Abstract
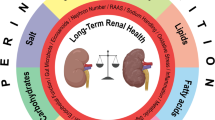
Adequate nutrition is fundamental to ensure undisturbed renal development. Macro- and micronutrient deficiency as well as energy overload or high-salt intake during gestation may significantly impair nephrogenesis and induce susceptibility toward disease. In addition, there is growing evidence that nutrition during early postnatal life is an important modulator of adult blood pressure and kidney function. The exact renal phenotype strongly depends on the type of dietary influence and the window of exposure. Thus, reduced glomerular count, microvascular rarefaction, and increased fibrosis are possible morphological findings. On the functional level, blood pressure levels, urinary protein excretion, and glomerular filtration rate are subject to dietary influences. Mechanistically, dysregulation of renin-angiotensin-aldosterone system (RAAS) components and other vasoactive substances, oxidative stress, altered mitochondrial energy metabolism, endoplasmic reticulum stress, and inflammatory processes are key factors. The present chapter gives an overview on current knowledge of dietary programming of renal disease. Defining the adequate amount of macro- and micronutrients which is needed for optimal kidney development remains a challenge for the future.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Blood pressure
- Glomerular count
- Glomerular filtration rate
- High-fat diet
- High-salt diet
- Low-protein diet
- Micronutrient deficiency
- Nephrogenesis
- Nephron number
- Proteinuria
- Renin-angiotensin-aldosterone system
Introduction
Renal development is tightly regulated (Challen et al. 2005), and human nephrogenesis starts by the tenth postconceptional week (Quigley 2012). In term-born children, the number of nephrons is determined at birth, whereas in preterm infants, nephron number may still increase postnatally (Sutherland et al. 2011; Fanni et al. 2012). Epidemiologic studies have linked intrauterine and early childhood conditions to unfavorable course of glomerulopathies (Zidar et al. 1998; Sheu and Chen 2001), decreased renal function in adulthood (Hallan et al. 2008), and increased risk of end-stage renal disease (Vikse et al. 2008). Serial ultrasound measurements of the kidney in a cohort of small for gestational age (SGA) infants revealed a marked reduction of renal growth rate compared to controls between 26 and 34 weeks of gestation, which suggests that the third trimester could be a critical period of renal programming (Konje et al. 1996). Although a variety of environmental conditions may influence nephrogenesis, adequate nutrition counts among the key factors ensuring undisturbed renal development (Fanni et al. 2012).
Generally, altered intake of macro- or micronutrients during critical developmental windows may lead to long-lasting effects on organ development, organ function, and susceptibility toward disease. In order to elucidate the mechanisms underlying dietary programming of renal disease, numerous animal models have been developed. Most authors have worked with rats in which kidney development is not completed before the second week of postnatal life (Neiss and Klehn 1981). The effects of dietary influences on renal outcome have been studied in a large variety of experimental settings like low-protein diet during gestation (Zeman 1968; Langley-Evans et al. 1999), calorie restriction during gestation (Bregere et al. 2010), maternal (Yamada-Obara et al. 2016) or postnatal high-fat diet (Aliou et al. 2016), maternal sodium overload (Cardoso et al. 2009), or postnatal hypernutrition (Boubred et al. 2007).
Regarding precise molecular mechanisms, a critical role of the renin-angiotensin system has been established (Woods et al. 2001; Bogdarina et al. 2007). However, programming of renal disease is a very complex process which cannot be explained by single dysregulated genes. The following article gives an overview on current knowledge of dietary programming of renal disease (Figs. 1, 2, 3, 4, and 5).
Effects of Dietary Intake During Gestation
Nutrient Deficiency During Gestation
Over the last decades, epidemiologists have studied the effects of exposure to famine during gestation on adult health parameters. Thus, it could be shown that the prevalence of microalbuminuria was elevated in adult persons aged 48–53 years who had been exposed to the Dutch Hunger Winter 1944/1945 during midgestation (Painter et al. 2005). Women born in rural areas during the Chinese famine years of 1959–1961 also had higher levels of proteinuria in their forth decade of life compared to women born before or after the famine (Huang et al. 2014).
Male rat offspring exposed to a multideficient diet in utero showed elevated plasma volume, blood pressure, and parameters of oxidative stress in the kidney (Magalhaes et al. 2006). In a baboon model, calorie restriction (CR) during gestation reduced tubular density (Cox et al. 2006) and altered fetal expression of genes affecting renal mitochondrial energy metabolism (Pereira et al. 2015). However, there is also some evidence for a potential beneficial effect of CR during gestation. A study in sheep suggested that CR in early gestation may provide protective effects against obesity-related nephropathy in the offspring by modulating the inflammatory system (Sharkey et al. 2009).
Low-Protein Diet During Gestation
The specific effect of protein restriction during gestation was tested in animal models. In 1968 already, Frances Zeman subjected rat dams to a casein restriction throughout gestation (6% vs. 24% in controls). Pups were sacrificed immediately after birth, and the kidneys were processed for histological studies. Kidneys from protein-restricted animals were characterized by fewer and less well-differentiated glomeruli, a greater proportion of connective tissue, and relatively fewer collecting tubules. Three decades later, Langley-Evans and colleagues studied different groups of rat offspring exposed to 9% casein restriction either throughout gestation or for single-week periods (days 0–7, 8–14, 15–22 of gestation). Controls were fed a diet containing 18% casein. At birth, nephron number was significantly reduced in offspring exposed to low-protein diet during the second and third weeks of gestation only. This indicates that the impact of protein deficiency depends on the window of exposure (Langley-Evans et al. 1999).
However, low-protein (LP) diet during gestation resulted in reduced nephron numbers in most studies with the exception of protein restriction during early pregnancy only (Jones et al. 2001; Woods et al. 2001, 2004; Siddique et al. 2014). Depending on the exact model and the time point investigated, many studies also demonstrate elevated arterial blood pressure (Langley-Evans et al. 1999; Woods et al. 2004; Black et al. 2015; Lozano et al. 2015) and reduced glomerular filtration rate (Nwagwu et al. 2000; DuBois et al. 2014; Lozano et al. 2015). Microvascular rarefaction, as shown in a sheep model, may contribute to these findings (Lloyd et al. 2012). Further functional restrictions in adult LP rat offspring were demonstrated in a study evaluating the furosemide diuretic response during adulthood. The extent of diuresis was decreased in both male and female LP animals (DuBois et al. 2014) indicating altered tubular function. In addition, low-protein animals may have less regenerative capacities to recover from secondary renal injury (Plank et al. 2006).
