given relatively homogeneous populations in toxicology, and challenges in determining effects across differing subpopulations in epidemiology?
-
How can exposures to psychosocial stressors be appropriately and jointly quantified and represented, given relatively little data beyond demographic information in most settings? Can defaults be established that are both meaningful and interpretable in a variety of settings?
-
Can a cumulative risk assessment meaningfully include both chemical and psychosocial stressors, if interventions typically target chemical stressors? Is the process different if a non-chemical stressor happens to be influenced by risk management activities (e.g., if cleaning up a pollution source in a community alleviates psychosocial stress)?
-
Which psychosocial stressors are potentially relevant for specific settings, chemical exposures, or outcomes?
The focus of this chapter is on the role of psychosocial stressors in human health cumulative risk assessment, with attention to a few key steps (i.e., exposure assessment, dose-response modeling). Available databases and metrics that could allow for characterization of exposure to psychosocial stressors are discussed, considering both ideal parameters and proxy measures and default assumptions that could be useful in the absence of detailed population-specific data. For dose-response modeling, strategies that could be used for epidemiological or toxicological evidence are considered, and similarities and differences from chemical mixtures are discussed. Finally, an illustrative case example is presented that emphasizes the viability of including psychosocial stressors using epidemiological evidence.
1.2 Background and Terminology
Psychosocial stressors (i.e., perceived stressors in our social environment) are hypothesized to lead to negative health outcomes directly, or through stress-related alterations in immune, neuroendocrine, or metabolic function, collectively referred to as ‘allostatic load' (McEwen 1998). Through these multiple stress-related pathways, chronic stress may serve to damage the individual’s health directly (Evans 2003) or may alter the individual’s susceptibility to exposures in the physical environment, such as air pollutants (Clougherty et al. 2014) or cold viruses (Cohen et al. 1991).
The psychosocial stressor pathways can be best understood in that psychological stress, regardless of the perceived stressor (social or otherwise), results when external demands exceed an individual’s perceived abilities and resources to meet those demands (Cohen et al. 1995). This may be best characterized as a three-phase process:
-
1.
Stressor (i.e., event, condition, or stimuli which pose a challenge)
-
2.
Appraisal (i.e., an individual’s perception or interpretation of the stressor)
-
3.
Response (e.g., psychological and physiological sequelae)
These phases are not independent, and all phases are required in order to exert a psychological or biological stress response; a stressor perceived as benign or beneficial generally produces no psychological stress response. Thus, exposure assessment for psychosocial stressors would ideally not simply catalog stressors (e.g., life events, community violence), but would rather emphasize total perceived stress (capturing response to multiple differently appraised stressors) or negative affect (e.g., anxiety, depression) as a cumulative indicator of mental distress and psychosocial stress (Kubzansky et al. 1999; Seeman et al. 2002). In cumulative risk assessment, it can be very challenging to quantify the appraisal and response phases, especially across large populations, though these factors influence the accuracy and interpretability of many psychosocial stressors. It is a topic of ongoing research to validate associations between community-level stressors (e.g., crime) and individual perceived stress and to identify factors which strengthen or weaken associations between stressor indicators and stress responses.
2 Exposure Assessment
Although much discussion on psychosocial stressors in cumulative risk assessment focuses on dose-response modeling, characterizing human exposures to psychosocial stressors is a critical step. It is extremely challenging to accurately characterize exposures to chemicals, especially in a community context where there is a need to account for multiple chemicals simultaneously. Psychosocial stressors can be even more challenging and cannot be quantitatively measured or modeled using only the same methods used for chemical exposures. In large part, this is because responses to psychosocial stressors vary with individual perception (i.e., “appraisal”), often influenced by history and context. Here, we briefly address four key dimensions of exposure assessment for psychosocial stressors:
-
1.
The need to characterize the mechanism(s) of action and hypothesized pathways of effect
-
2.
The need to carefully assess proxy variables for psychosocial stressors, considering the level of operation (i.e., community or individual level) and validating measures
-
3.
The need to consider correlations among psychosocial and chemical exposures, which influence the accurate development of statistical models for epidemiology and accurate interpretations of measures of association
-
4.
The need to establish default assumptions for psychosocial stressor exposures, in the absence of population-specific exposure data
2.1 Characterizing Mechanism(s) of Action/Pathways of Effect
Measuring psychosocial stressors is particularly challenging because many can act through multiple pathways. Some exposures can operate (simultaneously) as both a physical and psychological stressor. For example, noise can physically damage the inner ear but also can be a psychological stressor. The appropriate exposure assessment for the physical pathway would be direct measures of sound, while the appropriate exposure assessment for the psychosocial pathway would require measures of perceived annoyance. Although these measures may correlate, substantial exposure misclassification would occur where using physical measures alone for the psychosocial pathway. Likewise, heat may be a physical stressor, leading to heat exhaustion or hypertensive outcomes, and is also uncomfortable and therefore psychologically stressful over extended periods (one of many causes believed to contribute to greater urban violence during summer months and heat waves). Again, the optimal measure depends on the hypothesized pathway [i.e., apparent temperature (physical), or perceived discomfort (psychological)].
A related challenge is the possibility that some pollution sources may also be psychosocial stressors if, for example, residents perceive substantial risk from a local source or if the source’s presence suggests to residents that their health and well-being are not valued by the larger society (Bullard 1990). As such, it is often challenging to disentangle the physical and psychological aspects of pollution which impact communities near toxic sites (Elliott et al. 1993; Eyles et al. 1993)—and, again, the appropriate measure for each pathway would differ. It has been argued that having exposure assessment be homologous with dose-response modeling is a critical feature of risk assessment (National Research Council 2009, 2011), which is especially true for psychosocial stressors. Thus, we recommend that any exposure assessment begin with a clear conceptual model for hypothesized direct and indirect pathways to health effects, which, in turn, would drive the selection of exposure measures.
