Abstract
The International Society of Mild Approach Assisted Reproduction (ISMAAR) defined Mild Stimulation in-vitro fertilization (MS-IVF) as ‘a method when follicle stimulating hormone (FSH) or human menopausal gonadotropin (hMG) is administered at a lower dose and or for a shorter duration in a Gonadotropin releasing hormone (GnRH)-antagonist co-treated cycle, or when oral compounds, anti-estrogens or aromatase inhibitors (AIs) are used either alone or in combination with gonadotropins (Gn) with an aim to collect a fewer number of oocytes’ (Nargund et al. in Hum Reprod 22:2801–2804, 2007 [1]). Typically, the aim of a MS cycle is to retrieve between 2 to 7 oocytes through a treatment cycle with minimum deviation from normal human physiology. Sequential clomiphene citrate (CC) and low-dose Gn in an antagonist cycle was introduced by the name of ‘minimal stimulation’ IVF (Corfman et al. in Fertility and sterility 60:864–870, 1993 [2]); many authors continue using this term to denote IVF cycles with CC or AIs with or without Gn or GnRH antagonist co-treatment (Zarek and Muasher in Fertil Steril 95(8):2449–2455, 2011 [3]; Kato et al. in Reprod Biol Endocrinol 10:35 2012 [4]). MS-IVF has also been variously termed as ‘low-intensity’ IVF, ‘low intervention’ IVF or ‘mini’ IVF. It is to be noted that MS-IVF is not synonymous with ‘natural IVF’ which is defined as: ‘..IVF is carried out with oocytes collected from a woman’s ovary or ovaries in a spontaneous menstrual cycle without administration of any medication at any time during the cycle’ or ‘administration of GnRH antagonist to block the spontaneous luteinizing hormone (LH) surge with or without FSH or HMG as add-back therapy’ (Nargund et al. in Hum Reprod 22:2801–2804, 2007 [1]).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The International Society of Mild Approach Assisted Reproduction (ISMAAR) defined Mild Stimulation in-vitro fertilization (MS-IVF) as ‘a method when follicle stimulating hormone (FSH) or human menopausal gonadotropin (hMG) is administered at a lower dose and or for a shorter duration in a Gonadotropin realizing hormone (GnRH)-antagonist co-treated cycle, or when oral compounds, anti-estrogens or aromatase inhibitors (AIs) are used either alone or in combination with gonadotropins (Gn) with an aim to collect a fewer number of oocytes’ [1]. Typically, the aim of a MS-IVF is to retrieve between 2 to 7 oocytes through a treatment cycle with minimum deviation from normal human physiology. Sequential clomiphene citrate (CC) and low-dose Gn in an antagonist cycle was introduced by the name of ‘minimal stimulation’ IVF [2]; many authors continue using this term to denote IVF cycles with CC or AIs with or without Gn or GnRH antagonist co-treatment [3, 4]. MS-IVF has also been variously termed as ‘low-intensity’ IVF, ‘low intervention’ IVF or ‘mini’ IVF. It is to be noted that MS-IVF is not synonymous with ‘natural IVF’ which is defined as: ‘..IVF is carried out with oocytes collected from a woman’s ovary or ovaries in a spontaneous menstrual cycle without administration of any medication at any time during the cycle’ or ‘administration of GnRH antagonist to block the spontaneous luteinizing hormone (LH) surge with or without FSH or hMG as add-back therapy’ [1].
The concept of ‘mild’ ovarian stimulation is not new. Following the birth of the first IVF baby from a natural cycle, low dose of Gn with or without oral anti-estrogens were used in the early days of IVF, in order to achieve multi-follicular growth [5]. Subsequently, controlled ovarian hyperstimulation (COH) with higher dose of Gn prevailed in the IVF world, as pituitary downregulation (desensitisation) by GnRH agonist was introduced to prevent premature ovulation in late 1980s. The so-called long downregulation protocol soon became the mainstay of IVF treatment; today this is usually regarded as ‘conventional’ IVF (C-IVF). The aim of C-IVF is to produce as many oocytes as possible, to allow selection of one or more embryos for transfer from a decent cohort of embryos, and also to enable the remaining suitable embryos to be cryo-preserved [6]. The downregulation protocol thus requires administration of Gn, often for long duration and at a high dose, to develop follicles from completely shut-down ovaries [7]. The side effects and risks of intense ovarian stimulation and multiple embryo transfer (ET) in a C-IVF have been well recognized. Ovarian hyperstimulation syndrome (OHSS) and twin or higher-order birth are the two major concerns in relation to C-IVF programmes. In addition, prolonged treatment cycles with intense hormonal manipulation often causes physical discomfort and frequently appears as an emotional burden to the women undergoing treatment [8]. Not least, the cost of the treatment soars with the increasing requirement for medications. As a consequence, toward mid-90s, the need for a safer and more ‘patient-friendly’ ovarian stimulation protocol was called for [9, 10].
The advent of GnRH antagonist as an agent to suppress a premature LH surge and its increasing clinical use made the milder ovarian stimulation in IVF cycles possible. In contrast to GnRH agonists, the antagonists directly compete for the GnRH receptors in the pituitary and suppress the LH secretion within few hours of administration. Through a process of ‘topping-up’ the physiological follicular stimulation, only the healthier and more competent follicle(s) tend to develop [11], increasing the probability of obtaining better quality, euploid embryos [12]. Although fewer oocytes are obtained, comparable clinical outcomes are achieved in a treatment cycle which is less intense, less costly, safer, and more patient-friendly (see below) [13]. Compared to a C-IVF treatment, women find MS-IVF a less stressful experience and they are more likely to undergo repeat MS-IVF following a failed cycle [8, 14]. Today many centers around the world are actively involved in the practice of MS-IVF and its research.
MS Protocols
-
(1)
Low-dose Gn: A fixed low dose of Gn (usually 150 i.u./day of FSH), titrated with body mass index (BMI), is started in early follicular phase (either on 2nd day or day 5 of a natural menstrual cycle). GnRH antagonist (e.g., Cetrorelix) is commenced when the leading follicle is around 14 mm in diameter or if indicated by serum estradiol level (usually >800 pmol/l). Ovulation is triggered when 3 follicles reaches a diameter of 17 mm or greater. Oocyte retrieval is performed 35–36 h after the ovulation trigger.
-
(2)
Oral anti-estrogens-selective estrogen receptor modulator (SERMs) or AIs with or without Gn top-up: The SERM, commonly used is either CC (usually 100 mg/day) or tamoxifen (40 mg/day). Letrozole (2.5 mg/day) is the most commonly administered AI. There are two different regimens for anti-estrogens:
-
(a)
Anti-estrogens are administered for 5 days—starting from 2nd or 3rd day of a natural menstrual cycle and low dose (usually 150 iu) of FSH (±LH) is added from 5th day on either daily or alternate day, depending on the initial ovarian response. GnRH antagonist is commenced when the follicles are around 14 mm or as indicated by serum estradiol and LH levels.
-
(b)
CC or tamoxifen is commenced from 2nd or 3rd day of the cycle and continued until the day of ovulation trigger. FSH at a 150 iu daily dose may be added from 3rd–5th day and continued on alternate days or on a daily basis. SERMS, when administered in this way, effectively block the positive feedback action of estradiol on the initiation of LH surge; therefore, no antagonist is usually required to suppress the surge [15].
