Abstract
Previous chapters of this book have discussed the importance of subgingival microbial colonization and of the inflammatory-immune response as triggers of periodontal tissue breakdown. In fact, it appears clear that periodontal health or pathology is the result of the interaction between the human host and its invading microbes. Or perhaps we should not define them as ‘invading’, since it is well known that microbes not only coexist with their human host, but also provide multiple vital functions for the survival of the host itself [1]. Compelling evidence has now emerged to suggest that host genetic variants have a fundamental effect in regulating the host’s relationships with the microbial ‘guests’ and a better knowledge of how these effects are implemented is crucial in the understanding of disease processes. This chapter will review the evidence on the effect of host genetic factors on periodontal microbial colonization and will provide examples of how this could have an impact in clinical practice.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
7.1 Introduction
Previous chapters of this book have discussed the importance of subgingival microbial colonization and of the inflammatory-immune response as triggers of periodontal tissue breakdown. In fact, it appears clear that periodontal health or pathology is the result of the interaction between the human host and its invading microbes. Or perhaps we should not define them as ‘invading’, since it is well known that microbes not only coexist with their human host, but also provide multiple vital functions for the survival of the host itself [1]. Compelling evidence has now emerged to suggest that host genetic variants have a fundamental effect in regulating the host’s relationships with the microbial ‘guests’ and a better knowledge of how these effects are implemented is crucial in the understanding of disease processes. This chapter will review the evidence on the effect of host genetic factors on periodontal microbial colonization and will provide examples of how this could have an impact in clinical practice.
7.2 Infectogenomics
In the fourteenth century, one-third to half of the population living in Europe was exterminated by a mysterious disease which was called ‘the Black Death’. It is now known that this disease, later named ‘plague’, was most likely a rodent-associated, flea-borne zoonosis caused by Gram-negative bacterium Yersinia pestis [2]. Interestingly, among all people who came into contact with the bacterium, a large proportion became infected and died, some were ill but managed to survive and some had no clinical signs of infection. It appears plausible that each subject responded to infection with Yersinia pestis as well as to other potentially fatal infections in a way that was largely determined by his/her genetic make-up [2, 3]. A more up-to-date example is given by the HIV, the virus responsible for AIDS. Following transmission, HIV enters the bloodstream and infects helper T cells, macrophages and dendritic cells, causing killing of T cells (especially CD4 T cells) by CD8 cytotoxic lymphocytes, with reduction in CD4 T cell numbers and loss of cell-mediated immunity [4]. The HIV most commonly uses chemokine receptors CCR5 and/or CXCR4 co-receptor to enter its target cells. The CCR5 receptor is coded for by the CCR5 gene on chromosome 3. A deletion of a 32-bp segment in this gene (named CCR5-Δ32) has been discovered to result in a non-functional receptor which prevents this way of HIV R5 entry [4]. This genetic variant is rare in Africans/Asians and more common in North European, possibly due to selective pressure by previous epidemics [3, 5, 6]. Homozygosity to this gene variant is characterized by resistance to infection by the most common strain of HIV, while heterozygosity seems to confer partial resistance with slower progression after onset of AIDS [7]. Based on this principle, CCR5 receptor-antagonist drugs have been experimented for the treatment of AIDS [8].
The evidence described above is in line with a concept defined ‘infectogenomics’, suggesting that host genetic factors play a major role in determining the response to bacterial colonization [9, 10]. This concept can be extended also to the presence of common ‘symbiotic’ bacteria and not just pathogens. In other words, host genotypes may influence the composition of human biofilms, including oral biofilms [11]. Therefore, the composition of microbial biofilms in the human body will be dictated by a combination of genetic variants, coupled with environmental factors. As a result of this, a group of human diseases originate from a genetically determined failure to properly recognize or respond to members of the normal human microbiota [11]. This disease-predisposing effect can potentially extend not just to microbial diseases, in the traditional meaning of the term, such as, for example, bacterial vaginosis and periodontitis, but also to diseases not traditionally considered of microbial origin. Among them, rheumatoid arthritis, reactive arthritis and even cancer, which could be influenced by microbial shifts (dysbiosis) even at distant sites. Hence the concept of genetic dysbiosis, which suggests that host genetic variants could be responsible for a range of chronic human diseases through an effect on dysbiosis of microbial biofilms [11].