Because individual stress responses vary over time, and because individuals respond differently to most community-level stressors, there is increasing interest in developing biomarkers of stress. In theory, a well-characterized biomarker could facilitate epidemiological analysis and provide a comprehensive indicator of the response of an individual to multiple stressors. Stress is, however, by definition, a non-specific condition impacting a wide range of bodily systems (Selye 1936), many of which (e.g., inflammation) are also impacted by chemical and physical exposures, and the effects of which may vary with co-exposures, comorbidities, or other facets of individual physiologic susceptibility. Further, the timing of stressor exposure can greatly influence response (e.g., acute vs. chronic stress have very different physiologic sequelae). Taken together, it is unlikely that a single biomarker—or even a resolved suite of biomarkers—will reliably and meaningfully capture all stress responses, for all periods of interest.
Nevertheless, substantial research has examined the physiology of stress and the search for “biomarkers” of both acute and chronic stress. To date, most “biomarkers” identified have been immune or neuroendocrine markers associated with physiological stress responses—e.g., cytokines and glucocorticoids (Miller et al. 2002)—and an important emphasis has been on distinguishing biomarkers of acute stress (e.g., cortisol as an indicator of hypothalamic-pituitary-adrenal (HPA)-axis activity) from those of chronic stress (e.g., endocrine disruption or NF-κB signaling as an indicator of HPA-axis regulation) (Miller et al. 2007).
Formerly, corticosteroids (e.g., cortisol) in blood or saliva were emphasized as markers of HPA-axis activity, although stress-related HPA function changes lead to cortisol dysregulation (via glucocorticoid resistance and HPA regulation), not simply increased cortisol production. As such, cortisol can be difficult to interpret and generally better indicates acute, rather than chronic, stress. Importantly, it remains unknown how acute stress response may differ under chronic stress scenarios, and thus some more recent research emphasizes indicators of glucocorticoid resistance and neuroendocrine signaling (Miller et al. 2007). Other evidence suggests that C-reactive protein (CRP) may reasonably capture chronic stress; however, CRP is a non-specific immune marker also elevated in response to air pollution and other exposures (Clougherty et al. 2010a). Although no single biomarker is appropriate for all applications (Brunner 2007), suites of physiologic parameters have been developed to represent chronic “allostatic load” in humans and include indicators of cardiovascular function, metabolism, cholesterol, glucose metabolism, HPA-axis function, and sympathetic nervous system activity (Kubzansky et al. 1999; Seeman et al. 2002). Several studies document chronic stress effects on cardiovascular risk indicators (abdominal obesity, elevated serum triglycerides, lower levels of high-density lipoprotein (HDL) cholesterol, glucose intolerance, elevated blood pressure) (Brunner 2007), known collectively as “metabolic syndrome,” and this may provide a method for capturing cumulative stress effects on cardiovascular and systemic function.
It is important to recognize that biomarkers representing physiological responses to stress may provide insights that are more relevant to dose-response modeling, or to determining the mechanism of action, than to exposure measurement per se. There may be utility in characterizing some biomarkers for effects-based cumulative risk assessments, as multiple chemical and psychosocial stressors may influence cardiovascular function or other endpoints. Currently, however, these biomarkers do not necessarily inform exposure characterization. Following the stressor-appraisal-response model, commonly available exposure databases (e.g., census demographic data or community crime rates) may represent stressors, and biomarkers may capture aspects of stress response, but it is arguably individual appraisals that are most specific and germane to accurate assessment of psychosocial stress.
2.2 Use and Validation of Proxy Variables for Psychosocial Stressors
Many psychosocial stressors are difficult to measure or model directly, especially across all individuals in a large population. Thus, there is often value in identifying or constructing proxy variables to capture geographic patterns in stressor prevalence (e.g., community crime rates, school quality indicators), due to limited individual-level data. In many contexts, however, even characterization of relevant community-level stressors may not be viable, and risk assessors may wish to use relatively simple aggregate-level data on socioeconomic positon (SEP) or similar proxy measures. In such cases, validation of associations between stressor indicators and a representative sample of individual stressor perceptions would be encouraged.
In this case, analysts should also carefully describe the hypothesized pathways, differentiating to the degree possible between compositional vs. contextual variables. Compositional variables refer to measures that reveal information about the distribution of individuals within a community, whereas contextual variables reveal information about the setting in which individuals live. For example, community-level poverty measures could serve as a proxy for the likelihood of individual poverty (a compositional variable) or as an indicator of processes which function solely at the aggregate (or community) level (e.g., collective efficacy, social capital, disinvestment in a community). These latter community-level features which impact multiple individuals are contextual variables. For example, the percent of households under the poverty line could be a compositional variable reflecting individual-level likelihood of poverty or a contextual variable reflecting negative neighborhood attributes.
The impact of SEP on health has been extensively explored in many settings: using wealth or income as an index of status within and across countries (Subramanian and Kawachi 2004), in communities using measurements of perceived social standing (Singh-Manoux et al. 2005), and in workplace settings using job grade (Clougherty et al. 2010b; Marmot et al. 1991). Given numerous measures of SEP, and potential confusion about what these proxy variables capture for cumulative risk assessment, key definitions and concepts are described briefly here. SEP refers to the individual or family’s relative position in a society, particularly where economic and cultural factors determine resource access, or in hierarchical societies where psychosocial goods such as social influence or security are largely determined by social stature. SEP influences human health through a highly complex mix of many social and physical factors accumulating and interacting over the life course, including diet and health behaviors, healthcare access, and working and housing conditions. Increasingly, psychosocial stress appears to be one extremely important aspect of SEP influencing health, though SEP should not be assumed to be synonymous with psychosocial stress.
Wherever possible, validation studies should be performed to ensure that an aggregate-level indicator (especially when used as a compositional variable, to proxy for individual-level data) accurately captures intra-community contrast in the construct (and pathway) of interest. For example, community crime statistics used to proxy for crime-related stress could be validated using intra-community surveys on perceived crime exposures and chronic stress, then comparing crime indicators to the individual-level measures. While such validation studies may not always be practical, looking to existing validation and multilevel studies on stressor exposures and characterization may aid in accurately interpreting potential proxy variables, at both the individual and aggregate levels.
