Abstract
Virtual reality (VR) provides a unique platform to study the complex interactions between an individual’s movement and their environment. Although this innovative technology has not yet been widely used in Parkinson’s disease (PD) research, it has tremendous potential to advance both our understanding and treatment of gait impairments. In this chapter, we will first outline the variety of virtual reality systems available and contrast the associated advantages and disadvantages that warrant consideration for using virtual reality in experimental and/or therapeutic settings. We will then discuss the utility of VR in the scientific exploration of mechanisms that underlie gait impairments in PD. Finally, we will examine the effectiveness of using VR in a therapeutic setting based on the current research, and provide future directions for therapeutic interventions for gait in PD utilizing virtual reality.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Assessing the Utility of Virtual Reality
Virtual reality can be defined as a high quality computer interface which enables a person to interact with a virtual environment generated by a computer in real-time [1]. Similar to the real world, where we explore our environment with our senses, a virtual environment (VE) offers many comparable perceptual experiences, where our senses are able to gather information using vision, auditory, and somatosensory feedback. This information from the virtual environment, in combination with natural sensory (e.g., proprioception) inputs, is then used to guide movement within the virtual environment, and in most instances creates an immersive and realistic virtual experience for the user [1, 2]. Due to the compelling reality that an interactive and immersive virtual experience can elicit, this tool allows investigators to move beyond traditional laboratory experiments which focus on a specific component of behavior (in an artificial setting), and begins to examine the complexity of the brain and resultant behavior in a way that it is much closer to its actual form.
The key elements that contribute to an immersive virtual experience are: (1) delivering a 3-dimensional high-resolution image which incorporates stereoscopic display, and (2) integrating the user’s movement (using a movement tracking system) to display relevant sensory feedback about movement in real-time. Without these key elements, a less immersive experience is achieved that is more akin to looking through a window and observing a scene rather than being present and involved [1]. Therefore, the quality of the virtual reality system utilized will have an impact on the immersive presence that can be elicited (see Table 25.1, for examples of different virtual reality systems).
For example, a head-mounted display that allows stereoscopic viewing paired with motion tracking that simulates movement in the VE will provide a much more immersive sensory experience for the user compared to a 2-D computer display monitor with a mouse/keyboard to navigate a virtual environment. Nonetheless both systems (and everything in between) have advantages and disadvantages that should be weighed and considered. While the latter is convenient, easy to use/setup, relatively cheap, less likely to produce cybersickness (a form of motion-sickness that can occur as a result of VR), without a motion tracking system it has limited utility for the study of gait since it lacks the most relevant feedback (i.e., vision, proprioception, vestibular). Recent research has advanced this more basic virtual reality setup by constructing toe tapping pedals that were paired with a desktop monitor to facilitate the study of “gait” in virtual reality [3–5]. Although pressing pedals does not simulate the complexities of walking, it provided an opportunity to examine “gait” in virtual reality while simultaneously capturing functional magnetic resonance imaging or recording electroencephalography in order to study the neural underpinnings of severe gait impairments in PD. Interacting with a projection on the floor, such as walking to step over virtual obstacles or transverse lines, is another relatively cheap, convenient, and easy to use format of virtual reality, although might be argued to be less immersive since it remains heavily rooted in the real-world rather than being surrounded and moving through a virtual environment. Finally, a wireless head-mounted display (HMD) with motion tracking (e.g., vicom, optotrak, wearable accelerometers) is arguably the most immersive virtual experience one can achieve. It allows stereoscopic 3-dimensional viewing achieved with small monitors in front of each eye. Additionally, the user’s viewpoint can be synchronized to their head movement so that the user can explore the entire environment by “looking” and moving around. When paired with full body kinematics, avatars can be used to represent the person’s body position and movements in real-time providing even more detailed feedback about self-motion. Thus, the HMD virtual reality system can provide rich sensory feedback making the user’s virtual experiences strikingly immersive. However, this system is also more likely to result in greater cybersickness due its intensity [6, 7], and is problematic for individuals with PD that have dyskinesia or severe head tremor since this excessive movement would disrupt one’s ability to view the virtual environment and cause even greater cybersickness.
In addition to the features and limitations inherent to the virtual reality system, there are also many strengths from both an experimental and therapeutic perspective that makes virtual reality a sought after technology to investigate and rehabilitate gait in PD. Experimentally, virtual reality brings ease in creating controlled and safe, yet complex and dynamic environments and also extends the capabilities that the real world limits. For example, it is possible to:
-
Create busy sidewalks for individuals to navigate through (which might normally be very difficult to capture rich kinematic data)
-
Create stressful situations in order to observe how/whether gait breaks down (which would normally be potentially dangerous to perform in the real-world)
-
Provoke gait impairments which are typically difficult to elicit in experimental settings (such as freezing of gait)
-
Quantify information processing of stimuli and other cognitive processes, while walking in ecologically valid virtual environments which resemble tasks of daily living
-
Isolate, manipulate and even reweight sensory systems, or provide faulty sensory feedback (which can be insightful in trying to further understand visual control or sensorimotor integration necessary for adequate gait control).
Overall, interactions in virtual reality maximize gait and cognition simultaneously (e.g., requiring planning, attention, information processing of stimuli in the virtual environment, sensory integration) [1, 2, 8–10] (see Fig. 25.1), which is why this novel and innovative technology has the potential to advance the understanding of gait impairments.
Therapeutically, virtual reality offers many additional perks. Beyond being safe and affordable, training in virtual reality has been argued to provide similar if not greater benefits when contrasted with real-world equivalent training programs [1, 2, 8, 11–14]. These greater benefits have been suggested to result from enhanced motor learning through the use of augmented feedback, knowledge of performance, and knowledge of results which virtual reality can easily capitalize and exploit. Some additional reasons virtual reality may be superior are that it often eliminates distracting elements that are difficult to escape in rehab settings, it can be delivered in a personalized manner—adapted for those who need it, and it could even be delivered within the home by using gaming consoles. Therefore, virtual reality may also be a valuable rehabilitative tool for gait interventions in PD.