7.3 Evidence for Genetic Variants Influencing the Response to Microbial Challenge
Where is the evidence for the Infectogenomics principles outlined above? Circumstantial evidence can be derived from studies showing that monozygotic twins frequently have more similar gut microbiomes than non-twin siblings [12]. Furthermore, microbial profiles of faecal samples collected at various times from a given individual are more similar to each other than to the intestinal microbial communities in a different individual [13]. A little dip into the human genome can allow a better understanding of the host-microbial axis. More than 60 million common genetic variants in 19,000–25,000 genes located in 23 pairs of chromosomes are listed in the Single Nucleotide Polymorphism Database (dbSNP) by the National Center for Biotechnology in collaboration with National Human Genome Research Institute [14]. Different individuals are thought to be 99.4% identical in chromosomal structure and 99.9% identical at sequence level [15]. Functional SNPs are located in the gene promoter (affecting gene activity) or in the coding region of the gene (affecting the protein produced). The disease-predisposing effects may be determinant such as for haemophilia A, caused by a specific mutation (single gene defect) in the F8 gene leading to defects in coagulation factor VIII [16]. However, most diseases are characterized by a complex susceptibility profile, where a variety of SNPs contribute to the disease risk. Such SNPs may be involved, for example, in microbial recognition (determining aberrant responses to the normal microbiota), in the inflammatory cascade or in DNA repair (associated with a reduction in the ability to repair damaged DNA).
7.3.1 Microbial Recognition Genes
Following the earlier example of the HIV, it seems reasonable to believe that genetic variants affecting microbial recognition will have a major role in determining the composition of microbial biofilms. The search for the possible ‘microbial recognition’ gene affecting microbial colonization could focus on pattern-recognition receptors (PRRs), which recognize evolutionarily conserved constituents of microbes called pathogen-associated molecular patterns (PAMPs). PRRs include normally cell-bound proteins such as toll-like receptors (TLRs), RIG-I-like receptors (RLRs), NOD-like receptors (NLRs), C-type-lectin like receptors (CLRs), scavenger receptors (SCs), innate DNA receptor proteins termed AIM2-like receptors (ALRs), members of the complement pathways and peptidoglycan-recognition proteins (PRPs) and soluble PRRs (including collectins, ficolins, pentraxins, galectins, sCD14 and natural IgM). Upon microbial interaction, PRRs activate a series of downstream mechanisms through selective cells signalling, leading to the generation of pro- or anti-inflammatory proteins. Mutations in the coding or promoter regions of PRR genes could result in an altered ability to recognize microbial patterns, affecting the ‘binding/recognition’ process and its downstream pathways, leading to aberrant response to microbial challenge and shifts in the normal biofilm composition [17].
The circumstantial evidence for a role of host genetic variants in determining microbial colonization is strengthened by observations on inflammatory bowel disease, encompassing Crohn’s disease (CD) and ulcerative colitis (UC). Genetic variants in the NOD2 gene, coding for an intracellular pattern recognition receptor able to recognize molecules containing bacterial muramyl dipeptide [18], are now recognized as increasing the risk of CD [19]. In an experimental ileal inflammation model in mice [20], when NOD2-CD-susceptible animals were subjected to Toxoplasma gondii-induced ileitis, an increase in inflammation and dysbiosis was noticed (shift from mainly Gram-positive to Gram-negative bacteria, associated with invasive E. coli) compared to non-genetically susceptible animals. Furthermore, genetic variants in the NOD2 and autophagy-related 16-like 1 protein (ATG16L1) have been associated with gut microbiota structure alterations, including decreased Faecalibacterium levels and increased Escherichia levels [21]. These results are likely due to an alteration of the inflammatory cascade resulting from an aberrant response upon microbial recognition through the NOD2 receptor.