-
(a)
Advantages of MS-IVF
Since the inception of MS-IVF in clinical practice, there has been an increasing volume of evidence in the literature, describing its advantages over C-IVF. A number of randomised controlled trials (RCTs) and subsequent meta-analyses have also been published, comparing the effectiveness of the mild approach with the conventional ones. A review of the evidence is as follows:
Reduced Complexity, Less Medication, Fewer side Effects, and Better Tolerance
Prolonged suppression of the ovaries over a period of 2 weeks or more by GnRH agonist in conventional long downregulation protocol often gives rise to menopausal symptoms including hot flushes, night sweats, or mood swings. An initial flare reaction of the agonist is also responsible for ovarian cyst formation. These symptoms are absent when GnRH antagonists are administered in combination with low-dose Gn in MS-IVF cycles. A Cochrane review recognized significantly lower requirement for Gn in GnRH antagonist protocol, compared to that of agonist [7]. RCTs found total Gn doses were even lower, when Gn was commenced on cycle day 5 instead of day 2 of an antagonist cycle [16] or when co-treated with CC [17].
In the RCT by Heijnen et al. the depression, anxiety, and discomfort scores were not significantly different between MS-IVF and C-IVF [18]. On the other hand, a later report of the same RCT found significantly more symptoms of depression following a failed C-IVF cycle, compared to MS-IVF [19]. A study (n = 183) that specifically assessed patients’ attitude toward the acceptability of two different treatment regimens found more treatment-related stress with conventional downregulated protocol compared to that of MS-IVF [14]. Patients felt the stress of cycle cancellation more acceptable following MS-IVF in this study. Psychological burden, mainly stress from a treatment cycle has been shown to be the leading cause of drop out from IVF programme [20]. The anxiety scores and drop out rates were found to be >50% lower than those of C-IVF, when a mild approach IVF was undertaken [8]. MS-IVF treatment cycles also involve fewer injections and are overall less painful [17]. Not a single drop out was reported in the recent prospect cohort study of 163 women undergoing up to 3 cycles of CC+Gn mild IVF regimen [21]. Intense hormonal manipulation along the course of COH has been postulated to have a significant impact on the physical and mental health of the women, which may get worse in the event of cycle cancellation or treatment failure. The blood estrogen levels being closer to physiological concentrations, MS-IVF appeared to be better tolerated by women undergoing IVF treatment.
Fewer Risks
The Cochrane review cited earlier demonstrated a statistically significant reduction of the incidence of OHSS when GnRH antagonist protocol was used in place of agonist downregulation (OR 0.43, 95% CI 0.33–0.57) [7]. With a lower stimulation dose in MS-IVF, another meta-analysis found the OHSS risk even lesser (OR 0.27, 95% CI 0.11–0.66) [22]. RCTs and systematic reviews found significantly reduced incidence of OHSS in a treatment protocol combining CC with Gn [23–25]. MS-IVF allows administration of lower dose hCG for ovulation trigger which further lessens the risk of OHSS [26]. GnRH agonist trigger for final oocyte maturation has recently been shown to be extremely effective in prevention of OHSS. Not a single OHSS occurred in the largest cohort study (44, 468 IVF cycles) to date, by using a protocol comprising of CC plus Gn till the day of GnRH agonist trigger [4]. MS-IVF with agonist trigger would therefore boost the currently drive toward an ‘OHSS-free’ clinic. Trigger of ovulation with GnRH agonist is not possible in a downregulated cycle. One of the risks of generating a very high estrogen levels in hyper-stimulated cycles is venous thromboembolism [27]. An increased incidence of deep vein thrombosis or pulmonary embolism has been reported in pregnancies following IVF treatment [28]. Pulmonary embolism could be lethal. Although comparative data are lacking, at least theoretically, there would be a reduced risk of this complication in MS-IVF. Thus, from all respect, MS-IVF has been proved to be a safer treatment option.
Elective single embryo transfer (SET) is recognized as one of the most effective strategies in reducing the chance of multiple births within an IVF programme. One large RCT found significantly lower incidence of multiple pregnancy with similar cumulative livebirth rates (LBRs) when a mild regimen with SET was compared with C-IVF with double embryo transfer (DET) [18]. By applying strict SET policy in both mild approach and C-IVF cycles, one recent retrospective analysis of a large data base reported better cumulative LBRs (24% vs. 17.5%) with significantly fewer occurrences of OHSS and multiple pregnancy [29]. The aforementioned retrospective study by Kato et al. found very low incidence of ectopic pregnancy (0.36%, 9 out of 2523) and twin pregnancy (0.9%) by transferring single blastocyst following MS-IVF cycles [4].
High Proportion of Good Quality Oocyte/Embryo
Significantly fewer oocytes are retrieved in MS-IVF cycles [17, 22]. Analysis revealed that an optimum recovery of 13–15 oocytes maximized the LBR in C-IVF cycles [30, 31]. However, the same is not applicable for MS-IVF. An earlier RCT found 6 out of 10 women conceived when 4 or less oocytes were retrieved by MS-IVF, compared to none, when the similar numbers of oocytes were retrieved with long downregulation protocol [32]. A more recent RCT on good prognosis patients showed 46.7% top-grade embryos from mild IVF, compared to 42.1% from long protocol; however, the difference was not statistically significant [33]. It has been shown that 6 retrieved oocytes optimize LBR in mild approach IVF [11]. Intense downregulation regimens, by generating high number of oocytes also produce higher proportion of morphologically as well as chromosomally abnormal embryos [34]. One of the landmark RCTs (n = 111) found equal number of euploid embryos, whether mild or conventional IVF was undertaken, despite twice the number of embryos created in the latter [12]. Another more recent RCT (n = 265) found the doses of recombinant FSH strongly correlated with the number of recovered oocytes, but not with the number of blastocysts created [35]. Indeed, the blastocyst–oocyte ratio and fertilization rate (FR) declined with the increasing exogenous FSH dose in this study. Both the RCTs recruited women below 38 years. The emerging concept is that, due to low grade of stimulation, only healthier follicles with more competent eggs are encouraged to develop in MS-IVF cycles [11].
Improved Endometrial Receptivity
There is a large volume of evidence showing that very high, supra-physiological level of estrogen levels in the blood may adversely affect implantation. A basic science study demonstrated progressively less adhesiveness of mouse embryos with human endometrium from fertile oocyte donors, as they were exposed to increasing concentrations estrogen [36]. Very high serum estrogen levels at the time of ovulation trigger have been shown to be detrimental to the endometrial receptivity, regardless of the embryo quality [37–39]. Endometrial gene expression is altered in COH cycles with high circulating estrogen as well as progesterone levels, when compared with those in natural cycles or treatment cycles with low progesterone levels [40–42]. Gene expressions during receptive phase of the endometrium in antagonist co-treated mild stimulation cycles appeared to be closer to that found in physiological menstrual cycle than that of a long protocol [43, 44]. In practice, the implantation rates have been shown to be significantly lowered by high estradiol levels in normal or high responders [39]; milder stimulation in IVF cycles appeared to improve implantation [11, 45].