2.3 Incorporating Exposure Correlations
Exposure characterization in cumulative risk assessment should explicitly consider possible correlations among stressor exposures, both positive and negative, as these may impact exposure measurement error or apparent interaction effects. For example, if proximity to major roadways is associated with increased exposures to both traffic-related air pollutants and noise, then the exposure assessments should aim to differentiate these spatially and temporally confounded exposures to the extent possible.
Correlations could exist at the aggregate level (i.e., among contextual variables) or only as a function of individual behaviors or activities (individual-level compositional variables). For psychosocial stressors associated with multiple individual or contextual factors, especially for a community-scale cumulative risk assessment, simulation approaches to characterize multivariable demographic attributes with high geographic resolution may be warranted (Levy et al. 2014). Inclusion of geographic and demographic predictors of physical or chemical exposures, time activity patterns, and other exposure-relevant behaviors would facilitate modeling of psychosocial exposures.
It is recommended that each conceptual model be as clear and simple as can reasonably capture the key exposure(s) and pathway(s) of interest—even within a cumulative risk assessment which may ultimately include many interacting exposures or a complex disease outcome. Overloading the conceptual model may obscure the specific hypothesized pathways, and lead to overly complicated (and less meaningful) “kitchen-sink” analyses.
2.4 Establishing Default Assumptions
For psychosocial stressors, often difficult to characterize directly in a cumulative risk assessment, default distributions can be derived from administrative data (e.g., census variables, large-scale population surveys, surveillance data, or the peer-reviewed literature, depending on the stressor of interest). Understanding the readily available factors that correlate with psychosocial stress, and thereby could serve as proxies or predictors of individual stress or stressor exposures, would be crucial in conducting assessments that are both meaningful and comparable across applications. Risk assessors would greatly benefit from an exposure factors handbook or analogous database that extended to non-chemical stressors, as has been recommended by expert committees on risk assessment (National Research Council 2009).
3 Dose-Response Modeling
Dose-response modeling for cumulative risk assessment presents significant methodological challenges, including but not limited to the complexities of incorporating non-chemical stressors. For psychosocial stressors, insight may be derived from epidemiological or toxicological evidence (or a combination), but the evidence must be systematically evaluated to ensure meaningful outputs.
In general, psychosocial stressors can be evaluated comparably to chemical stressors, provided that the requisite exposure data and health evidence are available. For example, the concept of “sufficient similarity” is being explored for complex mixtures of chemicals, wherein major chemical components are found in similar proportions and similarities in health effects and dose-response relationships are also considered (see Chap. 15). For psychosocial stressors, similarities in the type and magnitude of health effects may fulfill “sufficient similarity” and suggest groupings of psychosocial stressors (or psychosocial and physical/chemical stressors) that could be beneficial to the cumulative risk assessment process. Similar to chemical groupings, psychosocial stressors may be reviewed for their co-occurrence, joint action, and mode of action. Psychosocial stressors may also contribute to dose-response modeling through an improved understanding of background exposures influencing the shape of the dose-response function for other stressors. In general, existing guidelines on chemical mixtures can be modified to include psychosocial and other non-chemical stressors, potentially through a focus on common adverse outcomes, rather than on common mode of action.
3.1 Centrality of Epidemiological Evidence for Psychosocial Factors/Developing Dose-Response Functions Using Epidemiology
In many cases, epidemiological evidence will be the only viable strategy for incorporating psychosocial stressors into cumulative risk assessment. If the exposure assessment relied on proxy variables for SEP or demographic attributes, these proxies do not translate readily into a toxicological context. More generally, there may not be animal models to represent the types of psychosocial stressors of interest. This raises considerable challenges given that relatively few epidemiological studies are able to fully characterize effects of multiple chemical and psychosocial stressors. If adequate epidemiology is available for all stressors of interest, developing dose-response functions for cumulative risk assessment may be relatively straightforward, though several key diagnostic questions still need to be answered before dose-response functions can be fully characterized.
First, the ideal evidence would involve studies examining all risk factors simultaneously and reported dose-response functions derived from multivariable models, controlling for co-exposures and testing for effect modification. Many epidemiological studies, however, are underpowered for such investigations or do not use statistical methods needed to discern the effects of stressors with common sociodemographic predictors or operating at multiple levels. Structural equation models have increasingly been used to evaluate the joint influence of multiple risk factors in epidemiological studies, allowing for direct and indirect effects to be simultaneously estimated (Peters et al. 2014). These and other statistical techniques for multi-exposure epidemiology require large sample sizes and are limited in the types of data they can adequately incorporate but can offer considerable insight on both proximal and distal causes.
In many situations, however, not all stressors of interest will have been included in a single epidemiological study. Extracting dose-response functions for different stressors from different studies, generally from regression models that do not include all relevant stressors, is a viable approach only where confounding is shown to be limited. While most epidemiological studies likely omit some candidate confounders, insight on the likelihood of significant correlations between exposures can be included based on external evidence and first principles. For example, two predominantly indoor pollutants, highly correlated with air exchange rates, would likely be positively correlated, whereas an ambient air pollutant and a foodborne exposure may be less correlated. Combining insights from different studies also requires judgments on the distribution of vulnerable individuals in the population and presence of potential modifiers.
Another complexity arises from epidemiological studies using socioeconomic and demographic covariates as proxies for non-chemical or lifestyle factors (including but not limited to psychosocial stress). For example, SEP may be included in a regression model linking lead with IQ decrements, with the idea that SEP could proxy for psychosocial stress, nutritional factors, presence of a stimulating home environment, or a number of other risk factors associated with neurodevelopment. Using the findings for SEP, either as a main effect or effect modifier, would require a careful judgment about what the term captures in the study population, and whether the same association is present in the population of interest for the cumulative risk assessment. Development of a detailed conceptual model that includes both proximal and distal effects on health, as described earlier, will facilitate this process.