2 Using Virtual Reality to Understand Underlying Mechanisms of Gait Impairments in Parkinson’s Disease
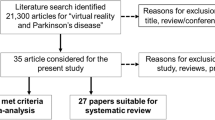
Although limited research has utilized virtual reality to study gait in PD, there has been three main arms of scientific investigation that have benefitted from this innovative technology which has contributed to the advancement in understanding underlying mechanisms of gait impairments in Parkinson’s disease. The first has focused on understanding the role of sensory feedback and examining deficits in sensorimotor integration which might contribute to gait impairments in PD. The second has examined how gait deficits are exacerbated in complex situations which require additional cognitive abilities (such as planning, attention, and task-switching) or interpretation of environmental demands (such as obstacles or threatening situations). The final contribution has arguably had the most dramatic impact on the understanding of a severe gait phenomenon, known as freezing of gait (FOG) , commonly experienced in PD (and thus received a substantial amount of attention in this chapter). Although the underlying cause and mechanism of freezing of gait remains unknown, virtual reality paired with brain imaging techniques such as fMRI and EEG has allowed research to make gigantic leaps in understanding FOG and developing devices to predict or prevent FOG episodes altogether.
2.1 Visual Control and Sensorimotor Integration During Gait
It has been well-established that individuals with PD are highly dependent on vision, particularly dynamic visual information (i.e., optic flow) during locomotion [15–19]. This excessive dependence on visual feedback during gait in PD has been suggested to reflect abnormal sensorimotor integration as a result of the disease [20–23]. Evidence of this has been provided by early studies which examined PD patients walking on a treadmill at a trained pace while manipulating the optic flow speed using virtual reality [24, 25]. In healthy older adults it is expected that increases in optic flow will lead to increases in gait speed, but eventually individuals demonstrate an adaptive shift in dependence from visual to proprioceptive feedback due to the “false” information delivered through VR [24]. Individuals with PD, however, demonstrate an exaggerated response in relation to changes in optic flow, which provides additional support that PD has increased susceptibility to depend on visual information to modulate gait [18]. There was also little evidence that PD patients actually reweighted visual and proprioceptive feedback like healthy older adults did. Instead, many PD did not even notice the incongruity, leading the authors to conclude that a discrepancy between the two kinesthetic signals (optic flow and proprioception) was likely already present. Corroborating these findings, another virtual reality study (utilizing HMD with kinematic movement tracking) manipulated optic flow speed in effort to further understand whether sensory-perceptual information contributed to gait impairments [26]. Previous research has noted that individuals with PD show distance estimation deficits only when required to walk to a target (compared to pointing or being passively moved with VR or in a wheelchair) [27, 28]. A follow-up study was done to disentangle whether delayed perceptual processing versus corrupt sensory integration was responsible for impairments in self-motion perception during gait. Similar to Schubert and colleagues, optic flow speed was increased and decreased relative to the participants’ gait speed; however, PD participants did not notice the discrepancy between the various forms of sensory feedback [26]. More interestingly, the study found that decoupling sensory feedback made older adults perform similarly to PD, in fact speeding up the optic flow speed made older adults display similar judgment accuracy and variability as PD at baseline (when optic flow matched gait speed). However, decoupling did not significantly influence PD participants’ estimations [26]. Taken together, these research studies (amongst others) suggest that proprioceptive deficits along with delayed sensory processing result in a mismatch of competing sensory information which not only disrupts normal sensorimotor integration in PD, but the erroneous signal (proprioception) eventually becomes suppressed in favor of the more appropriate information (vision), and gait suffers and is more vulnerable [24, 26, 27].
Other researchers have also used virtual reality to exploit visuoperceptual deficits such as impaired perception of optic flow [17, 29]. It has been argued that asymmetrical dopamine levels between the brain hemispheres might lead to the compression of one visual field more than the other (depending on side of asymmetry) [29]. As a result of this asymmetrical compression of the visual field, individuals with PD can misperceive optic flow since it appears that one hemi-field is moving faster than the other, and thus misrepresenting the speed of movement and heading [17, 29, 30]. Nonetheless PD participants are still highly dependent on optic flow to control gait, such that when the richness in optic flow information was reduced (Fig. 25.2), gait in PD was also shown to worsen (i.e., slower and smaller steps) [29]. Considering that even the visual form of kinesthesia (optic flow) may be disrupted in PD, and knowing how heavily individuals with PD rely on vision during gait to compensate for proprioceptive deficits, it is not surprising that these sensory-perceptual impairments could play a primary role in the breakdown of gait and balance in PD. Furthermore, accurate sensory feedback is essential for gait planning, selecting the correct motor program, making online gait adjustments, and correctly distributing attention. Taken together, gait impairments may become only more problematic when faced with navigating complex and threatening environments.
A virtual hallway where optic flow speed was manipulated separately on the right wall from the left wall, but dot density was equal (a); whereas (b) shows a manipulation of optic flow richness, where the dot density is significantly less on the left wall compared to the right. (Adopted from: [29])
2.2 Gait in Complex Environments
One of the key features of virtual reality is that it provides an ecologically valid platform for cognition and movement to be assessed and further understand how they interact in PD. Up until recently, cognitive functions were primarily assessed with pen and pencil type assessments which not only lacked the complexity of the everyday world and thus lacked ecologic validity [31, 32], but they are also limited in the generalizability and meaningfulness of their findings to reflect the capabilities in tasks of daily living [33]. For this reason, researchers have utilized virtual reality to create “everyday” environments in order to assess daily tasks that include different cognitive functions [32–34]. For example, one study constructed a virtual supermarket where participants were given a grocery list of items that needed to be bought (Fig. 25.3) [34]. This type of task focused on evaluating action planning, and showed that individuals with PD needed more time to execute this task (even though they moved at a constant speed using a joystick), covered a longer distance, and made more hesitations and stops. The authors concluded that this behavior demonstrated that individuals with PD had slower action planning, and were often inefficient at using contextual elements in the environment to aid the search for products. A similar paradigm was also employed where participants were asked to “walk” around an apartment (viewing the VE in a helmet and moving using a joystick) remembering objects and rooms that they had viewed in order to estimate cognition [32]. Interestingly, virtual narrow spaces were found to exaggerate reduced speeds in early non-freezing PD participants (even though they were not actually walking), something commonly seen in the real-world in PD and known to provoke FOG. Although this research has great potential in improving the assessment of cognition in a more ecological manner, more research studies are needed to know whether this will be useful, reliable, and clinically meaningful. Once this is established it would be useful to use these cognitive tasks to assess and quantify changes in gait in order to understand gait impairments outside of the laboratory and potentially prevent falls that are common in the home.