Comparable Treatment Success
Pregnancy outcomes including clinical pregnancy rates (CPRs), ongoing pregnancy rates (OPRs), and LBRs of MS-IVF have been compared with those of C-IVF in women with normal, low, and high ovarian reserve. The majority of RCTs that compared OPRs between low-dose Gn in an antagonist cycle and the long agonist protocol in good prognosis groups found no significant difference [12, 32]. The RCT by Hohmann et al. reported pregnancy rates of 20% per cycle and 38% per ET with MS-IVF (n = 49) compared to 22% per started cycle and 39% per ET with long protocol(n = 45) [32]. The other RCT by Baarts et al. demonstrated similar OPRs of 19% per started cycle and 34% per ET from MS-IVF (n = 55) as opposed to 17% per started cycle and 23% per ET with C-IVF [12]. The quality of both the trials was affected by their small sample sizes. In contrast, larger (n = 404) non-inferiority RCT, mentioned earlier, found significantly better LBRs in favour of long downregulation protocol (conventional: 24% vs. mild: 15.8% per ET, OR 0.59, CI 0.41–0.85); however, the cumulative LBRs after 1 year, which was the primary outcome in this study, remained the same between the two strategies [18]. It is interesting to note that this RCT by Heijnen et al. actually employed a SET strategy following MS-IVF, whereas DET in C-IVF. SET is known to reduce the chance of conceiving in any type of assisted conception programme [46]. This may explain why LBR per ET was lower in MS-IVF than that of C-IVF, even though cumulative LBRs were similar in that trial (MS-IVF: 43.4% vs. standard IVF: 44.7%). More recent retrospective analysis of large data base that applied strict SET policy in both mild (natural modified IVF) and conventional long downregulation approach, reported similar, if not better LBRs with the former [29]. Meta-analysis of these 3 RCTs found 22% OPRs/ET with MS-IVF and 26% OPR/ET with downregulation protocol; the difference was statistically significant [11]. Another more recent meta-analysis, that included the above 3 RCTs as well as 2 other RCTs revealed similar findings, with OPR per started cycles were 20 and 26% for MS-IVF and C-IVF, respectively, (OR 0.72, CI 0.55–0.93) [22]. The results of the aforementioned RCT by Heijnen et al. had large influence on the pooled data in these meta-analyses [11, 22]. A subsequent larger RCT (n = 412) on normal as well as ovulatory high-responders reported comparable LBRs between low-dose antagonist (150 daily FSH) and long agonist protocol—overall LBRs: 24.9% per started cycle and 28.6% per ET, versus 26.6% per started cycle and 28.6% per ET. LBRs from frozen-thawed ET cycles (21.4% per ET vs. 21.0%) as well as cumulative LBRs from fresh and subsequent frozen ETs together were also similar (42.7% vs. 41.7%) [33]. A report analyzing large volume of data (650,000 cycles) from the registry of the Society for Assisted Reproduction Technology (SART) in the United States identified an inverse relationship between the Gn doses and LBRs, independent of age, prognosis and retrieved oocyte number [47]. A combination of factors including embryo aneuploidy and reduced endometrial receptivity due to supra-physiological level of estrogen or premature progesterone rise has been speculated as possible explanations for this finding.
Treatment outcome are generally encouraging when oral agents, SERMS (usually CC) or AIs (letrozole) are used in MS-IVF protocols. A RCT (n = 100) with sequential CC and Gn protocol in normal responders found OPRs per started cycles similar to that with long downregulation protocol (32% vs. 26%) [48]. Two other RCTs using CC+Gn reported comparable pregnancy rates per ET, when judged against long downregulation protocol: 41.7% versus 40.0% in the RCT that used hMG in combination with CC (n = 120) [17] and 42.9% versus 36.6% in the other larger trial (n = 294) using CC + FSH regimen [24]. In contrast, another earlier RCT found better CPRs with the long protocol [49]. A Cochrane review of RCTs found no difference in LBRs, OPRs, and CPRs when cycles with CC + Gn were compared with long downregulation or antagonist protocol [23]. Later, another systematic review and meta-analysis of 7 trials (702 participants) comparing between CC+ antagonist and antagonist protocol in unselected population also found similar LBRs (CC+ antagonist: 30.2% vs. Antagonist: 26.0%) and miscarriage rates with significantly less risk of OHSS (0.5% vs. 4.1%) [25]. A RCT (n = 167) reported comparable CPR when CC was replaced by letrozole in the sequential regimen, with significantly higher implantation rate in women who received letrozole [50]. Evidence from retrospective studies comparing sequential CC+Gn and C-IVF in young women with normal ovarian reserve were conflicting; some clinical outcomes were in favour of ‘Mini-IVF’ [51], while others supported long downregulation protocol [52]. The MS-IVF protocol comprising of continuous administration of CC till the day of ovulation trigger +/-Gn has emerged as an effective low-cost IVF protocol without the need for GnRH-antagonist for suppression of premature LH surge [53]. Data from the largest retrospective cohort study to date, comprising of 20,244 cycles in 7244 Japanese women showed age-specific LBRs per fresh ET ranging from 30.0% in ≤29 years age-group to around 10% in women aged 40–45 years with the stimulation protocol as above, along with GnRH agonist as an ovulation trigger [4]. The authors reported age-matched LBRs of 37.7% and 44.5% following vitrified–thawed cleavage-stage embryo and blastocyst transfers, respectively, in the best prognosis patients. The figures were higher than those registered in the SART database in the United States [4]. Another large uncontrolled cohort study using a similar protocol found 20% CPRs per fresh SET and 41% by vitrified–thawed SET [54]. Both the studies demonstrated a better LBR per ET in vitrified–thawed cycles relative to fresh ET cycles. A negative impact of CC on the endometrial receptivity has been implicated for this discrepancy. More recently, a prospective cohort study on CC+Gn regimen among good responders reported an impressive cumulative LBRs of 70% when followed up to 2.4 months (3 fresh or frozen ET cycles) [21]. The effectiveness of sequential anti-estrogens and Gn in the perspective of low ovarian reserve has been described under the section of poor responders.
In brief, the current evidence on treatment outcomes of MS-IVF appear to be comparable to those of C-IVF in good prognosis populations. Although OPRs per cycles with low Gn regimen were generally reported to be inferior to those with long downregulation protocol among good prognosis women, cumulative LBRs have consistently been demonstrated to be at per with C-IVF in RCTs and large prospective trials [18, 21, 33]. Further data from well-designed RCTs, using different mild stimulation protocols in different age-groups and ovarian reserves would confirm if MS-IVF can be regarded as standard practice of IVF/ICSI treatment in all clinical scenarios.
Better Maternal and Perinatal Outcome
LBRs have been considered as the benchmark of success in assisted conception. However, a singleton, appropriately grown healthy baby at term is now proposed to be a better marker of a success in an IVF programme [55]. A retrospective study showed higher mean birthweight of the babies born out of MS-IVF [56]. Recently, an analysis of the a massive data set of 63,686 singleton birth found an association between high number of recovered oocytes and higher incidence of perinatal complications including preterm birth and low birth weight babies [57]. Very high estrogen levels at the end of treatment cycles and early pregnancy have also been linked with intra-uterine growth restrictions [58] and cardio-vascular dysfunctions in the neonates [59].
Reduced Treatment Cost
There is a paucity of well-conducted studies on the health–economy of MS-IVF in comparison to C-IVF. Admittedly, cost-effectiveness assessment varies in different clinical settings: SET versus DET (and resultant multiple pregnancy), fresh versus cumulative fresh plus frozen ETs, use of Gn versus oral agents or populations of normal versus low responders, and so on. Earlier studies on normal responders with varied study designs and outcome end-points found MS-IVF not a cost-effective option, even though consumption of medication was less [52, 60]. In the RCT by Heijnen et al., however, the overall cost of MS-IVF cycles up to 1 year with SET was reported to be lower than that of conventional IVF with DET [18]. The main reasons of this difference were lower rates of multiple pregnancy in the former group. Subsequent further cost-effectiveness analysis of the same RCT revealed higher incidence of OHSS, multiple pregnancy and preterm birth as well as neonatal care resulted in significantly increased total expenditure in the long downregulation group [61]. More recent RCTs that compared cost-effectiveness of CC-Gn-antagonist protocol with GnRH agonist downregulation protocols in poor responders identified clear economic advantage of MS protocols [25, 62, 63]. Indeed, extended course of CC till the trigger day has emerged as a potential option for ‘low-budget’ IVF, as this regimen suppress LH surge without the use of the expensive GnRH antagonist. Further, well-designed health–economic evaluation including the treatment cost and subsequent expenditure in pregnancy and delivery may confirm the overall cost-benefit of MS-IVF using both oral and injectable agents.