3.2 Developing Dose-Response Functions Using Toxicology
Despite the centrality of epidemiological evidence for psychosocial stressors, often only toxicological information is available for many chemical stressors. For non-cancer risk assessments, where the question of cumulative exposures is rather less well-studied than for cancer risk assessments, psychosocial stressors can be considered in three different places. First, if there is direct toxicological evidence on the psychosocial stressor illustrating a similar mode of action as a chemical stressor, it can be treated similarly to a chemical mixture. For example, in rat models of lead and chronic stress (Cory-Slechta et al. 2004, 2010), or concentrated air pollution and chronic stress (Clougherty et al. 2010a), the psychosocial stressor is considered in the same bioassay with well-characterized chemical or physical exposures. As proposed in the NRC report on cumulative risk assessment for phthalates (National Research Council 2008), dose addition can be applied in contexts other than congruent dose-response functions, allowing for a broader application. The NRC report also proposes approaches to establish benchmark dose (BMDL) values for chemical mixtures under an assumption of dose addition, which can be directly applied to psychosocial stressors as well if the analogous toxicological data are available and if the dose metrics are relevant to human populations. This is a viable approach in limited contexts where exposures to psychosocial stressors can be readily characterized in toxicological studies.
Second, psychosocial stressors can also contribute toward a general understanding of the appropriate conceptual model for chemical stressors evaluated toxicologically. In Science and Decisions (National Research Council 2009), the committee proposed that the functional form of a dose-response model could only be determined once a series of diagnostic questions were asked, related to the mode of action, relevant background exposures and endogenous processes, and vulnerable populations. Depending on the responses, the population dose-response function would reflect one of three conceptual models: (1) low-dose linear responses for individuals, with low-dose linear responses for the population; (2) non-linear responses for individuals with low-dose linear population responses with background dependence, and (3) non-linear responses for individuals with low-dose non-linear population responses independent from background. Historically, non-cancer responses have been considered to be of the third category (nonlinear for individuals with nonlinear population responses at low doses), although significant background exposures or other processes could be sufficient to linearize an otherwise nonlinear population dose-response function.
Practically speaking, this means that improved mechanistic knowledge for some psychosocial stressors could inform the shape of the dose-response function for those chemical stressors with adequate toxicological evidence. For example, increased risk of hypertension or elevated systolic/diastolic blood pressure has been associated with psychosocial stress, diet, and other non-chemical stressors, though perhaps not in toxicological data, in a manner necessary to follow the second approach above. The non-chemical stressors are associated with the outcome of interest and prevalent in the general population. This would imply that the toxicological evidence associating a chemical stressor with hypertension would be assumed to follow the second conceptual model above, with the point of departure (POD) used to develop a slope term and an estimated risk-specific dose. This approach is conceptually viable but has two significant challenges. First, as mentioned previously, it may be unclear whether the background processes are sufficient in magnitude to conclude that a low-dose linear model would be appropriate. Experience with some case studies would help to formalize this step. Second, one would not be able to quantify risks attributable to non-chemical stressors incorporated in this manner. While this would be problematic in contexts where these non-chemical stressors were the targets of risk management efforts, they would only be included in this manner if there were no adequate toxicology or epidemiology, in which case they would be omitted from traditional quantitative analysis regardless of the approach.
Third, psychosocial stressors could be captured within physiologically based pharmacokinetic (PBPK) or pharmacodynamic models that provide insight about how these stressors would influence delivered dose or pharmacodynamic outcomes that could be the endpoints of cumulative risk assessments. For example, evidence has shown that chronic psychosocial stress can influence metabolism and cause hormonal changes (Agarwal and Marshall 1998), which could be incorporated into PBPK models. So, even lacking direct toxicological evidence on the influence of psychosocial stressors, these stressors could be incorporated into cumulative risk assessments via an adjustment of either the delivered doses from the toxicological study or the interpretation of the pharmacodynamic outcome.
3.3 Combining Insights from Epidemiology and Toxicology
In some cases, there will be epidemiological evidence for a small number of stressors, toxicological evidence for other stressors, and perhaps a subset of stressors with both toxicological and epidemiological evidence. Developing a systematic approach to incorporate psychosocial stressors in this context will therefore be key to cumulative risk assessment.
Depending on the nature of the available evidence, a hybrid of the two approaches above would be warranted. In a situation where the preponderance of the evidence is toxicological and the epidemiology is not directly applicable, the more limited epidemiological information could help establish whether the toxicants should be considered as linear or non-linear at low doses. In situations where multiple compounds are well-characterized toxicologically and at least one is well-characterized epidemiologically, approaches can be used to establish dose equivalence within toxicological studies to allow for interpretation of the epidemiological evidence. For example (Benignus et al. 2005), toxicological studies have linked both toluene and alcohol with similar neurobehavioral effects. Epidemiological evidence is robust for alcohol but not available for toluene. The toxicological studies can be used to estimate the dose of toluene that is functionally equivalent to a dose of alcohol for a defined outcome, and this could be used as a bridge to interpret the alcohol epidemiology with respect to toluene exposure. This clearly involves a number of assumptions regarding comparable dose-response function shapes, but the approach can be generalized in a variety of ways.
Developing comparable dose-response models across epidemiological and toxicological studies, in a manner that would allow for the models to be quantitatively combined, would only be possible in a limited number of situations. The adverse outcomes would need to be comparable to one another, which may be possible for some physiological measures but would be challenging for outcomes such as asthma attacks, hospitalizations, and other common epidemiological endpoints. There would also need to be detailed understanding of the vulnerability characteristics of both the human and animal populations, to ensure that adequate adjustments were made to account for the presumed greater heterogeneity in the human population. It is likely that these criteria would be met very infrequently, so that more often, cumulative risk assessment would be primarily based on either epidemiological or toxicological evidence, using the other to help inform the conceptual model or determination of mode of action.
