Abstract
Contemporary surgical neuro-oncology traces its roots to Harvey Cushing in the study and treatment of brain tumors. Neurosurgical intervention plays a significant role in the management of brain tumors for tissue diagnosis through biopsy, and treatment through resection in most cases of isolated well-circumscribed brain tumors, often in combination with radiation therapy and chemotherapy. Neurosurgical consultation is almost always indicated for intracranial mass lesions in pediatric patients, and a general familiarity with principles of surgical management can be useful to the oncologist and radiation oncologist in providing appropriate counseling and creating a comprehensive multidisciplinary treatment plan. This chapter provides an overview of five important topics of surgical management and provides relevant clinical pearls: surgical approaches to brain tumors, hydrocephalus management, posterior fossa syndrome, steroid administration, and seizure management.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
Modern neurosurgery derives much of its origin from the pioneering work of Harvey Cushing in the study and treatment of brain tumors (Canale 1989). Today, surgical resection continues to be the first-line management in most cases of isolated well-circumscribed brain tumors, often in combination with radiation therapy and chemotherapy. Neurosurgical consultation is almost always indicated for cerebral mass lesions in pediatric patients, and a general familiarity with principles of surgical management can be useful to the oncologist and radiation oncologist in providing appropriate counseling and creating a treatment plan. This chapter provides an overview of five critical topics of surgical management: surgical approaches to brain tumors, hydrocephalus management, posterior fossa syndrome, steroid administration, and seizure management.
2 Surgical Approaches to Brain Tumors
Surgical resection remains the mainstay for definitive diagnosis and treatment for most brain tumors. A list of indications for surgery is beyond the scope of this chapter; however, tumors that are amenable to surgical resection usually fall under one of the following categories: (1) a primary brain tumor with well-defined margins; (2) a single intracerebral metastasis; (3) in the case of multiple metastases in a symptomatic patient, resection of the single metastasis that is causing symptoms; (4) a very large tumor causing mass effect amenable to debulking or complete resection; and (5) a tumor causing obstructive hydrocephalus. For tumors where surgery is not first-line treatment, an open or stereotactic biopsy may be performed to obtain tissue diagnosis. In rare circumstances, such as diffuse pontine glioma, with pathognomonic radiological findings, no surgical intervention (resection or biopsy) is necessary before proceeding with chemotherapy or radiation therapy.
Sampling cerebrospinal fluid for tumor markers, including beta-human chorionic gonadotropin and alfa-fetoprotein; tumor staging; and pathologic diagnosis from the lumbar cistern through a lumbar puncture is safe in the absence of tumor causing mass effect and obstructive hydrocephalus. Removal of cerebrospinal fluid in the setting of mass effect or hydrocephalus may precipitate a fatal herniation syndrome. Consultation with neurosurgical colleagues prior to lumbar puncture should be secured in uncertain cases of mass effect or hydrocephalus.
Most tumors in pediatric patients can be accessed and resected via one of five main types of craniotomies: pterional, suboccipital, retrosigmoid, interhemispheric, and regional craniotomies. Endonasal endoscopic or open transsphenoidal surgery may be considered in children with intrasellar and suprasellar tumors such as craniopharyngioma. The lack of aeration of the sphenoid sinus in young children remains the most important anatomic limitation to this approach. In the pediatric population, lesions affecting the skull base are rare and not necessarily treated by aggressive surgery. Because of this, skull base surgery, such as transcondylar far lateral approach, in children has not received much attention in the pediatric neurosurgical literature except by a few authors (Patel et al. 2012). A pterional craniotomy provides direct access to the middle cranial fossa, much of the anterior cranial fossa, and the lateral skull base. A skin incision is made just behind the hairline to preserve cosmesis. Common complications include transient swelling of the ipsilateral eye, atrophy of the temporalis muscle, temporalis muscle pain, and ptosis due to injury to the frontalis branch of the facial nerve. The suboccipital craniotomy provides direct access to the midline posterior fossa up to the midbrain. A dorsal midline skin incision is made near the occipital cervical junction and is mostly covered by the hairline with good cosmesis. Cerebrospinal fluid (CSF) is prone to leak from these incisions, and a known complication is the posterior fossa syndrome (discussed later in this chapter). Vertebral artery injury causing posterior circulation stroke is an uncommon but potentially devastating complication. The retrosigmoid craniotomy is used to gain access to the lateral posterior fossa and anterior pons. Portions of cranial nerves V through XII can be exposed via this approach. The retrosigmoid craniotomy is often used to resect cerebellopontine angle tumors. A common complication of this approach includes CSF leak (the air cells are usually exposed during this approach). The interhemispheric, or transcallosal craniotomy, provides access to the body to the lateral ventricles and the anterior portions of the third ventricle, including the foramen of Monroe. Common complications of this approach include injury to interhemispheric veins and “disconnection” syndromes from sectioning of the corpus callosum. Finally, various regional craniotomies (frontal, parietal, orbital, etc.) are often used to access superficial tumors. These involve small linear or S-shaped incisions, or horseshoe-shaped flaps directly over the tumor, and a craniotomy underneath. Convexity meningiomas are usually amenable to such craniotomies.
A variety of adjunctive options are available to assist the surgeon in performing an adequate resection with minimal or no postoperative neurological deficit. These include intraoperative neuro-navigation, intraoperative imaging (ultrasound and MRI), and neurophysiological monitoring.
2.1 Neuro-Navigation
Intraoperative navigation is now ubiquitous in most surgical centers. Navigation allows the surgeon to identify an anatomic point of interest during surgery (using a special pointed tip instrument) and to view the corresponding location on the patient’s preoperative MRI scan (Ng et al. 2010). This technique is useful to identify structures that must be avoided (such as a venous sinus or a large vein) or to have a sense of how much of a tumor remains to be resected (Orringer et al. 2012). Resection of a tumor often causes the brain to shift, so navigation is not completely reliable by itself for ensuring complete resection of a tumor. Another use is to assure accurate proximal placement of a shunt or Ommaya reservoir. Neuro-navigation requires a high-resolution MRI sequence called a STEALH MRI or, in the case of shunt or Ommaya placements, a STEALTH CT scan will suffice. If an MRI of the brain is ordered to work up a possible brain tumor (such as a patient with a mass lesion identified on a CT scan), it is useful to add a contrasted STEALTH sequence to the study. Doing so avoids a future trip back to the scanner for the sole purpose of obtaining the STEALTH sequence when surgery is being planned.