An example of the virtual environment used in the virtual multiple errands test . (Adopted from: [33])
Gait in PD has been shown to deteriorate in more complex situations which encompass a threat or secondary tasks, for example. The current theory as to why individuals with PD are so susceptible to interference in these more complex environments goes back to how PD consciously monitor and control gait with vision as a compensatory strategy to deal with the loss of useful proprioceptive feedback which is necessary for gait to be automatic. Because PD patients constantly having to pay attention to their walking , it has been proposed that this limits their attentional capacity to do other tasks and monitor other relevant information in the environment. By using virtual reality to create a carefully controlled complex environment, one can evaluate aspects of gait that are susceptible to interference and make recommendations for therapeutic interventions.
Stressful situations are commonly reported to elicit gait problems, falls, and freezing of gait in PD. In a series of studies, virtual reality was used to create a stressful and “virtually dangerous” environment to understand if and how threat/ anxiety influenced gait in PD and whether dopaminergic replacement therapy mediated this relationship [35–38]. These studies were performed using an HMD integrated with full body kinematics. Participants were asked to walk in virtual environments with and without threat (i.e., across an elevated plank versus a plank located on the ground) (Fig. 25.4). Across all studies, all participants (PD and healthy older adults) had greater levels of anxiety (self-reported and skin conductance levels) when they walked across the elevated plank compared to the plank on the ground. All participants also walked with a slower velocity, smaller steps, and greater step-to-step variability across the elevated compared to the ground plank. These findings were similar to what has been found when older adults were asked to walk across an elevated plank in the real-world, confirming that the experimental manipulation of threat with VR was effective, immersive, and realistic enough to elicit more cautious gait. The most interesting results of this work found that the elevated plank provoked a greater number of freezing of gait episodes in PD freezers and significantly more variable gait specifically in freezers compared to non-freezers [38] and in those with PD who had high trait anxiety (non-freezers) compared to those with PD who had low trait anxiety (non-freezers) and healthy older adults [35, 36]. Highly trait anxious PD also appeared to be less able to use visual feedback about their lower limbs when it was provided to improve gait, especially when walking across the elevated plank [35]. Notably, the frequency of FOG in freezers and step-to-step variability (among other gait parameters) in highly trait anxious PD were improved with dopaminergic replacement therapy [35, 36, 38]. Furthermore, dopaminergic medication also improved step time variability in highly trait anxious PD when visual feedback about their lower limbs was available. Taken together, this research provided strong evidence to suggest that anxiety influenced PD gait, possibly by demanding shared processing resources at the level of the basal ganglia, which may interfere with other processes (such as processing sensory feedback) necessary to control gait [39]. Researchers postulated that dopaminergic replacement therapy might have improved information processing within the basal ganglia and thus alleviated some of the interference due to the competition for shared resources [40]. In conclusion, this VR approach allowed investigators to evaluate the impact anxiety has on gait in PD, and offer a mechanistic explanation for how anxiety exacerbates gait impairments in PD. Overall, walking in threatening environments likely demands greater voluntary control and as result also demands more attentional resources (similar to being distracted by a dual-task while walking), however, given the limited resources available in individuals with PD, anxiety and threatening environments may overload the system and manifest gait deficits.
Virtual environments that have been used to induce anxiety by asking participants to walk across a plank that is located on the ground (a) compared to a plank located above a deep pit (b). Virtual visual feedback about the lower limbs was also manipulated (c, d) and synchronized using a full kinematic motion tracking system. (Adopted from: [41])
2.3 Using VR to Uncover Neural Correlates of Freezing of Gait
Other studies have used a VE that requires participants to navigate a virtual corridor using binary response buttons while performing a modified stop-signal task to elicit a behavioral surrogate of FOG that occurs in either the hands [42] or feet [4, 5]. Although the task does not require balance, postural adjustments, or utilization of the muscles of the upper legs, by manipulating cognitive and perceptual load (through the administration of a complex stop-signal task and through the navigation of embedded narrow doorways, respectively), the task (displayed in Fig. 25.5) has been shown to elicit many of the known clinical characteristics of FOG, including paroxysmal cessations in ankle flexion [5], heightened step-to-step variability [3], and worsening of motor output in the presence of cognitive [43] and perceptual load [44].
An example of the virtual environment used during fMRI . The configuration of the foot pedals is shown in the top right corner inset which enabled a simulation of virtual “gait.” The bottom image depicts the varying complexity of the task/cues and an example of a patient’s footstep pattern as these cues are presented. (Adopted from: [5])
Importantly, the gait-based VE has been successfully combined with functional neuroimaging to improve our understanding of the neural mechanisms underlying the manifestation of freezing behavior. In an early fMRI study, Shine and colleagues contrasted paroxysmal freezing episodes with epochs of normal “walking,” and found that episodes of freezing were related to an increased BOLD response in prefrontal cortical regions, with a decreased BOLD response in motor cortex and bilateral striatum [45]. These results suggested the hypothesis that freezing of gait is related to impaired functional connectivity between the striatum and frontoparietal cortex, a prediction that was later confirmed using the same VE task [46] in combination with a novel method for estimating fluctuations in coupling strength between neural regions over time [47]. Subsequently, the same VE paradigm was used to delineate the patterns of abnormal BOLD response associated with cognitive load [48] and the completion of turns [49], both of which are known to exacerbate freezing episodes in susceptible individuals [50]. Together, these results highlight the importance of utilizing VE tasks to understand symptoms of neurodegenerative disorders that would otherwise be difficult to interrogate using neuroimaging analyses.