Limitations of MS-IVF
Potential Cycle Cancellation
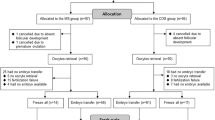
A treatment cycle is usually canceled as a consequence of inadequate response or premature ovulation. A meta-analysis of 3 RCTs conducted on women with normal ovarian reserve found an increased incidence of cycle cancellation before oocytes retrieval in MS-IVF, as compared to conventional IVF (16% vs. 9%; OR 2.55, CI 1.62–4.02) [22]. In the large series with extended CC+Gn protocol, oocytes were obtained from around 80% of cycles in women below 44 years of age, despite only 2.1% cycles abandoned due to premature ovulation [4]. Similar inference was dawn in a RCT on women with poor ovarian reserve: CC+Gn in antagonist protocol was found to be associated with less chance of progression to ET in comparison to high-dose antagonist in a RCT (39% vs. 54%), although the incidence of cycle cancellation due to premature ovulation remained the same between the protocols (14% on each side) [62]. Another large RCT on poor responders reported higher cycle cancellation with CC+Gn cycles, as compared to downregulated cycles (13% vs. 2.7%) [64]. Ovarian aging and high BMI have been reported to be associated with cycle cancellation due to under-response [65].
In contrast, several other studies failed to find an increased risk of cycle cancellation by using MS-IVF. A prospective study with CC+Gn protocol in normal responders reported less chance of cycle cancellation (4.7% vs. 34.0%) [66]. Only 1% of the cycles were abandoned out of 205 women recruited in the MS-IVF arm in a RCT involving normal or high responders [33]. Two other RCTs mentioned earlier, that used CC+Gn as mild stimulation protocol in good prognosis patients, found similar cycle cancellation when compared with long protocol: Karimzadeh et al. reported 4% cancellation rate, while it was 16.9% in the trial by Weigert et al. [24, 48]. No cycle was canceled due to premature ovulation in the RCT comprising of 60 normo-responders in the MS-IVF group with CC+Gn protocol [17]. The Cochrane review on COH with CC+Gn regimen found an overall increased incidence of cycle cancellation when compared with downregulation protocol, but there was no difference in the sub-group where mid-cycle GnRH antagonist was used [23]. Low cancellation rates have also been reported in retrospective studies on poor responders applying CC+Gn protocol (11.7%) [67], or latrozole+Gn protocol (4.2%) [63]. Cancellation rates due to premature ovulation were between 2.1–2.8% by administration of CC up till ovulation trigger [4]. From the current evidence, it appears that the risk of cycle cancellation in MS-IVF is low and comparable to that of C-IVF, at least among good prognosis patients and when one of the oral agents were used in mild approach cycles.
The criteria for cycle cancellation due to under-response need to be set differently in MSIVF. The aim of MS-IVF is to collect higher quality and lower number of eggs. If this is taken into account, cycle cancellations would be rare and successful cycle outcomes are likely in the presence of less than 3 mature follicles at the time of trigger.
Fewer Embryos for Cryo-Preservation
The intention of MS-IVF is to generate fewer oocytes and embryos; so there should be less availability of excess embryo(s) for cryo-preservation [68]. A number of trials reported availability of fewer embryos for transfer or fewer cycles with embryo freezing when one of MS-IVF strategies was employed in good prognosis women [48, 69]. However, the higher probability of obtaining good quality embryos from MS-IVF cycles may somewhat offset this disadvantage in achieving successful outcome [32]. A number of studies including large RCTs demonstrated satisfactory cumulative OPRs/LBRs despite fewer oocytes being recovered and fewer embryos being created in MS-IVF [18, 21, 32, 33].
Less Flexible Scheduling for the Clinic and Need for High Quality Laboratory
Extended service in the weekends and a high standard of embryology laboratory are prerequisites for MS-IVF. Judicious monitoring by ultrasound and hormone levels and timely intervention may avoid premature ovulation and resultant cycle cancellation. A 7-day service and increased need for intense monitoring are some of the factors which make MS-IVF less acceptable to many clinicians involved in the practice of assisted reproduction.
Place of Mild Stimulation IVF in Current Practice
Poor Responders in Assisted Conception
MS-IVF protocols have probably been most extensively tested and applied in the treatment of poor responders. After an era of intensive COH with very high doses of Gn for poor responder women, it is now widely believed that increasing the stimulation does not translate in to better outcome [35, 70]. No improvement in the CPRs per stated cycle and per ET were found by doubling daily FSH dose from 150 iu to 300 iu in an antagonist cycle designed for poor responders [3]. There was some suggestion that GnRH antagonist protocol improved blastocyst quality and pregnancy outcome following multiple failed cycles due to poor response with GnRH agonist [71]. A recent large RCT (n = 695) that included women with poor ovarian reserve and or previous poor response found a higher incidence of cycle cancellation (13% vs. 2.7%) and fewer metaphase II oocytes, but similar implantation rates, CPRs per cycle (13.2% vs. 15.3%), per ET (23.2% vs. 19.9%) and OPRs per ET (17.8% vs. 16.8%) with CC+FSH-antagonist group, compared to those of long downregulation regimen [64]. The CC+Gn mild stimulation protocol has also been assessed against ‘micro-dose flare’ protocol [72] and ‘short agonist flare’ protocol [62] in RCTs involving women with poor ovarian reserve and reported no clear advantage of one way of management over the other. The latter study, which was a non-inferiority RCT of 304 subjects, inferred that the LBRs of either regimen were low (CC: 3% vs. high-dose ‘short’ protocol: 2% per started cycle; 9% per ET on either group); nevertheless, CC+Gn+antagonist conferred more cost savings [62]. Evidence is limited in relation to effectiveness of MS-IVF in older women [73]. In the large cohort series by Kato et al., CC+Gn and agonist trigger regimen resulted in 12.5% CPR and 7.4% LBR per cleavage-stage ET, while 31.6% CPR and 17.7% LBR per vitrified–thawed ET in women’s age-group between 40 and 43 years—these outcomes were claimed to be comparable with age-matched SART registry outcome data; however, the CPRs and LBRs fell significantly in women ≥45-year age [4, 54]. In the sub-group of women between >37 years and 41 years (n = 180), a retrospective study reported non-significantly higher CPR and LBRs per ET with CC+Gn-antagonist protocol, compared to those of long downregulation (12.1% vs. 8.1% and 6.1% vs. 2.7%, respectively) [74]. The clinical outcomes have also been linked with basal serum FSH levels. Sub-group analysis of the RCT by Ragni et al. found that CC+Gn-antagonist protocol did better in women with previous poor response but not in women with serum FSH levels >12 iu [62]. Low LBRs have also been observed when FSH was >15 iu in a cohort study [54]. AI, letrozole was used as an alternative to CC in poor responders. A retrospective study (n = 141) reported significantly higher CPRs (31.4% vs. 12.7%) and LBRs (21.4% vs. 7%) in MS-IVF comprising of letrozole + Gn-antagonist combination as opposed to high Gn dose (≥300 iu/day) in an antagonist protocol [63]. Other retrospective studies found similar LBRs or CPRs between letrozole and conventional antagonist protocol, despite higher oocyte yield and increased number of available embryos [67, 75]. When compared between CC and letrozole as mild stimulation agents, a recent RCT (n = 391) found significantly thicker endometrium and better implantation rate with letrozole; however, the CPRs were similar [50].