2.2 Intraoperative Imaging
Intraoperative ultrasound can be used once the dura is exposed, and this modality is useful for localizing the tumor when planning a durotomy and to assess for completeness of tumor resection (El Beltagy et al. 2010). In most centers, ultrasound is the only real-time intraoperative imaging available to assess for extent of tumor resection, in combination with direct visualization (Cheon 2015). Intraoperative MRI is becoming increasingly more common. There is level 2 evidence that intraoperative MRI-guided surgery is more effective than conventional neuro-navigation in increasing extent of tumor resection in glioblastoma patients (Kubben et al. 2011). Intraoperative MRI is especially helpful when dealing with an infiltrating tumor, when the margin between the tumor and normal brain is difficult to discern by direct visualization.
2.3 Intraoperative Monitoring
Finally, intraoperative neurophysiological monitoring utilizes various electrophysiological techniques to monitor the integrity of neural structures during surgery (Ng et al. 2010). Somatosensory evoked potentials can be used to localize the central sulcus (and hence to know the location of the motor strip just anterior) because a characteristic phase reversal (inversion of the N20/P20 component) occurs across the central sulcus (Cedzich et al. 1996). Motor evoked potentials can be used to monitor the integrity of the corticospinal tract during resection of motor strip tumors (Taniguchi et al. 1993). Brainstem auditory evoked potentials are often used to monitor cochlear function during surgery for a cerebellopontine angle tumor, when hearing preservation is the goal, and also to monitor patients during brainstem surgery (Yamakami et al. 2009). EMG and stimulated EMG are useful during surgery in the posterior fossa or in the cerebellopontine angle to monitor the function of various cranial nerves, especially the facial nerve (Isaacson et al. 2003).
3 Hydrocephalus Management
Hydrocephalus is defined as the excessive accumulation of CSF within the ventricles of the brain. It is among the most common complications of cerebral mass lesions. Hydrocephalus in the pediatric population always warrants neurosurgical consultation and often requires immediate treatment. Therefore, knowledge of this condition and prompt recognition are critical.
Various anatomical locations are especially susceptible to obstruction of CSF flow, including the cerebral aqueduct (only a few millimeters in diameter), the foramen of Monroe, and the arachnoid granulations. In addition, certain mass lesions can obstruct the temporal horn of the lateral ventricle, causing a “trapped temporal horn” (Chen et al. 2013) These are examples of obstructive hydrocephalus, which occurs when CSF circulation is blocked proximal to the arachnoid granulations (Oreskovic and Klarica 2011). By contrast, communicating hydrocephalus occurs when CSF absorption is blocked at the level of the arachnoid granulations. If physiologic CSF circulation is restored, hydrocephalus often resolves or at least stabilizes without the need for CSF diversion. For example, it was long known that the incidence of hydrocephalus after removal of a fourth ventricular tumor was somewhat common—about 18–40%. This frequency caused some early authors to recommend prophylactic CSF diversion in all patients who underwent surgery to resect a posterior fossa tumor (Sainte-Rose et al. 2001). A recent study, however, identified the risk factors for postoperative hydrocephalus in this population, allowing surgeons to risk-stratify preoperatively the need for CSF diversion (Table 4.1). The risk factors for developing hydrocephalus after surgery for a posterior fossa tumor include age less than 2 years, presence of transependymal edema, moderate or severe hydrocephalus, cerebral metastases, and preoperative suspicion for medulloblastoma, ependymoma, or dorsal exophytic brainstem glioma (Riva-Cambrin et al. 2009; Foreman et al. 2013). The implication of these results is that many patients who undergo resection of a posterior fossa tumor do not need prophylactic CSF diversion (such as a shunt or endoscopic third ventriculostomy [ETV]) since removal of the tumor restores physiologic CSF circulation and cures the hydrocephalus.
Prompt recognition of hydrocephalus is critical. In a nonverbal patient, the first indication is often that the parents notice lethargy, irritability, nausea, vomiting, or a seizure (Shiminski-Maher and Disabato 1994). In a patient who is able to communicate, headaches are the cardinal symptom. The headaches are worse in a recumbent position at night or on first rising in the morning and improved with sitting or standing throughout the day. Bradycardia probably results from pressure on the dorsal motor nucleus of the vagus nerve in the medulla and on the nucleus ambiguous, which contains preganglionic parasympathetic neurons whose axons travel with the vagus nerve (Siegel et al. 2015). Papilledema is a key physical finding and almost always indicates that intracranial pressure (ICP) is elevated. However, its absence does not exclude elevated ICP as papilledema can take several days to develop (Hayreh and Hayreh 1977; Steffen et al. 1996). In cases where the physical finding of papilledema is in doubt and the rest of the workup is equivocal, evaluation by an ophthalmologist may be necessary. Other physical findings of subacute/chronic hydrocephalus include distended scalp veins, upward gaze palsy from pressure on the midbrain, a bulging fontanelle, and a head circumference that crosses percentiles. In infants with an open fontanelle, the initial symptoms may be more subtle since the open fontanelle initially provides compliance against changes in ICP.
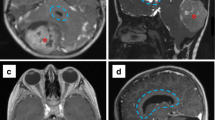
Cerebral imaging often provides the first indication of hydrocephalus in a cancer patient. On CT scans, ventriculomegaly is the obvious sign and, in acute cases, there is a distinct hypodense-blurred margin to the ventricles. The third ventricle is the most compliant; often, the first radiographic sign of increased ventricular pressure is a distended or “rounded” third ventricle. Cortical sulcal effacement may occur with large ICP elevations. T2 MRI sometimes shows hyperintense transependymal CSF flow, which is especially prominent around the ventricular horns. The corpus callosum may be thinned and stretched upward. Quantitative measures include an Evan’s ratio (ratio of the bifrontal horn diameter to the intracranial diameter) greater than 1/3 and a temporal horn width greater than 3 mm (Osborn 2013). In practice, the Evan’s ratio is more useful for trending ventricle size rather than diagnosing hydrocephalus since the diagnosis is usually apparent from other radiographic features.