4 Illustrative Case Example
To illustrate some of these approaches for incorporating psychosocial stressors, a case study example is presented, drawing on the epidemiological literature suggesting significant effect modification of associations between urban air pollutants and childhood asthma by chronic stressors prevalent in urban environments, notably exposure to violence (ETV). A process by which cumulative risk assessment could include this psychosocial stressor in the presence of chemical/ physical stressors is described, intending that the structure could extend to other stressors in a specific risk management context.
Asthma is a multifactorial illness impacted by a host of social, environmental, and genetic risk factors. As such, it serves as an appropriate case study for considering the interplay among two (or many more) risk factors—acting separately or in tandem—toward shaping patterns of asthma etiology and exacerbation in the urban environment.
This example may be conceptualized as within either a stressor-based or effects-based cumulative risk assessment (Menzie et al. 2007). For example, an analysis might consider the health benefits of multiple stressors reduced through traffic mitigation efforts and would need to take into account the modifying influence of key psychosocial stressors. Similarly, an analysis might be focused on geographic areas with elevated asthma prevalence or rates of exacerbation, determining key contributors to these patterns, in which case ETV and air pollution may be important to consider.
Air pollution and chronic stressors have been explored together in several epidemiological studies (e.g., Shankardass et al. 2009; Chen et al. 2008), and common distributions have been explored due to concerns about spatial correlations and potential confounding (e.g., traffic-related air pollution is spatially confounded by traffic-related noise) (Allen et al. 2009). ETV is explored here due, in part, to a small but growing literature on the salience of urban violence as a key chronic stressor which may modify pollution effects on health. A study of asthmatic children in Boston public housing reported altered response to indoor allergen exposures with caregiver-reported fear of violence (Clougherty et al. 2006). A longitudinal study of childhood asthma etiology in East Boston reported significant associations with nitrogen dioxide (NO2) exposures, but only among children with above-median prior lifetime exposure to violence (Clougherty et al. 2007). This model also informed one toxicological study exploring the effect of an aggressor stress (Social Dominance Paradigm), as a modifier of concentrated particulate air pollution (CAPs) effects on respiratory function in rats (Clougherty et al. 2010a); the authors reported substantively different responses to CAPs by stress group, with only stressed animals breathing more frequently and shallowly (e.g., hyperventilation) in response to increased CAPs exposures.
A few studies have explored other chronic stressors as modifiers of air pollution effects on asthma outcomes, though issues related to exposure measurement and the relative temporality between stress and pollution exposures have proven challenging. Aside from this small epidemiological literature suggesting a strong effect, there are several reasons why ETV is an appropriate stressor to examine in a cumulative risk assessment context:
-
1.
Most importantly, violence is one of the few stressors that is rarely positively appraised. As described in the Exposure Assessment section above, under Characterizing mechanism(s) of action/ pathways of effect, perceived or psychosocial stress is strongly mediated through individual perception (appraisal). Unlike ETV, most other stressors may be appraised either positively or negatively (e.g., one may view losing a job as a good or bad thing, depending on whether one enjoyed the job or needed the financial benefit). A positive appraisal can render the stressor null; as such, most other stressors lend themselves to exposure misclassification. Exposure to violence, however, is almost never characterized as a positive exposure.
-
2.
Outside of the rare instances of physical altercation, most of the impact of “exposure to violence” is through fear, hypervigilance, or stress-related pathways. (And, indeed, the experience of “fear of violence” can vary by gender, age, race, class, and other personal or community-level factors.) But, because most ETV impact occurs via psychosocial pathways, unlike other urban community stressors (e.g., housing quality), the hypothesized psychosocial pathway is relatively unconfounded by co-occurring physical impacts.
-
3.
Analyses of spatial patterning in urban exposures suggest that ETV is not always spatially confounded by poverty and other stressors (Shmool et al. 2014). Thus, the health impacts of ETV conceivably can be disentangled from those of SEP, which is a much more complicated construct entailing a broad array of physical (e.g., diet) and psychosocial (e.g., discriminatory experience) exposures, at both the individual and community level, accumulating over the life course.
-
4.
Crime data, albeit an imperfect community-level ETV indicator, is collected systematically by every police department nationwide, often according to standard criteria (i.e., felony crimes). Reporting bias remains a challenge—and certainly differs by jurisdiction and type of crime—but the data are collected and publicly available nationwide.
While the details listed above are specific to ETV, the logic used to validate its inclusion is generalizable. Any psychosocial stressor under consideration would require a logical exposure metric that can be reasonably and systematically collected, evidence for a causal effect on a defined health outcome, and a systematic determination that the exposure metric is reasonably sensitive and specific for the health outcome in question.
To incorporate interaction effects in a cumulative risk assessment, we first recommend careful development of a conceptual model for the hypothesized relationships among the exposures of interest, with attention to modes of action (MOA) or common adverse outcomes. Here, our relatively simple conceptual model captures some of the key constructs of interest:
-
1.
A psychosocial stressor (e.g., ETV) and air pollution exposures may separately influence childhood asthma etiology or exacerbation.
-
2.
Perceived ETV (as a chronic stressor) may, through “allostatic load” pathways, alter individual susceptibility to air pollution exposures in the progression of asthma.
Notably, many more conceptual models are possible, considering the myriad of exposures that impact upon childhood asthma. Here, we restrict our analysis to the one key exposure (air pollution) and one key hypothesized psychosocial effect modifier (ETV). A typical conceptual model likely would be more complex, with explicit consideration of multiple causal pathways and both proximal and distal risk factors for health.
Here, a community-level indicator (e.g., crime rates) serves to proxy (albeit imperfectly) for individual-level perceived ETV. For analyses in which both community-level and individual-level data are available, it would be preferable to use the individual data as the primary exposure metric and to explore the community-level indicator as a predictor of the individual-level variable or as a contextual variable interacting (in a hierarchical model) with the individual-level variable. It is recommended that each conceptual model be as clear and simple as can reasonably capture the key exposure(s) and pathway(s) of primary interest.