Some evidence exists also for the effect of microbial recognition genes on microbial presence in vaginal biofilms. In a study on the vaginal microbiota of 144 pregnant women, detection of A. vaginae and G. vaginalis by PCR was studied in relation to 34 single nucleotide polymorphisms pertaining to 9 genes involved with Toll-like receptor-mediated pathogen recognition and/or regulation. While no association between these SNPs and presence of bacterial vaginosis was detected, some of the studied SNPs were associated with carriage of A. vaginae and G. vaginalis during early pregnancy. The authors suggested that some degree of genetic susceptibility involving pathogen recognition may occur, which influences vaginal presence of potential pathogenic microorganism [22]. In a separate study on 238 pregnant women, TLR4 genotypes were associated with increases in vaginal pH and in vaginal detection of Gardnerella vaginalis, Prevotella, Bacteroides and Porphyromonas, suggesting that genetic variants may drive a change in the vaginal environment which favours the growth of pathogenic bacteria [23].
7.3.2 Genes Involved in Inflammatory Pathways
It is now becoming clear that inflammation can have profound effects on microbial communities, causing a progressive decrease in the microbial diversity through an increased availability of substrates for growth of Gram-negative bacteria (e.g. iron and serum, dead or dying cells) and loss of niche and substrates for Gram-positive flora (e.g. mucus, goblet cells) [24]. Therefore, it is conceivable that variants in genes directly involved in inflammatory pathways, could impact the threshold for dysbiosis and the ability to resolve the dysbiosis-inflammation cycle generated by an acute trigger [20]. Based on this concept, genetic variants affecting inflammatory responses may be major candidates for an effect on microbial biofilm composition. The evidence for this comes mainly from studies on periodontal disease which will be discussed in the next section.
7.4 Genetic Effects on Microbial Colonization: Studies in Periodontal Disease
Previous chapters of this book described how pathogenic pathways leading to periodontal breakdown involve the role of subgingival microbes, host response and environmental factors and how important the crosstalk between host and bacteria is. This chapter introduced the concept of ‘Infectogenomics’ to mean the effect of host genetic background on the colonizing microbes, and examples relative to inflammatory bowel disease and bacterial vaginosis have been provided. In the last 10–15 years, evidence for periodontal infectogenomics [25] has also emerged. In particular, it is striking how the JP2 leukotoxic strain of A. actinomycetemcomitans has a strong tropism of for subjects of mainly North African and West African descent, increasing the risk of development of Localised Aggressive Periodontitis (LAgP) [26]. Since carriage of this strain does not seem to depend on geographic location but rather on ancestry, it is likely to be linked with heritability and with the host genetic make-up. Figures 7.1 and 7.2 show a typical clinical and radiographic presentation of a case of Localized Aggressive Periodontitis (LAgP), characterized by a molar-incisor pattern of bone and periodontal attachment loss.
Panoramic radiograph of patient shown in Fig. 7.1. Please note localized alveolar bone loss affecting mainly upper right central incisor and first molars
The understanding that heritability accounts for about half of the risk of developing periodontitis [27] has led to a flourish of studies trying to identify inflammatory, metabolic or structural gene polymorphisms which could predispose to periodontal diseases [28]. Most studies focused on selected candidate SNPs, starting from the case-control association study suggesting an effect of the Interleukin-1 (IL-1) ‘composite genotype’ on disease predisposition [29]. More recent studies are often using an explorative genome-wide approach [30, 31]. However, studies so far failed to reach a consensus after analyses in different populations and settings, with promising studies pointing towards the role of SNPs in ANRIL (antisense non-coding RNA in the INK4 locus), COX2 (cyclooxygenase 2), IL-10 (Interleukin-10) and DEFB1 (β-defensin-1) and possibly others in disease predisposition [31, 32]. These genes are involved, respectively, in glucose and fatty acid metabolism regulation (ANRIL gene) [33], coding for antimicrobial peptides involved in the epithelial response to microbial invasion (DEFDB1 gene) [34] and in the periodontal inflammatory response (COX2 and IL-10 genes) [35, 36].