Procedures for treating hydrocephalus are among the most established in the field of neurosurgery. They include the external ventricular drain (EVD or “ventriculostomy”), ETV, and shunts. The most rapid method for treating obstructive hydrocephalus is an EVD. This procedure can be done in the operating room or (in emergency circumstances) at the bedside with local anesthesia. It utilizes a frontal approach to target drain placement near the foramen of Monroe. The distal tip of the ventricular drain is tunneled under and out through the skin and connected to a reservoir to collect CSF through the siphon effect of gravity. CSF is drained either by pressure (0–20 cm above the ear of the patient) or by volume (a fixed volume of 10–15 cc per hour). Under or over drainage of CSF should be avoided. The EVD is an ideal choice in several scenarios: acute hydrocephalus to temporize the patient pending operating room availability or pending operative planning for complex tumors, when hydrocephalus is known to be due to a cause that will soon be reversed (such as a fourth ventricle obstructive tumor), or when diagnostic ICP readings are necessary if the diagnosis of hydrocephalus is unclear but strongly suspected (lumbar puncture opening pressure is not a reliable indicator of ICP in noncommunicating hydrocephalus and may precipitate life-threatening herniation).
Long-term treatments for hydrocephalus are the ETV and ventricular shunts. ETV involves endoscopic navigation via a cranial burr hole to the floor of the third ventricle and fenestration of the third ventricle through the tuber cinerium. This provides an alternate route of egress, as CSF can flow directly from the third ventricle to the pre-pontine cistern after this procedure is performed. The complications of an ETV are primarily periprocedural. Visual obscuration of the endoscopic camera can be caused by even a slight amount of intraventricular blood. Coagulating the bleeding vessel is difficult through a single channel endoscope. Damage to the fornices may occur with devastating clinical outcomes, including the loss of short- and long-term memory. Hypothalamic damage can manifest as diabetes insipidus, amenorrhea, change in appetite, growth hormone disturbance, hypothyroidism, loss of thirst, electrolyte abnormalities, or other components of hypothalamic-pituitary axis disruption (Bouras and Sgouros 2011). Damage to the basilar artery, which has a variable location in relation to the floor of the third ventricle and is sometimes difficult to visualize at the time of puncture, can be fatal. Postoperative complications include CSF leak (3.1%), meningitis (2.3%), hemorrhage (1.7%), subdural CSF collection (1.7%), and seizure (1%) (Sacko et al. 2010). Furthermore, an ETV may obstruct at any time, but the majority of failures occur within the first 6 months after surgery; in patients with aqueductal stenosis or tumors, there may be a second “peak” of failures 3 years after surgery (Lam et al. 2014).
Ventricular shunts are among the most well-established procedures in the field of neurosurgery. They usually utilize either a frontal or occipital entry point to target the lateral ventricle. A peritoneal termination is usually favored (ventriculoperitoneal shunt) with enough catheter length coiled in the abdominal cavity to account for the child’s growth, but other sites can be used, including the heart (ventriculoatrial shunt), lung (ventriculopleural shunt), or gallbladder (least commonly used). Non-peritoneal sites are usually used after several prior peritoneal insertions have been performed, after which peritoneal adhesions will develop. CSF diversion from the lumbar spine to the peritoneum (lumboperitoneal shunt) is also an option in patients with communicating hydrocephalus. Shunts carry a high risk of failure. In a study of new shunts placed in pediatric patients, there was a 40% risk of failure in 1 year and a 50% risk of failure in 2 years. Overall, there is a 5% risk of failure per year. Obstruction (31%) and infection (8%) are the most common causes of failure, but after 6 months, the infection risk is miniscule (Drake et al. 1998). Compared to endoscopic techniques, shunts have a low upfront cost, but the cost increases over time. Retrospective data showed that 42% of shunt procedures are shunt revisions. Of the $100 million spent on caring for shunt patients each year, about half is spent on revisions (Bondurant and Jimenez 1995). Shunts also carry a significant risk of seeding tumor at the distal site; a recent meta-analysis showed that 27% of cases of primary brain tumors in children that metastasized were related to shunt placement, with germ cell tumors being the most common shunt-related metastasis (Rickert 2003). Due to the major complications associated with shunt placement in patients with brain tumors, the decision to commit a patient to a shunt requires careful consideration. If a shunt is placed, programmable valves susceptible to the effects of the strong magnetic field in an MRI scanner should be avoided, as patients with brain tumors usually require serial MRIs into the foreseeable future. If a programmable shunt valve is used, patients need a skull X-ray (orthogonal to the shunt valve such that its setting can be determined) before and after each MRI to ensure that the valve settings was not inadvertently changed by the strong magnetic waves.
When endoscopic capabilities are available to a neurosurgeon, the decision of whether to perform an ETV or shunt can be aided by the ETV success score (Table 4.2) (Kulkarni et al. 2009). The ETV success score assigns a higher likelihood of ETV success by 6 months for older children, children with brain tumors (especially tumors causing aqueductal stenosis), and patients with no previous shunt. Since an ETV is often technically difficult in newborns and infants, a practical derivation of the ETV success score is that for a child 6 months or older with tumor-related hydrocephalus, an ETV would be expected to have at least 50% success rate by 6 months. Because placing a shunt commits a patient to a high near-term risk of infection and an unremitting risk of obstruction, some practitioners tend to give patients a trial of an ETV before resorting to a shunt. The role of ETV in the management of hydrocephalus is actively being studied. As technological advancements arrive (including flexible endoscopes capable of entering the temporal horns, which will allow near full coagulation of the CSF-producing choroid plexus), ETV will gain a greater role in treating hydrocephalus. A recent study showed that when ETV is combined with partial choroid plexus cauterization, the 6-month success rate is improved from 45% expected from the ETV success score to 59% (Stone and Warf 2014).