In sum, it should be emphasized that virtual reality has advanced researchers’ ability to examine more complex gait as well as cognition in greater detail than ever before. In the last decade, these lines of research have provided data that has helped progress the current understanding of gait impairments in PD, and also re-assess existing pathophysiological models of gait deficits (such as freezing). For example, prior to examining gait with fMRI , mechanisms underlying freezing of gait were initially discussed using broad concepts such as executive dysfunction, sensory-perceptual deficits, decoupling of anticipatory postural adjustments, and so on (see these reviews for more detail [50, 51]). In fact, only in the past decade have various hypotheses begun to incorporate more detailed levels of neurobiology and consideration for damaged circuitry. One of the most widely accepted theoretical views focuses primarily on the dopaminergic depletion within the basal ganglia, which was theorized to limit information processing of complementary yet competing inputs from different cortico-striatal pathways (see Fig. 25.6). However, after taking into consideration recent neuroimaging findings that highlight reduced functional connectivity and decoupling between key neural networks during virtual gait, researchers have revised theoretical models of gait impairment in PD to be more sophisticated [52], and identified a key paradigm shift that is necessary in order to fully understand underlying neural mechanisms of gait (Fig. 25.6a, b). Therefore, virtual reality has played a tremendous role in advancing our understanding mechanisms of gait impairments in PD.
A schematic illustrating a paradigm shift from previously focusing on faulty circuitry underlying gait abnormalities in PD towards understanding functional connectivity between neural networks which underlie gait impairments in PD (e.g., FOG). Note the abbreviations: SMA supplementary motor area, GPi globus pallidus interna, SNr substantia nigra reticulate, PPN pedunculopontine nucleus, OFC orbitofrontal cortex, NAcc nucleus accumbens, DLPFC dorsal lateral prefrontal cortex
3 Rehabilitating Gait in Parkinson’s Disease with Virtual Reality
As our understanding of gait deficits in PD becomes more comprehensive, the ultimate goal of this research is to translate the current knowledge about mechanisms underlying gait impairment into novel therapeutic interventions that will effectively improve gait in PD. One way to facilitate this translation is to create rehabilitative strategies that focus on improving or overcoming contributing factors by entraining the brain to either repair itself or compensate in through some form of neuroplasticity to restore function. As stated above, one mechanism that VR has highlighted is the role of sensory feedback and sensorimotor integration on gait. Complex situations which require cognitive abilities (planning, attention, task-switching, etc.), or interpretation of environmental demands (obstacles, threat), are also known to exacerbate gait deficits in PD. Based on these findings, recent therapeutic strategies have focused primarily in two domains: (1) sensory cueing and (2) intense motor-cognitive training (i.e., walking with continuous cognitive tasks). In recent years, by utilizing virtual reality, research has advanced therapeutic interventions and their efficacy. For example, research has shown that visual and auditory cue training is more effective when delivered in an integrated feedback fashion (e.g., closed-loop) rather than being feedforward (e.g., open-loop), which has been shown to be less effective [53, 54]. VR provides an easy, consistent, and controlled method to maximize gait and cognition simultaneously [1, 2, 8, 32, 55]. Another advantage of virtual reality is the way in which training can be implemented. It creates a fun, “game-like” atmosphere that is enjoyable and conducive to high adherence. Training in VR has even been suggested to be superior compared to real-world equivalent training programs [1, 2, 8, 11–14], since it capitalizes on principles of motor learning with enhanced and immersive feedback (such as auditory and visual feedback of successful and unsuccessful performance). This was confirmed by a recent Cochrane review which favored VR therapeutic approaches for stroke rehabilitation compared to conventional therapies [56]. Difficulty and intensity of training programs can also be easily modulated with a VR format by increasing number of stimuli, distractors, and speed, which are difficult to control and manipulate in real-world settings [8]. Finally, one of the major advantages of VR is that training can simulate daily activities. It also enables at-home training, due to the portability and current computing capacity which is capable of measuring and providing performance feedback to users during and following gait training. Overall VR training may be a practical and useful tool to target sensory and cognitive deficits that contribute to gait impairments, and thus provide new opportunities to improve gait, mobility, and ultimately quality of life in those living with PD. In the following sections we will discuss research utilizing virtual reality as a method for therapeutic intervention for gait impairments in PD.
3.1 Using Sensory Cues in VR for Gait Improvement
It has been known for some time now that using sensory cues such as a metronome or transverse lines on the ground can significantly help impaired gait in those with PD, and even alleviate FOG in some instances. The notion that sensory input can help overcome these severe gait deficits suggests that the motor program for gait might be intact but not adequately selected due to sensory impairments in PD [20, 54]. The spinocerebellar, spinothalamic, spinoreticular, and spinohypothalamic tracts carry somatosensory information/feedback (such as proprioception) up to the brain during gait [20, 54], which modulates internal timing that helps to plan and predict future movements. Internal timing has been shown to be disrupted in PD [57], as a result of striatal dopaminergic depletion since the underlying neural networks for internal timing involve the basal ganglia (BG) , supplementary motor area (SMA) , and primary motor cortex (PMC) [58, 59], where the BG serves the most crucial role as it generates the internal pacing required for time estimation [60, 61]. In fact, a reduction in dopaminergic innervation to the BG in PD causes slower internal pacing [60], which manifests impaired motor and perceptual timing abilities [28, 62]. Not surprisingly, research has also shown that internal timing is argued to be more affected among those PD with gait deficits (e.g., freezing of gait) compared to those without [63].