The impact of age and ovarian reserve on the outcome of MS-IVF in poor responders requires further evaluation in large prospective trials. Even though the final outcomes appear to be similar, substantially reduced use of medication, shorter duration of treatment, and treatment cost ultimately lessen the physical and psychological and economic burden associated with aggressive IVF treatment among the poor responders [25, 62, 63].
Fertility Preservation for Cancer Patients
A very special indication of MS-IVF is in the field of fertility preservation through oocyte/embryo freezing for women with estrogen sensitive malignancies. Since the inception of natural cycle IVF, it has drawn attention as a potential ‘no stimulation’ assisted conception for fertility preservation of young women with breast cancer. Anti-estrogens, tamoxifen, and AIs (e.g., Letrozole) have been widely used in an ovarian stimulation protocol for women known to have estrogen receptor-positive breast cancer to prevent the risk of cancer recurrence from high estrogenic state in this process [76]. Tamoxifen, by its anti-estrogenic property protects the breast tissue from high levels of circulating estrogen, while letrozole, by inhibiting aromatase enzyme in the granulosa cells limits serum estradiol levels and also reduces Gn requirement in antagonist cycles [77, 78]. In a prospective study of 215 patients with breast cancer, the hazard ratio of cancer recurrence 0.56 (95% CI, 0.17–1.9) was not increased and the survival was not compromised following letrozole stimulation [79]. Letrozole has also been successfully used for young women with a history of endometrial cancer [80]. The scope of MS-IVF expanded further with the introduction of in-vitro maturation (IVM) following recovery of oocyte from both dominant and non-dominant follicles in natural or modified natural cycle IVF [81]. More oocytes/embryos for transfer or cryo-preservation can be made available in this way [81]. Initial reports of IVM in a pure natural cycle were satisfactory [82]. One study found a maturation rate of 77.4% and CPR of 29.9% in cycles with low-dose FSH priming and HCG, without increase in the risk of cancer recurrence [83]. The use of mild stimulation with anti-estrogen co-treatment or application of IVM needs to be explored further through prospective research.
Low-cost IVF in Low-Resourced Condition
As the cost of medications is less, MS-IVF is considered in low-resourced countries. Inexpensive oral agents—anti-estrogens are widely used for low-cost IVF treatment. When administration of CC or tamoxifen is extended beyond the usual 5-day course, right up to the day of ovulation trigger, it has been shown to suppress LH surge (and thereby ovulation) [15, 84]. This obviates the need for expensive GnRH antagonists and frequent ultrasound monitoring. The Gn, if needed in addition, is kept at a very low dose: typically, on alternate days for a short period. Reports of this regimen are encouraging [4, 53]; large prospective controlled trials are required to establish its effectiveness. Along with the use of ‘simplified culture media’ and minimal luteal phase support, promotion of this low-cost IVF programme is one of the leading global agendas of ISMAAR today. The objective is to make IVF treatment more accessible and affordable in developing countries [85].
Patient-Centerd Assisted Conception
There has been a move from a ‘clinician-centerd’ to ‘patient-centerd’ approach in assisted conception service. Many clinics are more comfortable with the downregulation protocol that helps in better cycle scheduling and avoidance of weekend work. MS-IVF is considered ‘patient-centerd’ as it reduces patient’s physical discomfort and distress pertaining to intense ovarian stimulation. It does not compromise patient’s safety, while maintaining a comparable treatment outcome. Not the least, it is more favorable to patients’ budget. Getting the treatment ‘fitted’ in to women’s natural cycle, it causes less disruption to their working life [61, 86]. Women are more likely to seek MS-IVF after having gone through failed C-IVF with aggressive ovarian stimulation [8]. Flexibility in the protocol in MS-IVF has made the treatment more ‘tailor-made’ to patients’ clinical characteristics, emotional and financial need. Again, ISMAAR has taken an important role in propagating the concept of patient-centerd IVF worldwide [85].
Future Prospect
Progress in the field of MS-IVF has raised the hope that it could replace C-IVF in the future under all clinical circumstances [87, 88]. The major deterrents in achieving this goal are as follows: lack of robust RCT data on the efficacy of MS-IVF in good prognosis patients, the clinicians’ attitude of adhering to convenient cycle scheduling, satisfaction in retrieving as many oocytes as possible, and variation in the standard of embryology laboratories and the public funding policies in some part of the world [73].
The future lies in the hands of researchers and proactive clinicians to take MS-IVF further. Well-designed clinical trials are required to evaluate MS-IVF more analytically. Ideally, an adequately powered RCT should compare the cost and treatment outcomes, particularly in terms of cumulative LBRs of combined fresh and vitrified–thawed SET cycles between MS-IVF and C-IVF, with the analysis in different clinical settings. The final goal of any assisted conception treatment would be a ‘singleton healthy livebirth at term’. Allegedly high cancellation rates, which somewhat lower the per-cycle CPRs or LBRs, may be minimized by the use of anti-estrogens throughout the proliferative phase until the trigger day [4], careful monitoring of cycles by ultrasound scans along with knowledge of serum estradiol and LH levels and the use of indomethacin in selected cases [89, 90] with rescue oocyte retrieval in the event of premature LH surge. An efficient vitrification programme would be an essential prerequisite to improve cumulative pregnancies [73]. Further advancement in IVM may make more embryos available for cryo-preservation [68]. Equally important is to work toward building up robust protocols taking account of the patient’s characteristics and develop clear criteria of choosing between different mild stimulation protocols [73]. Women’s age and BMI may have influence on the ovarian response [65]; these factors need to be taken into account while customising the protocol for individual patients. Further promotion of MS-IVF may be possible through education, training, and research [88]. Communication between the investigators and publishing research data on the progress would increase clinicians’ acceptance of the mild approach.
Conclusion
Mild stimulation IVF has emerged as a safer, cheaper, and more patient-friendly alternative to conventional IVF. Although fewer oocytes are released, equivalent numbers of high quality euploid embryos can be obtained with this approach. Available data from several RCTs and large retrospective studies on MS-IVF versus conventional regimens depicted comparable treatment outcomes. The use of oral agents in a MS-IVF protocol has been shown to be advantageous, particularly in poor responders, as it seems at least as effective as C-IVF with considerable cost saving. Further research may prove mild approach to be a cost-effective and acceptable treatment option for all women undergoing IVF treatment.
References
Nargund G, Fauser BC, Macklon NS, Ombelet W, Nygren K, Frydman R. Rotterdam ICGoTfOSfIVF: The ISMAAR proposal on terminology for ovarian stimulation for IVF. Hum Reprod. 2007;22(11):2801–4.
Corfman RS, Milad MP, Bellavance TL, Ory SJ, Erickson LD, Ball GD. A novel ovarian stimulation protocol for use with the assisted reproductive technologies. Fertil Steril. 1993;60(5):864–70.
Zarek SM, Muasher SJ. Mild/minimal stimulation for in vitro fertilization: an old idea that needs to be revisited. Fertil Steril. 2011;95(8):2449–55.
Kato K, Takehara Y, Segawa T, Kawachiya S, Okuno T, Kobayashi T, Bodri D, Kato O. Minimal ovarian stimulation combined with elective single embryo transfer policy: age-specific results of a large, single-centre. Japan Cohort Reprod Biol Endocrinol. 2012;10:35.
