Abstract
This chapter presents the common impairments in gait that are fundamental to neurodegenerative diseases and provide examples from studies on aging, Parkinson’s disease, a classical neurodegenerative disease, and multiple sclerosis, an inflammatory progressive disease that involves neuronal loss. Factors that contribute to problems in mobility are discussed along with current treatment approaches. The review of these topics leads to the rationale and potential advantages of VR-based methods for improving walking and mobility in patients with neurodegenerative disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara ObjectiveTo present a review of VR augmented training for improving walking and reducing fall risk in patients with neurodegenerative disease.
8.1 Neurodegenerative Diseases
Neurodegeneration is the umbrella term for the progressive loss of structure or function of neurons or neuronal death. Neurodegeneration can be found in all levels of neuronal circuitry ranging from molecular to systemic. Neurodegeneration in essence is part of the normal process of aging. With aging, neurons gradually lose function and white matter lesions start to appear. However the term is most often associated with pathological processes known as neurodegenerative diseases including diseases such as Parkinson’s disease (PD) and Alzheimer’s disease (AD) (Bredesen, Rao, & Mehlen, 2006) which in a sense could be considered “rapid aging diseases.” In fact, the greatest risk factor for neurodegenerative diseases is aging, with neurons gradually losing more function as the disease progresses with age and with the involvement of extended brain regions and networks that affect different modalities resulting in motor and cognitive deficits (Bredesen et al., 2006; Lin & Beal, 2006).
Many common features exist among different neurodegenerative diseases such as atypical protein assemblies and induced cell death. However, the brain regions that are involved differ between the diseases and therefore lead to different initial symptoms and pathologies (Bredesen et al., 2006; Rubinsztein, 2006). For example, AD is characterized by loss of neurons and synapses in the cerebral cortex and certain subcortical regions while PD is characterized by the death of dopamine-generating cells in the basal ganglia. Nevertheless, as the disease progresses, multiple brain regions may be involved and symptoms are highly variable. Affected systems include motor, cognitive function, autonomic, and affective function. Motor and physical deficits include muscle weakness, loss of range, changes in posture, and reduced aerobic capacity which have a direct impact on balance, gait, and mobility (Schenkman & Butler, 1989). Autonomic function includes urinary and bowl control as well as cardiac denervation (Goldstein, 2003). Cognitive and affective deficits include reduced attention and impaired executive function which affect task planning, dual tasking, sensory integration, judgment, and reasoning (van Iersel, Kessels, Bloem, Verbeek, & Olde Rikkert, 2008; Yogev-Seligmann, Hausdorff, & Giladi, 2008) and behavioral changes that involve depression, loss of motivation and initiation, and increased anxiety.
In this chapter, we briefly discuss the common impairments in gait that are fundamental to neurodegenerative diseases and provide examples from studies on aging, PD, a classical neurodegenerative disease, and multiple sclerosis (MS), an inflammatory progressive disease that involves neuronal loss. Factors that contribute to problems in mobility will be presented along with current treatment approaches. The review of these topics will lead to the rationale and potential advantages of virtual reality-based methods for improving walking and mobility in patients with neurodegenerative disease.
8.2 Gait Impairments and Falls in Neurodegenerative Conditions
Gait impairments and falls are ubiquitous among the general older adult population and among patients with common neurological diseases. Approximately 30 % of community-dwelling elderly over the age of 65 fall at least once a year, and 6 % of these falls result in fractures (Blake et al., 1988; Tinetti, Speechley, & Ginter, 1988). These figures are even higher in populations with pathologies such as PD, with an annual incidence of 60–80 % (Tinetti et al., 1988; Wood, Bilclough, Bowron, & Walker, 2002), at least twice that of the general elderly population. The impact of falls is severe. Falls often lead to institutionalization and loss of functional independence, disability, depression, and social isolation (Rubenstein & Josephson, 2006). Given the significance of falls on quality of life and functional independence, the careful assessment of the mechanisms that underlie the reasons for falls is needed prior to considering the appropriate therapeutic interventions.
With aging, elderly individuals generally walk more slowly, with shorter strides, decreased arm swing, and longer double-limb support times (Morris, Huxham, McGinley, & Iansek, 2001; Morris, Iansek, Matyas, & Summers, 1994). Fear of falling, a cautious gait (Ashburn, Stack, Pickering, & Ward, 2001; Legters, 2002), gait unsteadiness, or inconsistency and dysrhythmicity of stepping have also been closely associated with decreased mobility and an increased risk of falls in the elderly and are recognized mediators of fall risk (Hausdorff et al., 2001; Hausdorff & Yogev, 2006).
Commonly observed gait changes in individuals with PD also include small shuffling steps and spatial and temporal asymmetry (Morris, Iansek, Matyas, & Summers, 1996; Morris et al., 2001) as well as start hesitation, difficulty in maneuvering through tight or occluded spaces (Bloem, Hausdorff, Visser, & Giladi, 2004; Gray & Hildebrand, 2000), and a loss of consistency in one’s ability to produce a steady gait rhythm, which in turn produces stride-to-stride variability (Baltadjieva, Giladi, Gruendlinger, Peretz, & Hausdorff, 2006; Hausdorff, Cudkowicz, Firtion, Wei, & Goldberger, 1998). In PD, reports on the effects of cueing support the idea that impairment of internal clocking mechanisms results in disruption of the normal motor programming. It seems that the “internal cueing” needed to perform automatic, sequential movements (Baltadjieva et al., 2006; Schaafsma et al., 2003) is the principal determinant of the increased gait variability in PD, while force production issues are important, but secondary (Baltadjieva et al., 2006). In support of this hypothesis, it is noted that stride variability improves, to some degree, in response to dopamine treatment (Schaafsma et al., 2003) and in response to external cueing (Rubenstein, Giladi, & Hausdorff, 2002; Thaut et al., 1996).
In MS, common symptoms include paresis, sensory impairment, spasticity, balance deficits, and fatigue (O’Sullivan, 1984). These impairments often lead to gait disturbances and difficulty walking. Approximately 50 % of individuals with MS will require assistance and/or an assistive device to ambulate short distances within 15 years of onset of the disease (Weinshenker, 1994), and between 50 and 60 % of people with MS identify fatigue as the worst symptom that they experience (Fisk, Pontefract, Ritvo, Archibald, & Murray, 1994; Freal, Kraft, & Coryell, 1984), which in turn severely affects functional walking endurance and independence.
8.3 Obstacle Negotiation and Dual Tasking: Two Key Elements to Functional Independence
8.3.1 Obstacle Negotiation
The alterations in gait that commonly occur in aging and neurodegenerative disease may be further challenged in complex everyday, walking environments that require obstacle negotiation. These challenges further increase the risk of falls in these populations. Obstacle crossing is a daily activity that involves tasks such as going up a curb or stepping over a crack in the ground or a branch. A decline in obstacle crossing performance with advancing age has been implicated in the high incidence of trips and stumbles in older adults (Overstall, Exton-Smith, Imms, & Johnson, 1977; Tinetti et al., 1988). In patients with PD, obstacle avoidance (Robinson et al., 2005) and dual or multitasking situations (Brown & Brockmole, 2010) have been implicated as the foremost extrinsic (environmental) risk factors for falls. The majority of trips arise from errors in foot contact with ground-based obstacles during obstacle negotiation (Fingerhut, Cox, & Warner, 1998). Compared to healthy young adults, older adults walk more slowly during obstacle crossing (Chapman & Hollands, 2007; Lowrey, Watson, & Vallis, 2007) with smaller steps (Chen, Ashton-Miller, Alexander, & Schultz, 1994; Lowrey et al., 2007) and land dangerously closer to the obstacle with their lead limb after crossing (Galna, Murphy, & Morris, 2010; Lowrey et al., 2007), increasing the risk of falls. Vitorio, Pieruccini-Faria, Stella, Gobbi, and Gobbi (2010) compared obstacle crossing between patients with mild-to-moderate PD and age-matched older adults and found that during the approach phase, people with PD demonstrated even shorter stride length and greater stride duration than controls. For the crossing phase, people with PD demonstrated shorter step length over the obstacle and a shorter distance from the lead limb foot to the obstacle both before and after crossing.
