Abstract
Manual lymphatic drainage (MLD)-based decongestive lymphatic therapy (DLT) has long been the mainstay of treatment in the contemporary management of chronic lymphedema. Reconstructive lymphatic surgery is the best option for the management of chronic lymphedema when performed at the optimal time. It is also a viable option for lymphedema patients who have failed to respond to DLT alone.
Continued postoperative DLT and compression therapy are required as supplemental therapy in the group of lymphedema patients who are poor responders to DLT. Postoperative DLT is even more important when reconstructive surgery is performed at a suboptimal or later stage of lymphedema. Long-term patient compliance with DLT and compression therapy is critical following surgical therapy in the group of poor responders to DLT.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
-
Reconstructive lymphatic surgery remains controversial mainly because of poor reproducibility and a wide variety of mixed outcomes.
-
The optimal timing of the surgical procedure has been recognized as the most critical factor for its long-term durability.
-
Long-term patient compliance with decongestive lymphatic therapy and compression therapy is critical following surgical therapy.
Restoration and maintenance of normal limb function and normal cosmetic appearance are the main goals of treatment of the lymphedematous limb [1, 2, 6, 7].
Manual lymphatic drainage (MLD)-based complex decongestive therapy (CDT) [8,9,10,11] has long been the mainstay of treatment in the contemporary management of chronic lymphedema. Its clinical validity as well as its legitimacy is thoroughly reviewed in the two previous sections: Section VI (Physical and Medical Management) and Section VII (Practical issues in the Physiotherapeutic Approach to Lymphedema).
Because of the ease of availability and accessibility, in addition to having no risk to add «harm» to an already deranged lymphatic system, its value has been overestimated as the sole treatment modality for long-term management. Unfortunately, one crucial aspect of DLT has been neglected: «DLT is neither a panacea nor a curative method.» It is only effective in slowing progression at best and never restores the lost function. This remains its Achilles heel. When DLT is discontinued, the lymphedematous condition deteriorates often at a faster rate, requiring a lifetime commitment that, again, only slows progression.
Such reliance on DLT-based therapy was partly due to the old concept that chronic lymphedema is a simple «static» condition characterized by soft tissue swelling of the affected limb/region after blockage of the lymph-transporting/collecting system. Chronic lymphedema is not a static condition but is actually a steadily progressing condition independent of the efficacy of DLT [12,13,14,15].
Chronic lymphedema is a «continuously changing» condition of degenerative and inflammatory processes involving the skin and soft tissue in addition to the lymphatic vessels and lymph nodes. This condition is characterized clinically by recurrent episodes of dermatolymphoadenitis, resulting in diffuse, irreversible tissue fibrosis. What began as a simple phenomenon of accumulation of lymph fluid eventually becomes a disabling and distressing limb condition affecting the entire surrounding soft tissue beyond the lymphatic system.
With a better understanding of the disease process, contemporary treatment of lymphedema has evolved into an approach that is focused on strategies aimed at preserving and improving quality of life for better social, functional, and psychological adaptation in addition to the control of the lymphatic disorder [3,4,5, 16].
Various surgical treatments introduced throughout the last century, especially for curative and reconstructive purposes, were revisited with different points of view in order to improve patient quality of life [17,18,19,20]. The role of reconstructive lymphatic surgery has also changed in that its new, different role is focused more to provide improvement of patient quality of life as a whole [21,22,23,24]. Detailed information regarding these reconstructive surgical treatments is further reviewed through eight other chapters in Section VIII.
Despite reconstructive surgery having been known to be the ideal treatment to restore normal lymphatic function with a chance of a «cure» for decades, this unique treatment modality still remains controversial mainly because of poor reproducibility and a wide variety of mixed outcomes. The mixed outcomes are most likely due to the variation in the selection of patients and variability in the indications for treatment by different surgical teams in different countries [2, 24, 25].
Among the various criteria required for successful outcome, the «optimal timing» of the surgical procedure has been recognized as the most critical factor not only for immediate success but also for its long-term durability. New knowledge of lymphodynamics and autonomous peristaltic propulsion by the «lymphangion» system once again confirmed how critical the «optimal timing» of surgery is in order to relieve the lymphatic obstruction before permanent damage occurs [2, 25].
Reconstructive surgery is only successful when performed at the «earlier» stage of chronic lymphedema, before residual lymphatic vessels are damaged by prolonged lymphatic hypertension. Injured lymphatic vessels (not yet destroyed) can be effectively rejuvenated and restored to normal function by continuous MLD-based DLT postoperatively.
Reconstructive surgery is, therefore, most effective when performed in the earlier stage of lymphedema, when residual lymphatic vessels remain functionally intact with the ability to relieve lymphatic obstruction and lymph stasis after successful lymphatic reconstruction.