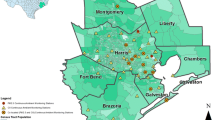
It may be determined that solely of interest are community-level stressors, which may act primarily through psychosocial pathways and are captured reasonably through aggregate data. If so, the construct of interest (e.g., ETV) is first defined, then existing data are catalogued that may reasonably indicate the construct (e.g., felony crimes, murders, robberies, at police precinct level). For community-scale metrics and environmental exposures (e.g., air pollution), it can be valuable to apply spatial methods in Geographic Information Systems (GIS) to evaluate relative spatial distributions within and among exposures. Here, it would be valuable to understand:
-
1.
Spatial (neighborhood-to-neighborhood) variability in crime rates—this extent of spatial “clustering” (or spatial autocorrelation) within a stressor can be formally tested using GIS-based methods such as geographically weighted regression (GWR) or local indicators of spatial association (LISA). This analysis indicates how each exposure, separately, varies across the region of interest. In an ongoing investigation of social stressor patterning across New York City, significant spatial variation was found within all stressors examined, across multiple domains (e.g., economic stressors, crime and violence exposures, resource access, school-based stressors, etc.) (Shmool et al. 2014).
-
2.
Spatial correlations between and among psychosocial stressors and pollutant exposures (e.g., correlation between ETV and air pollution) may be examined by comparing spatial distributions, and quantified using spatial autoregressive modeling (SAR). This analysis indicates the potential for confounding and/or effect modification between exposures. In New York City, social stressors were found to vary substantially in their spatial patterning, and not all stressors were correlated with poverty or pollution exposures (Shmool et al. 2014).
Developing the conceptual framework would normally involve initial screening-level quantification of health risks to determine whether the stressors are significant enough to merit inclusion. In this case, the relative risks of air pollution and ETV, from the epidemiological literature, are high enough, and the exposures sufficiently ubiquitous, to substantiate their inclusion. While the focus here is on epidemiological evidence, toxicological insights enhance the plausibility of the observed interaction (Virgolini et al. 2005, 2006; Cory-Slectha et al. 2004, 2010).
It is generally preferable to determine relative risks that consider both stressors simultaneously (whether as main effects or effect modifiers). Conceptually, the underlying epidemiological models would primarily be of two broad structures:
-
1.
Direct effect of psychosocial stressor on the outcome:
-
2.
Direct effect of a physical/chemical exposure on the outcome:
In each case, the confounders could include the other exposure, though effect modification likely would not be considered at this stage. Importantly, the best available metrics of each exposure may differ significantly in sensitivity and specificity (if, for example, the best available metric of ETV is a community-level index, and the best available metric of air pollution is a modeled residence-specific estimate). Thus, differential exposure misclassification needs be considered, both when comparing separate models that examine two different exposures on a common health endpoint, and when merging both exposure metrics into the same epidemiological model.
At this stage, the underlying epidemiological study often would use GIS methods to visualize and assess spatial relationships among exposures (stressors) of interest. These associations can be examined by comparing spatial maps of each stressor with that of the outcome variable (e.g., asthma hospitalizations) and quantified using SAR, to quantify these separate (unadjusted) associations. This step assumes that each stressor/exposure of interest carried forward should have a significant independent association with the outcome of interest, regardless of co-exposures or effect modifiers. In some cases, however, this may not be true; in one longitudinal study of childhood asthma etiology (Clougherty et al. 2007), significant associations between traffic-related NO2 and asthma etiology were observed solely among children with above-median ETV. In cases of strong effect modification, the effect of the physical exposure of interest (air pollution) may be diluted to non-significance, if the sample has a high enough prevalence of low-susceptibility individuals. This concern may be alleviated through sensitivity testing wherein potential modifiers and exposures are considered iteratively prior to final exclusion. The heuristic epidemiologic model for such analyses would be:
Statistical tools, such as multiple and logistic regression and process models, can be used to explore the contributions of various stressors to the health endpoint of interest.
At this stage, GIS-based spatial approaches can be used to visualize and examine the overlay of stressors with the observed health effects. As above, maps of each exposure and outcome can be compared and formally tested using SAR or similar models, to assess the extent of spatial autocorrelation. A refinement that may be useful at this stage is examining the combined (joint) spatial distributions in ETV and air pollution (or the spatial distribution in a composite index that combines these exposures) against the spatial distribution in the health outcome of interest (e.g., maps of asthma hospitalizations). Unaccounted-for nonlinear or other complex joint distributions (such as that observed in Shmool et al. 2015) can lead to mis-specification or misinterpretation of epidemiological results, particularly when incorporating multiple exposures or interactions into the model.
Finally, an epidemiologic model would explore the possibility of interactions. Knowledge reflected in conceptual models should provide a grounding (and some limits on) the interactions considered. Clear mechanistic hypotheses indicating which stressor is hypothesized to modify each exposure are needed for useful, interpretable epidemiological analyses and related cumulative risk assessment output. Conceivably, this could lead to some stressors being considered only as effect modifiers, because no plausible mechanism exists for a main effect absent another stressor of interest. The incorporation of too many interactions, or interactions not supported by a plausible mechanistic pathway, however, can complicate the analysis, reduce statistical power, and lead to uninterpretable results (especially as the number of stressors under consideration increases). Of note, the interaction between the chemical and psychosocial stressor may not be a simple linear association, and statistical techniques that allow for multidimensional smoothed functions of health response associated with multiple stressors may be informative. The heuristic epidemiological model that would support this interaction analysis is:
Epidemiological models being developed for cumulative risk assessment applications could also be designed to be responsive to the ultimate risk management decisions. For example, if the risk management strategies in question focused on air pollution exposures, it may be most salient to explicitly consider the influence of ETV as an effect modifier. Understanding the main effect of ETV would be less relevant, although it does contribute to an understanding of background rates of disease and characteristics of high-risk subpopulations. Although this is not an appreciable reduction in effort for a two-stressor analysis, an analysis of numerous stressors would benefit greatly from the analytical boundaries created through an appropriately focused set of risk management options.