Rapid recognition of ETV failure or shunt failure is critical, and if there is any concern for failure, a neurosurgeon must be consulted. The radiographic finding of newly enlarged ventricles in a patient with a shunt or ETV indicates failure; no other workup is necessary. However, many times comparison CT scans are not available or the CT scan is equivocal for ventricular dilatation. Also, patients with shunt failure do not always have dilated ventricles (Sellin et al. 2014). In such cases, one must rely on the clinical history and physical exam to diagnose the failure, or a shunt tap of the reservoir. If an ETV was performed, a CINE MRI scan of the brain can be performed to evaluate for flow through the fenestration in the floor of the third ventricle.
In the uncommon case that a patient presents with acute hydrocephalus due to distal shunt failure (usually symptoms of distal failure are more indolent), a shunt tap to remove CSF may be lifesaving. When distal failure of a ventriculoperitoneal shunt is suspected, an abdominal CT is often performed to check for a pseudocyst, infection, or very uncommonly tumor seeding at distal end of the shunt. In cases of symptomatic shunt obstruction, the only definitive treatment is emergent shunt revision or temporization with an EVD.
4 Posterior Fossa Syndrome
In 1985, Rekate reported several cases of mutism in children after posterior fossa surgery (Rekate et al. 1985). Since then, there have been many reports of mutism following surgery for cerebellar tumors. The posterior fossa syndrome (PFS) includes various specific linguistic, cognitive, and behavioral symptoms that occur after surgery for lesions of the cerebellum. Symptoms typically develop a few days after an otherwise normal postoperative course after resection of a posterior fossa tumor in a child (Wells et al. 2008). (PFS has been reported in adults, but it is uncommon (Marien et al. 2013)) The hallmark symptom of PFS is mutism (“cerebellar mutism”), which is often accompanied by frontal-like behavioral symptoms such as abulia, apathy, or lack of concern (Levisohn et al. 2000). After remission of the mutism, patients continue to be dysarthric; speech is present but impaired by motor difficulty, and this rarely normalizes (Wells et al. 2008). Hence, PFS is sometimes called “mutism and subsequent dysarthria syndrome.” Importantly, there are no long tract signs and no supranuclear or cranial nerve palsies (Wells et al. 2008). The presenting symptoms are usually transient and resolve with time, but long-term adverse sequela may include decline of general intelligence and scholarly underachievement (Steinlin et al. 2003; De Smet et al. 2009). PFS was initially reported as “rare,” but a recent prospective series of patients undergoing medulloblastoma resection reported an incidence of 24% (Robertson et al. 2006).
The pathophysiology behind PFS has not yet been determined. Two main hypotheses, which are not mutually exclusive, have been advanced to explain the symptoms of PFS: interruption of the dentatothalamocortical pathway due to bilateral damage to the dentate nuclei and cerebellar swelling.
4.1 Interruption of the Dentatothalamocortical Pathway as a Possible Cause of PFS
The dentatothalamocortical pathway is the primary outflow tract from the cerebellum. It originates at the dentate nucleus, sends projections through the ipsilateral superior cerebellar peduncle, decussates in the midbrain tegmentum, and synapses in the contralateral ventrolateral thalamus. There, synapses occur with second order neurons that project to the supplementary motor area (Kandel 2013). Myelination is incomplete in children, and this may lead to greater susceptibility to disturbances of this pathway in younger patients (Ildan et al. 2002). Crutchfield observed that lesions along this pathway lead to mutism (Crutchfield et al. 1994): Mutism has been reported after stereotactic lesioning of both dentate nuclei for treatment of a dyskinetic syndrome (Fraioli and Guidetti 1975). Mutism has been reported after bilateral thalamotomy for Parkinson’s disease (Siegfried et al. 1970). Finally, lesions of the supplemental motor area can also cause mutism (Crutchfield et al. 1994). MRI studies of patients with PFS often show evidence of proximal injury along this pathway (Morris et al. 2009). In fact, a recent anatomical study demonstrated in cadavers the high susceptibility of the dentate nuclei to damage during various posterior fossa surgical approaches (Akakin et al. 2014). Sagging of the cerebellum into a postsurgical resection cavity may cause distortions of these tracts as well, exacerbating injury. Crutchfield observed that when lesions occur in this pathway, symptomatic recovery (when it occurs) is usually quite sudden—from mutism to the immediate return of words and sentences (Crutchfield et al. 1994). From this clinical observation, the authors hypothesized that lesions along this pathway cause an inhibition of cortical language centers, and recovery reverses the inhibition. It is possible that the dentatothalamocortical pathway contributes a permissive input to cortical language circuitry that, when restored, allows rapid recuperation of linguistic ability.
4.2 Cerebellar Swelling as a Possible Cause of PFS
Ferrante proposed that postoperative vasospasm of cerebellar arteries could cause ischemia and subsequent cerebellar swelling and edema (Ferrante et al. 1990). To date, there have been no clinical studies of cerebral angiography after posterior fossa surgery to evaluate for vasospasm. SPECT studies have shown hypoperfusion of the left cerebellar hemisphere in a patient with PFS, and the abnormality resolved together with the mutism (Clerico et al. 2002; Ersahin et al. 1996). A recent series also showed that 92% of patients with PFS had postoperative cerebellar edema, and the edema often affected the middle and superior cerebellar peduncle (Wells et al. 2010). The same study showed that patients who developed PFS often had tumors that invaded into the brainstem. It is conceivable that the cerebellar swelling may result from retraction and other manipulations during surgery and not necessarily from vasospasm.
Splitting of the vermis, especially the inferior part, has been suggested to cause PFS (Dailey et al. 1995). In fact, the telovelar approach for resecting posterior fossa tumors was developed specifically to avoid splitting the vermis (Mussi and Rhoton 2000). However, this association between splitting the vermis and PFS is questioned by some modern authors (Pitsika and Tsitouras 2013). Robertson showed no correlation between vermis tumor location and the development of PFS (Robertson et al. 2006). They noted that the majority of patients with posterior fossa tumors underwent radical resection through the vermis and did not develop mutism afterward. Hydrocephalus had, at one time, been proposed as the cause of PFS (Ferrante et al. 1990). However, later studies showed no association between hydrocephalus and PFS (Crutchfield et al. 1994; Catsman-Berrevoets and Aarsen 2010).