Jones HW Jr, Jones GS, Andrews MC, Acosta A, Bundren C, Garcia J, Sandow B, Veeck L, Wilkes C, Witmyer J, et al. The program for in vitro fertilization at Norfolk. Fertil Steril. 1982;38(1):14–21.
Macklon NS, Stouffer RL, Giudice LC, Fauser BC. The science behind 25 years of ovarian stimulation for in vitro fertilization. Endocr Rev. 2006;27(2):170–207.
Al-Inany HG, Youssef MA, Aboulghar M, Broekmans F, Sterrenburg M, Smit J, Abou-Setta AM: Gonadotrophin-releasing hormone antagonists for assisted reproductive technology. Cochrane Database Syst Rev 2011(5):CD001750.
Verberg MF, Eijkemans MJ, Heijnen EM, Broekmans FJ, de Klerk C, Fauser BC, Macklon NS. Why do couples drop-out from IVF treatment? A Prospective Cohort Study Hum Reprod. 2008;23(9):2050–5.
Edwards RG, Lobo R, Bouchard P. Time to revolutionize ovarian stimulation. Hum Reprod. 1996;11(5):917–9.
Rongieres-Bertrand C, Olivennes F, Righini C, Fanchin R, Taieb J, Hamamah S, Bouchard P, Frydman R. Revival of the natural cycles in in-vitro fertilization with the use of a new gonadotrophin-releasing hormone antagonist (Cetrorelix): a pilot study with minimal stimulation. Hum Reprod. 1999;14(3):683–8.
Verberg MF, Eijkemans MJ, Macklon NS, Heijnen EM, Baart EB, Hohmann FP, Fauser BC, Broekmans FJ. The clinical significance of the retrieval of a low number of oocytes following mild ovarian stimulation for IVF: a meta-analysis. Hum Reprod Update. 2009;15(1):5–12.
Baart EB, Martini E, Eijkemans MJ, Van Opstal D, Beckers NG, Verhoeff A, Macklon NS, Fauser BC. Milder ovarian stimulation for in-vitro fertilization reduces aneuploidy in the human preimplantation embryo: a randomized controlled trial. Hum Reprod. 2007;22(4):980–8.
Ubaldi F, Rienzi L, Baroni E, Ferrero S, Iacobelli M, Minasi MG, Sapienza F, Romano S, Colasante A, Litwicka K, et al. Hopes and facts about mild ovarian stimulation. Reprod Biomed Online. 2007;14(6):675–81.
Hojgaard A, Ingerslev HJ, Dinesen J. Friendly IVF: patient opinions. Hum Reprod. 2001;16(7):1391–6.
Messinis IE, Templeton A. Blockage of the positive feedback effect of oestradiol during prolonged administration of clomiphene citrate to normal women. Clin Endocrinol (Oxf). 1988;29(5):509–16.
Blockeel C, Sterrenburg MD, Broekmans FJ, Eijkemans MJ, Smitz J, Devroey P, Fauser BC. Follicular phase endocrine characteristics during ovarian stimulation and GnRH antagonist cotreatment for IVF: RCT comparing recFSH initiated on cycle day 2 or 5. J Clin Endocrinol Metab. 2011;96(4):1122–8.
Lin YH, Hwang JL, Seow KM, Huang LW, Hsieh BC, Tzeng CR. Comparison of outcome of clomiphene citrate/human menopausal gonadotropin/cetrorelix protocol and buserelin long protocol–a randomized study. Gynecol Endocrinol. 2006;22(6):297–302.
Heijnen EM, Eijkemans MJ, De Klerk C, Polinder S, Beckers NG, Klinkert ER, Broekmans FJ, Passchier J, Te Velde ER, Macklon NS, et al. A mild treatment strategy for in-vitro fertilisation: a randomised non-inferiority trial. Lancet. 2007;369(9563):743–9.
de Klerk C, Macklon NS, Heijnen EM, Eijkemans MJ, Fauser BC, Passchier J, Hunfeld JA. The psychological impact of IVF failure after two or more cycles of IVF with a mild versus standard treatment strategy. Hum Reprod. 2007;22(9):2554–8.
Olivius C, Friden B, Borg G, Bergh C. Why do couples discontinue in vitro fertilization treatment? Cohort Study Fertil Steril. 2004;81(2):258–61.
Ferraretti AP, Gianaroli L, Magli MC, Devroey P. Mild ovarian stimulation with clomiphene citrate launch is a realistic option for in vitro fertilization. Fertil Steril. 2015;104(2):333–8.
Matsaseng T, Kruger T, Steyn W. Mild ovarian stimulation for in vitro fertilization: are we ready to change? Meta-analysis Gynecol Obstet Invest. 2013;76(4):233–40.
Gibreel A, Maheshwari A, Bhattacharya S: Clomiphene citrate in combination with gonadotropins for controlled ovarian stimulation in women undergoing in vitro fertilization. Cochrane Database Syst Rev. 2012, 11:CD008528.
Weigert M, Krischker U, Pohl M, Poschalko G, Kindermann C, Feichtinger W. Comparison of stimulation with clomiphene citrate in combination with recombinant follicle-stimulating hormone and recombinant luteinizing hormone to stimulation with a gonadotropin-releasing hormone agonist protocol: a prospective, randomized study. Fertil Steril. 2002;78(1):34–9.
Figueiredo JB, Nastri CO, Vieira AD, Martins WP. Clomiphene combined with gonadotropins and GnRH antagonist versus conventional controlled ovarian hyperstimulation without clomiphene in women undergoing assisted reproductive techniques: systematic review and meta-analysis. Arch Gynecol Obstet. 2013;287(4):779–90.
Nargund G, Hutchison L, Scaramuzzi R, Campbell S. Low-dose HCG is useful in preventing OHSS in high-risk women without adversely affecting the outcome of IVF cycles. Reprod Biomed Online. 2007;14(6):682–5.
Mor YS, Schenker JG. Ovarian hyperstimulation syndrome and thrombotic events. Am J Reprod Immunol. 2014;72(6):541–8.
Hansen AT, Kesmodel US, Juul S, Hvas AM. Increased venous thrombosis incidence in pregnancies after in vitro fertilization. Hum Reprod. 2014;29(3):611–7.
Groen H, Tonch N, Simons AH, van der Veen F, Hoek A, Land JA. Modified natural cycle versus controlled ovarian hyperstimulation IVF: a cost-effectiveness evaluation of three simulated treatment scenarios. Hum Reprod. 2013;28(12):3236–46.
Sunkara SK, Rittenberg V, Raine-Fenning N, Bhattacharya S, Zamora J, Coomarasamy A. Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Hum Reprod. 2011;26(7):1768–74.
van der Gaast MH, Eijkemans MJ, van der Net JB, de Boer EJ, Burger CW, van Leeuwen FE, Fauser BC, Macklon NS. Optimum number of oocytes for a successful first IVF treatment cycle. Reprod Biomed Online. 2006;13(4):476–80.
Hohmann FP, Macklon NS, Fauser BC. A randomized comparison of two ovarian stimulation protocols with gonadotropin-releasing hormone (GnRH) antagonist cotreatment for in vitro fertilization commencing recombinant follicle-stimulating hormone on cycle day 2 or 5 with the standard long GnRH agonist protocol. J Clin Endocrinol Metab. 2003;88(1):166–73.