High-Salt Diet During Gestation
Human data on kidney function of children exposed to defined amounts of sodium chloride during gestation is not available. Kidney outcome in rat offspring whose mothers were exposed to water containing 1% sodium chloride throughout gestation was studied at the age of 3 months. Interestingly, only urinary protein excretion was increased in the saline group, whereas the number of nephrons, blood pressure, renal hemodynamics, and renal oxidative stress were not different between the groups. If the dams were also maintained on saline during lactation, the effect on the renal phenotype in the offspring was more prominent. These animals also had a reduced glomerular filtration rate, signs of oxidative stress, and an increase in plasma volume (Cardoso et al. 2009). In another study, both low-sodium (0.07% NaCl) and high-sodium (3%) diet throughout gestation and lactation caused reduced glomerular number. In addition, high-salt (3%) offspring developed arterial hypertension (Koleganova et al. 2011). Adult offspring exposed to 4% NaCl diet throughout gestation and lactation developed hypernatremia and elevated plasma levels of corticosterone. Blood pressure was only elevated in male offspring (Gray et al. 2013). In ewes fed a high-salt diet, kidney weight to body weight ratio was reduced in the offspring going along with changes in the renal and systemic renin-angiotensin-aldosterone system (Chadwick et al. 2009, Mao et al. 2013).
Maternal Obesity and High-Fat Diet During Gestation
Epidemiologic studies suggest that there is an association between maternal obesity and elevated systolic blood pressure in midchildhood (Perng et al. 2014). In addition, a preconceptional body mass index of greater than 30 kg/m2 was identified as a risk factor for bilateral renal aplasia/hypoplasia (Slickers et al. 2008).
Consistent with these findings, rat offspring exposed to high-fat diet during gestation and weaned to normal-fat diet developed arterial hypertension. On the molecular level, permanent changes in key RAAS elements were dependent on the exact window of exposure (Guberman et al. 2013). In another study, rat offspring exposed to a lard-rich diet during gestation had reduced renal renin activity and Na+, K+−ATPase enzyme activity at 180 days of age (Armitage et al. 2005). Both in utero and postnatal exposure of rats to high-fat diet induced glomerulosclerosis and tubulointerstitial fibrosis at 17 weeks of age going along with albuminuria (Jackson et al. 2012).
Micronutrient Deficiency During Gestation
Small epidemiologic studies suggest that maternal vitamin A deficiency might be associated with reduced renal volume in the neonate (Goodyer et al. 2007; El-Khashab et al. 2013).
This hypothesis is supported by the observation that vitamin A deprivation during rat gestation induced a nephron deficit in the offspring (Lelievre-Pegorier et al. 1998). A similar effect was demonstrated in rat models of iron and zinc deficiency during gestation. Adult offspring of iron-deficient dams had reduced glomerular density and arterial hypertension (Lisle et al. 2003). Zinc deficiency during gestation and postweaning period caused a nephron deficit, increased systolic blood pressure, and decreased glomerular filtration rate going along with signs of oxidative stress, fibrosis, and increased apoptosis. Postweaning normalization of zinc only partially normalized these findings (Tomat et al. 2008).
Substance Use During Gestation
It is general knowledge that substance use during gestation can have negative influence on the health and well-being of the offspring. Although alterations in organ development and function are often considered as toxic effects in the first line, there is an overlap between toxic and programming effects during critical developmental windows.
In a large human cohort study, maternal smoking showed a dose-dependent effect on fetal kidney volume (Taal et al. 2011). Continued maternal smoking during pregnancy was associated with lower eGFR in school-aged children, whereas smoking during the first trimester was only associated with a higher risk of microalbuminuria (Kooijman et al. 2015). Another epidemiological study demonstrates that smoking during the periconceptional period may increase the risk of bilateral renal aplasia/hypoplasia. The same study also identified binge drinking during the second month of pregnancy as a risk factor for renal agenesis/hypoplasia (Slickers et al. 2008). In animals, ethanol exposure on two occasions during rat gestation induced low nephron number and elevated arterial blood pressure in the offspring (Gray et al. 2010). Rat metanephroi cultured in the presence of ethanol showed less ureteric branching and reduced glomerular numbers. Coculture with retinoic acid ameliorated these findings (Gray et al. 2012). In sheep, repeated alcohol exposure during the second half of gestation similarly reduced nephron numbers in the offspring (Gray et al. 2008).
Rat offspring exposed to 120 mg/kg of caffeine daily during gestation developed significant renal alterations indicative of glomerulosclerosis and interstitial fibrosis. In detail, the authors observed thickening of the glomerular basement membrane, expansion of the mesangium, partial tubular atrophy, and ultrastructural damage of podocytes. On the molecular level, low renal angiotensin II receptor type 2 expression was present in both fetal and adult offspring (Ao et al. 2015).
Effects of Altered Dietary Intake in the Postnatal Period
Early Nutrition
There is growing evidence that early nutrition as represented by early weight gain is an important modulator of adult blood pressure and kidney function.
Epidemiologic data suggest that not only prenatal but also postnatal growth patterns are associated with adult blood pressure (Ben-Shlomo et al. 2008). In a large US multicenter cohort study, pronounced catch-up growth in small for gestational age (SGA) babies resulted in an increased risk of arterial hypertension. Since lack of catch-up growth was associated with an increased risk of infection and low IQ, the authors suggested that rapid catch-up growth to the 30th centile during the first months of life and slower catch-up growth up to the 50th centile might be ideal (Lei et al. 2015). Another SGA cohort study observed that nutrition with a protein-enriched formula during the first months of life was associated with increased diastolic and mean arterial blood pressure values at 6–8 years of age.
In a rat model of placental insufficiency, cross-fostering the restricted offspring to control dams ameliorated both renal morphology and blood pressure in adulthood. Restricted pups raised by their own mothers developed arterial hypertension and reduced nephron number. Cross-fostering restricted pups to control mothers normalized nephron number and prevented the development of arterial hypertension (Wlodek et al. 2007). In another study, offspring exposed to LP diet prenatally and cross-fostered to foster dams receiving standard diet did not develop elevated blood pressure and presented with normal glomerular filtration rate in adulthood (Lozano et al. 2015). Conversely, offspring from standard diet dams cross-fostered to a low-protein foster mother (NP/LP) developed arterial hypertension. On the molecular level, the latter group had increased renal NKCC2 and NCC cotransporter expression which was not present in a LP/LP group. Both NP/LP and LP/LP offspring had elevated plasma renin and angiotensin II levels (Siddique et al. 2014).