It is important to note that although PD patients have impairments with internal timing, they can still use external cues to inform temporal-based decisions such as when the next footstep should be carried out. The effectiveness of external cues is thought to be due to distinct neural networks underlying internal versus external timing [54]. External timing mainly engages automatic timing systems by recruiting the cerebellum and thus is less dependent on the faulty BG and SMA [64]. Therefore, external cues (such as metronome beats or transverse lines) can serve as a proxy for impaired internal timing [65, 66] and improve gait by inducing motor-sensory feedback signals that recalibrate internal pacing. Virtual reality provides yet another medium to deliver external cues that the BG is unable to effectively generate and thereby repair a key issue that is at the core of gait impairments in PD.
Recently, researchers have begun to develop virtual reality devices that enhance external cues for rehabilitation in both the auditory and visual domains. Although cueing has been used over the past two decades as a helpful therapy for gait in PD, recent advancements in wearable VR technology have improved the efficacy of this rehabilitation strategy. One example is “intelligent glasses ,” designed to be portable and have built-in headphones which enable users to listen to a metronome like auditory cue while walking [67]. In a small study of just ten PD patients these auditory cues have been shown to improve cadence, stride length, and walking speed compared to walking without auditory cues [67]. Likewise, many studies have shown that matching footsteps to visual cues such as transverse lines on the ground or using VR glasses which deliver visual cues while walking on a treadmill improves gait (increased stride length and velocity, while reduced gait variability and FOG) in PD [68–70]. One of the main limitations of fixed-tempo auditory and fixed-equidistant visual cueing is that they require increased attentional demand to synchronize individual footsteps, which imposes a cognitive load and promotes gait breakdown [54, 71, 72]. Additionally, fixed cueing is also easy for the participant to fall out of sequence with the cues, making them less effective and potentially even more problematic, such as provoking FOG [73].
Recent research has argued that these open-loop “fixed-cueing” strategies may not be the most effective for improving gait, since these sensory signals are not generated or affected by the users’ own movement which is arguably a key feature of gait-related feedback [53, 73]. Thus, recent work has begun investigating closed-loop effects of visual cues on the regulation and rehabilitation of gait [73]. Research that directly compared open- and closed-loop visual cues showed that the closed-loop configuration produced nearly twice the improvement in average walking speed and stride length. This led to the conclusions that closed-loop VR systems are more effective at improving gait in PD patients than open-loop versions [73].
WalkMate is a closed-loop device which synchronizes foot pressure sensors to auditory cues. This apparatus appears to be a promising tool based on its ability to reduce gait variability in PD patients [74]. Another recent study used VR glasses to project a virtual checkered floor into the user’s visual field. As the user walks, the VR floor adapts to the user’s body movements by simulating the visual effect of walking [41]. The user’s goal was to match their steps with the adjacent floor tile in order to regulate gait. This closed-loop system also produced encouraging results which demonstrated improvements in walking speed and stride length.
Since limited research has implemented closed-loop VR sensory feedback of whole body movement in locomotion, further research is needed to conduct randomized control trials with sufficient power to stringently evaluate the efficacy of VR-based therapies for PD. It also remains unclear whether current VR interventions have long-lasting effects. Future research should attempt to maximize the effects of cueing by utilizing multi-sensory cueing systems that can provide responsive and dynamic cues in the auditory, visual, and tactile domains [1, 54]. If a multi-sensory and adaptive VR device could respond to patients’ movements, it may also demand less attention which might lead to a superior gait therapy. Research has assessed how receptive the Parkinson’s population would be to this type of virtual reality technology (e.g., smart glasses wearable computers) [75], and overall patients were very enthusiastic about this type of assistive device to facilitate daily living activities.
3.2 Utilizing VR to Challenge Cognitive Functioning During Gait Training
Executive functions play a critical role in the regulation of gait and freezing [76– 78], especially in complex environments where decisions need to be made in real-time [18, 19, 79]. Based on the strong relationship between cognitive functioning and gait impairment, it has been suggested that motor and cognitive training combined are likely to be more efficacious compared to simple gait training or using sensory cues. Instead of training with sensory cues, which consume attention and reduces their capacity to cope with complex situations, motor-cognitive training promotes these situations and provides an opportunity to improve planning, decision making, and online adjustments. For example, dual-tasking (DT) and obstacle negotiation both rely heavily on the availability of ample cognitive resources due to the need for motor planning and visually dependent gait regulation [80, 81]. Thus, it seems reasonable to focus training on improving one’s ability to cope directly with these situations, with the objective of transferring these skills to instances encountered on a daily basis. This is the approach that Mirelman and colleagues took by designing an intense and progressive rehabilitation program. The aim of the program was to promote cognitive processing by monitoring multiple stimuli simultaneously (delivered in VR), while walking and continuously negotiating obstacles on a treadmill [8, 55]. The virtual environment was able to impose varying degrees of cognitive load which demanded attention, response selection, and several perceptual processes, while tracking participants’ foot movements. This training program was performed 3 times per week for 6 weeks, and produced very promising results. Typical gait improvements were found (increased gait speed, stride length, and increased obstacle clearance) which resemble treadmill training without VR imposing a cognitive load [8]. However, the added benefit of training with VR was made evident during evaluation of DT performance at post-test. Dual-task costs improved dramatically after training (31 %) and participants also demonstrated improved performance on the trail making tasks (a test of set-shifting and processing speed). It was suggested that this intense motor-cognitive combined therapy utilizing VR improved gait and also improved attention, set-shifting, and planning, which positively impacted DT ability [8]. These impressive gains were retained for at least 4 weeks after training ceased. Limitations of this study should be noted, since training was performed with a small sample, and a historical control group was used as a comparison rather than active control group.