Nevertheless, in reality, the majority of «ideal» lymphatic reconstruction candidates are never offered timely intervention when the residual lymphatic system is still salvageable and are, instead, treated with DLT. When reconstructive lymphatic surgery is belatedly considered, it is often after the window of opportunity has already passed and the patient is left with an unsalvageable condition with damaged and paralyzed lymphatic vessels.
Furthermore, reconstructive surgery requires a commitment by a multidisciplinary team in order to achieve and maintain successful long-term results. Reconstructive lymphatic surgery requires a dedicated and experienced microsurgical team (e.g., lymphovenous and lympho-lymphatic anastomosis). Such an undertaking requires significant resources that are often far beyond what is available at the majority of many capable medical institutes.
Assessment of lymphatic function in lymphedema patients who are potential reconstructive candidates relies heavily on radionuclide lymphoscintigraphy. The current status of lymphoscintigraphy is far from perfect in providing adequate data to allow determination of the feasibility and subsequent planning of lymphatic reconstruction [10, 26,27,28]. Lately, MR lymphangiography and indocyanine green lymphangiography may provide high-resolution imaging required for planning lymphatic reconstruction [29,30,31,32].
This ideal treatment has been extremely limited to a few select patients. Although there is no doubt that it is more theoretically sound than DLT, with a definite chance of a «cure,» it is still far from being a practical treatment in the day-to-day management of chronic lymphedema. Nevertheless, through the last decade, many consider a new role of reconstructive surgery to serve as a supplemental therapy to augment DLT-based physical therapy in lymphedema patients described as poor responders [1, 2, 7].
Lately, reconstructive surgery is limited to lymphedema patients who are determined to be poor to nonresponders to conventional DLT-based treatment. Since DLT-based treatment is invariably effective in the majority of chronic lymphedema patients, the recommendation has been to delay surgical therapy until DLT-based therapy has been maximized with no further improvement. In reality, however, reconstructive surgery is often recommended by a multidisciplinary care team only after properly documenting that the patient has failed extensive DLT, is determined to be a «treatment failure,» and has experienced steady progression of the disease for at least 2 years.
Lymphedema patients where maximal DLT-based therapy has failed are then considered for additional reconstructive surgical therapy. These patients are typically clinical stage II or III, based on our experience. This stage of lymphedema is generally too advanced and is long after the ideal time period for reconstructive surgery to be curative [1, 2, 7].
Therefore reconstructive surgery, when limited to a «supplemental role» in the management of lymphedema in the poor to nonresponding group of DLT patients, is often doomed to fail from the outset. Lymphatic reconstructive surgery is now offered as an adjunctive treatment in the management of lymphedema along with DLT-based treatment since both treatment modalities have mutually complementary effects.
Reconstructive surgical therapy requires maintenance DLT to allow the treated lymphatic vessels to regain its function after being in a «paralyzed» condition. The success of reconstructive surgical therapy in this situation is totally dependent on patient compliance with postoperative DLT [1, 2, 7].
Patient compliance with lifelong maintenance DLT is the single most important factor that directly influences the long-term results of reconstructive surgical therapy. A comprehensive treatment plan incorporating both surgical and postoperative maintenance treatment modalities as part of a multidisciplinary approach will produce the most effective results. The various modes of surgical therapy have recently been found to be more effective when combined with DLT.
1 Clinical Experiences (Personal)
Among 1065 lymphedema patients (131 males and 934 females, 259 primary and 806 secondary, age range 2 months to 82 years), a total of 32 patients were selected for lymphovenous anastomotic surgery (LVAS; n = 19 patients) and free lymph node transplant surgery (FLTS; n = 13 patients), during a 10-year period (January 1995 to December 2004) [1, 7, 21, 22].
All 32 patients were selected due to failure of DLT alone to relieve intractable symptoms with various indications. Various noninvasive tests including lymphoscintigraphy were performed to determine clinical and laboratory staging in all surgical candidates.
The inclusion criteria and indications for reconstructive surgery were:
-
Failure to respond to therapy at clinical stage I or II
-
Progression of the disease to an advanced stage (e.g., stage I to stage II, or stage II to stage III) in the setting of DLT-based treatment
-
Chylo-reflux combined extremity lymphedema
-
High recurrence of local and systemic infection
-
Poor tolerance to DLT-based conservative treatment
We never initiated the surgery as the primary mode of therapy. We selected various reconstructive surgical therapies as a supplemental treatment to DLT.
For lymphovenous anastomotic surgery (LVAS), the candidates were offered the surgery when DLT-based treatment failed or when it was not sufficient to prevent the rapid progression of the disease: clinical stages I to II, or early stage II to late stage II.