However, control rats exposed to early hypernutrition induced by litter-size reduction developed significantly increased systolic blood pressure and proteinuria (Boubred et al. 2007) and decreased glomerular filtration rate (Alcazar et al. 2012). On the morphological level, the number of nephrons was increased, but there was enhanced glomerulosclerosis (Boubred et al. 2007). Mechanistically, this was accompanied by SOCS-3-mediated intrinsic renal leptin resistance (Alcazar et al. 2012). When litter-size reduction was performed in offspring exposed to LP diet in utero, the animals similarly developed arterial hypertension and glomerulosclerosis, but nephron number was reduced (Boubred et al. 2009).
Postnatal Calorie Restriction
In a mouse model, calorie restriction (CR) mitigated the effects of renal aging. Thus, CR mice had decreased glomerular basement membrane thickening and autophagy. Interestingly, a modulation of dietary fat composition had additional beneficial effects (Calvo-Rubio et al. 2016). In another study investigating the effect of calorie restriction on renal ischemia reperfusion injury, CR showed dose-dependent protective effects. Protein restriction (PR) in addition to CR further improved renal outcome. From a mechanistic point of view, the authors provide evidence that altered activation of AMPK and mTORC1 could play a crucial role and that administration of leptin mitigates the beneficial effects of CR/PR (Robertson et al. 2015).
Postnatal High-Salt Diet
In a rat study, challenge with drinking water containing 2% sodium chloride from postnatal week 12 until postnatal week 16 did not alter blood pressure or renal function in control animals. In contrast, former IUGR offspring developed sodium-dependent hypertension, reduced glomerular filtration rate, and albuminuria (Sanders et al. 2005).
Postnatal High-Fat Diet
Adult mice fed a high-fat diet (HFD) for 14 weeks developed significant proteinuria. Renal gene expressions of renin, angiotensin-converting enzyme, and tubular injury markers NGAL and KIM-1 were elevated. Protein expressions of ER stress markers BiP and CHOP were also increased (Li et al. 2016). In another mouse model, long-term HFD for 28 weeks resulted in enhanced mitochondrial damage in podocytes, proximal tubules, and endothelial cells. Furthermore, infiltration with CD68+ macrophages was increased, and proinflammatory markers were upregulated. Treatment with SS-31 which protects mitochondrial cristae structure mitigated all these effects (Szeto et al. 2016). In rats, high-fat diet induced proteinuria and ultrastructural changes in podocyte morphology. On the molecular level, the authors observed changes in the expression of proteins relevant for podocyte function like desmin, nephrin, and CD2AP (Chen et al. 2016).
Postnatal Micronutrient Deficiency
Vitamin D levels are known to be reduced in many different clinical settings. In a population-based cohort study, low plasma 25-hydroxyvitamin D levels were associated with an increased risk of developing albuminuria (Keyzer et al. 2015). However, in another population, these findings could not be confirmed (Guessous et al. 2015). In rodents, it could be shown that 1,25-vitamin D3-deficient animals develop podocyte injury (Sonneveld et al. 2016). In these mice, a slit diaphragm protein expressed by podocytes (TRPC6) was upregulated. Administration of 1,25-D3 brought TRPC6 expression back to normal and normalized podocyte morphology and urinary protein excretion (Sonneveld et al. 2013).
In a lacto-vegetarian population, the role of micronutrient deficiency was studied in the context of arterial hypertension. Data analysis revealed that low intake of vitamin C, folic acid, and zinc may increase the risk of developing arterial hypertension (Chiplonkar et al. 2004).
Molecular Mechanisms of Dietary Renal Programming
Regarding molecular mechanisms of dietary renal programming, there is strong evidence for a critical role of the renin-angiotensin-aldosterone system (RAAS), although study results are partly contradictory.
In newborn low-protein rat pups, renal renin gene and protein expression was significantly suppressed (Woods et al. 2001). In the adrenal gland of neonatal LP rats, gene expression of the angiotensin II receptor type 1b was upregulated (Bogdarina et al. 2007). At 4 weeks of age, male LP rats responded with a greater decrease in glomerular filtration rate when challenged with a bolus of enalapril followed by an infusion of angiotensin II. In the kidney, angiotensin II receptor type I expression was increased (Sahajpal and Ashton 2003). At 4 and 13 weeks of age, plasma angiotensin-converting enzyme (ACE) activity in LP offspring was elevated going along with increased systolic blood pressure. Renin activity in these animals was normal, and plasma angiotensin II concentrations were only slightly elevated (Langley-Evans and Jackson 1995).
High-salt diet (8% NaCl) during the second half of gestation in ewes induced decreased plasma angiotensin II levels in fetal offspring which normalized postnatally. Gene expressions of AGT, AT1, AT2, and ACE were elevated during fetal life and, except for AT2, decreased at postnatal day 90 (Mao et al. 2013). In another sheep study, salt-enriched diet (14% NaCl) or grazing saltbush during gestation decreased basal renin activity in the offspring. Challenged with salt, saltbush offspring still had decreased renin activity, whereas renin activity in high-salt offspring normalized (Chadwick et al. 2009). High-fat diet during gestation, lactation, or postweaning specifically influenced RAAS elements in adipose tissue dependent upon the timing of exposure (Guberman et al. 2013; Li et al. 2016). Treatment of human proximal tubule epithelial cells (HK2) with saturated fatty acid palmitic acid induced an increase in the cellular expression of ER stress markers as well as increased angiotensin II concentrations in cultured medium. RAAS blockade with valsartan or aliskiren protected the cells from the development of ER stress (Li et al. 2016). Caffeine exposure during gestation in rats induced downregulation of the angiotensin II receptor type 2 (Ao et al. 2015).
However, not only RAAS components but also other vasoactive substances and blood pressure-regulating systems are nutrient-sensitive. Thus, maternal LP diet in rats reduced renal 11betaHSD2 expression in adult offspring (Bertram et al. 2001). Other mechanisms involved in dietary programming of renal function are oxidative stress (Magalhaes et al. 2006; Tomat et al. 2008; Costa et al. 2016), mitochondrial energy metabolism (Pereira et al. 2015; Szeto et al. 2016), ER stress (Li et al. 2016), and inflammation (Szeto et al. 2016).