Uncertainty analysis is emphasized as a key component of any cumulative risk assessment. For the epidemiology that may underlie a cumulative risk assessment, this goes beyond reported confidence intervals to include sensitivity analyses for the parameters included in the final models. It is strongly recommended that any cumulative risk assessment extract information on the sensitivity of epidemiological findings to some key assumptions. Similarly, researchers conducting epidemiological studies aiming to inform cumulative risk assessment should explicitly report uncertainties.
Because some important modifiers and predictors may be lost by omitting variables prior to testing interactions (i.e., researchers and risk assessors may miss effects that only become apparent through effect modification), some sensitivity testing on covariate selection is needed. This can be done by:
-
Swapping order of terms/interactions tested in models
-
Identifying key hypothesized predictors and modifiers carried throughout the analysis, regardless of significance
-
Using automated variable selection procedures using both predictors and modifiers (e.g., regression trees)
-
Using automated variable selection procedures that do not assume linearity or specific interaction structures (e.g., random forest), to identify underutilized stressor(s) for which data are available, but the relationships of such exposures with the outcome of interest have not been recognized fully in the main model
Finally, there remains significant utility in establishing that available exposure metrics accurately capture variability in the stressor(s) of interest. An effective way to do so, for aggregate-level indices (e.g., community violence rates), is to implement surveys (questionnaires) on individual’s perceived stress (1) to systematically determine whether community-level indices accurately capture community-to-community variation in mean individual-level violence exposures and (2) to select those aggregate-level metrics that best reflect individual variation in stressor exposures.
In summary, this case example illustrates that a psychosocial stressor such as exposure to violence can be incorporated reasonably into cumulative risk assessments including air pollution, as there is a biologically plausible linkage with a common adverse outcome (supported by some findings from both toxicology and epidemiology), an approach for exposure characterization that involves reasonable proxies from public databases, and empirical evidence supporting main effects and effect modification for both key stressors. Other non-chemical stressors can be evaluated and included through analogous approaches.
5 Conclusions
Data on psychosocial stressors indicate important effects on health that can interact with chemical environmental exposures. For psychosocial stressors, challenges arise with exposure assessment, dose-response modeling, and risk characterization in the context of risk management. In general, the exposure assessment phase of cumulative risk assessment requires increased attention, given both the need to characterize effects of simultaneous exposure to multiple chemical stressors and the need to develop meaningful proxies of exposure to psychosocial and other non-chemical stressors that are challenging to characterize directly. Development of a strong conceptual model including proximal and distal effects on health will help in determining the appropriate constructs for the analysis. This step is key, as many psychosocial stressors can influence health through multiple pathways, and many proxies for psychosocial stressor exposures can represent multiple stressors. Dose-response modeling using epidemiological data can benefit from systematic modeling approaches tied to well-developed conceptual models and using techniques such as structural equation modeling to identify associations with proximal and distal factors. Toxicological evidence may be more limited for psychosocial stressors, but even where evidence is insufficient to incorporate a psychosocial stressor into a mixtures analysis, consideration of psychosocial stressors can contribute toward selecting a conceptual dose-response model and may be incorporated into PBPK models or other analyses related to delivered doses or pharmacodynamic outcomes. The case example illustrates that it is viable to incorporate selected psychosocial stressors into cumulative risk assessment, following a systematic logic for well-structured exposure characterization and epidemiological modeling.
References
Agarwal, S.K., and G.D. Marshall. 1998. Glucocorticoid-induced type 1/type 2 cytokine alterations in humans: A model for stress-related immune dysfunction. Journal of Interferon & Cytokine Research 18: 1059–1068.
Allen, R.W., H. Davies, M.A. Cohen, G. Mallach, J.D. Kaufman, and S.D. Adar. 2009. The spatial relationship between traffic-generated air pollution and noise in 2 U.S. cities. Environmental Research 109: 334–342.
Benignus, V.A., P.J. Bushnell, and W.K. Boyes. 2005. Toward cost-benefit analysis of acute behavioral effects of toluene in humans. Risk Analysis 25 (2): 447–456.
Brunner, E. 2007. Biology and health inequality. PLoS Biology 5 (11): e267.
Bullard, R.D. 1993. Confronting Environmental Racism: Voices from the Grassroots. Cambridge, MA: South End Press.
———. 1990. Dumping in Dixie: Race, Class and Environmental Quality. Boulder: Westview Press.
Chen, E., H.M. Scheier, R.C. Strunk, and M. Brauer. 2008. Chronic traffic-related air pollution and stress interact to predict biologic and clinical outcomes in asthma. Environmental Health Perspectives 116 (7): 970–975.
Clougherty, J.E., J.I. Levy, H.P. Hynes, and J.D. Spengler. 2006. A longitudinal analysis of the efficacy of environmental interventions on asthma-related quality of life and symptoms among children in urban public housing. The Journal of Asthma 43 (5): 335–343.
Clougherty, J.E., J.I. Levy, L.D. Kubzansky, P.B. Ryan, S.F. Suglia, M.J. Canner, and R.J. Wright. 2007. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environmental Health Perspectives 115 (8): 1140–1146.
Clougherty, J.E., C.A. Rossi, J. Lawrence, M.S. Long, E.A. Diaz, R.H. Lim, B. McEwen, P. Koutrakis, and J.J. Godleski. 2010a. Chronic social stress and susceptibility to concentrated ambient fine particles in rats. Environmental Health Perspectives 118 (6): 769–775.
Clougherty, J.E., K. Souza, and M.R. Cullen. 2010b. Work and its role in shaping the social gradient in health. Annals of the New York Academy of Sciences 1186: 102–124.
Clougherty, J.E., and L.D. Kubzansky. 2010. A framework for examining social stress and susceptibility to air pollution in respiratory health. Environmental Health Perspectives 117 (9): 1351–1358.
Clougherty, J.E., J.L.C. Shmool, and L.D. Kubzansky. 2014. The role of non-chemical stressors in mediating socioeconomic susceptibility to environmental chemicals. Current Environmental Health Reports 1 (4): 302–313.