Age-related deficits in vision, proprioception, visual-spatial orientation, cognition, and attention can also negatively impact postural stability and lower limb kinematics when crossing obstacles (Lord, Smith, & Menant, 2010; Menant, St George, Fitzpatrick, & Lord, 2010). Indeed, obstacle negotiation is attentionally demanding and thus relies heavily on the availability of ample cognitive resources due to the need for motor planning and visually dependent gait regulation (Brown, McKenzie, & Doan, 2005). In fact, in situations when attention is divided, older people negotiate obstacles even more slowly and contact more obstacles (Menant et al., 2010). With neurodegeneration, motor and cognitive abilities deteriorate and the ability to negotiate obstacles depreciates even further (Vitorio et al., 2010).
8.3.2 Executive Function, Attention, and Dual Tasking
Diminished cognitive function, specifically executive function (EF) and attention, negatively affects gait and postural stability in older adults, in individuals with PD, and in patients with MS (Adams & Parsons, 2003; Woollacott & Shumway-Cook, 2002). EF refers to a variety of higher cognitive processes including initiation of goal-directed behavior, intention of action, planning, working memory, and attention (Fuster, 1999). Attention is driven in part by sensory perception and refers to the selection of a preferred stimulus for a particular action while ignoring or rejecting the irrelevant (D’Esposito, Ballard, Zarahn, & Aguirre, 2000; Jueptner, Frith, Brooks, Frackowiak, & Passingham, 1997; Passingham, 1996; Rowe et al., 2002; Yogev et al., 2005). Lezak (1995) divided EF into four major components: volition, planning, purposive action, and effective performance (action monitoring). Others also explicitly include cognitive inhibition as an EF component (Stuss & Alexander, 2000; Yogev-Seligmann et al., 2008). Impairment of one or more of these EF components may impact one’s ability to walk efficiently and safely. Poor self-awareness of limitations, an aspect of volition, might result in an increased risk of falling (van Iersel et al., 2008). Impaired planning skills can lead to getting lost, choices that produce inefficient pathways or unnecessary effort to arrive at a destination, and collisions with obstacles.
Healthy young adults pay little attention to their gait when they walk in simple, unobstructed environments. However when encountering complex environments such as uneven surfaces, negotiating obstacles, diminished visibility, or crowded places their walking becomes slower. This also occurs when young adults are asked to walk and perform another task simultaneously (i.e., dual task, DT) (Beauchet et al., 2003; Ebersbach et al., 1999; Gage, Sleik, Polych, McKenzie, & Brown, 2003; Yogev, Plotnik, Peretz, Giladi, & Hausdorff, 2006). Healthy older adults and, to a greater extent, patient populations (e.g., patients with PD or MS) not only slow down, increasing double-limb support on the ground, but also become less stable (i.e., increased gait variability) (Bond & Morris, 2000; Hausdorff, Balash, & Giladi, 2003; Sheridan, Solomont, Kowall, & Hausdorff, 2003; Yogev et al., 2005) (see Fig. 8.1).
Example of swing time series in a patient with PD and a control under usual walking conditions and when performing a dual task (serial 7 subtractions). Variability increases during dual tasking in the subject with PD, but not in the control subject. Adapted from Yogev et al. (2005)
The simultaneous performance of two or more tasks often creates a conflict and a need to determine which of the tasks receives priority, especially when information processing is limited (Pashler, 1994). Bloem et al. (Bloem, Boers, Cramer, Westendorp, & Gerschlager, 2001; Bloem, van Vugt, & Beckley, 2001) reported that young adults and healthy elderly spontaneously prioritize gait stability over success on the “secondary,” cognitive task, when no specific prioritization instructions or allocation of attention is given. This “posture first strategy” makes sense from an ecologic perspective as it helps to prevent loss of balance. Interestingly, with aging, this prioritization is not as efficient increasing the “cost” of performing a secondary task and thus increasing the risk of falls. Further, several studies have shown that DT during gait in patients with PD results in a slower walk, with shorter strides, and much higher “DT” decrement than that seen in controls (Bloem, Valkenburg, Slabbekoorn, & Willemsen, 2001; Bond & Morris, 2000; Hausdorff et al., 2003; Lundin-Olsson, Nyberg, & Gustafson, 1997; Yogev et al., 2006).
8.4 Cognitive Deficits and Their Contribution to Gait Problems and Fall Risk
In the past decade, many studies have contributed to the body of knowledge on the importance of cognitive function in walking. Gait is no longer considered to be an automatic, biomechanical task; instead, the role of cognitive function is increasingly recognized (Alexander & Hausdorff, 2008; Yogev-Seligmann et al., 2008). Cognitive impairments are common in neurodegenerative diseases even in the early stages of the disease, and they tend to further deteriorate as the disease progresses. In the following paragraph, we briefly summarize the evidence indicating that impaired cognitive function is related to gait disturbances in specific neurodegenerative conditions. This relationship is important because it helps to define the requirements for optimal interventions, as described further below.
8.4.1 Parkinson’s Disease
Cognitive impairment is a well-recognized non-motor feature of PD. About 15–40 % of patients with PD suffer some degree of cognitive impairment (Muslimovic, Post, Speelman, & Schmand, 2005). The main feature of cognitive decline associated with PD is impairment of EF. Deficits in EF can already be detected shortly after motor symptoms appear (Aarsland, Bronnick, Larsen, Tysnes, & Alves, 2009). EF is traditionally associated with the frontal lobes and related brain networks. The area of the prefrontal lobe and, in particular, the dorsolateral prefrontal cortex (DLPFC, Brodmann’s area 9) and the cingulate cortex (e.g., the anterior cingulate: ACC, Brodmann’s areas 24, 32) have been related to the cognitive aspects of EF (Lezak, 1995; Stuss & Alexander, 2000; Yogev-Seligmann et al., 2008). In general, the anterior parts of the frontal lobes are involved with aspects of self-regulation, such as inhibition and self-awareness, whereas the dorsal parts are involved with reasoning processes.
In PD, cognitive deterioration also manifests as a profound difficulty in motor planning, resulting in both slowness of initiating motor action, slowed generation of ideas and plans, and reduced performance on tasks that involve attentional processes. This becomes especially apparent during DT activities. As noted above, studies have shown that DT during gait in patients with PD causes patients to walk slower, with shorter strides, and much higher “DT” decrement than that seen in controls (Bloem, Valkenburg, et al., 2001; Bond & Morris, 2000; Hausdorff et al., 2003; Lundin-Olsson et al., 1997; Lundin-Olsson, Nyberg, & Gustafson, 1998). In fact, several studies demonstrated a relationship between attention abilities, gait, and fall risk in PD (Deane et al., 2002; Hausdorff et al., 2003, 2006; Yogev et al., 2006).
8.4.2 Multiple Sclerosis
The neuropathology of MS is characterized by multifocal inflammatory demyelination and neuroaxonal injury (Tomassini et al., 2012). The prevalence of cognitive impairments in persons with MS is high, with estimates ranging from 43 to 65 % (Peyser, Rao, LaRocca, & Kaplan, 1990; Rao et al., 1991). Processing speed, attention, EF, learning, and memory are common areas of cognition affected by MS (Arnett et al., 1997; Calabrese, 2006; Drew, Tippett, Starkey, & Isler, 2008). While these common cognitive impairments have been identified in MS, it is important to underscore that the pattern of cognitive decline in each patient with MS is variable and unpredictable (Larocca, 2011).