Dietary Interventions
A better knowledge of the mechanisms and principles leading to programming of renal disease bears the opportunity to develop strategies with the aim of modifying the long-term effects of unfavorable environmental conditions (“reprogramming”). In addition, this knowledge can also be used to establish interventional approaches to influence the natural course of “nonprogrammed” pathologic conditions.
Most studies on “nutritional reprogramming” of renal disease have been performed in animals. However, there are a couple of interventional studies in humans. In rural Bangladesh, the effect of early food supplementation (608 kcal/day energy and 18 g/day of vegetable protein) and micronutrient supplementation (containing either iron and folate or multiple micronutrients) during pregnancy was studied. Adjusted analysis provided evidence that there is a small but significant positive effect of food supplementation on blood pressure at age 4.5 years. In addition, high-iron supplement was associated with a higher GFR (Hawkesworth et al. 2013). Nepalese children whose mothers had been supplemented with the daily allowance of 15 vitamins and minerals during pregnancy had a slightly lower blood pressure at age 2.5 years than controls (Vaidya et al. 2008). Maternal supplementation with folic acid or folic acid + iron + zinc reduced the risk of developing albuminuria in 6–8-year-old Nepalese children (Stewart et al. 2009). In an Argentinian study, the effect of additional 2 g calcium per day during pregnancy was studied in 5–9-year-old children. Children whose mothers had been assigned to the calcium group had lower systolic blood pressure values (Belizan et al. 1997). Calcium supplementation in a small group of 11-year-old children also provided a small blood pressure-lowering effect (Gillman et al. 1995). In a small European study, supplementation of infant formula with LCPUFAs reduced blood pressure values at 6 years of age compared to standard formula-fed infants (Forsyth et al. 2003).
In animals, most dietary interventions have been performed in the low-protein model of IUGR. Thus, it is obvious that supplementation of single amino acids might have a positive effect. Indeed, supplementation of a low-protein diet with 3% glycine during gestation prevented the development of arterial hypertension in the offspring (Jackson et al. 2002).
Since oxidative stress may significantly impair nephrogenesis and adequate levels of retinoic acid are crucial for normal kidney development (Lee et al. 2012), several studies have focused on the importance of retinoic acid and other antioxidants. In one study, administration of a single dose of retinoic acid (20 mg/kg) during low-protein gestation at embryonic day 11.5 normalized nephron number in the offspring (Makrakis et al. 2007). However, postnatal treatment with retinoic acid in preterm baboons had neither beneficial nor negative effects on glomerular number or glomerular morphology (Sutherland et al. 2009). Supplementation of lazaroid, a lipid peroxidase inhibitor, throughout LP gestation prevented the development of arterial hypertension. In addition, capillary density normalized and measures of vascular function improved (Cambonie et al. 2007). Administration of ACH09, a grape skin extract with antioxidant properties, normalized nephron numbers in LP offspring (Costa et al. 2016).
A further approach is the administration of food or spices with anti-inflammatory properties. Curcumin has been studied in various settings and exerts both anti-inflammatory and antioxidant effects. In a rat model of postnatal kidney damage induced by unilateral ureteral obstruction, there was evidence for the activation of an antiapoptotic mechanism by increased expression of the TRADD-RIP-TRAF complex (Hashem et al. 2016). Another study could demonstrate that curcumin can alleviate diabetic nephropathy by regulating the Wnt pathway (Ho et al. 2016).
Conclusion
Both macro- and micronutrient deficiency and overload during critical developmental windows may significantly impair nephrogenesis and induce susceptibility toward disease. Defining the adequate amount of macro- and micronutrients which is needed for optimal kidney development remains a challenge for the future.
Mini-dictionary of Terms
-
Blood Pressure – Intravascular pressure. Blood pressure is influenced by cardiac output, vascular resistance and intravascular volume.
-
Gestation – Pregnancy.
-
Glomerular count – Used to estimate nephron number.
-
Glomerular Filtration Rate (GFR) – Blood volume which is filtered by the kidney during a defined time unit. GFR is the most common measure of renal function. In clinical practice, creatinine or cystatin C based calculations are usually used to estimate GFR.
-
High-Fat Diet – Nutrient composition with increased percentage of fat (e.g. 30-60% of calories in rodents).
-
High-Salt Diet – Increased dietary intake of salt.
-
Low-Protein Diet – Reduced intake of protein (e.g. in rodents: 6-9 g protein in 100 g diet).
-
Micronutrient Deficiency – Dietary lack of one or more micronutrients (e.g. vitamins, minerals) essential to an individual’s health.
-
Nephrogenesis – Development of the kidney.
-
Nephron Number – The nephron is the basic structural and functional unit of the kidney. Nephron number considerably varies between individuals. Low nephron number has been linked to an increased risk of cardiovascular and renal disease.
-
Postnatal(ly) – After birth.
-
Proteinuria – Increased excretion of proteins by the kidney resulting in elevated concentrations of proteins in the urine.
-
Renin-angiotensin-aldosterone system (RAAS) – Hormons (renin, angiotensinogen, angiotensin, aldosterone) interacting to regulate blood pressure, intravascular volume and plasma sodium concentration. In addition, local effects like cardiac remodeling are known.
Key Facts of Nephrogenesis
-
Nephrogenesis is a tightly controlled process, and small changes in gene or protein expression during critical timespans may significantly impair renal development.
-
Human nephrogenesis starts by the tenth postconceptional week.
-
The final kidney originates from two embryonic tissues: the ureteric bud forming the collecting duct system of the kidney and the mesonephros which will form the nephrons.
-
In humans, the number of nephrons is fixed at term, but it can vary between three hundred thousand and two millions per kidney
-
There are numerous causes for a reduction in nephron number including ethnicity; prematurity; placental insufficiency; maternal diets deficient in protein, iron, or vitamin A; maternal hyperglycemia; and intrauterine exposure to certain drugs(e.g., COX-2 inhibitors).
-
Reduced nephron number has been linked to the development of arterial hypertension and susceptibility toward renal disease in later life.
Summary Points
-
Adequate nutrition is fundamental to ensure undisturbed renal development.
-
Macro- and micronutrient deficiency as well as energy overload or high-salt intake during gestation may significantly impair nephrogenesis and induce susceptibility toward disease.
-
In addition, there is growing evidence that early nutrition is an important modulator of adult blood pressure and kidney function.
-
The exact renal phenotype strongly depends on the type of dietary influence and the window of exposure.
-
In order to elucidate the mechanisms underlying dietary programming of renal disease, numerous animal models have been developed.