Finally, a major advantage of virtual reality is the possibility that these motor-cognitive therapeutic interventions could be delivered in a home setting. Off-the-shelf gaming consoles make this idea feasible, relatively cheap, and accessible. For example, the Microsoft Kinect tracks full body motion using an infra-red camera while promoting integrated simulation of motor and cognitive functions. In fact, a recent study assessed the feasibility, safety, and outcomes of playing four existing Kinect Adventures!™ games (which encompass undefined motor and cognitive training) in 7 PD participants [82]. The participants completed fourteen 1-h sessions 3 times per week. The main findings of this study were that the Kinect training was both safe and feasible for patients with Hoehn and Yahr stage 2 and 3 Parkinson’s disease. Additionally, improvements in gaming performance and other gait assessments were also seen, although due to small sample and a lack of control group, no statistical results were reported. Nonetheless this study provides evidence that at-home training, which utilizes virtual reality using gaming software, is feasible and possibly effective for improving gait. However, further research is needed to investigate and develop effective at-home motor-cognitive training programs that are aimed at improving gait.
References
Holden MK. Virtual environments for motor rehabilitation: review. Cyberpsychol Behav. 2005;8:187–211. doi:10.1089/cpb.2005.8.187. discussion 212–9.
Mirelman A, Maidan I, Deutsch JE. Virtual reality an motor imagery: promising tools for assessment and therapy in Parkinson’s disease. Mov Disord. 2013;28:1597–608.
Gilat M, Shine JM, Bolitho SJ, et al. Variability of stepping during a virtual reality paradigm in Parkinson’s disease patients with and without freezing of gait. PLoS One. 2013;8:e66718. doi:10.1371/journal.pone.0066718.
Shine JM, Ward PB, Naismith SL, et al. Utilising functional MRI (fMRI) to explore the freezing phenomenon in Parkinson’s disease. J Clin Neurosci. 2011;18:807–10. doi:10.1016/j.jocn.2011.02.003.
Shine JM, Matar E, Bolitho SJ, et al. Modeling freezing of gait in Parkinson’s disease with a virtual reality paradigm. Gait Posture. 2013;38:104–8. doi:10.1016/j.gaitpost.2012.10.026.
Nichols S. Physical ergonomics of virtual environment use. Appl Ergon. 1999;30:79–90.
Stanney K, Kennedy R, Drexleer J, et al. Motion sickness and proprioceptive after effects following virtual environment exposure. Appl Ergon. 1999;30:27–38.
Mirelman A, Maidan I, Herman T, et al. Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J Gerontol A Biol Sci Med Sci. 2011;66A:234–40.
Cole S, Yoo D, Knutson B. Interactivity and reward-related neural activation during a serious videogame. PLoS One. 2012;7:e33909.
Messier J, Adamovich SV, Jackson D, et al. Visuomotor learning in immersive 3D virtual reality in Parkinson’s disease and in aging. Exp Brain Res. 2007;179:457–74.
Griffin HJ, Greenlaw R, Limousin P, et al. The effect of real and virtual visual cues on walking in Parkinson’s disease. J Neurol. 2011;258:991–1000. doi:10.1007/s00415-010-5866-z.
Todorov E, Shadmer R, Bizzi E. Augmented feedback presented in a virtual environment accelerates learning a difficult motor task. J Mot Behav. 1997;29:147–58.
Rose F, Attree E, Brooks B, et al. Training in virtual environments: transfer to real world tasks and equivalence to real task training. Ergonomics. 2000;43:494–511.
Jaffe D, Brown D, Pierson-Carey C, et al. Stepping over obstacles to improve walking in individuals with poststroke hemiplegia. J Rehabil Res Dev. 2004;41:283–92.
Azulay JP, Mesure S, Amblard B, et al. Increased visual dependence in Parkinson’s disease. Percept Mot Skills. 2002;95:1106–14.
Martens KAE, Almeida QJ. Dissociating between sensory and perceptual deficits in PD: more than simply a motor deficit. Mov Disord. 2012;27:387–92. doi:10.1002/mds.24042.
Davidsdottir S, Wagenaar R, Young D, et al. Impact of optic flow perception and egocentric coordinates on veering in Parkinson’s disease. Brain. 2008;131:2882–93. doi:10.1093/brain/awn237.
Iansek R, Danoudis M, Bradfield N. Gait and cognition in Parkinson’s disease: implications for rehabilitation. Rev Neurosci. 2013;24:293–300.
Lord S, Galna B, Coleman S, et al. Cognition and gait show a selective pattern of association dominated by phenotype in incident Parkinson’ s disease. Front Aging Neurosci. 2014;6:1–9. doi:10.3389/fnagi.2014.00249.
Patel N, Jankovic J, Hallett M. Sensory aspects of movement disorders. Lancet Neurol. 2014;13:100–12. doi:10.1016/S1474-4422(13)70213-8.
Kaji R, Murase N. Sensory function of basal ganglia. Mov Disord. 2001;16:593–4.
Abbruzzese G, Berardelli A. Sensorimotor integration in movement disorders. Mov Disord. 2003;18:231–40. doi:10.1002/mds.10327.
Adamovich SV, Berkinblit MB, Hening W, et al. The interaction of visual and proprioceptive inputs in pointing to actual and remembered targets in Parkinson’s disease. Neuroscience. 2001;104:1027–41. doi:10.1016/S0306-4522(01)00099-9.
Schubert M, Prokop T, Brocke F, et al. Visual kinesthesia and locomotion in Parkinson’s disease. Mov Disord. 2005;20:141–50.
Prokop T, Schubert M, Berger W. Visual influence on human locomotion. Modulation to changes in optic flow. Exp Brain Res. 1997;114:63–70.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Does manipulating the speed of visual flow in virtual reality change distance estimation while walking in Parkinson’ s disease ? Exp Brain Res. 2015;233:787–95. doi:10.1007/s00221-014-4154-z.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Dopaminergic contributions to distance estimation in Parkinson’s disease: a sensory-perceptual deficit? Neuropsychologia. 2013;51:1426–34. doi:10.1016/j.neuropsychologia.2013.04.015.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. A closer look at mechanisms underlying perceptual differences in Parkinson’s freezers and non-freezers. Neuroscience. 2014;274:162–9. doi:10.1016/j.neuroscience.2014.05.022.