Sigmund Socransky and Anne Haffajee were probably the first to investigate the relationships between SNPs supposed to affect the periodontitis trait and presence of subgingival microbes. In their 2000 paper, they observed an association between IL-1 genotypes and presence of subgingival microbes [37]. In particular, more IL-1 ‘genotype positive’ subjects [29] exhibited high mean counts of ‘red’ and ‘orange’ subgingival species than ‘genotype negative’ subjects. Bacteria found at higher levels in IL-1 genotype positive subjects were Bacteroides forsythus, Treponema denticola, the Fusobacterium nucleatum subspecies, Fusobacterium periodonticum, Campylobacter gracilis, Campylobacter showae, Streptococcus constellatus, Streptococcus intermedius, Streptococcus gordonii and 3 Capnocytophaga species. The differences in bacterial colonization by genotype were mainly visible in deep periodontal pockets (>6 mm). Based on these results, the authors postulated that genetic variants might either directly affect bacterial growth and virulence or alter the inflammatory milieu, favouring the growth of specific bacteria. In contrast with these findings, no associations between IL-1 composite genotypes and subgingival bacteria analysed by PCR were detected in a similar study published shortly afterwards [38].
Our group has extensively investigated the associations between candidate genetic variants affecting the inflammatory response (e.g. interleukin-1 and interleukin-6 genes) and subgingival detection of periodontopathogenic bacteria by culture and polymerase chain reaction (PCR). In 45 untreated aggressive periodontitis (AgP) patients from London, IL6 and Fc-γ polymorphisms were both associated with increased odds of detecting A. actinomycetemcomitans, P. gingivalis and T. forsythensis after adjustment for age, ethnicity, smoking and disease severity [39]. In particular, subjects with supposedly pro-inflammatory IL6 genotypes [40, 41] had increased detection of A. actinomycetemcomitans and P. gingivalis. The study was repeated in a rural population living in Andhra Pradesh, India [42]. Subjects had subgingival plaque samples taken and analysed by checkerboard DNA-DNA analysis for 40 periodontal taxa and had their DNA extracted for IL6 SNP analyses. In this population not exposed to regular dental care and to use of antibiotics, most subjects harboured A. actinomycetemcomitans and P. gingivalis subgingivally, which did not allow any analysis on bacterial detection by genotype. However, associations between IL6 genotypes and elevated counts of A. actinomycetemcomitans and Capnocytophaga sputigena were observed, strengthening the previous report. This was further confirmed when a population of 267 chronic and aggressive periodontitis patients was studied. Host DNA samples were extracted from blood samples and analysed for five IL6 SNPs, while subgingival plaque samples were analysed by PCR for the presence of A. actinomycetemcomitans and P. gingivalis. The study confirmed again the association between IL6 supposedly ‘pro-inflammatory’ genetic variants and presence of A. actinomycetemcomitans and of both bacteria concomitantly [43]. To explore this concept further, we conducted a pilot treatment study on 12 AgP patients selected based on their IL6 genotypes (‘pro-inflammatory IL6 haplotype positive’ vs. ‘IL6 haplotype negative’). In this population, higher A. actinomycetemcomitans counts were detected subgingivally in IL6 ‘haplotype positive’ subjects before treatment. Despite a reduction after non-surgical and surgical treatment, these subjects showed a sharp increase in counts of A. actinomycetemcomitans again 3 months after periodontal treatment, suggesting a strong genetic influence on gingival pocket re-colonization, which was not observed in IL6 ‘haplotype negative’ subjects [44].
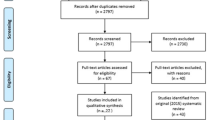
A larger study used a genome-wide approach in 1020 subjects participating in the Atherosclerosis Risk In Communities (ARIC) study to investigate the relationship between host genotypes and eight periodontal pathogens analysed by checkerboard DNA-DNA hybridization [45]. They detected no genome-wide significant signals, but suggestive evidence (p < 5 × 10−6) of association for 13 genetic loci and ‘red’ and ‘orange’ complex microbiota. The same effect direction was detected in a second sample of 123 African-American participants. Interestingly, these authors confirmed the moderate association our group previously reported between IL6 SNPs and high ‘red complex’ colonization. No association was detected between any of the identified SNPs with CP diagnosis, suggesting once more the examination of bacterial colonization as a distinct trait to ‘presence of disease’ [45]. Recently, in a case-control study analysing polymorphism TBX21-1993T/C (rs4794067) in healthy (n = 218), chronic periodontitis (n = 197) and gingivitis patients (n = 193), no associations were detected between genotypes and presence of ‘red complex’ bacteria [46]. A summary of genetic variants shown to be associated to detection of subgingival periodontal bacteria is provided in Table 7.1. A more systematic and comprehensive review of the literature on periodontal infectogenomics has been recently published [47].