-
Reduced glomerular count, microvascular rarefaction, or increased fibrosis are possible morphological findings.
-
Mechanistically, dysregulation of renin-angiotensin-aldosterone system (RAAS) components and other vasoactive substances, oxidative stress, altered mitochondrial energy metabolism, endoplasmic reticulum stress, and inflammatory processes are key factors.
-
On the functional level, blood pressure levels, urinary protein excretion, and glomerular filtration rate are subject to dietary influences.
-
In interventional studies, the effect of dietary supplementation with vitamin A, iron, folic acid, zinc, calcium, long-chain polyunsaturated fatty acids, or antioxidants has been tested and yielded some beneficial effects.
-
Defining the adequate amount of macro- and micronutrients which is needed for optimal kidney development remains a challenge for the future.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- ACH09:
-
Grape skin extract with antioxidant properties
- AGT:
-
Angiotensinogen
- AT1:
-
Angiotensin II receptor type 1
- AT2:
-
Angiotensin II receptor type 2
- AMPK:
-
5′ adenosine monophosphate-activated protein kinase
- BiP:
-
ER stress marker
- CD2AP:
-
CD2-associated protein
- CHOP:
-
ER stress marker
- CR:
-
Calorie restriction
- eGFR:
-
Estimated glomerular filtration rate
- ER stress:
-
Endoplasmic reticulum stress
- GFR:
-
Glomerular filtration rate
- HFD:
-
High-fat diet
- IQ:
-
Intelligence quotient
- IUGR:
-
Intrauterine growth restriction
- KIM-1:
-
Kidney injury molecule-1, biomarker for renal proximal tubule injury
- LCPUFAs:
-
Long-chain polyunsaturated fatty acids
- LP:
-
Low protein
- mTORC1:
-
Mammalian target of rapamycin complex 1
- NaCl:
-
Sodium chloride
- NCC:
-
Sodium-chloride symporter
- NGAL:
-
Neutrophil gelatinase-associated lipocalin, biomarker for acute kidney injury
- NKCC2:
-
Sodium-potassium-chloride cotransporter
- PR:
-
Protein restriction
- RAAS:
-
Renin-angiotensin-aldosterone system
- SGA:
-
Small for gestational age
- SS-31:
-
Substance which protects mitochondrial cristae
- TRPC6:
-
Transient receptor potential cation channel, subfamily C, member 6
- US:
-
United States
References
Alcazar MA, Boehler E, Rother E, Amann K, Vohlen C, von Horsten S, Plank C, Dotsch J (2012) Early postnatal hyperalimentation impairs renal function via SOCS-3 mediated renal postreceptor leptin resistance. Endocrinology 153(3):1397–1410
Aliou Y, Liao MC, Zhao XP, Chang SY, Chenier I, Ingelfinger JR, Zhang SL (2016) Post-weaning high-fat diet accelerates kidney injury, but not hypertension programmed by maternal diabetes. Pediatr Res 79(3):416–424
Ao Y, Sun Z, Hu S, Zuo N, Li B, Yang S, Xia L, Wu Y, Wang L, He Z, Wang H (2015) Low functional programming of renal AT2R mediates the developmental origin of glomerulosclerosis in adult offspring induced by prenatal caffeine exposure. Toxicol Appl Pharmacol 287(2):128–138
Armitage JA, Lakasing L, Taylor PD, Balachandran AA, Jensen RI, Dekou V, Ashton N, Nyengaard JR, Poston L (2005) Developmental programming of aortic and renal structure in offspring of rats fed fat-rich diets in pregnancy. J Physiol 565(Pt 1):171–184
Belizan JM, Villar J, Bergel E, del Pino A, Di Fulvio S, Galliano SV, Kattan C (1997) Long-term effect of calcium supplementation during pregnancy on the blood pressure of offspring: follow up of a randomised controlled trial. BMJ 315(7103):281–285
Ben-Shlomo Y, McCarthy A, Hughes R, Tilling K, Davies D, Smith GD (2008) Immediate postnatal growth is associated with blood pressure in young adulthood: the Barry Caerphilly Growth Study. Hypertension 52(4):638–644
Bertram C, Trowern AR, Copin N, Jackson AA, Whorwood CB (2001) The maternal diet during pregnancy programs altered expression of the glucocorticoid receptor and type 2 11beta-hydroxysteroid dehydrogenase: potential molecular mechanisms underlying the programming of hypertension in utero. Endocrinology 142(7):2841–53
Black MJ, Lim K, Zimanyi MA, Sampson AK, Bubb KJ, Flower RL, Parkington HC, Tare M, Denton KM (2015) Accelerated age-related decline in renal and vascular function in female rats following early-life growth restriction. Am J Phys Regul Integr Comp Phys 309(9):R1153–R1161
Bogdarina I, Welham S, King PJ, Burns SP, Clark AJ (2007) Epigenetic modification of the renin-angiotensin system in the fetal programming of hypertension. Circ Res 100(4):520–526
Boubred F, Buffat C, Feuerstein JM, Daniel L, Tsimaratos M, Oliver C, Lelievre-Pegorier M, Simeoni U (2007) Effects of early postnatal hypernutrition on nephron number and long-term renal function and structure in rats. Am J Physiol Ren Physiol 293(6):F1944–F1949
Boubred F, Daniel L, Buffat C, Feuerstein JM, Tsimaratos M, Oliver C, Dignat-George F, Lelievre-Pegorier M, Simeoni U (2009) Early postnatal overfeeding induces early chronic renal dysfunction in adult male rats. Am J Physiol Ren Physiol 297(4):F943–F951
Bregere C, Rebrin I, Gallaher TK, Sohal RS (2010) Effects of age and calorie restriction on tryptophan nitration, protein content, and activity of succinyl-CoA:3-ketoacid CoA transferase in rat kidney mitochondria. Free Radic Biol Med 48(4):609–618
Calvo-Rubio M, Buron MI, Lopez-Lluch G, Navas P, de Cabo R, Ramsey JJ, Villalba JM, Gonzalez-Reyes JA (2016) Dietary fat composition influences glomerular and proximal convoluted tubule cell structure and autophagic processes in kidneys from calorie-restricted mice. Aging Cell 15(3):477–487