Cohen, S., D.A. Tyrrell, and A.P. Smith. 1991. Psychological stress and susceptibility to the common cold. New England Journal of Medicine 325 (9): 606–612.
Cohen, S., R.C. Kessler, and G.L. Underwood. 1995. Measuring stress: A guide for health and social scientists. New York: Oxford University Press.
Cory-Slechta, D.A., M.B. Virgolini, M. Thiruchelvam, D.D. Weston, and M.R. Bauter. 2004. Maternal stress modulates the effects of developmental lead exposure. Environmental Health Perspectives 112 (6): 717–730.
Cory-Slechta, D.A., S. Stern, D. Weston, J.L. Allen, and S. Liu. 2010. Enhanced learning deficits in female rats following lifetime pb exposure combined with prenatal stress. Toxicological Sciences 117 (2): 427–438.
Elliott, S.J., S.M. Taylor, S. Walter, D. Stieb, J. Frank, and J. Eyles. 1993. Modelling psychosocial effects of exposure to solid waste facilities. Social Science & Medicine 37 (6): 791–804.
Evans, G.W. 2003. A multimethodological analysis of cumulative risk and allostatic load among rural children. Developmental Psychology 39 (5): 924–933.
Eyles, J., S.M. Taylor, N. Johnson, and J. Baxter. 1993. Worrying about waste: Living close to solid waste disposal facilities in southern Ontario. Social Science & Medicine 37 (6): 805–812.
Kubzansky, L.D., I. Kawachi, and D. Sparrow. 1999. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: Any help from the concept of allostatic load? Annals of Behavioral Medicine 21 (4): 330–338.
Levy, J.I., M.P. Fabian, and J.L. Peters. 2014. Community-wide health risk assessment using geographically resolved demographic data: A synthetic population approach. PLoS One 9 (1): e87144.
Lipfert, F.W. 2004. Air pollution and poverty: Does the sword cut both ways? Journal of Epidemiology and Community Health 58 (1): 2–3.
Marmot, M.G., G.D. Smith, S. Stansfeld, C. Patel, F. North, J. Head, I. White, E. Brunner, and A. Feeney. 1991. Health inequalities among British civil servants: The Whitehall II study. Lancet 337 (8754): 1387–1393.
McEwen, B.S. 1998. Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences 840: 33–44.
Menzie, C.A., M.M. MacDonell, and M. Mumtaz. 2007. A phased approach for assessing combined effects from multiple stressors. Environmental Health Perspectives 115 (5): 807–816.
Miller, G.E., S. Cohen, and A.K. Ritchey. 2002. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid-resistance model. Health Psychology 21 (6): 531–541.
Miller, G.E., E. Chen, and E.S. Zhou. 2007. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin 133 (1): 25–45.
National Research Council. 2009. Science and decisions: Advancing risk assessment. Washington: National Research Council.
———. 2011. Improving health in the United States: The role of health impact assessment. Washington: National Research Council.
———. 2008. Phthalates and cumulative risk assessment: The tasks ahead. Washington: National Research Council.
Peters, J.L., M.P. Fabian, and J.I. Levy. 2014. Combined impact of lead, cadmium, polychlorinated biphenyls and non-chemical risk factors on blood pressure in NHANES. Environmental Research 132: 93–99.
Seeman, T.E., B.H. Singer, C.D. Ryff, G. Dienberg Love, and L. Levy-Storms. 2002. Social relationships, gender, and allostatic load across two age cohorts. Psychosomatic Medicine 64 (3): 395–406.
Selye, H. 1936. A syndrome produced by diverse nocuous agents. Nature 138: 32. https://doi.org/10.1038/138032a0.
Shankardass, K., R. McConnell, M. Jerrett, J. Milam, J. Richardson, and K. Berhane. 2009. Parental stress increases the effect of traffic-related air pollution on childhood asthma incidence. PNAS 106 (30): 12406–12411.
Shmool, J.L.C., L.D. Kubzansky, O. Dotson Newman, J. Spengler, P. Shepard, and J.E. Clougherty. 2014. Social stressors and air pollution across New York City: A spatial approach for assessing correlation among multiple exposures. Environmental Health 13 (91). https://doi.org/10.1186/1476-069X-13-91.
Shmool, J.L.C., J.F. Bobb, K. Ito, B. Elston, D.A. Savitz, Z. Ross, T.D. Matte, S. Johnson, F. Dominici, and J.E. Clougherty. 2015. Area-level socioeconomic deprivation, nitrogen dioxide exposure, and term birth weight in New York City. Environmental Research 142: 624–632. https://doi.org/10.1016/j.envres.2015.08.019.
Singh-Manoux, A., M.G. Marmot, and N.E. Adler. 2005. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine 67 (6): 855–861.
Subramanian, S.V., and I. Kawachi. 2004. Income inequality and health: What have we learned so far? Epidemiologic Reviews 26: 78–91.
U.S. Environmental Protection Agency. 2003. Framework for cumulative risk assessment. Washington: U.S. Environmental Protection Agency.
Virgolini, M.B., K. Chen, D.D. Weston, M.R. Bauter, and D.A. Cory-Slechta. 2005. Interactions of chronic lead exposure and intermittent stress: Consequences for brain catecholamine systems and associated behaviors and HPA axis function. Toxicological Sciences 87 (2): 469–482.
Virgolini, M.B., M.R. Bauter, D.D. Weston, and D.A. Cory-Slechta. 2006. Permanent alterations in stress responsivity in female offspring subjected to combined maternal lead exposure and/or stress. Neurotoxicology 27 (1): 11–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Clougherty, J.E., Levy, J.I. (2018). Psychosocial and Chemical Stressors. In: Rider, C., Simmons, J. (eds) Chemical Mixtures and Combined Chemical and Nonchemical Stressors. Springer, Cham. https://doi.org/10.1007/978-3-319-56234-6_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-56234-6_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56232-2
Online ISBN: 978-3-319-56234-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)