All patients selected met all the inclusion criteria for this additional treatment, particularly among the «secondary» lymphedema patients. Nineteen patients (mean age 49 years; female =18, male =1; primary =4, secondary =15) underwent a minimum of 3–4 anastomoses between healthy, well-functioning collecting lymph vessels and competent branches of the saphenous vein.
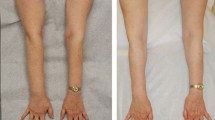
At 6 months, 16 out of 19 LVAS patients with good compliance to maintain postoperative MLD/compression therapy had clinically satisfactory improvement, while the other noncompliant 3 failed. At 24 months, 8 out of 16 were compliant and 8 were not. The noncompliant patients showed progressive deterioration, while the compliant patients maintained their improvement.
At 48 months, 2 out of the 8 compliant patients dropped out. Three of the remaining 6 maintained satisfactory clinical and lymphoscintigraphic improvement.
For free lymph node transplant surgery (FLTS), candidates were selected based on the same indications as for LVAS but the priority for «primary» lymphedema with progress from clinical stages II to III. Thirteen patients (mean age 34 years; female = 10, male = 3; primary =6, secondary =7) at clinical stages II or III underwent FLTS using a microsurgical free grafting technique when LVAS could not be performed.
At 12 months, 10 of the 13 FLTS patients with good compliance to MLD showed clinical improvement with a successful graft, but the remaining 2 with poor compliance with the MLD failed.
At 24 months, 8 patients were compliant and 5 were not. Compliant patients maintained clinical improvement while the remaining noncompliant patients showed progressive deterioration.
Conclusion
Reconstructive lymphatic surgery is the best option for the treatment of chronic lymphedema when performed at the optimal time. It is also a viable treatment option for lymphedema patients who have failed to respond to DLT alone. Postoperative DLT and compression therapy are required as supplemental therapy in the group of poor responders to DLT. Postoperative DLT is even more important when performing lymphatic surgery at a less ideal, later stage of lymphedema.
Long-term patient compliance with DLT and compression therapy is absolutely essential for satisfactory clinical improvement and maintenance following reconstructive lymphatic surgery. This is especially true in the group of patients who are poor responders to DLT therapy alone.
Highlighted References
Lee BB. Current issue in management of chronic lymphedema: personal reflection on an experience with 1065 patients. Lymphology. 2005;38:28.
Lee BB, Andrade M, Antignani PL, Boccardo F, Bunke N, Campisi C, Damstra R, Flour M, Forner-Cordero J, Gloviczki P, Laredo J, Partsch H, Piller N, Michelini S, Mortimer P, Rabe E, Rockson S, Scuderi A, Szolnoky G, Villavicencio JL. Diagnosis and Treatment of Primary Lymphedema. Consensus Document of the International Union of Phlebology (IUP)-2013. Int Angiol. 2013;32(6):541–74.
Lee BB. Surgical management of lymphedema. In: Tredbar LL, Morgan CL, Lee BB, Simonian SJ, Blondeau B, eds. Lymphedema—diagnosis and treatment. London: Springer; 2008:55–63, chap 6.
Lee BB, Kim YW, Kim DI, Hwang JH, Laredo J, Neville R. Supplemental surgical treatment to end stage (stage IV –V) of chronic lymphedema. Int Angiol. 2008;27(5):389–95.
Lee BB, Laredo J. Pathophysiology of Primary Lymphedema. Chapter 12. In: Neligan PC, Piller NB, Masia J, editors. Complete medical and surgical management. Boca Raton: CRC Press; 2016a. p. 177–88.
References
Lee BB. Chronic lymphedema, no more step child to modern medicine! Eur J Lymphol. 2004;14(42):6–12.
Lee BB, Kim DI, Whang JH, Lee KW. Contemporary management of chronic lymphedema – personal experiences. Lymphology. 2002;35(suppl):450–5.
Foldi E, Foldi M, Weissletter H. Conservative treatment of lymphedema of the limbs. Angiology. 1985;36:171–80.
Hwang JH, Lee KW, Chang DY, et al. Complex physical therapy for lymphedema. J Kor Acad Rehabil Med. 1998;22:224–9.
Hwang JH, Kwon JY, Lee KW, et al. Changes in lymphatic function after complex physical therapy for lymphedema. Lymphology. 1999;32:15–21.
Leduc O, Bourgeois P, Leduc A. Manual of lymphatic drainage: scintigraphic demonstration of its efficacy on colloidal protein reabsorption. In: Partsch H, editor. Progress in Lymphology IX. Amsterdam: Elsevier/Excerpta Medica; 1988.
Foldi E. Prevention of dermatolymphangioadenitis by combined physiotherapy of the swollen arm after treatment for breast cancer. Lymphology. 1996;29:48–9.