Cambonie G, Comte B, Yzydorczyk C, Ntimbane T, Germain N, Le NL, Pladys P, Gauthier C, Lahaie I, Abran D, Lavoie JC, Nuyt AM (2007) Antenatal antioxidant prevents adult hypertension, vascular dysfunction, and microvascular rarefaction associated with in utero exposure to a low-protein diet. Am J Phys Regul Integr Comp Phys 292(3):R1236–R1245
Cardoso HD, Cabral EV, Vieira-Filho LD, Vieyra A, Paixao AD (2009) Fetal development and renal function in adult rats prenatally subjected to sodium overload. Pediatr Nephrol 24(10):1959–1965
Chadwick MA, Vercoe PE, Williams IH, Revell DK (2009) Dietary exposure of pregnant ewes to salt dictates how their offspring respond to salt. Physiol Behav 97(3–4):437–445
Challen G, Gardiner B, Caruana G, Kostoulias X, Martinez G, Crowe M, Taylor DF, Bertram J, Little M, Grimmond SM (2005) Temporal and spatial transcriptional programs in murine kidney development. Physiol Genomics 23(2):159–171
Chen JY, Jian DY, Lien CC, Lin YT, Ting CH, Chen LK, Hsu TC, Huang HM, Wu YT, Kuan TT, Chao YW, Wu LY, Huang SW, Juan CC (2016) Adipocytes play an etiological role in the podocytopathy of high-fat diet-fed rats. J Endocrinol 231:109–120
Chiplonkar SA, Agte VV, Tarwadi KV, Paknikar KM, Diwate UP (2004) Micronutrient deficiencies as predisposing factors for hypertension in lacto-vegetarian Indian adults. J Am Coll Nutr 23(3):239–247
Costa MR, Pires KM, Nalbones-Barbosa MN, Dos Santos Valenca S, Resende AC, de Moura RS (2016) Grape skin extract-derived polyphenols modify programming-induced renal endowment in prenatal protein-restricted male mouse offspring. Eur J Nutr 55(4):1455–1464
Cox LA, Nijland MJ, Gilbert JS, Schlabritz-Loutsevitch NE, Hubbard GB, McDonald TJ, Shade RE, Nathanielsz PW (2006) Effect of 30 percent maternal nutrient restriction from 0.16 to 0.5 gestation on fetal baboon kidney gene expression. J Physiol 572(Pt 1):67–85
DuBois BN, Pearson J, Mahmood T, Nguyen D, Thornburg K, Cherala G (2014) Perinatal growth restriction decreases diuretic action of furosemide in adult rats. Eur J Pharmacol 728:39–47
El-Khashab EK, Hamdy AM, Maher KM, Fouad MA, Abbas GZ (2013) Effect of maternal vitamin A deficiency during pregnancy on neonatal kidney size. J Perinat Med 41(2):199–203
Fanni D, Gerosa C, Nemolato S, Mocci C, Pichiri G, Coni P, Congiu T, Piludu M, Piras M, Fraschini M, Zaffanello M, Iacovidou N, Van Eyken P, Monga G, Faa G, Fanos V (2012) “Physiological” renal regenerating medicine in VLBW preterm infants: could a dream come true? J Matern Fetal Neonatal Med 25(Suppl 3):41–48
Forsyth JS, Willatts P, Agostoni C, Bissenden J, Casaer P, Boehm G (2003) Long chain polyunsaturated fatty acid supplementation in infant formula and blood pressure in later childhood: follow up of a randomised controlled trial. BMJ 326(7396):953
Gillman MW, Hood MY, Moore LL, Nguyen US, Singer MR, Andon MB (1995) Effect of calcium supplementation on blood pressure in children. J Pediatr 127(2):186–192
Goodyer P, Kurpad A, Rekha S, Muthayya S, Dwarkanath P, Iyengar A, Philip B, Mhaskar A, Benjamin A, Maharaj S, Laforte D, Raju C, Phadke K (2007) Effects of maternal vitamin A status on kidney development: a pilot study. Pediatr Nephrol 22(2):209–214
Gray SP, Kenna K, Bertram JF, Hoy WE, Yan EB, Bocking AD, Brien JF, Walker DW, Harding R, Moritz KM (2008) Repeated ethanol exposure during late gestation decreases nephron endowment in fetal sheep. Am J Phys Regul Integr Comp Phys 295(2):R568–R574
Gray SP, Denton KM, Cullen-McEwen L, Bertram JF, Moritz KM (2010) Prenatal exposure to alcohol reduces nephron number and raises blood pressure in progeny. J Am Soc Nephrol 21(11):1891–1902
Gray SP, Cullen-McEwen LA, Bertram JF, Moritz KM (2012) Mechanism of alcohol-induced impairment in renal development: could it be reduced by retinoic acid? Clin Exp Pharmacol Physiol 39(9):807–813
Gray C, Al-Dujaili EA, Sparrow AJ, Gardiner SM, Craigon J, Welham SJ, Gardner DS (2013) Excess maternal salt intake produces sex-specific hypertension in offspring: putative roles for kidney and gastrointestinal sodium handling. PLoS One 8(8):e72682
Guberman C, Jellyman JK, Han G, Ross MG, Desai M (2013) Maternal high-fat diet programs rat offspring hypertension and activates the adipose renin-angiotensin system. Am J Obstet Gynecol 209(3):262 e261–262 e268
Guessous I, McClellan W, Kleinbaum D, Vaccarino V, Hugues H, Boulat O, Marques-Vidal P, Paccaud F, Theler JM, Gaspoz JM, Burnier M, Waeber G, Vollenweider P, Bochud M (2015) Serum 25-hydroxyvitamin D level and kidney function decline in a Swiss general adult population. Clin J Am Soc Nephrol 10(7):1162–1169
Hallan S, Euser AM, Irgens LM, Finken MJ, Holmen J, Dekker FW (2008) Effect of intrauterine growth restriction on kidney function at young adult age: the Nord Trondelag Health (HUNT 2) Study. Am J Kidney Dis 51(1):10–20
Hashem RM, Mohamed RH, Abo-El-matty DM (2016) Effect of curcumin on TNFR2 and TRAF2 in unilateral ureteral obstruction in rats. Nutrition 32(4):478–485
Hawkesworth S, Wagatsuma Y, Kahn AI, Hawlader MD, Fulford AJ, Arifeen SE, Persson LA, Moore SE (2013) Combined food and micronutrient supplements during pregnancy have limited impact on child blood pressure and kidney function in rural Bangladesh. J Nutr 143(5):728–734
Ho C, Hsu YC, Lei CC, Mau SC, Shih YH, Lin CL (2016) Curcumin rescues diabetic renal fibrosis by targeting superoxide-mediated Wnt signaling pathways. Am J Med Sci 351(3):286–295