Summarizing the findings above, there is now increasing evidence that host genetic variants can have an effect on periodontal pathology by influencing the subgingival bacteria composition. The shifts in A. actinomycetemcomitans, P. gingivalis and more in general ‘red complex’ bacteria may be a small representation of changes in the subgingival biofilm (‘dysbiosis’) (see Fig. 7.3). There is still a lack of studies investigating whether health-associated bacteria may be affected by specific genetic variants. The supposed shift towards a more pathogenic microbiota may occur through the effects on microbial recognition and inflammation discussed above. It is conceivable that a more inflamed milieu, characteristic of patients with ‘pro-inflammatory’ genetic profiles, may favour the growth of bacteria which grow well in inflamed environments, then shifting the whole microbiota towards a disease-predisposing one.
7.5 Challenges and Future Directions
Periodontal genetic research still has a long way to go before it identifies clear predisposing host gene variants in different populations. This is complicated by issues such as sample size, definition of health and disease, genetic methodology, difficulty at controlling for other predisposing factors and epigenetic influences. Recently, gene variants in the IRF5 gene have been associated with IBD [48], while SNPs in the DEFDB1 gene and PRDM1 gene have been associated with chronic and aggressive periodontitis, respectively ([31, 49]). These gene polymorphisms appear to be able to contribute to a disturbance of the immunological barrier, thus promoting dysbiosis of the local microflora, potentially predisposing to disease. Hence, it would be interesting to focus periodontal infectogenomics research on a variety of genes with an effect on microbial recognition and host response. The availability of new metagenomics techniques gives the possibility to explore the associations with health-associated as well as with pathogenic bacteria. Furthermore, there is a lack of studies in periodontally healthy populations, which could give some insights on the genetic influence on the host-microbe crosstalk in health-associated biofilms. Among subjects with healthy periodontia living in a rural population in India, the association between IL6 genetic variants and A. actinomycetemcomitans was confirmed (as in periodontitis patients) [42]. However, a paucity of data exists on healthy subjects in other settings. A better knowledge of how gene variants affect the composition of the subgingival biofilm could shed light into potential pathogenic pathways and could open new management avenues. The above-mentioned pilot study in AgP patients selected based on their IL6 haplotypes [44] could, for example, suggest that ‘IL6 positive’ subjects may benefit from adjunctive antimicrobial therapy, as they might be more likely to have a tendency to re-developing dysbiotic, disease-associated biofilms also after treatment. Studying mechanisms of association between the subgingival biofilm and other biofilms elsewhere in the body, such as in gastro-intestinal tract, vagina and skin, could shed light into mechanisms of host-bacteria crosstalk.
Clinical Relevance
-
Host genetic variants seem to play an important role in determining the composition of microbial biofilms in the human body, including the dental biofilm.
-
Some subjects may be more predisposed to periodontal disease onset and progression through the activity of host genetic variants in the response to the microbial challenge.
-
Knowing which subjects are more predisposed to colonization by specific microbes could affect the clinical management of periodontitis cases.
References
Ruby E, Henderson B, McFall-Ngai M. Microbiology—we get by with a little help from our (little) friends. Science. 2004;303:1305–7.
Gage KL, Kosoy MY. Natural history of plague: perspectives from more than a century of research. Annu Rev Entomol. 2005;50:505–28.
Galvani AP, Slatkin M. Evaluating plague and smallpox as historical selective pressures for the CCR5-Delta 32 HIV-resistance allele. Proc Natl Acad Sci U S A. 2003;100:15276–9.
Carrington M, Dean M, Martin MP, et al. Genetics of HIV-1 infection: chemokine receptor CCR5 polymorphism and its consequences. Hum Mol Genet. 1999;8:1939–45.
Duncan SR, Scott S, Duncan CJ. Reappraisal of the historical selective pressures for the CCR5-Delta 32 mutation. J Med Genet. 2005;42:205–8.