Lin C, Wagenaar R, Young D, et al. Effects of Parkinson’s disease on optic flow perception for heading direction during navigation. Exp Brain Res. 2014;232:1343–55. doi:10.1007/s00221-014-3853-9.Effects.
Ehgoetz Martens KA, Pieruccini-Faria F, Silveira CR, et al. The contribution of optic flow to freezing of gait in left- and right-PD: different mechanisms for a common phenomenon? Parkinsonism Relat Disord. 2013;19:1046–8. doi:10.1016/j.parkreldis.2013.06.011.
Chan RCK, Shum D, Toulopoulou T, et al. Assessment of executive functions: review of instruments and identification of critical issues. Arch Clin Neuropsychol. 2008;23:201–16. doi:10.1016/j.acn.2007.08.010.
Albani G, Pignatti R, Bertella L, et al. Common daily activities in the virtual environment: a preliminary study in parkinsonian patients. Neurol Sci. 2002;23:49–50. doi:10.1007/s100720200064.
Cipresso P, Albani G, Serino S, et al. Virtual multiple errands test (VMET): a virtual reality-based tool to detect early executive functions deficit in Parkinson’s disease. Front Behav Neurosci. 2014;8:405. doi:10.3389/fnbeh.2014.00405.
Klinger E, Chemin L, Lebreton S, et al. Virtual action planning in action Parkinson’s disease: a control study. Cyberpsychol Behav. 2006;9:342–7.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Virtually-induced threat in Parkinson’s: dopaminergic interactions between anxiety and sensory-perceptual processing while walking. Neuropsychologia. 2015:1–10. doi:10.1016/j.neuropsychologia.2015.05.015.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Anxiety-provoked gait changes are selectively dopa-responsive in Parkinson’s disease. Eur J Neurosci. 2015:1–8. doi:10.1111/ejn.12928.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Evaluating the link between dopaminergic treatment, gait impairment, and anxiety in Parkinson’s disease. Mov Disord Clin Pract. Published Online First: 2016. doi:10.1002/mdc3.12298.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Does anxiety cause freezing of gait in Parkinson’s disease? PLoS One. 2014;9:e106561. doi:10.1371/journal.pone.0106561.
Lewis SJG, Barker RA. A pathophysiological model of freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord. 2009;15:333–8. doi:10.1016/j.parkreldis.2008.08.006.
Lewis SJG, Barker RA. Understanding the dopaminergic deficits in Parkinson’s disease: insights into disease heterogeneity. J Clin Neurosci. 2009;16:620–5. doi:10.1016/j.jocn.2008.08.020.
Ehgoetz Martens KA, Ellard CG, Almeida QJ. Virtually-induced threat in Parkinson’s: dopaminergic interactions between anxiety and sensory-perceptual processing while walking. Neuropsychologia. Published Online First: 2015. doi:10.1016/j.neuropsychologia.2015.05.015.
Naismith SL, Lewis SJG. The specific contributions of set-shifting to freezing of gait in Parkinson’s disease. Mov Disord. 2010;25:1000–4.
Matar E, Shine JM, Naismith SL, et al. Using virtual reality to explore the role of conflict resolution and environmental salience in freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord. 2013;19:937–42.
Matar E, Shine JM, Naismith SL, et al. Virtual reality walking and dopamine: opening new doorways to understanding freezing of gait in Parkinson’s disease. J Neurol Sci. 2014;344:182–5. doi:10.1016/j.jns.2014.06.054.
Shine JM, Matar E, Ward PB, et al. Exploring the cortical and subcortical functional magnetic resonance imaging changes associated with freezing in Parkinson’s disease. Brain. 2013;136:1204–15. doi:10.1093/brain/awt049.
Shine JM, Matar E, Ward PB, et al. Freezing of gait in Parkinson’s disease is associated with functional decoupling between the cognitive control network and the basal ganglia. Brain. 2013;136:3671–81. doi:10.1093/brain/awt272.
Shine JM, Koyejo O, Bell PT, et al. Estimation of dynamic functional connectivity using multiplication of temporal derivatives. Neuroimage. 2015;122:399–407.
Shine JM, Matar E, Ward PB, et al. Differential neural activation patterns in patients with Parkinson’s disease and freezing of gait in response to concurrent cognitive and motor load. PLoS One. 2013;8:e52602. doi:10.1371/journal.pone.0052602.
Gilat M, Shine JM, Walton CC, et al. Brain activation underlying turning in Parkinson’s disease patients with and without freezing of gait: a virtual reality fMRI study brain activation underlying turning in Parkinson’ s disease patients with and without freezing of gait: a virtual real. npj Park Dis. 2015;1:15020. doi:10.1038/npjparkd.2015.20.
Nutt JG, Bloem BR, Giladi N, et al. Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011;10:734–44. doi:10.1016/S1474-4422(11)70143-0.
Nieuwboer A, Giladi N. Characterizing freezing of gait in Parkinson’s disease: models of an episodic phenomenon. Mov Disord. 2013;28:1509–19. doi:10.1002/mds.25683.
Lewis SJG, Shine JM. The next step: a common neural mechanism for freezing of gait. Neuroscientist 2014. doi:10.1177/1073858414559101.
Baram Y. Virtual sensory feedback for gait improvement in neurological patients. Front Neurol. 2013;4:138. doi:10.3389/fneur.2013.00138.
Ashoori A, Eagleman DM, Jankovic J. Effects of auditory rhythm and music on gait disturbances in Parkinson’s disease. Front Neurol. 2015;6:1–11. doi:10.3389/fneur.2015.00234.
Mirelman A, Rochester L, Reelick M, et al. V-TIME: a treadmill training program augmented by virtual reality to decrease fall risk in older adults: study design of a randomized controlled trial. BMC Neurol. 2013;13:15. doi:10.1186/1471-2377-13-15.