5 Mass Effect/Intracranial Pressure Management
Several temporizing measures can be employed to treat tumor-related mass effect and the associated increase in ICP, pending definitive treatment. The head of the bed should be elevated to 30–45°. This reduces ICP by enhancing venous outflow but, at the same time, slightly diminishes MAP and cerebral perfusion pressure. The head should face straightforward (not turned to one side)—this also enhances venous drainage. The first-line pharmacological agent for the non-emergent treatment of tumor-associated mass effect is steroids, usually dexamethasone (discussed later in this chapter). Hyperventilation lowers ICP by reducing the partial pressure of CO2, which, by various physiologic mechanisms, reduces cerebral blood volume. Hyperventilation can be used for brief periods of time with a pCO2 goal of 30–35 but should not be used for long-term treatment of elevated ICP, as it places patients at risk for cerebral ischemia. The mechanism by which mannitol lowers ICP is controversial, but it may involve improved rheology (plasma expansion reduces the hematocrit, which increases cerebral blood outflow) (Burke et al. 1981). Diuresis and osmotic effects are more delayed and take 15–30 min for onset. In urgent situations, 1 g/kg of mannitol can be given intravenously over 30 min. Hypertonic saline also has an osmotic effect, and 3% saline is often given therapeutically through a central line with serum sodium checks performed every 6 h to maintain sodium levels of 145–155.
6 Steroids
Glucocorticoids are a well-established treatment for tumor-associated edema. They are frequently used in the following scenarios: (1) to temporize a patient who has a surgically resectable brain tumor while the definitive resection is being planned; (2) to reduce swelling in the perioperative period (after the operation, the dose is tapered down); (3) in combination with certain chemotherapy regimens to reduce edema during administration of the therapeutic agent; (4) to minimize swelling during radiation therapy; and (5) to palliate swelling in the setting of an inoperable brain tumor. Clinically, a response is usually seen within a few hours (because the pharmacologic action of steroids modifies DNA transcription (Ratman et al. 2013)). Thus, steroids are not the first-line agent for a tumor-associated ICP crisis (Alberti et al. 1978). Dexamethasone is the most commonly used glucocorticoid for treating tumor-associated cerebral edema, as its low level of mineralocorticoid activity reduces the potential for fluid retention (Galicich et al. 1961). Dexamethasone may also have a lower risk of infection and cognitive impairment compared to other steroids (Batchelor and DeAngelis 1996). Steroids are effective in treating vasogenic edema, which occurs due to disruption of the blood–brain barrier (Bebawy 2012). In contradistinction, they are not effective in treating cytotoxic edema, which occurs due to cellular swelling (such as the edema that occurs after a stroke).
Steroids are associated with a number of common complications, which usually occur after chronic use. These are three of the most important complications that are of particular concern: peptic ulcers, steroid myopathy, and adrenal insufficiency (Addison’s disease). Peptic ulceration is a well-known complication of steroids, and this is magnified by the intrinsic risk of ulceration posed by a brain tumor (“Cushing’s ulcer”). Gastrointestinal prophylaxis, usually by way of a proton pump inhibitor, is the standard of care whenever steroids are administered. Patients affected by steroid myopathy typically develop proximal muscle weakness between the ninth and twelfth weeks of glucocorticoid treatment, with no muscle pain and normal reflexes (Pereira and Freire de Carvalho 2011). Withdrawal or lowering the steroid dose is the treatment, although it is not always possible, and doing so is not always effective in symptom amelioration. Glucocorticoids suppress the HPA axis, and this can lead to secondary adrenal insufficiency, which can manifest as life-threatening hypotension (Krasner 1999). Among brain tumor patients treated with glucocorticoids, 1% will develop secondary adrenal insufficiency (Da Silva and Schiff 2007). Symptoms of adrenal insufficiency (e.g., somnolence, nausea and vomiting, confusion, delirium, abulia, and coma) are prone to manifest during tapering (Gordijn et al. 2012) and are often incorrectly attributed to mass effect. Therefore, a high index of suspicion is necessary, and an ACTH stimulation test should be considered when such symptoms are encountered during glucocorticoid tapering.
7 Seizure Management
Anywhere from 30 to 50% of patients with a brain tumor will present initially with a seizure (Perucca 2013). Commonly used antiepileptic medications in children include levetiracetam (Keppra), phenytoin (Dilantin), valproate (Depakote), phenobarbital, carbamazepine (Tegretol), lamotrigine (Lamictal), felbamate (Felbatol), pregabalin (Lyrica), and topiramate (Topomax). The choice of which to use as a long-term first-line agent usually depends on the side effect profile. Evaluation by a pediatric neurologist is advised for all patients who have had a seizure to determine an appropriate antiepileptic regimen.
In the setting of an active seizure, the immediate goal is to stabilize the patient and then seek evaluation by a pediatric neurologist for long-term antiepileptic management. A representative protocol for seizure management is shown in Table 4.3 (Greenberg 2010). When a patient has sustained seizure activity that does not resolve spontaneously, the first-line agent to administer is a benzodiazepine. Several doses of lorazepam (Ativan) can be used in an attempt to break the seizure. Intravenous loading doses of Keppra and/or Dilantin can be then given. If these measures fail, then the next course of action would be an intravenous sedative drip (versed or propofol for example), which will require intubation (Treatment of convulsive status epilepticus. Recommendations of the Epilepsy Foundation of America’s Working Group on Status Epilepticus 1993; Sirven and Waterhouse 2003). Even if a sedative drip is not used, the airway should always be monitored closely; sometimes, intubation becomes necessary due to the combined effects of benzodiazepines and mental alteration impairing protection of the airway.