A recent review concluded that the changes in postural control underlying gait impairments and fall risk in MS are primarily due to slowed somatosensory conduction and impaired central integration of information (Cameron & Lord, 2010). Some of these main predictors appear to be related to the cognitive capacities of sustained attention, processing speed, and EF. In addition, patients with a clinically isolated syndrome and a diagnosis of possible MS had greater decrements in speed and gait stability during cognitive tasks than healthy controls, suggesting that there may be cognitive difficulties interfering with parameters of gait even during the earliest stages of the disease (Kalron, Dvir, & Achiron, 2010). Using a DT paradigm, Benedict et al. also showed that patients with MS had greater decrements in walking speed than healthy controls (Benedict et al., 2011; Benedict & Zivadinov, 2011). Interestingly, the degree of the decrement was related to fatigue, measures of general cognitive function, and self-reported cognitive errors rather than measures of overall disability, and processing speed and EF were also found to be significant predictors of lower and upper motor function in patients with MS (Benedict et al., 2011; Benedict & Zivadinov, 2011).
D’Orio et al. (2012) investigated the associations between cognitive functions, walking speed, and falls in patients with MS. They found that after controlling for age, gender, and disease severity, slower processing speed and IQ predicted slower gait speed, while poorer verbal memory predicted increased frequency of falls. Thus, the authors concluded that specific cognitive functions are meaningfully related to mobility limitations in patients with MS and that risk assessment for gait decline and falls should include cognitive assessment in patients with MS (D’Orio et al., 2012).
8.4.3 Older Adults
Age-associated changes in cognitive function are well documented. Memory may be the most widely reported complaint; however, EF and attentional deficits are also evident. The frontal lobes are apparently highly susceptible to age-associated changes (Craik & Grady, 2002; Dorfman, 1998). These include lesions of diffused white matter, which might affect fronto-striatal circuits and cause, among other things, impairment in EF (Buckner, 2004). Neuropsychological studies demonstrated impaired EF in generally healthy elderly subjects. This includes difficulties in problem solving that requires flexible thinking and cognitive shifting, impaired response inhibition, and impaired creative thinking (Dorfman, 1998). These impairments place older adults at a heightened risk of falling when they attempt to perform two or more tasks simultaneously, even if the tasks are otherwise considered to be automatic or demand minimal attention (Marsh & Geel, 2000). When performing dual tasks, reaction time becomes significantly longer in older adults, gait velocity is reduced, and stride length variability and stride time increase (van Iersel et al., 2008). These effects are even larger among elderly fallers than in the general elderly population (Herman, Mirelman, Giladi, Schweiger, & Hausdorff, 2010; Montero-Odasso et al., 2009; Yogev-Seligmann et al., 2008).
In a prospective study that investigated 201 healthy older adults who were free from falls in the year prior to baseline testing, Herman et al. (2010) showed that worse EF scores at baseline were associated with falls that occurred during the 2-year follow-up (Herman et al., 2010) (see Fig. 8.2). In an extension to this study, EF and gait variability during DT were still the strongest predictors of falls during 5 years of follow-up, reenforcing the importance of evaluating cognitive function as part of the assessment of fall risk and impaired mobility in the elderly.
Survival curves illustrating the percent of participants who did not fall (the y-axes) as a function of time and executive function group (left) or DT gait variability (right). Participants with worse EF (lowest quartile) or increased DT gait variability were more likely to become fallers and recurrent fallers sooner than those with better EF or DT gait (upper quartile). Adapted from Herman et al.
8.5 Physical and Motor Rehabilitation in Neurodegenerative Diseases
To understand the advantages of training mobility in virtual reality, we first briefly summarize the current “state of the art” in mobility rehabilitation. Given the progressive decline in neurodegenerative pathology and aging of the brain areas responsible for learning, it was previously thought that training could not elicit long-term effects in these patient populations; therefore management was based on compensation and prevention rather than rehabilitation. Recent evidence suggests, however, that this is not the case (Graybiel, 2005; Herman, Giladi, & Hausdorff, 2009; Wu & Hallett, 2005). Several key features for successful motor learning have been identified: learning sessions should be intensive (Guadagnoli, Leis, Van Gemmert, & Stelmach, 2002; Jobges et al., 2004), focus on a single desired outcome, and involve extensive feedback. Interventions following these principles have provided new evidence on impressive training effects as well as retention effects after training even in the face of neurodegeneration (Abbruzzese, Trompetto, & Marinelli, 2009; Mirelman et al., 2010; Rochester et al., 2010; Verghese et al., 2002).
Physical therapy (PT) is often prescribed for older adults and patients with PD in order to maximize function and minimize secondary complications. PT is delivered through movement rehabilitation within the context of education and support for the whole person (Deane et al., 2001). Although there are presently no widely accepted, standardized guidelines for treatment (Graybiel, 2005), PT covers different treatment techniques. Recommended interventions include strengthening, fitness training and active and functional task exercises using “strategy training,” where the person is taught how to best utilize his/her ability in order to overcome difficulties, and cueing strategies to enhance gait (Graybiel, 2005). Still, recent meta-analyses concluded that there is little evidence to support or refute the use of PT for patients with PD, in part because of methodological flaws in published studies (Deane et al., 2001; Ellis et al., 2005; Graybiel, 2005; Rubenstein et al., 2002).
8.5.1 Cueing
Sensory cueing has been used extensively as a form of “strategy training” to improve function in PD. One explanation for this phenomenon suggests that “tricks” (cues) are effective because they activate the pre-motor cortical system either by bypassing the basal ganglia or by better focusing the cortico-basal ganglia–thalamo–cortical motor loop in relation to other psychomotor or associative loops (Lowenthal et al., 2004). For example, training with rhythmic auditory stimulation (RAS) demonstrated that patients with PD were able to match their cadence to a beat that was set at 10 % faster than their baseline values, significantly improving their velocity and stride length (Dam et al., 1996; Lowenthal et al., 2004). Walking while hearing RAS improves the rhythmicity of gait in a sense that provides an external rhythm by which a person can improve his/her gait. Patients who underwent gait training combined with auditory cueing improved significantly, as compared to patients who received only conventional PT (Marchese, Diverio, Zucchi, Lentino, & Abbruzzese, 2000; Van Wegen et al., 2006). Some studies also showed long-term effects (at least 6 weeks) after training. Similar findings were observed after training with visual and somatosensory cues, although significant long-term effects were not observed (Nieuwboer et al., 2007). Despite the promising evidence of cueing, therapy based on cueing does not address everyday tasks that challenge mobility such as dual-task activities or obstacle avoidance.
8.5.2 The Treadmill as a Pacemaker and a Rehabilitation Tool
Several studies suggested that training with a treadmill (TT) can enhance overground routine walking in patients with a variety of neurological diseases. Perhaps the most obvious relief is seen in stroke patients and in patients with spinal cord injuries (Laufer, Dickstein, Chefez, & Marcovitz, 2001). A handful of studies have also examined the effects of TT on the gait of PD patients (Herman, Giladi, Gurevich, & Hausdorff, 2005; Miyai et al., 2000, 2002) and MS (Benedetti et al., 2009; Pilutti et al., 2011). Training with TT and BWS improved physical and mental subscales and provided beneficial effects on quality of life and potentially reduced fatigue in patients with MS (Benedetti et al., 2009; Pilutti et al., 2011). The mechanism by which TT improves gait in PD is not yet clear. TT may activate neuronal circuits that mediate central pattern generators (Muir & Steeves, 1997) or enhance motor learning by reinforcing the synaptic connections in the spinal cord level or triggering reorganization of neural networks (Mathiowetz & Haugen, 1994). Walking on a moving walkway may also inherently provide external cueing, mediated through proprioceptive and vestibular receptors (Holden, 2005).
Results from recent studies support the efficacy and long-term carryover effects of TT on gait and balance with some reduction in fear of falling in patients with PD (Kurtais, Kutlay, Tur, Gok, & Akbostanci, 2008; Toole, Maitland, Warren, Hubmann, & Panton, 2005). Retention of TT training effects was reported along with carryover effects on QOL (Herman, Giladi, Gruendlinger, & Hausdorff, 2007). In fact, TT has become widely available and is often prescribed to promote mobility, exercise, and physical activity, even in nursing home facilities. Although TT is apparently beneficial in improving usual walking in patients with PD, TT alone apparently does not generate improvements in dual-tasking abilities or lead to a reduction in fall risk. This lack of an effect on dual tasking and fall risk likely stems from the fact that TT focuses exclusively on usual walking, essentially ignoring the more complex, attention-demanding situations that are common in daily activity and community ambulation.