Stephens JC, Reich DE, Goldstein DB, et al. Dating the origin of the CCR5-Delta 32 AIDS-resistance allele by the coalescence of haplotypes. Am J Hum Genet. 1998;62:1507–15.
Marmor M, Sheppard HW, Donnell D, et al. Homozygous and heterozygous CCR5-Delta 32 genotypes are associated with resistance to HIV infection. J Acquir Immune Defic Syndr. 2001;27:472–81.
Lederman MM, Penn-Nicholson A, Cho M, et al. Biology of CCR5 and its role in HIV infection and treatment. J Am Med Assoc. 2006;296:815–26.
Cooke GS, Hill AV. Genetics of susceptibility to human infectious disease. Nat Rev Genet. 2001;2:967–77.
Kellam P, Weiss RA. Infectogenomics: insights from the host genome into infectious diseases. Cell. 2006;124:695–7.
Nibali L, Henderson B, Sadiq ST, et al. Genetic dysbiosis: the role of microbial insults in chronic inflammatory diseases. J Oral Microbiol. 2014;6. doi: 10.3402/jom.v6.22962
Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–4.
Matsuki T, Watanabe K, Fujimoto J, et al. Quantitative PCR with 16S rRNA-gene-targeted species-specific primers for analysis of human intestinal bifidobacteria. Appl Environ Microbiol. 2004;70:167–73.
Sherry ST, Ward MH, Kholodov M, et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001;29:308–11.
Girirajan S, Campbell CD, Eichler EE. Human copy number variation and complex genetic disease. Annu Rev Genet. 2011;45:203–26.
Fomin ME, Togarrati PP, Muench MO. Progress and challenges in the development of a cell-based therapy for hemophilia A. J Thromb Haemost. 2014;12:1954–65.
Karin M, Lawrence T, Nizet V. Innate immunity gone awry: linking microbial infections to chronic inflammation and cancer. Cell. 2006;124:823–35.
Inohara N, Chamaillard M, McDonald C, et al. NOD-LRR proteins: role in host-microbial interactions and inflammatory disease. Annu Rev Biochem. 2005;74:355–83.
Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411:603–6.
Craven M, Egan CE, Dowd SE, et al. Inflammation drives dysbiosis and bacterial invasion in murine models of ileal Crohn’s disease. PLoS One. 2012;7:e41594.
Frank DN, Amand ALS, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104:13780.
Verstraelen H, Verhelst R, Nuytinck L, et al. Gene polymorphisms of Toll-like and related recognition receptors in relation to the vaginal carriage of Gardnerella vaginalis and Atopobium vaginae. J Reprod Immunol. 2009;79:163–73.
Genc MR, Vardhana S, Delaney ML, et al. Relationship between a toll-like receptor-4 gene polymorphism, bacterial vaginosis-related flora and vaginal cytokine responses in pregnant women. Eur J Obstet Gynecol Reprod Biol. 2004;116:152–6.
Hajishengallis G, Liang S, Payne MA, et al. Low-abundance biofilm species orchestrates inflammatory periodontal disease through the commensal microbiota and complement. Cell Host Microbe. 2011;10:497–506.
Nibali L, Donos N, Henderson B. Periodontal infectogenomics. J Med Microbiol. 2009;58:1269–74.
Haubek D, Ennibi OK, Poulsen K, et al. Risk of aggressive periodontitis in adolescent carriers of the JP2 clone of Aggregatibacter (Actinobacillus) actinomycetemcomitans in Morocco: a prospective longitudinal cohort study. Lancet. 2008;371:237–42.
Michalowicz BS, Diehl SR, Gunsolley JC, et al. Evidence of a substantial genetic basis for risk of adult periodontitis. J Periodontol. 2000;71:1699–707.
Laine ML, Crielaard W, Loos BG. Genetic susceptibility to periodontitis. Periodontol 2000. 2012;58:37–68.
Kornman KS, Crane A, Wang HY, et al. The interleukin-1 genotype as a severity factor in adult periodontal disease. J Clin Periodontol. 1997;24:72–7.
Divaris K, Monda KL, North KE, et al. Exploring the genetic basis of chronic periodontitis: a genome-wide association study. Hum Mol Genet. 2013;22:2312–24.