The perioperative prophylactic use of antiepileptic agents in a patient with a brain tumor who has never had a seizure is controversial. The use of prophylactic antiepileptic agents is well established in the setting of head trauma (Temkin et al. 1990), but the “trauma” that occurs in the surgical resection of brain tumors is different in that it occurs in a controlled environment and locally around the tumor. Conclusions from the trauma literature, therefore, do not generalize to patients with brain tumors. A prospective single-institution randomized trial of 123 adult postsurgical primary brain tumor patients compared seizure-free survival in patients who received either prophylactic phenytoin or no prophylaxis (Wu et al. 2013). However, the trial was terminated because the incidence of clinically significant early seizures was so similar between the arms (3% in the observation group versus 2% in the prophylaxis group) that it was deemed unlikely that a significant difference would ever be found. Nonetheless, the prophylaxis group did experience significantly higher adverse events (18% versus 0%, p < 0.01). Another randomized trial of prophylactic antiepileptic agents in 100 adult brain tumor patients (39 of whom had surgery) was also terminated early due to no statistically significant differences in seizure incidence (28% in the observation group versus 24% in the prophylaxis group) (Forsyth et al. 2003). These were trials in adults, and no trials exist in pediatric patients. It remains to be seen whether patients with tumors in certain high-risk locations, such as the temporal lobe, would benefit from perioperative seizure prophylaxis. In practice, there tends to be a very low threshold for starting antiepileptic agents in pediatric patients who have tumors in high-risk locations in whom there is a suspicion for a seizure. Among adult patients with astrocytomas who presented with preoperative seizures, 77% were seizure-free, and 95% had meaningful improvement in seizure control, a year after surgery (Chaichana et al. 2009). The implication is that the actual removal of the tumor itself may be the most important factor in providing long-term seizure control.
References
Akakin A, Peris-Celda M, Kilic T, Seker A, Gutierrez-Martin A, Rhoton A Jr (2014) The dentate nucleus and its projection system in the human cerebellum: the dentate nucleus microsurgical anatomical study. Neurosurgery 74(4):401–424.; discussion 424–405. doi:10.1227/NEU.0000000000000293
Alberti E, Hartmann A, Schutz HJ, Schreckenberger F (1978) The effect of large doses of dexamethasone on the cerebrospinal fluid pressure in patients with supratentorial tumors. J Neurol 217(3):173–181
Batchelor T, DeAngelis LM (1996) Medical management of cerebral metastases. Neurosurg Clin N Am 7(3):435–446
Bebawy JF (2012) Perioperative steroids for peritumoral intracranial edema: a review of mechanisms, efficacy, and side effects. J Neurosurg Anesthesiol 24(3):173–177. doi:10.1097/ANA.0b013e3182578bb5
Bondurant CP, Jimenez DF (1995) Epidemiology of cerebrospinal fluid shunting. Pediatr Neurosurg 23(5):254–258. discussion 259
Bouras T, Sgouros S (2011) Complications of endoscopic third ventriculostomy. J Neurosurg Pediatr 7(6):643–649. doi:10.3171/2011.4.PEDS10503
Burke AM, Quest DO, Chien S, Cerri C (1981) The effects of mannitol on blood viscosity. J Neurosurg 55(4):550–553. doi:10.3171/jns.1981.55.4.0550
Canale DJ (1989) William Osler and “the special field of neurological surgery”. J Neurosurg 70(5):759–766. doi:10.3171/jns.1989.70.5.0759
Catsman-Berrevoets CE, Aarsen FK (2010) The spectrum of neurobehavioural deficits in the Posterior Fossa Syndrome in children after cerebellar tumour surgery. Cortex 46(7):933–946. doi:10.1016/j.cortex.2009.10.007. S0010-9452(09)00282-2 [pii]
Cedzich C, Taniguchi M, Schafer S, Schramm J (1996) Somatosensory evoked potential phase reversal and direct motor cortex stimulation during surgery in and around the central region. Neurosurgery 38(5):962–970
Chaichana KL, Parker SL, Olivi A, Quinones-Hinojosa A (2009) Long-term seizure outcomes in adult patients undergoing primary resection of malignant brain astrocytomas. Clinical article. J Neurosurg 111(2):282–292. doi:10.3171/2009.2.JNS081132
Chen CC, Kasper EM, Zinn PO, Warnke PC (2013) Management of entrapped temporal horn by temporal horn to prepontine cistern shunting. World Neurosurg 79(2):404.e7–404.10. doi:10.1016/j.wneu.2011.02.025. S1878-8750(11)00144-6 [pii]
Cheon JE (2015) Intraoperative neurosonography revisited: effective neuronavigation in pediatric neurosurgery. Ultrasonography 34(2):79–87. doi:10.14366/usg.14054. usg.14054 [pii]
Clerico A, Sordi A, Ragni G, Festa A, Cappelli C, Maini CL (2002) Brief report: transient mutism following posterior fossa surgery studied by single photon emission computed tomography (SPECT). Med Pediatr Oncol 38(6):445–448. doi:10.1002/mpo.1361
Crutchfield JS, Sawaya R, Meyers CA, Moore BD III (1994) Postoperative mutism in neurosurgery. Report of two cases. J Neurosurg 81(1):115–121. doi:10.3171/jns.1994.81.1.0115
Da Silva AN, Schiff D (2007) Adrenal insufficiency secondary to glucocorticoid withdrawal in patients with brain tumor. Surg Neurol 67(5):508–510. doi:10.1016/j.surneu.2006.07.018. S0090-3019(06)00770-1 [pii]
Dailey AT, GM MK II, Berger MS (1995) The pathophysiology of oral pharyngeal apraxia and mutism following posterior fossa tumor resection in children. J Neurosurg 83(3):467–475. doi:10.3171/jns.1995.83.3.0467