Casano S, Guidetti D, Patriarca A, Pittatore G, Gennarelli G, Revelli A. MILD ovarian stimulation with GnRH-antagonist vs. long protocol with low dose FSH for non-PCO high responders undergoing IVF: a prospective, randomized study including thawing cycles. J Assist Reprod Genet. 2012;29(12):1343–51.
Haaf T, Hahn A, Lambrecht A, Grossmann B, Schwaab E, Khanaga O, Hahn T, Tresch A, Schorsch M. A high oocyte yield for intracytoplasmic sperm injection treatment is associated with an increased chromosome error rate. Fertil Steril. 2009;91(3):733–8.
Arce JC, Andersen AN, Fernandez-Sanchez M, Visnova H, Bosch E, Garcia-Velasco JA, Barri P, de Sutter P, Klein BM, Fauser BC: Ovarian response to recombinant human follicle-stimulating hormone: a randomized, antimullerian hormone-stratified, dose-response trial in women undergoing in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2014, 102(6):1633–1640 e1635.
Valbuena D, Martin J, de Pablo JL, Remohi J, Pellicer A, Simon C. Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76(5):962–8.
Fauser BC, Devroey P. Reproductive biology and IVF: ovarian stimulation and luteal phase consequences. Trends Endocrinol Metab. 2003;14(5):236–42.
Valbuena D, Jasper M, Remohi J, Pellicer A, Simon C. Ovarian stimulation and endometrial receptivity. Hum Reprod. 1999;14(Suppl 2):107–11.
Simon C, Cano F, Valbuena D, Remohi J, Pellicer A. Clinical evidence for a detrimental effect on uterine receptivity of high serum oestradiol concentrations in high and normal responder patients. Hum Reprod. 1995;10(9):2432–7.
Haouzi D, Assou S, Mahmoud K, Tondeur S, Reme T, Hedon B, De Vos J, Hamamah S. Gene expression profile of human endometrial receptivity: comparison between natural and stimulated cycles for the same patients. Hum Reprod. 2009;24(6):1436–45.
Horcajadas JA, Minguez P, Dopazo J, Esteban FJ, Dominguez F, Giudice LC, Pellicer A, Simon C. Controlled ovarian stimulation induces a functional genomic delay of the endometrium with potential clinical implications. J Clin Endocrinol Metab. 2008;93(11):4500–10.
Labarta E, Martinez-Conejero JA, Alama P, Horcajadas JA, Pellicer A, Simon C, Bosch E. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011;26(7):1813–25.
Devroey P, Bourgain C, Macklon NS, Fauser BC. Reproductive biology and IVF: ovarian stimulation and endometrial receptivity. Trends Endocrinol Metab. 2004;15(2):84–90.
Haouzi D, Assou S, Dechanet C, Anahory T, Dechaud H, De Vos J, Hamamah S. Controlled ovarian hyperstimulation for in vitro fertilization alters endometrial receptivity in humans: protocol effects. Biol Reprod. 2010;82(4):679–86.
Simon C. Garcia Velasco JJ, Valbuena D, Peinado JA, Moreno C, Remohi J, Pellicer A: Increasing uterine receptivity by decreasing estradiol levels during the preimplantation period in high responders with the use of a follicle-stimulating hormone step-down regimen. Fertil Steril. 1998;70(2):234–9.
Prados N, Quiroga R, Caligara C, Ruiz M, Blasco V, Pellicer A, Fernandez-Sanchez M: Elective single versus double embryo transfer: live birth outcome and patient acceptance in a prospective randomised trial. Reprod Fertility Dev. 2014.
Baker VL, Brown MB, Luke B, Smith GW, Ireland JJ: Gonadotropin dose is negatively correlated with live birth rate: analysis of more than 650,000 assisted reproductive technology cycles. Fertil Steril. 2015, 104(5):1145–1152 e1145.
Karimzadeh MA, Ahmadi S, Oskouian H, Rahmani E. Comparison of mild stimulation and conventional stimulation in ART outcome. Arch Gynecol Obstet. 2010;281(4):741–6.
Dhont M, Onghena A, Coetsier T, De Sutter P. Prospective randomized study of clomiphene citrate and gonadotrophins versus goserelin and gonadotrophins for follicular stimulation in assisted reproduction. Hum Reprod. 1995;10(4):791–6.
Eftekhar M, Mohammadian F, Davar R, Pourmasumi S. Comparison of pregnancy outcome after letrozole versus clomiphene treatment for mild ovarian stimulation protocol in poor responders. Iran J Reprod Med. 2014;12(11):725–30.
Williams SC, Gibbons WE, Muasher SJ, Oehninger S. Minimal ovarian hyperstimulation for in vitro fertilization using sequential clomiphene citrate and gonadotropin with or without the addition of a gonadotropin-releasing hormone antagonist. Fertil Steril. 2002;78(5):1068–72.
Mansour R, Aboulghar M, Serour GI, Al-Inany HG, Fahmy I, Amin Y. The use of clomiphene citrate/human menopausal gonadotrophins in conjunction with GnRH antagonist in an IVF/ICSI program is not a cost effective protocol. Acta Obstet Gynecol Scand. 2003;82(1):48–52.
Kawachiya S, Segawa T, Kato K, Takehara Y, Teramoto S. Kato. O.: The Effectiveness of Clomiphene Citrate in Suppressing the LH surge in the Minimal Stimulation IVF Protocol. Fertil Steril. 2006;86(Suppl 2):S412.
Zhang J, Chang L, Sone Y, Silber S. Minimal ovarian stimulation (mini-IVF) for IVF utilizing vitrification and cryopreserved embryo transfer. Reprod Biomed Online. 2010;21(4):485–95.
Frydman R, Nargund G. Mild approaches in assisted reproduction–better for the future? Fertil Steril. 2014;102(6):1540–1.
Pelinck MJ, Keizer MH, Hoek A, Simons AH, Schelling K, Middelburg K, Heineman MJ. Perinatal outcome in singletons after modified natural cycle IVF and standard IVF with ovarian stimulation. Eur J Obstet Gynecol Reprod Biol. 2010;148(1):56–61.
Sunkara SK, La Marca A, Seed PT, Khalaf Y. Increased risk of preterm birth and low birthweight with very high number of oocytes following IVF: an analysis of 65 868 singleton live birth outcomes. Hum Reprod. 2015;30(6):1473–80.
Hu XL, Feng C, Lin XH, Zhong ZX, Zhu YM, Lv PP, Lv M, Meng Y, Zhang D, Lu XE, et al. High maternal serum estradiol environment in the first trimester is associated with the increased risk of small-for-gestational-age birth. J Clin Endocrinol Metab. 2014;99(6):2217–24.
Xu GF, Zhang JY, Pan HT, Tian S, Liu ME, Yu TT, Li JY, Ying WW, Yao WM, Lin XH, et al. Cardiovascular dysfunction in offspring of ovarian-hyperstimulated women and effects of estradiol and progesterone: a retrospective cohort study and proteomics analysis. J Clin Endocrinol Metab. 2014;99(12):E2494–503.
Kovacs P, Matyas S. Bernard l A, Kaali SG: Comparison of clinical outcome and costs with CC + gonadotropins and gnrha + gonadotropins during Ivf/ICSI cycles. J Assist Reprod Genet. 2004;21(6):197–202.
Polinder S, Heijnen EM, Macklon NS, Habbema JD, Fauser BJ, Eijkemans MJ. Cost-effectiveness of a mild compared with a standard strategy for IVF: a randomized comparison using cumulative term live birth as the primary endpoint. Hum Reprod. 2008;23(2):316–23.