8.5.3 Multifactorial Interventions
The complex symptoms in neurodegenerative conditions that lead to mobility decline and an increased fall risk highlight the need for multifactorial interventions (Gillespie et al., 2009; Kannus, Sievanen, Palvanen, Jarvinen, & Parkkari, 2005). Earlier reviews suggested that multifactorial interventions may be among the most effective, and the American Geriatrics Society and British Geriatrics Society recommended this approach as a primary treatment strategy in their guideline for prevention of falls (2011). Exercise groups have become a widely accepted approach as a rehabilitation technique for the elderly and patients with neurodegenerative disease. Typically, group exercise programs are held two or three times per week for an hour and are supervised by physical therapists or trained exercise instructors. The programs include a combination of exercises to improve flexibility, strength, and balance and some level of aerobic conditioning. Within the exercise category, there is some evidence for the effectiveness of three different approaches in reducing both rate of falls and risk of falling while improving mobility: multiple component group exercise, Tai Chi as a group exercise, and individually prescribed multiple component exercise carried out at home (Gillespie et al., 2009). Although one RCT demonstrated significant effects of Tai Chi on fall frequency in PD (Li et al., 2012), the effects on fall risk generally tend to be small and the reported changes are focused on motor aspects with limited long-term retention (Gillespie et al., 2009; Goodwin, Richards, Taylor, Taylor, & Campbell, 2008; Kannus et al., 2005).
Weerdesteyn et al. (2006) demonstrated that a 5-week exercise program that trained dual-task gait and a highly structured and complex obstacle negotiation task leads to a dramatic reduction in the number of falls reported in the trained group (46 %), as compared to the control group of older adults. Similarly, Yogev-Seligmann, Giladi, Brozgol, and Hausdorff (2012) demonstrated that DT costs during walking respond to training in patients with PD. These findings suggest that appropriate training of DT could be effective in improving the ability to both divide attention and improve stability while walking in complex situations. Because most walking takes place in these more challenging conditions, the potential influence on functional ambulation and fall risk cannot be underscored.
8.6 Evidence for the Added Benefits of VR Augmented Training in Neurodegenerative Disease
Mahoney (2010) suggested that in order for rehabilitation interventions to be successful in improving mobility and reducing the risk of falls, they need to address three major constructs: (1) content: training should be intensive, be focused on the key impairment, and become progressively more rigorous; (2) fit the target population; and (3) intervention process: delivery of the intervention should maximize uptake and include mechanisms to maximize motor learning and induce a behavioural change. The motor learning literature dictates that with proper training, older adults and even patients with various motor disorders or cognitive deficits can improve their functional ability, even in the presence of ongoing disease and motor dysfunction (Schwenk, Zieschang, Oster, & Hauer, 2010; Shumway-Cook, Woollacott, Kerns, & Baldwin, 1997; Winstein, 1990).
These key elements can be easily achieved using VR systems making VR, at least theoretically, a useful tool for intervention in neurodegenerative conditions. The impetus for using VR is that the technology may enable individualized repetitive practice of motor function, graded in accordance to the needs and level of ability of the person while engaging in and stimulating cognitive processes. At the same time, VR provides feedback about performance that may assist with learning new motor strategies of movement. The realism of the virtual environments permits individuals to safely explore their environments independently, increasing their sense of autonomy and independence in directing their own therapeutic experience. Participants with different disorders and motor impairments report that these training sessions are typically quite enjoyable and motivating allowing for higher intensity of training in short duration protocols with relatively low patient burden (de Bruin, Dorflinger, Reith, & Murer, 2010; Deutsch & Mirelman, 2007; Fung, Richards, Malouin, McFadyen, & Lamontagne, 2006; Holden, 2005; Keshner & Weiss, 2007). With advances in technology, VR systems have become affordable and more portable allowing for easy use. The use of VR in the literature varies widely. In the following section, we describe the evidence found in the literature on VR interventions for improving gait and mobility and reducing the risk of falls in patients with PD and MS and in older adults.
8.6.1 Parkinson’s Disease
VR has been used with subjects with PD as an evaluation tool for cognitive and executive function assessments. EF difficulties in planning were easily detected (Klinger, Chemin, Lebreton, & Marie, 2006). Subjects with PD demonstrated the ability to learn new paradigms of movement, but at a slower pace and with more difficulties in movement corrections (Albani et al., 2002; Messier et al., 2007) compared to control participants.
Only a handful of studies have investigated the use of VR for studying gait in PD. Studies include investigating navigation abilities in PD as well as training gait and performance using VR. Davidsdottir, Wagenaar, Young, and Cronin-Golomb (2008) examined the impact of optic flow and egocentric coordinates on navigation during walking in patients with PD. Thirty-one patients with PD (Hoehn and Yahr II–IV) and 18 healthy age-matched controls participated in the study. The researchers used a head-mounted display to project a virtual environment (VE) consisting of a virtual hallway, composed of two sidewalls of white random dots on a black background, with a black floor and ceiling devoid of texture. Participants walked overground at a speed of 0.8 m/s while observing a virtual scene with varied optic flow speeds. Veering was assessed as the change in gait during the trials using a motion capture system. The results showed that parietal-mediated perception of visual space is affected in PD including perception of optic flow speed and egocentric midline coordinates. Side of motor-symptom onset and gender affected spatial performance (with women more affected than men). The walking assessment demonstrated that visual input affected veering, which corresponded to the shifting of the egocentric midline rather than to abnormal perception of optic flow speed. These findings are in line with previous studies reporting impaired navigational abilities in PD patients as seen on the route-walking test (Bowen, Hoehn, & Yahr, 1972) and in indirect measurements of visuospatial neuropsychological tests (Bowen et al., 1972; Heikkila, Turkka, Korpelainen, Kallanranta, & Summala, 1998; Radford, Lincoln, & Lennox, 2004), further suggesting that cognitive and visual-spatial dysfunction, rather than motor impairments per se, can contribute to difficulties in navigation.
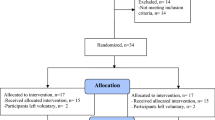
To address the motor and cognitive deficits that commonly contribute to fall risk, Mirelman et al. (2010) developed a VR system based on an obstacle navigation task. Twenty patients with PD (H&Y II–III), walked on a treadmill, while wearing a safety harness, three times a week for 6 weeks. The virtual scene consisted of an outdoor environment of a boardwalk on which virtual obstacles were placed at random intervals. Participants walked in the VE negotiating obstacles and tried to avid stepping on them by stepping over them. Using a camera for motion capture which tracked the movement of the feet, the patient’s movements were inserted into the VR simulation and projected on the wall in front of the treadmill via a large projector (Fig. 8.3). Visual and auditory feedbacks were provided by the VR simulation upon error (stepping or hitting an obstacle) and at the end of each walk in the form of knowledge of results. After 6 weeks of training, comfortable gait speed significantly improved, as did stride length, gait variability, and overground obstacle negotiation. The DT decrement (cost of dual tasking on gait as compared to single task) became smaller (i.e., better), and there was evidence of improved task planning and set shifting, i.e., cognitive function measured using neuropsychological standardized tests. Increased gait speeds under all conditions (comfortable, fast, DT, and 6-min walk) were not only maintained at follow-up but also continued to improve 4 weeks later at the time of follow-up, suggesting that the training generated a positive feedback loop that modified behavior and overall mobility (perhaps a result of motor learning) (Mirelman et al., 2010). DT walking abilities were significantly improved after TT + VR, much more than that seen among subjects who trained only with treadmill, without VR.