De Smet HJ, Baillieux H, Wackenier P, De Praeter M, Engelborghs S, Paquier PF, De Deyn PP, Marien P (2009) Long-term cognitive deficits following posterior fossa tumor resection: a neuropsychological and functional neuroimaging follow-up study. Neuropsychology 23(6):694–704. doi:10.1037/a0016106. 2009-20255-002 [pii]
Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J Jr, Haines S, Schiff SJ, Cochrane DD, Steinbok P, MacNeil N (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43(2):294–303. discussion 303–295
El Beltagy MA, Aggag M, Kamal M (2010) Role of intraoperative ultrasound in resection of pediatric brain tumors. Childs Nerv Syst 26(9):1189–1193. doi:10.1007/s00381-010-1091-4
Ersahin Y, Mutluer S, Cagli S, Duman Y (1996) Cerebellar mutism: report of seven cases and review of the literature. Neurosurgery 38(1):60–65. discussion 66
Ferrante L, Mastronardi L, Acqui M, Fortuna A (1990) Mutism after posterior fossa surgery in children. Report of three cases. J Neurosurg 72(6):959–963. doi:10.3171/jns.1990.72.6.0959
Foreman P, III MCS, Naftel R, Griessenauer CJ, Ditty BJ, Agee BS, Riva-Cambrin J, Wellons J III (2013) Validation and modification of a predictive model of postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 12(3):220–226. doi:10.3171/2013.5.PEDS1371
Forsyth PA, Weaver S, Fulton D, Brasher PM, Sutherland G, Stewart D, Hagen NA, Barnes P, Cairncross JG, DeAngelis LM (2003) Prophylactic anticonvulsants in patients with brain tumour. Can J Neurol Sci 30(2):106–112
Fraioli B, Guidetti (1975) Effects of stereotactic lesions of the dentate nucleus of the cerebellum in man. Appl Neurophysiol 38(2):81–90
Galicich JH, French LA, Melby JC (1961) Use of dexamethasone in treatment of cerebral edema associated with brain tumors. J Lancet 81:46–53
Gordijn MS, Gemke RJ, van Dalen EC, Rotteveel J, Kaspers GJ (2012) Hypothalamic-pituitary-adrenal (HPA) axis suppression after treatment with glucocorticoid therapy for childhood acute lymphoblastic leukaemia. Cochrane Database Syst Rev 5:CD008727. doi:10.1002/14651858.CD008727.pub2
Greenberg MS (2010) Handbook of neurosurgery, 7th edn. Greenberg Graphics, Tampa, FL
Hayreh MS, Hayreh SS (1977) Optic disc edema in raised intracranial pressure. I. Evolution and resolution. Arch Ophthalmol 95(7):1237–1244
Ildan F, Tuna M, Erman T, Gocer AI, Zeren M, Cetinalp E (2002) The evaluation and comparison of cerebellar mutism in children and adults after posterior fossa surgery: report of two adult cases and review of the literature. Acta Neurochir 144(5):463–473. doi:10.1007/s007010200067
Isaacson B, Kileny PR, El-Kashlan H, Gadre AK (2003) Intraoperative monitoring and facial nerve outcomes after vestibular schwannoma resection. Otol Neurotol 24(5):812–817
Kandel ER (2013) Principles of neural science, 5th edn. McGraw-Hill, New York
Krasner AS (1999) Glucocorticoid-induced adrenal insufficiency. JAMA 282(7):671–676. jgn90000 [pii]
Kubben PL, ter Meulen KJ, Schijns OE, ter Laak-Poort MP, van Overbeeke JJ, van Santbrink H (2011) Intraoperative MRI-guided resection of glioblastoma multiforme: a systematic review. Lancet Oncol 12(11):1062–1070. doi:10.1016/S1470-2045(11)70130-9. S1470-2045(11)70130-9 [pii]
Kulkarni AV, Drake JM, Mallucci CL, Sgouros S, Roth J, Constantini S (2009) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus. J Pediatr 155(2):254–259.e251. doi:10.1016/j.jpeds.2009.02.048. S0022-3476(09)00207-8 [pii]
Lam S, Harris D, Rocque BG, Ham SA (2014) Pediatric endoscopic third ventriculostomy: a population-based study. J Neurosurg Pediatr 14(5):455–464. doi:10.3171/2014.8.PEDS13680
Levisohn L, Cronin-Golomb A, Schmahmann JD (2000) Neuropsychological consequences of cerebellar tumour resection in children: cerebellar cognitive affective syndrome in a paediatric population. Brain 123(Pt 5):1041–1050
Marien P, De Smet HJ, Wijgerde E, Verhoeven J, Crols R, De Deyn PP (2013) Posterior fossa syndrome in adults: a new case and comprehensive survey of the literature. Cortex 49(1):284–300. doi:10.1016/j.cortex.2011.06.018. S0010-9452(11)00206-1 [pii]
Morris EB, Phillips NS, Laningham FH, Patay Z, Gajjar A, Wallace D, Boop F, Sanford R, Ness KK, Ogg RJ (2009) Proximal dentatothalamocortical tract involvement in posterior fossa syndrome. Brain 132(Pt 11):3087–3095. doi:10.1093/brain/awp241. awp241 [pii]
Mussi AC, Rhoton AL Jr (2000) Telovelar approach to the fourth ventricle: microsurgical anatomy. J Neurosurg 92(5):812–823. doi:10.3171/jns.2000.92.5.0812
Ng WH, Mukhida K, Rutka JT (2010) Image guidance and neuromonitoring in neurosurgery. Childs Nerv Syst 26(4):491–502. doi:10.1007/s00381-010-1083-4
Oreskovic D, Klarica M (2011) Development of hydrocephalus and classical hypothesis of cerebrospinal fluid hydrodynamics: facts and illusions. Prog Neurobiol 94(3):238–258. doi:10.1016/j.pneurobio.2011.05.005. S0301-0082(11)00076-1 [pii]
Orringer DA, Golby A, Jolesz F (2012) Neuronavigation in the surgical management of brain tumors: current and future trends. Expert Rev Med Devices 9(5):491–500. doi:10.1586/erd.12.42
Osborn AG (2013) Osborn’s brain: imaging, pathology, and anatomy, 1st edn. Amirsys Publishing, Salt Lake City, UT
Patel AJ, Gressot LV, Cherian J, Desai SK, Jea A (2012) Far lateral paracondylar versus transcondylar approach in the pediatric age group: CT morphometric analysis. J Clin Neurosci 21(12):2194–2200. doi:10.1016/j.jocn.2014.05.022