Choi JY, Hwang JH, Park JM, et al. Risk assessment of dermatolymphangioadenitis by lymphoscintigraphy in patients with lower extremity lymphedema. Korean J Nucl Med. 1999a;33(2):143–51.
Olszewski WL. Episodic dermatolymphangioadenitis (DLA) in patients with lymphedema of the lower extremities before and after administration of benzathine penicillin: a preliminary study. Lymphology. 1996;29:126–31.
Lee BB, Bergan JJ. New clinical and laboratory staging systems to improve management of chronic lymphedema. Lymphology. 2005;38(3):122–9.
Lee BB, Laredo J, Neville R. Combined clinical and laboratory (Lymphoscintigraphic) staging. chapter 13. section IV – clinical diagnosis, page 97–104. In: Byung-Boong L, Bergan J, Rockson, Stanley G, editors. LYMPHEDEMA: a concise compendium of theory and practice. 1st ed. London: Springer; 2011a.
Baumeister RGH, Siuda S. Treatment of lymphedemas by microsurgical lymphatic grafting: What is proved? Plast Reconstr Surg. 1990;85:64–74.
Becker C, Hidden G, Godart S, et al. Free lymphatic transplant. Eur J Lymphol. 1991;6:75–80.
Krylov VS, Milanov NO, Abalmasov KG, Sandrikov VA, Sadovnikov VI. Reconstructive microsurgery in treatment of lymphoedema in extremities. Int Angiol. 1985;4(2):171–5.
Campisi C, Boccardo F, Zilli A, Maccio A, Napoli F. Long-term results after lymphatic-venous anastomoses for the treatment of obstructive lymphedema. Microsurgery. 2001;21(4):135–9.
Lee BB, Laredo J, Neville R. Reconstructive surgery for chronic lymphedema: a viable option, but. Vascular. 2011b;19(4):195–205.
Lee BB, Laredo J, Neville R. Current Status of Lymphatic Reconstructive Surgery for Chronic Lymphedema: It Is Still an Uphill Battle! Int J Angiol. 2011c;20(2):73–9.
Gloviczki P, Fisher J, Hollier LH, Pairolero PC, Schirger A, Wahner HW. Microsurgical lymphovenous anastomosis for treatment of lymphedema: a critical review. J Vasc Surg. 1988;7(5):647–52.
Gloviczki P. Review. Principles of surgical treatment of chronic lymphoedema. Int Angiol. 1999;18(1):42–6.
Lee BB, Andrade M, Bergan J, Boccardo F, Campisi C, Damstra R, Flour M, Gloviczki P, Laredo J, Piller N, Michelini S, Mortimer P, Villavicencio JL. Diagnosis and treatment of Primary Lymphedema - Consensus Document of the International Union of Phlebology (IUP)-2009. Int Angiol. 2010 Oct;29(5):454–70.
Lee BB, Laredo J. Radionuclide Lymphoscintigraphy. Chapter 26. In: Neligan PC, Piller NB, Masia J, editors. Complete medical and surgical management. Boca Raton, FL: CRC Press; 2016b. p. 349–64.
Lee BB, Laredo J. Contemporary role of lymphoscintigraphy: we can no longer afford to ignore! Editorial. Phlebology. 2011;26:177–8.
Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med. 2003;44(1):43–57.
Liu NF, Lu Q, Wu XF. Comparison of radionuclide lymphoscintigraphy and dynamic magnetic resonance lymphangiography for investigating extremity lymphoedema. Br J Surg. 2010;97:359–65.
Liu NF, Lu Q, Jiang ZH. Anatomic and functional evaluation of lymphatics and lymph nodes in diagnosis of lymphatic circulation disorders with contrast magnetic resonance lymphangiography. J Vasc Surg. 2009;49:980–7.
Yamamoto T, Koshima I. Splash, Stardust, or Diffuse pattern: differentiation of dermal backflow pattern is important in indocyanine green lymphography. Plast Reconstr Surg. 2014;133(6):e887–8.
Yamamoto T, Narushima M, Doi K, Oshima A, Ogata F, Mihara M, Koshima I, Mundinger GS. Characteristic indocyanine green lymphography findings in lower extremity lymphedema: the generation of a novel lymphedema severity staging system using dermal backflow patterns. Plast Reconstr Surg. 2011;127(5):1979–86.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Lee, BB., Laredo, J. (2018). Current Dilemmas and Controversies in Reconstructive Surgery for Lymphedema. In: Lee, BB., Rockson, S., Bergan, J. (eds) Lymphedema. Springer, Cham. https://doi.org/10.1007/978-3-319-52423-8_52
Download citation
DOI: https://doi.org/10.1007/978-3-319-52423-8_52
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52421-4
Online ISBN: 978-3-319-52423-8
eBook Packages: MedicineMedicine (R0)