The VR simulation consists of a boardwalk with obstacles. On the left, a patient trains on a treadmill while viewing the virtual environment. Center and right: Different types of challenges and feedback provided. Mirelman et al. (2010)
Recently two groups independently started to look at VR as a tool for characterization of freezing of gait (FOG). FOG is a common episodic gait disorder in PD which occurs most often in conflict situations such as gait initiation, turns, crowded places, and narrow pathways. FOG has been associated with deficits in bilateral coordination, EF, and emotional state (Nutt et al., 2011; Plotnik, Giladi, & Hausdorff, 2009; Plotnik & Hausdorff, 2008). Using VR to study and elucidate the mechanism of FOG enables to subject patients to different FOG-inducing situations in a safe environment. Park et al. described in a methodology paper the development of a virtual reality (VR)-based body weight-supported treadmill interface (BWSTI) designed and applied to investigate FOG. The VR-based BWSTI was tested with three patients with PD who were known to have FOG. Visual stimuli that might cause FOG were shown to them, while the speed adaptation controller adjusted treadmill speed to follow the subjects’ own preferred speed. Two of the three subjects demonstrated FOG during the treadmill walking. Shine, Ward, Naismith, Pearson, and Lewis (2011) reported a case study in which a VR simulation was used to investigate walking under dual-tasking conditions using fMRI. The participant was instructed to simulate walking by pressing two pedals while concurrently performing cognitive tasks such as the stroop test or following simple commands on a screen. The results showed distinct activation patterns during “walking,” “dual-task walking,” and episodes of freezing. Patients with FOG exhibited delayed motor responses (Gilat et al., 2013; Matar, Shine, Naismith, & Lewis, 2013; Shine et al., 2012), impaired sequencing (Matar et al., 2013), and a specific decrease in neural activation in the anterior insula, ventral striatum, and subthalamic nucleus (STN) (Shine, Matar, et al. 2013; Shine, Naismith, et al. 2013) demonstrating a distinct control of gait. Together these studies highlight the potential utility of VR in elucidating the underlying neural correlates of the freezing phenomenon in PD. The relatively large number of studies that used VR to assess FOG may be related to the unique susceptibility of FOG to cognitive, emotional, and sensory stimulation which can easily be manipulated using VR and is more challenging to reproduce overground (Mirelman, Maidan, & Deutsch, 2013).
8.6.2 Multiple Sclerosis
Very few studies have looked at the use of VR for treatment of MS-related gait disorders. Fulk (2005) described the results of a locomotor training using both a body weight support (BWS) with a treadmill (TM) and overground walking as well as a VR-based balance intervention to improve walking ability, balance, and endurance for a 48-year-old female with MS. The intervention was provided twice weekly for 12 weeks and after which the patient showed improved gait speed, endurance, and balance. These improvements were sustained for at least 2 months post-intervention.
Baram and Miller used a portable visual-feedback VR apparatus consisting of stereoscopic glasses to provide visual cues of a virtual tiled floor in a checkerboard arrangement, responding dynamically to the patient’s own motion, much like a real floor, fixed in space. In their first study (Baram & Miller, 2006), 16 patients with cerebellar ataxia due to MS participated in a single evaluation session consisting of four training bouts. In general, subjects with moderate-to-severe gait impairments showed an average online improvement (while walking with the device) of 13.46 % in their walking speed, while patients whose baseline walking speed was above the median walking speed of the group improved their speed by 1.47 %. In a follow-up study (Baram & Miller, 2010), 10 patients trained with a simulation that provided cues of transverse lines while 11 patients trained with virtual checkerboard tiles, both provided by a wearable virtual reality device. Following 20-min training with the device and 10-min rest, performance without the device was measured again and compared to the baseline performance. The group training with the transverse tiles showed significantly better immediate results in walking speed and stride length overground as compared to the control group; however, long-term training effects were not assessed and therefore the transfer and retention of this training to “real-world” environment are yet to be studied.
8.6.3 Older Adults
Reports on the use of VR for training of balance, gait, and fall risk among older adults are also scarce. The use of VR for older adults has been primarily used for balance training and cognitive training or to improve upper extremity function (Cherniack, 2010; de Bruin, Schoene, Pichierri, & Smith, 2010). Pichierri, Wolf, Murer, and de Bruin (2011) recently reviewed nine studies that used computerized interventions such as VR or gaming for training of older adults, but only two of those investigated forms of mobility. de Bruin, Dorflinger, et al. (2010) studied the transfer effects on gait characteristics of elderly who executed a traditional progressive physical balance and resistance training with integrated computer game of dancing (Dance Dance Revolution). The task of the dancing game consisted of stepping on arrows on a dance pad. Results indicated a positive effect of the computer game dancing training on relative DT costs of walking, e.g., stride time and step length. The more traditional physical training consisting of fitness and balance exercises showed no transfer effects to DT cost-related gait characteristics.
In another study looking at perceptual adaptation (Buccello-Stout et al., 2008), 16 adults, aged 66–81 years, were randomized to one of the two groups. Both groups first completed six trials of walking an obstacle course. Participants then trained twice a week for 4 weeks. In the training, the control group walked on a treadmill for 20 min while viewing a static visual scene and the experimental group walked on a treadmill for 20 min while viewing a rotating visual scene that provided a perceptual-motor mismatch. Following training, both groups were tested again on the obstacle course. The group trained with the rotating visual scene performed faster on the obstacle course and had fewer penalties than those who received a static visual scene, and training effects were retained for at least 4 weeks. Exposure to perceptual-motor mismatch induced information processing and provided a motor–cognitive training that resulted in an adaptive training effect that improved balance and gait in this group of older adults.
Recently, Mirelman et al.(2011) conducted a pilot study among five elderly idiopathic fallers who trained using the same TT + VR protocol as described above (in the study with patients with PD) (Mirelman et al., 2011). The purpose of the study was to examine the effects of training with VR on the frequency of falls measured over a period of 6 months. Five elderly females (mean age 78.2 ± 5.3 years), with a history of more than two falls in the 6 months prior to the study and who were otherwise healthy, participated in the study. Subjects walked on a treadmill while negotiating virtual obstacles three times a week for 6 weeks. After 6 weeks, improvements in gait speed and stride length were observed under usual, DT, and obstacle negotiation conditions. Additional very promising results include improvements in endurance and functional abilities and a marked decrease (improvement) in the DT cost. Frequency of falls in this small pilot study decreased by 73 % compared to the fall rate 6 months before the intervention. This very exciting finding suggests that perhaps using VR for motor–cognitive training in the elderly could lead to enhanced usual walking performance and major improvements in the ability to allocate attention to simultaneous tasks, and subjects learn to walk safely when negotiating obstacles. Conceivably these gains could then potentially reduce fall risk and fall rate in this population.
8.7 Future Directions
Patients with neurodegenerative disease suffer from deficits in motor and cognitive function that lead to an increased risk of falls. Until recently, therapeutic options for this population consisted of maintaining function and preventing deterioration. In the past decade there has been a shift in the understanding that even in the face of neurodegeneration, learning and plasticity can be achieved and hence treatment should be targeted towards improving function. However still, current therapeutic options do not fully address the multifactorial motor and cognitive deficits associated with neurodegeneration in an optimal fashion. The advances in technology, affordability, and accessibility have opened the door for assessing whether VR could be used for the geriatric population and for those with neurodegenerative diseases. There are only a small number of studies using VR for training gait and reducing falls in this population; however the evidence is encouraging demonstrating that VR is likely helpful for addressing impairments among a diverse group of older adults. However, large-scale randomized controlled trials are needed to provide evidence-based results for reducing fall frequency. In addition, many questions remain about optimal dosing, retention, and the utility of VR for achieving motor learning in the presence of neurodegenerative disease. The existing studies should provide a springboard for exciting future work.
References
Aarsland, D., Bronnick, K., Larsen, J. P., Tysnes, O. B., & Alves, G. (2009). Cognitive impairment in incident, untreated Parkinson disease: The Norwegian ParkWest study. Neurology, 72(13), 1121–1126.
Abbruzzese, G., Trompetto, C., & Marinelli, L. (2009). The rationale for motor learning in Parkinson’s disease. European Journal of Physical and Rehabilitation Medicine, 45(2), 209–214.