Pereira RM, Freire de Carvalho J (2011) Glucocorticoid-induced myopathy. Joint Bone Spine 78(1):41–44. doi:10.1016/j.jbspin.2010.02.025. S1297-319X(10)00089-8 [pii]
Perucca E (2013) Optimizing antiepileptic drug treatment in tumoral epilepsy. Epilepsia 54(Suppl 9):97–104. doi:10.1111/epi.12452
Pitsika M, Tsitouras V (2013) Cerebellar mutism. J Neurosurg Pediatr 12(6):604–614. doi:10.3171/2013.8.PEDS13168
Ratman D, Vanden Berghe W, Dejager L, Libert C, Tavernier J, Beck IM, De Bosscher K (2013) How glucocorticoid receptors modulate the activity of other transcription factors: a scope beyond tethering. Mol Cell Endocrinol 380(1–2):41–54. doi:10.1016/j.mce.2012.12.014. S0303-7207(12)00538-2 [pii]
Rekate HL, Grubb RL, Aram DM, Hahn JF, Ratcheson RA (1985) Muteness of cerebellar origin. Arch Neurol 42(7):697–698
Rickert CH (2003) Extraneural metastases of paediatric brain tumours. Acta Neuropathol 105(4):309–327. doi:10.1007/s00401-002-0666-x
Riva-Cambrin J, Detsky AS, Lamberti-Pasculli M, Sargent MA, Armstrong D, Moineddin R, Cochrane DD, Drake JM (2009) Predicting postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 3(5):378–385. doi:10.3171/2009.1.PEDS08298
Robertson PL, Muraszko KM, Holmes EJ, Sposto R, Packer RJ, Gajjar A, Dias MS, Allen JC (2006) Incidence and severity of postoperative cerebellar mutism syndrome in children with medulloblastoma: a prospective study by the Children’s Oncology Group. J Neurosurg 105(6 Suppl):444–451. doi:10.3171/ped.2006.105.6.444
Sacko O, Boetto S, Lauwers-Cances V, Dupuy M, Roux FE (2010) Endoscopic third ventriculostomy: outcome analysis in 368 procedures. J Neurosurg Pediatr 5(1):68–74. doi:10.3171/2009.8.PEDS08108
Sainte-Rose C, Cinalli G, Roux FE, Maixner R, Chumas PD, Mansour M, Carpentier A, Bourgeois M, Zerah M, Pierre-Kahn A, Renier D (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95(5):791–797. doi:10.3171/jns.2001.95.5.0791
Sellin JN, Cherian J, Barry JM, Ryan SL, Luerssen TG, Jea A (2014) Utility of computed tomography or magnetic resonance imaging evaluation of ventricular morphology in suspected cerebrospinal fluid shunt malfunction. J Neurosurg Pediatr 14(2):160–166. doi:10.3171/2014.4.PEDS13451
Shiminski-Maher T, Disabato J (1994) Current trends in the diagnosis and management of hydrocephalus in children. J Pediatr Nurs 9(2):74–82
Siegel A, Sapru HN, Siegel H (2015) Essential neuroscience, 3rd edn. Wolters Kluwer Health, Philadelphia, PA
Siegfried J, Esslen E, Gretener U, Ketz E, Perret E (1970) Functional anatomy of the dentate nucleus in the light of stereotaxic operations. Confin Neurol 32(1):1–10
Sirven JI, Waterhouse E (2003) Management of status epilepticus. Am Fam Physician 68(3):469–476
Steffen H, Eifert B, Aschoff A, Kolling GH, Volcker HE (1996) The diagnostic value of optic disc evaluation in acute elevated intracranial pressure. Ophthalmology 103(8):1229–1232
Steinlin M, Imfeld S, Zulauf P, Boltshauser E, Lovblad KO, Ridolfi Luthy A, Perrig W, Kaufmann F (2003) Neuropsychological long-term sequelae after posterior fossa tumour resection during childhood. Brain 126(Pt 9):1998–2008. doi:10.1093/brain/awg195. awg195 [pii]
Stone SS, Warf BC (2014) Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment for infant hydrocephalus: a prospective North American series. J Neurosurg Pediatr 14(5):439–446. doi:10.3171/2014.7.PEDS14152
Taniguchi M, Cedzich C, Schramm J (1993) Modification of cortical stimulation for motor evoked potentials under general anesthesia: technical description. Neurosurgery 32(2):219–226
Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR (1990) A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med 323(8):497–502. doi:10.1056/NEJM199008233230801
Treatment of convulsive status epilepticus. (1993) Recommendations of the Epilepsy Foundation of America’s Working Group on Status Epilepticus JAMA 270(7):854–9
Wells EM, Walsh KS, Khademian ZP, Keating RF, Packer RJ (2008) The cerebellar mutism syndrome and its relation to cerebellar cognitive function and the cerebellar cognitive affective disorder. Dev Disabil Res Rev 14(3):221–228. doi:10.1002/ddrr.25
Wells EM, Khademian ZP, Walsh KS, Vezina G, Sposto R, Keating RF, Packer RJ (2010) Postoperative cerebellar mutism syndrome following treatment of medulloblastoma: neuroradiographic features and origin. J Neurosurg Pediatr 5(4):329–334. doi:10.3171/2009.11.PEDS09131
Wu AS, Trinh VT, Suki D, Graham S, Forman A, Weinberg JS, McCutcheon IE, Prabhu SS, Heimberger AB, Sawaya R, Wang X, Qiao W, Hess KR, Lang FF (2013) A prospective randomized trial of perioperative seizure prophylaxis in patients with intraparenchymal brain tumors. J Neurosurg 118(4):873–883. doi:10.3171/2012.12.JNS111970
Yamakami I, Yoshinori H, Saeki N, Wada M, Oka N (2009) Hearing preservation and intraoperative auditory brainstem response and cochlear nerve compound action potential monitoring in the removal of small acoustic neurinoma via the retrosigmoid approach. J Neurol Neurosurg Psychiatry 80(2):218–227. doi:10.1136/jnnp.2008.156919
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Momin, E.N., Khan, M., Jea, A. (2018). Surgical Principles in the Treatment of Pediatric Brain Tumors. In: Mahajan, A., Paulino, A. (eds) Radiation Oncology for Pediatric CNS Tumors. Springer, Cham. https://doi.org/10.1007/978-3-319-55430-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-55430-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55428-0
Online ISBN: 978-3-319-55430-3
eBook Packages: MedicineMedicine (R0)