Huang C, Guo C, Nichols C, Chen S, Martorell R (2014) Elevated levels of protein in urine in adulthood after exposure to the Chinese famine of 1959–61 during gestation and the early postnatal period. Int J Epidemiol 43(6):1806–1814
Jackson AA, Dunn RL, Marchand MC, Langley-Evans SC (2002) Increased systolic blood pressure in rats induced by a maternal low-protein diet is reversed by dietary supplementation with glycine. Clin Sci (Lond) 103(6):633–639
Jackson CM, Alexander BT, Roach L, Haggerty D, Marbury DC, Hutchens ZM, Flynn ER, Maric-Bilkan C (2012) Exposure to maternal overnutrition and a high-fat diet during early postnatal development increases susceptibility to renal and metabolic injury later in life. Am J Physiol Ren Physiol 302(6):F774–F783
Jones SE, Bilous RW, Flyvbjerg A, Marshall SM (2001) Intra-uterine environment influences glomerular number and the acute renal adaptation to experimental diabetes. Diabetologia 44(6):721–728
Keyzer CA, Lambers-Heerspink HJ, Joosten MM, Deetman PE, Gansevoort RT, Navis G, Kema IP, de Zeeuw D, Bakker SJ, de Borst MH, P. S. Group (2015) Plasma vitamin D level and change in albuminuria and eGFR according to sodium intake. Clin J Am Soc Nephrol 10(12):2119–2127
Koleganova N, Piecha G, Ritz E, Becker LE, Muller A, Weckbach M, Nyengaard JR, Schirmacher P, Gross-Weissmann ML (2011) Both high and low maternal salt intake in pregnancy alter kidney development in the offspring. Am J Physiol Ren Physiol 301(2):F344–F354
Konje JC, Bell SC, Morton JJ, de Chazal R, Taylor DJ (1996) Human fetal kidney morphometry during gestation and the relationship between weight, kidney morphometry and plasma active renin concentration at birth. Clin Sci (Lond) 91(2):169–175
Kooijman MN, Bakker H, Franco OH, Hofman A, Taal HR, Jaddoe VW (2015) Fetal smoke exposure and kidney outcomes in school-aged children. Am J Kidney Dis 66(3):412–420
Langley-Evans SC, Jackson AA (1995) Captopril normalises systolic blood pressure in rats with hypertension induced by fetal exposure to maternal low protein diets. Comp Biochem Physiol A Physiol 110(3):223–8
Langley-Evans SC, Welham SJ, Jackson AA (1999) Fetal exposure to a maternal low protein diet impairs nephrogenesis and promotes hypertension in the rat. Life Sci 64(11):965–974
Lee LM, Leung CY, Tang WW, Choi HL, Leung YC, McCaffery PJ, Wang CC, Woolf AS, Shum AS (2012) A paradoxical teratogenic mechanism for retinoic acid. Proc Natl Acad Sci U S A 109(34):13668–13673
Lei X, Chen Y, Ye J, Ouyang F, Jiang F, Zhang J (2015) The optimal postnatal growth trajectory for term small for gestational age babies: a prospective cohort study. J Pediatr 166(1):54–58
Lelievre-Pegorier M, Vilar J, Ferrier ML, Moreau E, Freund N, Gilbert T, Merlet-Benichou C (1998) Mild vitamin A deficiency leads to inborn nephron deficit in the rat. Kidney Int 54(5):1455–1462
Li C, Lin Y, Luo R, Chen S, Wang F, Zheng P, Levi M, Yang T, Wang W (2016) Intrarenal renin-angiotensin system mediates fatty acid-induced ER stress in the kidney. Am J Physiol Ren Physiol 310(5):F351–F363
Lisle SJ, Lewis RM, Petry CJ, Ozanne SE, Hales CN, Forhead AJ (2003) Effect of maternal iron restriction during pregnancy on renal morphology in the adult rat offspring. Br J Nutr 90(1):33–39
Lloyd LJ, Foster T, Rhodes P, Rhind SM, Gardner DS (2012) Protein-energy malnutrition during early gestation in sheep blunts fetal renal vascular and nephron development and compromises adult renal function. J Physiol 590(2):377–393
Lozano G, Elmaghrabi A, Salley J, Siddique K, Gattineni J, Baum M (2015) Effect of prenatal programming and postnatal rearing on glomerular filtration rate in adult rats. Am J Physiol Ren Physiol 308(5):F411–F419
Magalhaes JC, da Silveira AB, Mota DL, Paixao AD (2006) Renal function in juvenile rats subjected to prenatal malnutrition and chronic salt overload. Exp Physiol 91(3):611–619
Makrakis J, Zimanyi MA, Black MJ (2007) Retinoic acid enhances nephron endowment in rats exposed to maternal protein restriction. Pediatr Nephrol 22(11):1861–1867
Mao C, Liu R, Bo L, Chen N, Li S, Xia S, Chen J, Li D, Zhang L, Xu Z (2013) High-salt diets during pregnancy affected fetal and offspring renal renin-angiotensin system. J Endocrinol 218(1):61–73
Neiss WF, Klehn KL (1981) The postnatal development of the rat kidney, with special reference to the chemodifferentiation of the proximal tubule. Histochemistry 73(2):251–268
Nwagwu MO, Cook A, Langley-Evans SC (2000) Evidence of progressive deterioration of renal function in rats exposed to a maternal low-protein diet in utero. Br J Nutr 83(1):79–85
Painter RC, Roseboom TJ, van Montfrans GA, Bossuyt PM, Krediet RT, Osmond C, Barker DJ, Bleker OP (2005) Microalbuminuria in adults after prenatal exposure to the Dutch famine. J Am Soc Nephrol 16(1):189–194
Pereira SP, Oliveira PJ, Tavares LC, Moreno AJ, Cox LA, Nathanielsz PW, Nijland MJ (2015) Effects of moderate global maternal nutrient reduction on fetal baboon renal mitochondrial gene expression at 0.9 gestation. Am J Physiol Ren Physiol 308(11):F1217–F1228
Perng W, Gillman MW, Mantzoros CS, Oken E (2014) A prospective study of maternal prenatal weight and offspring cardiometabolic health in midchildhood. Ann Epidemiol 24(11):793–800. e791
Plank C, Ostreicher I, Hartner A, Marek I, Struwe FG, Amann K, Hilgers KF, Rascher W, Dotsch J (2006) Intrauterine growth retardation aggravates the course of acute mesangioproliferative glomerulonephritis in the rat. Kidney Int 70(11):1974–1982