Adams, R., & Parsons, O. (2003). Neuropsychology for clinical practice: Etiology, assessment, and treatment of common neurologic disorders. Washington, DC: American Psychological Association.
Albani, G., Pignatti, R., Bertella, L., Priano, L., Semenza, C., Molinari, E., et al. (2002). Common daily activities in the virtual environment: A preliminary study in parkinsonian patients. Neurological Sciences, 23(Suppl. 2), S49–S50.
Alexander, N. B., & Hausdorff, J. M. (2008). Linking thinking, walking, and falling. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 63(12), 1325–1328.
Arnett, P. A., Rao, S. M., Grafman, J., Bernardin, L., Luchetta, T., Binder, J. R., et al. (1997). Executive functions in multiple sclerosis: An analysis of temporal ordering, semantic encoding, and planning abilities. Neuropsychology, 11(4), 535–544.
Ashburn, A., Stack, E., Pickering, R. M., & Ward, C. D. (2001). A community-dwelling sample of people with Parkinson’s disease: Characteristics of fallers and non-fallers. Age and Ageing, 30(1), 47–52.
Baltadjieva, R., Giladi, N., Gruendlinger, L., Peretz, C., & Hausdorff, J. M. (2006). Marked alterations in the gait timing and rhythmicity of patients with de novo Parkinson’s disease. European Journal of Neuroscience, 24(6), 1815–1820.
Baram, Y., & Miller, A. (2006). Virtual reality cues for improvement of gait in patients with multiple sclerosis. Neurology, 66(2), 178–181.
Baram, Y., & Miller, A. (2010). Glide-symmetric locomotion reinforcement in patients with multiple sclerosis by visual feedback. Disability and Rehabilitation. Assistive Technology, 5(5), 323–326.
Beauchet, O., Kressig, R. W., Najafi, B., Aminian, K., Dubost, V., & Mourey, F. (2003). Age-related decline of gait control under a dual-task condition. Journal of American Geriatrics Society, 51(8), 1187–1188.
Benedetti, M. G., Gasparroni, V., Stecchi, S., Zilioli, R., Straudi, S., & Piperno, R. (2009). Treadmill exercise in early multiple sclerosis: A case series study. European Journal of Physical and Rehabilitation Medicine, 45(1), 53–59.
Benedict, R. H., Holtzer, R., Motl, R. W., Foley, F. W., Kaur, S., Hojnacki, D., et al. (2011). Upper and lower extremity motor function and cognitive impairment in multiple sclerosis. Journal of the International Neuropsychological Society, 17(4), 643–653.
Benedict, R. H., & Zivadinov, R. (2011). Risk factors for and management of cognitive dysfunction in multiple sclerosis. Nature Reviews. Neurology, 7(6), 332–342.
Blake, A. J., Morgan, K., Bendall, M. J., Dallosso, H., Ebrahim, S. B., Arie, T. H., et al. (1988). Falls by elderly people at home: Prevalence and associated factors. Age and Ageing, 17(6), 365–372.
Bloem, B. R., Boers, I., Cramer, M., Westendorp, R. G., & Gerschlager, W. (2001). Falls in the elderly. I. Identification of risk factors. Wiener Klinische Wochenschrift, 113(10), 352–362.
Bloem, B. R., Hausdorff, J. M., Visser, J. E., & Giladi, N. (2004). Falls and freezing of gait in Parkinson’s disease: A review of two interconnected, episodic phenomena. Movement Disorders, 19(8), 871–884.
Bloem, B. R., Valkenburg, V. V., Slabbekoorn, M., & Willemsen, M. D. (2001). The multiple tasks test: Development and normal strategies. Gait & Posture, 14(3), 191–202.
Bloem, B. R., van Vugt, J. P., & Beckley, D. J. (2001). Postural instability and falls in Parkinson’s disease. Advances in Neurology, 87, 209–223.
Bond, J. M., & Morris, M. (2000). Goal-directed secondary motor tasks: Their effects on gait in subjects with Parkinson disease. Archives of Physical Medicine and Rehabilitation, 81(1), 110–116.
Bowen, F. P., Hoehn, M. M., & Yahr, M. D. (1972). Parkinsonism: Alterations in spatial orientation as determined by a route-walking test. Neuropsychologia, 10(3), 355–361.
Bredesen, D. E., Rao, R. V., & Mehlen, P. (2006). Cell death in the nervous system. Nature, 443(7113), 796–802.
Brown, L. A., & Brockmole, J. R. (2010). The role of attention in binding visual features in working memory: Evidence from cognitive ageing. The Quarterly Journal of Experimental Psychology, 63(10), 2067–2079.
Brown, L. A., McKenzie, N. C., & Doan, J. B. (2005). Age-dependent differences in the attentional demands of obstacle negotiation. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 60(7), 924–927.
Buccello-Stout, R. R., Bloomberg, J. J., Cohen, H. S., Whorton, E. B., Weaver, G. D., & Cromwell, R. L. (2008). Effects of sensorimotor adaptation training on functional mobility in older adults. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 63(5), 295–300.
Buckner, R. L. (2004). Memory and executive function in aging and AD: Multiple factors that cause decline and reserve factors that compensate. Neuron, 44(1), 195–208.
Calabrese, P. (2006). Neuropsychology of multiple sclerosis—An overview. Journal of Neurology, 253(Suppl. 1), I10–I15.
Cameron, M. H., & Lord, S. (2010). Postural control in multiple sclerosis: Implications for fall prevention. Current Neurology and Neuroscience Reports, 10(5), 407–412.
Chapman, G. J., & Hollands, M. A. (2007). Evidence that older adult fallers prioritise the planning of future stepping actions over the accurate execution of ongoing steps during complex locomotor tasks. Gait & Posture, 26(1), 59–67.
Chen, H. C., Ashton-Miller, J. A., Alexander, N. B., & Schultz, A. B. (1994). Effects of age and available response time on ability to step over an obstacle. Journal of Gerontology, 49(5), M227–M233.
Cherniack, E. P. (2010). Not just fun and games: Applications of virtual reality in the identification and rehabilitation of cognitive disorders of the elderly. Disability and Rehabilitation. Assistive Technology, 6(4), 283–289.
Craik, F. I. M., & Grady, C. L. (2002). Aging, memory and frontal lobe functioning. In D. T. Stuss & R. T. Knight (Eds.), Principles of frontal lobe function (pp. 528–540). New York, NY: Oxford University Press.
Dam, M., Tonin, P., Casson, S., Bracco, F., Piron, L., Pizzolato, G., et al. (1996). Effects of conventional and sensory-enhanced physiotherapy on disability of Parkinson’s disease patients. Advances in Neurology, 69, 551–555.
Davidsdottir, S., Wagenaar, R., Young, D., & Cronin-Golomb, A. (2008). Impact of optic flow perception and egocentric coordinates on veering in Parkinson’s disease. Brain, 131(Pt 11), 2882–2893.
de Bruin, E., Dorflinger, M., Reith, A., & Murer, K. (2010). The effect of dance dance revolution gaming compared to conventional physical training on dual task walking costs in elderly. Parkinsonism & Related Disorders, 16, s59.
de Bruin, E. D., Schoene, D., Pichierri, G., & Smith, S. T. (2010). Use of virtual reality technique for the training of motor control in the elderly. Some theoretical considerations. Zeitschrift für Gerontologie und Geriatrie, 43(4), 229–234.
Deane, K. H., Ellis-Hill, C., Jones, D., Whurr, R., Ben Shlomo, Y., Playford, E. D., et al. (2002). Systematic review of paramedical therapies for Parkinson’s disease. Movement Disorders, 17(5), 984–991.
Deane, K. H., Jones, D., Ellis-Hill, C., Clarke, C. E., Playford, E. D., & Ben Shlomo, Y. (2001). A comparison of physiotherapy techniques for patients with Parkinson’s disease. Cochrane Database of Systematic Reviews, 1, CD002815.
D’Esposito, M., Ballard, D., Zarahn, E., & Aguirre, G. K. (2000). The role of prefrontal cortex in sensory memory and motor preparation: An event-related fMRI study. NeuroImage, 11(5 Pt 1), 400–408.