Ragni G, Levi-Setti PE, Fadini R, Brigante C, Scarduelli C, Alagna F, Arfuso V, Mignini-Renzini M, Candiani M, Paffoni A, et al. Clomiphene citrate versus high doses of gonadotropins for in vitro fertilisation in women with compromised ovarian reserve: a randomised controlled non-inferiority trial. Reprod Biol Endocrinol. 2012;10:114.
Lazer T, Dar S, Shlush E. Al Kudmani BS, Quach K, Sojecki A, Glass K, Sharma P, Baratz A, Librach CL: Comparison of IVF Outcomes between Minimal Stimulation and High-Dose Stimulation for Patients with Poor Ovarian Reserve. Int J Reprod Med. 2014;2014:581451.
Revelli A, Chiado A, Dalmasso P, Stabile V, Evangelista F, Basso G, Benedetto C. “Mild” vs. “long” protocol for controlled ovarian hyperstimulation in patients with expected poor ovarian responsiveness undergoing in vitro fertilization (IVF): a large prospective randomized trial. J Assist Reprod Genet. 2014;31(7):809–15.
Verberg MF, Eijkemans MJ, Macklon NS, Heijnen EM, Fauser BC, Broekmans FJ. Predictors of low response to mild ovarian stimulation initiated on cycle day 5 for IVF. Hum Reprod. 2007;22(7):1919–24.
D’Amato G, Caroppo E, Pasquadibisceglie A, Carone D, Vitti A, Vizziello GM. A novel protocol of ovulation induction with delayed gonadotropin-releasing hormone antagonist administration combined with high-dose recombinant follicle-stimulating hormone and clomiphene citrate for poor responders and women over 35 years. Fertil Steril. 2004;81(6):1572–7.
Jovanovic VP, Kort DH, Guarnaccia MM, Sauer MV, Lobo RA. Does the addition of clomiphene citrate or letrazole to gonadotropin treatment enhance the oocyte yield in poor responders undergoing IVF? J Assist Reprod Genet. 2011;28(11):1067–72.
Verberg MF, Macklon NS, Nargund G, Frydman R, Devroey P, Broekmans FJ, Fauser BC. Mild ovarian stimulation for IVF. Hum Reprod Update. 2009;15(1):13–29.
Stimpfel M, Vrtacnik-Bokal E, Pozlep B, Virant-Klun I. Comparison of GnRH agonist, GnRH antagonist, and GnRH antagonist mild protocol of controlled ovarian hyperstimulation in good prognosis patients. Int J Endocrinol. 2015;2015:385049.
Land JA, Yarmolinskaya MI, Dumoulin JC, Evers JL. High-dose human menopausal gonadotropin stimulation in poor responders does not improve in vitro fertilization outcome. Fertil Steril. 1996;65(5):961–5.
Takahashi K, Mukaida T, Tomiyama T, Goto T, Oka C. GnRH antagonist improved blastocyst quality and pregnancy outcome after multiple failures of IVF/ICSI-ET with a GnRH agonist protocol. J Assist Reprod Genet. 2004;21(9):317–22.
Mohsen IA, El Din RE. Minimal stimulation protocol using letrozole versus microdose flare up GnRH agonist protocol in women with poor ovarian response undergoing ICSI. Gynecol Endocrinol. 2013;29(2):105–8.
Fauser BC, Nargund G, Andersen AN, Norman R, Tarlatzis B, Boivin J, Ledger W. Mild ovarian stimulation for IVF: 10 years later. Hum Reprod. 2010;25(11):2678–84.
Yoo JH, Cha SH, Park CW, Kim JY, Yang KM, Song IO, Koong MK, Kang IS, Kim HO. Comparison of mild ovarian stimulation with conventional ovarian stimulation in poor responders. Clin Exp Reprod Med. 2011;38(3):159–63.
Lee KH, Kim CH, Suk HJ, Lee YJ, Kwon SK, Kim SH, Chae HD, Kang BM. The effect of aromatase inhibitor letrozole incorporated in gonadotrophin-releasing hormone antagonist multiple dose protocol in poor responders undergoing in vitro fertilization. Obstet Gynecol Sci. 2014;57(3):216–22.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–53.
Oktay K, Hourvitz A, Sahin G, Oktem O, Safro B, Cil A, Bang H. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J Clin Endocrinol Metab. 2006;91(10):3885–90.
Oktay K. Further evidence on the safety and success of ovarian stimulation with letrozole and tamoxifen in breast cancer patients undergoing in vitro fertilization to cryopreserve their embryos for fertility preservation. J Clin Oncol. 2005;23(16):3858–9.
Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol. 2008;26(16):2630–5.
Azim A, Oktay K. Letrozole for ovulation induction and fertility preservation by embryo cryopreservation in young women with endometrial carcinoma. Fertil Steril. 2007;88(3):657–64.
Chian RC, Uzelac PS, Nargund G. In vitro maturation of human immature oocytes for fertility preservation. Fertil Steril. 2013;99(5):1173–81.
Lim JH, Yang SH, Xu Y, Yoon SH, Chian RC. Selection of patients for natural cycle in vitro fertilization combined with in vitro maturation of immature oocytes. Fertil Steril. 2009;91(4):1050–5.
Fadini R. Dal Canto MB, Mignini Renzini M, Brambillasca F, Comi R, Fumagalli D, Lain M, Merola M, Milani R, De Ponti E: Effect of different gonadotrophin priming on IVM of oocytes from women with normal ovaries: a prospective randomized study. Reprod Biomed Online. 2009;19(3):343–51.
Al-Inany H, Azab H, El-Khayat W, Nada A, El-Khattan E, Abou-Setta AM. The effectiveness of clomiphene citrate in LH surge suppression in women undergoing IUI: a randomized controlled trial. Fertil Steril. 2010;94(6):2167–71.
Nargund G, Chian RC. ISMAAR: Leading the global agenda for a more physiological, patient-centred, accessible and safer approaches in ART. J Assist Reprod Genet. 2013;30(2):155–6.
Dixon S. Faghih Nasiri F, Ledger WL, Lenton EA, Duenas A, Sutcliffe P, Chilcott JB: Cost-effectiveness analysis of different embryo transfer strategies in England. BJOG. 2008;115(6):758–66.
Edwards RG. IVF, IVM, natural cycle IVF, minimal stimulation IVF - time for a rethink. Reproductive biomedicine online. 2007;15(1):106–19.
Nargund G, Frydman R. Towards a more physiological approach to IVF. Reprod Biomed Online. 2007;14(5):550–2.
Kadoch IJ, Al-Khaduri M, Phillips SJ, Lapensee L, Couturier B, Hemmings R, Bissonnette F. Spontaneous ovulation rate before oocyte retrieval in modified natural cycle IVF with and without indomethacin. Reprod Biomed Online. 2008;16(2):245–9.
Rijken-Zijlstra TM, Haadsma ML, Hammer C, Burgerhof JG, Pelinck MJ, Simons AH, van Echten-Arends J, Arts JG, Land JA, Groen H, et al. Effectiveness of indometacin to prevent ovulation in modified natural-cycle IVF: a randomized controlled trial. Reprod Biomed Online. 2013;27(3):297–304.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Datta, A., Campbell, S., Nargund, G. (2017). Minimal or Mild Ovarian Stimulation for IVF: Overview. In: Chian, RC., Nargund, G., Huang, J. (eds) Development of In Vitro Maturation for Human Oocytes. Springer, Cham. https://doi.org/10.1007/978-3-319-53454-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-53454-1_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53452-7
Online ISBN: 978-3-319-53454-1
eBook Packages: MedicineMedicine (R0)