Quigley R (2012) Developmental changes in renal function. Curr Opin Pediatr 24(2):184–190
Robertson LT, Trevino-Villarreal JH, Mejia P, Grondin Y, Harputlugil E, Hine C, Vargas D, Zheng H, Ozaki CK, Kristal BS, Simpson SJ, Mitchell JR (2015) Protein and calorie restriction contribute additively to protection from renal ischemia reperfusion injury partly via leptin reduction in male mice. J Nutr 145(8):1717–1727
Sahajpal V, Ashton N (2003) Renal function and angiotensin AT1 receptor expression in young rats following intrauterine exposure to a maternal low-protein diet. Clin Sci (Lond) 104(6):607–14
Sanders MW, Fazzi GE, Janssen GM, Blanco CE, De Mey JG (2005) High sodium intake increases blood pressure and alters renal function in intrauterine growth-retarded rats. Hypertension 46(1):71–75
Sharkey D, Gardner DS, Symonds ME, Budge H (2009) Maternal nutrient restriction during early fetal kidney development attenuates the renal innate inflammatory response in obese young adult offspring. Am J Physiol Ren Physiol 297(5):F1199–F1207
Sheu JN, Chen JH (2001) Minimal change nephrotic syndrome in children with intrauterine growth retardation. Am J Kidney Dis 37(5):909–914
Siddique K, Guzman GL, Gattineni J, Baum M (2014) Effect of postnatal maternal protein intake on prenatal programming of hypertension. Reprod Sci 21(12):1499–1507
Slickers JE, Olshan AF, Siega-Riz AM, Honein MA, Aylsworth AS, S. National Birth Defects Prevention (2008) Maternal body mass index and lifestyle exposures and the risk of bilateral renal agenesis or hypoplasia: the National Birth Defects Prevention Study. Am J Epidemiol 168(11):1259–1267
Sonneveld R, Ferre S, Hoenderop JG, Dijkman HB, Berden JH, Bindels RJ, Wetzels JF, van der Vlag J, Nijenhuis T (2013) Vitamin D down-regulates TRPC6 expression in podocyte injury and proteinuric glomerular disease. Am J Pathol 182(4):1196–1204
Sonneveld R, Hoenderop JG, Stavenuiter AW, Ferrantelli E, Baltissen MP, Dijkman HB, Florquin S, Rops AL, Wetzels JF, Berden JH, van der Vlag J, Nijenhuis T (2016) 1,25-vitamin D3 deficiency induces albuminuria. Am J Pathol 186(4):794–804
Stewart CP, Christian P, Schulze KJ, Leclerq SC, West KP Jr, Khatry SK (2009) Antenatal micronutrient supplementation reduces metabolic syndrome in 6- to 8-year-old children in rural Nepal. J Nutr 139(8):1575–1581
Sutherland MR, Gubhaju L, Yoder BA, Stahlman MT, Black MJ (2009) The effects of postnatal retinoic acid administration on nephron endowment in the preterm baboon kidney. Pediatr Res 65(4):397–402
Sutherland MR, Gubhaju L, Moore L, Kent AL, Dahlstrom JE, Horne RS, Hoy WE, Bertram JF, Black MJ (2011) Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J Am Soc Nephrol 22(7):1365–1374
Szeto HH, Liu S, Soong Y, Alam N, Prusky GT, Seshan SV (2016) Protection of mitochondria prevents high fat diet-induced glomerulopathy and proximal tubular injury. Kidney Int 90:997–1011
Taal HR, Geelhoed JJ, Steegers EA, Hofman A, Moll HA, Lequin M, van der Heijden AJ, Jaddoe VW (2011) Maternal smoking during pregnancy and kidney volume in the offspring: the Generation R Study. Pediatr Nephrol 26(8):1275–1283
Tomat AL, Inserra F, Veiras L, Vallone MC, Balaszczuk AM, Costa MA, Arranz C (2008) Moderate zinc restriction during fetal and postnatal growth of rats: effects on adult arterial blood pressure and kidney. Am J Phys Regul Integr Comp Phys 295(2):R543–R549
Vaidya A, Saville N, Shrestha BP, Costello AM, Manandhar DS, Osrin D (2008) Effects of antenatal multiple micronutrient supplementation on children’s weight and size at 2 years of age in Nepal: follow-up of a double-blind randomised controlled trial. Lancet 371(9611):492–499
Vikse BE, Irgens LM, Leivestad T, Hallan S, Iversen BM (2008) Low birth weight increases risk for end-stage renal disease. J Am Soc Nephrol 19(1):151–157
Wlodek ME, Mibus A, Tan A, Siebel AL, Owens JA, Moritz KM (2007) Normal lactational environment restores nephron endowment and prevents hypertension after placental restriction in the rat. J Am Soc Nephrol 18(6):1688–1696
Woods LL, Ingelfinger JR, Nyengaard JR, Rasch R (2001) Maternal protein restriction suppresses the newborn renin-angiotensin system and programs adult hypertension in rats. Pediatr Res 49(4):460–467
Woods LL, Weeks DA, Rasch R (2004) Programming of adult blood pressure by maternal protein restriction: role of nephrogenesis. Kidney Int 65(4):1339–1348
Yamada-Obara N, Yamagishi SI, Taguchi K, Kaida Y, Yokoro M, Nakayama Y, Ando R, Asanuma K, Matsui T, Ueda S, Okuda S, Fukami K (2016) Maternal exposure to high-fat and high-fructose diet evokes hypoadiponectinemia and kidney injury in rat offspring. Clin Exp Nephrol 20:853–861
Zeman FJ (1968) Effects of maternal protein restriction on the kidney of the newborn young of rats. J Nutr 94(2):111–116
Zidar N, Cavic MA, Kenda RB, Koselj M, Ferluga D (1998) Effect of intrauterine growth retardation on the clinical course and prognosis of IgA glomerulonephritis in children. Nephron 79(1):28–32
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this entry
Cite this entry
Nüsken, E., Nüsken, KD., Dötsch, J. (2019). Diet and Epigenetic Alteration of Renal Function. In: Patel, V., Preedy, V. (eds) Handbook of Nutrition, Diet, and Epigenetics. Springer, Cham. https://doi.org/10.1007/978-3-319-55530-0_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-55530-0_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55529-4
Online ISBN: 978-3-319-55530-0
eBook Packages: MedicineReference Module Medicine