Deutsch, J. E., & Mirelman, A. (2007). Virtual reality-based approaches to enable walking for people poststroke. Topics in Stroke Rehabilitation, 14(6), 45–53.
Dorfman, J. (1998). Problem solving, inhibition and frontal lobe function. In N. Raz (Ed.), The other side of the error team: Aging and development as model systems in cognitive neuroscience (pp. 395–448). Amsterdam, The Netherlands: Elsevier Science.
D’Orio, V. L., Foley, F. W., Armentano, F., Picone, M. A., Kim, S., & Holtzer, R. (2012). Cognitive and motor functioning in patients with multiple sclerosis: Neuropsychological predictors of walking speed and falls. Journal of the Neurological Sciences, 316(1–2), 42–46.
Drew, M., Tippett, L. J., Starkey, N. J., & Isler, R. B. (2008). Executive dysfunction and cognitive impairment in a large community-based sample with multiple sclerosis from New Zealand: A descriptive study. Archives of Clinical Neuropsychology, 23(1), 1–19.
Ebersbach, G., Heijmenberg, M., Kindermann, L., Trottenberg, T., Wissel, J., & Poewe, W. (1999). Interference of rhythmic constraint on gait in healthy subjects and patients with early Parkinson’s disease: Evidence for impaired locomotor pattern generation in early Parkinson’s disease. Movement Disorders, 14(4), 619–625.
Ellis, T., de Goede, C. J., Feldman, R. G., Wolters, E. C., Kwakkel, G., & Wagenaar, R. C. (2005). Efficacy of a physical therapy program in patients with Parkinson’s disease: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 86(4), 626–632.
Fingerhut, L. A., Cox, C. S., & Warner, M. (1998). International comparative analysis of injury mortality. Findings from the ICE on injury statistics. International Collaborative Effort on Injury Statistics. Advance Data, 303, 1–20.
Fisk, J. D., Pontefract, A., Ritvo, P. G., Archibald, C. J., & Murray, T. J. (1994). The impact of fatigue on patients with multiple sclerosis. Canadian Journal of Neurological Sciences, 21(1), 9–14.
Freal, J. E., Kraft, G. H., & Coryell, J. K. (1984). Symptomatic fatigue in multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 65(3), 135–138.
Fulk, G. D. (2005). Locomotor training and virtual reality-based balance training for an individual with multiple sclerosis: A case report. Journal of Neurologic Physical Therapy, 29(1), 34–42.
Fung, J., Richards, C. L., Malouin, F., McFadyen, B. J., & Lamontagne, A. (2006). A treadmill and motion coupled virtual reality system for gait training post-stroke. Cyberpsychology & Behavior, 9(2), 157–162.
Fuster, J. M. (1999). Synopsis of function and dysfunction of the frontal lobe. Acta Psychiatrica Scandinavica, Supplement, 395, 51–57.
Gage, W. H., Sleik, R. J., Polych, M. A., McKenzie, N. C., & Brown, L. A. (2003). The allocation of attention during locomotion is altered by anxiety. Experimental Brain Research, 150(3), 385–394.
Galna, B., Murphy, A. T., & Morris, M. E. (2010). Obstacle crossing in people with Parkinson’s disease: Foot clearance and spatiotemporal deficits. Human Movement Science, 29(5), 843–852.
Gilat, M., Shine, J. M., Bolitho, S. J., Matar, E., Kamsma, Y. P. T., Naismith, S. L., et al. (2013). Variability of stepping during a virtual reality paradigm in Parkinson’s disease patients with and without freezing of gait. PLoS One, 8(6), e66718.
Gillespie, L. D., Robertson, M. C., Gillespie, W. J., Lamb, S. E., Gates, S., Cumming, R. G., et al. (2009). Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews, 2, CD007146.
Goldstein, D. S. (2003). Dysautonomia in Parkinson’s disease: Neurocardiological abnormalities. Lancet Neurology, 2(11), 669–676.
Goodwin, V. A., Richards, S. H., Taylor, R. S., Taylor, A. H., & Campbell, J. L. (2008). The effectiveness of exercise interventions for people with Parkinson’s disease: A systematic review and meta-analysis. Movement Disorders, 23(5), 631–640.
Gray, P., & Hildebrand, K. (2000). Fall risk factors in Parkinson’s disease. Journal of Neuroscience Nursing, 32(4), 222–228.
Graybiel, A. M. (2005). The basal ganglia: Learning new tricks and loving it. Current Opinion in Neurobiology, 15(6), 638–644.
Guadagnoli, M. A., Leis, B., Van Gemmert, A. W., & Stelmach, G. E. (2002). The relationship between knowledge of results and motor learning in Parkinsonian patients. Parkinsonism & Related Disorders, 9(2), 89–95.
Hausdorff, J. M., Balash, J., & Giladi, N. (2003). Effects of cognitive challenge on gait variability in patients with Parkinson’s disease. Journal of Geriatric Psychiatry and Neurology, 16(1), 53–58.
Hausdorff, J. M., Cudkowicz, M. E., Firtion, R., Wei, J. Y., & Goldberger, A. L. (1998). Gait variability and basal ganglia disorders: Stride-to-stride variations of gait cycle timing in Parkinson’s disease and Huntington’s disease. Movement Disorders, 13(3), 428–437.
Hausdorff, J. M., Doniger, G. M., Springer, S., Yogev, G., Giladi, N., & Simon, E. S. (2006). A common cognitive profile in elderly fallers and in patients with Parkinson’s disease: The prominence of impaired executive function and attention. Experimental Aging Research, 32(4), 411–429.
Hausdorff, J. M., Nelson, M. E., Kaliton, D., Layne, J. E., Bernstein, M. J., Nuernberger, A., et al. (2001). Etiology and modification of gait instability in older adults: A randomized controlled trial of exercise. Journal of Applied Physiology, 90(6), 2117–2129.
Hausdorff, J. M., & Yogev, G. (2006). Cognitive function may be important for fall injury prevention trials. Journal of the American Geriatrics Society, 54(5), 865–866.
Heikkila, V. M., Turkka, J., Korpelainen, J., Kallanranta, T., & Summala, H. (1998). Decreased driving ability in people with Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 64(3), 325–330.
Herman, T., Giladi, N., Gruendlinger, L., & Hausdorff, J. M. (2007). Six weeks of intensive treadmill training improves gait and quality of life in patients with Parkinson’s disease: A pilot study. Archives of Physical Medicine and Rehabilitation, 88(9), 1154–1158.
Herman, T., Giladi, N., Gurevich, T., & Hausdorff, J. M. (2005). Gait instability and fractal dynamics of older adults with a “cautious” gait: Why do certain older adults walk fearfully? Gait & Posture, 21(2), 178–185.
Herman, T., Giladi, N., & Hausdorff, J. M. (2009). Treadmill training for the treatment of gait disturbances in people with Parkinson’s disease: A mini-review. Journal of Neural Transmission, 116(3), 307–318.
Herman, T., Mirelman, A., Giladi, N., Schweiger, A., & Hausdorff, J. M. (2010). Executive control deficits as a prodrome to falls in healthy older adults: A prospective study linking thinking, walking, and falling. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 65(10), 1086–1092.
Holden, M. K. (2005). Virtual environments for motor rehabilitation: Review. Cyberpsychology & Behavior, 8(3), 187–211.
Jobges, M., Heuschkel, G., Pretzel, C., Illhardt, C., Renner, C., & Hummelsheim, H. (2004). Repetitive training of compensatory steps: A therapeutic approach for postural instability in Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 75(12), 1682–1687.
Jueptner, M., Frith, C. D., Brooks, D. J., Frackowiak, R. S., & Passingham, R. E. (1997). Anatomy of motor learning. II. Subcortical structures and learning by trial and error. Journal of Neurophysiology, 77(3), 1325–1337.