Laver K, George S, Thomas S, et al. Cochrane review: virtual reality for stroke rehabilitation. Eur J Phys Rehabil Med. 2012;48:523–30.
Jones C, Jahanshahi M. Motor and perceptual timing in Parkinson’s disease. Adv Exp Med Biol. 2014;829:265–90.
Chen J, Penhune V, Zatorre R. Listening to musical rhythms recruits motor regions of the brain. Cereb Cortex. 2008;18:2844–54.
Bengtsson S, Ullen F, Ehrsson H, et al. Listening to rhythms activates motor and premotor cortices. Cortex. 2009;45:62–71.
Pastor M, Artieda J, Jahanshahi M, et al. Time estimation and reproduction is abnormal in Parkinson’s disease. Brain. 1992;115:211–25.
Coull JT, Cheng R, Meck WH. Neuroanatomical and neurochemical substrates of timing. Neuropsychopharmacology. 2010;36:3–25. doi:10.1038/npp.2010.113.
O’Boyle D, Freeman J, Cody F. The accuracy and precision of timing of self-paced, repetitive movements in subjects with Parkinson’s disease. Brain. 1996;119:51–70.
Tolleson C, Dobolyi D, Roman O, et al. Dysrhythmia of timed movements in Parkinson’s disease and freezing of gait. Brain Res. 1624;2015:222–31.
Beudel M, Galama S, Leenders K, et al. Time estimation in Parkinson’s disease and degenerative cerebellar disease. Neuroreport. 2008;19:1055–8.
Nombela C, Hughes L, Owen AM, et al. Into the groove: can rhythm influence Parkinson’s disease? Neurosci Biobehav Rev. 2013;37:2564–70.
Nieuwboer A, Rochester L, Muncks L, et al. Motor learning in Parkinson’s disease: limitations and potential for rehabilitation. Parkinsonism Relat Disord. 2009;15:S53–8.
Lopez W, Higuera C, Fonoff E, et al. Listenmee and Listenmee smartphone application: sychronizing walking to rhythmic auditory cues to improve gait in Parkinson’s disease. Hum Mov Sci. 2014;37:147–56.
Jiang Y, Norman K. Effects of visual and auditory cues on gait initiation in people with Parkinson’s disease. Clin Rehabil. 2006;20:36–45.
Luessi F, Mueller L, Breimhorst M, et al. Influence of visual cues on gait in Parkinson’s disease during treadmill walking at multiple velocities. J Neurol Sci. 2012;314:78–82.
Lee S, Yoo J, Ryu J, et al. The effect of visual and auditory cues on freezing of gait in patients with Parkinson’s disease. Am J Phys Med Rehabil. 2012;91:2–11.
Yogev G, Giladi N, Peretz C, et al. Dual tasking, gait rhythmicity, and Parkinson’s disease: which aspects of gait are attention demanding? Eur J Neurosci. 2005;22:1248–56. doi:10.1111/j.1460-9568.2005.04298.x.
Rochester L, Nieuwboer A, Baker K, et al. The attentional cost of external rhythmical cues and their impact on gait in Parkinson’s disease: effect of cue modality and task complexity. J Neural Transm. 2007;114:1243–8.
Badarny S, Aharon-Peretz J, Susel Z, et al. Virtual reality feedback cues for improvement of gait in patients with Parkinson’s disease. Tremor Other Hyperkinet Mov (N Y) 2014;4:225. doi:10.7916/D8V69GM4.
Hove M, Suzuki K, Uchitomi H, et al. Interactive rhythmic auditory stimulation reinstates natural 1/f timing in gait of Parkinson’s patients. PLoS One. 2012;7:e32600.
Zhao Y, Heida T, van Wegem E, et al. E-health support in people with Parkinson’s disease with smart glasses: a survey of user requirements and expectations in the Netherlands. J Parkinsons Dis. 2015;5:369–78.
Walton CC, Shine JM, Mowszowski L, et al. Impaired cognitive control in Parkinson’s disease patients with freezing of gait in response to cognitive load. J Neural Transm. 2015;122:653–60.
Walton CC, O’Callaghan C, Hall JM, et al. Antisaccade errors reveal cognitive control deficits in Parkinson’s disease with freezing of gait. J Neurol. 2015;262:2745–54. doi:10.1007/s00415-015-7910-5.
Shine JM, Naismith SL, Palavra NC, et al. Attentional set-shifting deficits correlate with the severity of freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord. 2013;19:388–90. doi:10.1016/j.parkreldis.2012.07.015.
Rochester L, Galna B, Lord S, et al. The nature of dual-task interference during gait in incident Parkinson’s disease. Neuroscience. 2014;265:83–94. doi:10.1016/j.neuroscience.2014.01.041.
Brown LA, McKenzie NC, Doan JB. Age-dependent differences in the attentional demands of obstacle negotiation. J Gerontol A Biol Sci Med Sci. 2005;60:924–7.
Pieruccini-Faria F, Ehgoetz Martens KA, Silveira C, et al. Interactions between cognitive and sensory load while planning and controlling complex gait adaptations in Parkinson’s disease. BMC Neurol. 2014;14. doi:10.1186/s12883-014-0250-8.
Pompeu JE, Arduini LA, Botelho AR, et al. Feasibility, safety and outcomes of playing Kinect Adventures! for people with Parkinson’s disease: a pilot study. Physiotherapy (United Kingdom) 2014;100:162–8. doi:10.1016/j.physio.2013.10.003.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Martens, K.A.E., Shine, J.M., Lewis, S.J.G. (2017). Using Virtual Reality to Advance the Understanding and Rehabilitation of Gait Impairments in Parkinson’s Disease. In: Barbieri, F., Vitório, R. (eds) Locomotion and Posture in Older Adults. Springer, Cham. https://doi.org/10.1007/978-3-319-48980-3_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-48980-3_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-48979-7
Online ISBN: 978-3-319-48980-3
eBook Packages: MedicineMedicine (R0)