Schaefer AS, Bochenek G, Manke T, et al. Validation of reported genetic risk factors for periodontitis in a large-scale replication study. J Clin Periodontol. 2013;40:563–72.
Ikuta T, Inagaki Y, Tanaka K, et al. Gene polymorphism of beta-defensin-1 is associated with susceptibility to periodontitis in Japanese. Odontology. 2015;103:66–74.
Bochenek G, Hasler R, El Mokhtari NE, et al. The large non-coding RNA ANRIL, which is associated with atherosclerosis, periodontitis and several forms of cancer, regulates ADIPOR1, VAMP3 and C11ORF10. Hum Mol Genet. 2013;22:4516–27.
Durr M, Peschel A. Chemokines meet defensins: the merging concepts of chemoattractants and antimicrobial peptides in host defense. Infect Immun. 2002;70:6515–7.
Loo WTY, Wang M, Jin LJ, et al. Association of matrix metalloproteinase (MMP-1, MMP-3 and MMP-9) and cyclooxygenase-2 gene polymorphisms and their proteins with chronic periodontitis. Arch Oral Biol. 2011;56:1081–90.
Sabat R, Grutz G, Warszawska K, et al. Biology of interleukin-10. Cytokine Growth Factor Rev. 2010;21:331–44.
Socransky SS, Haffajee AD, Smith C, et al. Microbiological parameters associated with IL-1 gene polymorphisms in periodontitis patients. J Clin Periodontol. 2000;27:810–8.
Papapanou P, Neiderud AM, Sandros J, Dahlen G. Interleukin-1 gene polymorphism and periodontal status. A case-control study. J Clin Periodontol. 2001;28:389–96.
Nibali L, Ready DR, Parkar M, et al. Gene polymorphisms and the prevalence of key periodontal pathogens. J Dent Res. 2007;86:416–20.
Fife MS, Ogilvie EM, Kelberman D, et al. Novel IL-6 haplotypes and disease association. Genes Immun. 2005;6:367–70.
Fishman D, Faulds G, Jeffery R, et al. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Investig. 1998;102:1369–76.
Nibali L, Madden I, Franch Chillida F, Heitz-Mayfield L, Brett P, Donos N. -174 genotype associated with Aggregatibacter actinomycetemcomitans in Indians. Oral Dis. 2011;17(2):232–7.
Nibali L, D’Aiuto F, Ready D, Parkar M, Yahaya R, Donos N. No association between A actinomycetemcomitans or P gingivalis and chronic or aggressive periodontitis diagnosis. Quintessence Int. 2012;43(3):247–54.
Nibali L, Pelekos G, Habeeb R, et al. Influence of IL-6 haplotypes on clinical and inflammatory response in aggressive periodontitis. Clin Oral Investig. 2013;17:1235–42.
Divaris K, Monda KL, North KE, et al. Genome-wide association study of periodontal pathogen colonization. J Dent Res. 2012;91:21S–8S.
Cavalla F, Biguettii CC, Colavite PM, et al. TBX21-1993T/C (rs4794067) polymorphism is associated with increased risk of chronic periodontitis and increased T-bet expression in periodontal lesions, but does not significantly impact the IFN-g transcriptional level or the pattern of periodontophatic bacterial infection. Virulence. 2015;6:293–304.
Nibali L, Di Iorio A, Onabolu O, Lin G. Periodontal infectogenomics: systematic review of associations between host genetic variants and subgingival microbial detection. J Clin Periodontol. 2016;43(11):889–900.
Anderson CA, Boucher G, Lees CW, et al. Meta-analysis identifies 29 additional ulcerative colitis risk loci, increasing the number of confirmed associations to 47. Nat Genet. 2011;43:246–52.
Schaefer AS, Jochens A, Dommisch H, et al. A large candidate-gene association study suggests genetic variants at IRF5 and PRDM1 to be associated with aggressive periodontitis. J Clin Periodontol. 2014;41:1122–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Nibali, L. (2018). Genetic Influences on the Periodontal Microbial-Host Crosstalk. In: Bostanci, N., Belibasakis, G. (eds) Pathogenesis of Periodontal Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-53737-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-53737-5_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53735-1
Online ISBN: 978-3-319-53737-5
eBook Packages: MedicineMedicine (R0)