Kalron, A., Dvir, Z., & Achiron, A. (2010). Walking while talking—Difficulties incurred during the initial stages of multiple sclerosis disease process. Gait & Posture, 32(3), 332–335.
Kannus, P., Sievanen, H., Palvanen, M., Jarvinen, T., & Parkkari, J. (2005). Prevention of falls and consequent injuries in elderly people. Lancet, 366(9500), 1885–1893.
Keshner, E. A., & Weiss, P. T. (2007). Introduction to the special issue from the proceedings of the 2006 International Workshop on Virtual Reality in Rehabilitation. Journal of Neuroengineering and Rehabilitation, 4, 18.
Klinger, E., Chemin, I., Lebreton, S., & Marie, R. M. (2006). Virtual action planning in Parkinson’s disease: A control study. Cyberpsychology & Behavior, 9(3), 342–347.
Kurtais, Y., Kutlay, S., Tur, B. S., Gok, H., & Akbostanci, C. (2008). Does treadmill training improve lower-extremity tasks in Parkinson disease? A randomized controlled trial. Clinical Journal of Sport Medicine, 18(3), 289–291.
Larocca, N. G. (2011). Impact of walking impairment in multiple sclerosis: Perspectives of patients and care partners. Patient, 4(3), 189–201.
Laufer, Y., Dickstein, R., Chefez, Y., & Marcovitz, E. (2001). The effect of treadmill training on the ambulation of stroke survivors in the early stages of rehabilitation: A randomized study. Journal of Rehabilitation Research and Development, 38(1), 69–78.
Legters, K. (2002). Fear of falling. Physical Therapy, 82(3), 264–272.
Lezak, M. D. (1995). Neuropsychological assessment. New York, NY: Oxford University Press.
Li, F., Harmer, P., Fitzgerald, K., Eckstrom, E., Stock, R., Galver, J., et al. (2012). Tai chi and postural stability in patients with Parkinson’s disease. The New England Journal of Medicine, 366(6), 511–519.
Lin, M. T., & Beal, M. F. (2006). Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature, 443(7113), 787–795.
Lord, S. R., Smith, S. T., & Menant, J. C. (2010). Vision and falls in older people: Risk factors and intervention strategies. Clinics in Geriatric Medicine, 26(4), 569–581.
Lowenthal, J., Gruedlinger, L., Baltadjieva, R., Herman, T., Hausdorff, J. M., & Giladi, N. (2004). Effects of rhythmic auditory stimulation on gait dynamics in Parkinson’s disease. Movement Disorders, 19, S139.
Lowrey, C. R., Watson, A., & Vallis, L. A. (2007). Age-related changes in avoidance strategies when negotiating single and multiple obstacles. Experimental Brain Research, 182(3), 289–299.
Lundin-Olsson, L., Nyberg, L., & Gustafson, Y. (1997). “Stops walking when talking” as a predictor of falls in elderly people. Lancet, 349(9052), 617.
Lundin-Olsson, L., Nyberg, L., & Gustafson, Y. (1998). Attention, frailty, and falls: The effect of a manual task on basic mobility. Journal of the American Geriatrics Society, 46(6), 758–761.
Mahoney, J. E. (2010). Why multifactorial fall-prevention interventions may not work: Comment on “Multifactorial intervention to reduce falls in older people at high risk of recurrent falls”. Archives of Internal Medicine, 170(13), 1117–1119.
Marchese, R., Diverio, M., Zucchi, F., Lentino, C., & Abbruzzese, G. (2000). The role of sensory cues in the rehabilitation of parkinsonian patients: A comparison of two physical therapy protocols. Movement Disorders, 15(5), 879–883.
Marsh, A. P., & Geel, S. E. (2000). The effect of age on the attentional demands of postural control. Gait & Posture, 12(2), 105–113.
Matar, E., Shine, J. M., Naismith, S. L., & Lewis, S. J. (2013). Using virtual reality to explore the role of conflict resolution and environmental salience in freezing of gait in Parkinson’s disease. Parkinsonism & Related Disorders, 19(11), 937–942.
Mathiowetz, V., & Haugen, J. B. (1994). Motor behavior research: Implications for therapeutic approaches to central nervous system dysfunction. The American Journal of Occupational Therapy, 48(8), 733–745.
Menant, J. C., St George, R. J., Fitzpatrick, R. C., & Lord, S. R. (2010). Impaired depth perception and restricted pitch head movement increase obstacle contacts when dual-tasking in older people. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 65(7), 751–757.
Messier, J., Adamovich, S., Jack, D., Hening, W., Sage, J., & Poizner, H. (2007). Visuomotor learning in immersive 3D virtual reality in Parkinson’s disease and in aging. Experimental Brain Research, 179(3), 457–474.
Mirelman, A., Maidan, I., & Deutsch, J. E. (2013). Virtual reality and motor imagery: Promising tools for assessment and therapy in Parkinson’s disease. Movement Disorders, 28(11), 1597–1608.
Mirelman, A., Maidan, I., Herman, T., Deutsch, J. E., Giladi, N., & Hausdorff, J. M. (2010). Virtual reality for gait training: Can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 66(2), 234–240.
Mirelman A, Raphaeli Baer N, Dorfman M, Brozgol M, Giladi N, Hausdorff JM. (2011). Virtual Reality in Idiopathic fallers - A pilot study.: IEEE. doi: 10.1109/ICVR.2011.5971846.
Miyai, I., Fujimoto, Y., Ueda, Y., Yamamoto, H., Nozaki, S., Saito, T., et al. (2000). Treadmill training with body weight support: Its effect on Parkinson’s disease. Archives of Physical Medicine and Rehabilitation, 81(7), 849–852.
Miyai, I., Fujimoto, Y., Yamamoto, H., Ueda, Y., Saito, T., Nozaki, S., et al. (2002). Long-term effect of body weight-supported treadmill training in Parkinson’s disease: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 83(10), 1370–1373.
Montero-Odasso, M., Bergman, H., Phillips, N. A., Wong, C. H., Sourial, N., & Chertkow, H. (2009). Dual-tasking and gait in people with mild cognitive impairment. The effect of working memory. BMC Geriatrics, 9, 41–42.
Morris, M. E., Huxham, F. E., McGinley, J., & Iansek, R. (2001). Gait disorders and gait rehabilitation in Parkinson’s disease. Advances in Neurology, 87, 347–361.
Morris, M. E., Iansek, R., Matyas, T. A., & Summers, J. J. (1994). The pathogenesis of gait hypokinesia in Parkinson’s disease. Brain, 117(Pt 5), 1169–1181.
Morris, M. E., Iansek, R., Matyas, T. A., & Summers, J. J. (1996). Stride length regulation in Parkinson’s disease. Normalization strategies and underlying mechanisms. Brain, 119(Pt 2), 551–568.
Muir, G. D., & Steeves, J. D. (1997). Sensorimotor stimulation to improve locomotor recovery after spinal cord injury. Trends in Neurosciences, 20(2), 72–77.
Muslimovic, D., Post, B., Speelman, J. D., & Schmand, B. (2005). Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology, 65(8), 1239–1245.
Nieuwboer, A., Kwakkel, G., Rochester, L., Jones, D., van Wegen, E., Willems, A. M., et al. (2007). Cueing training in the home improves gait-related mobility in Parkinson’s disease: The RESCUE trial. Journal of Neurology, Neurosurgery, and Psychiatry, 78(2), 134–140.
Nutt, J. G., Bloem, B. R., Giladi, N., Hallett, M., Horak, F. B., & Nieuwboer, A. (2011). Freezing of gait: Moving forward on a mysterious clinical phenomenon. Lancet Neurology, 10(8), 734–744.
O’Sullivan, S. B. (1984). Perceived exertion. A review. Physical Therapy, 64(3), 343–346.
Overstall, P. W., Exton-Smith, A. N., Imms, F. J., & Johnson, A. L. (1977). Falls in the elderly related to postural imbalance. British Medical Journal, 1(6056), 261–264.
Pashler, H. (1994). Dual-task interference in simple tasks: Data and theory. Psychological Bulletin, 116(2), 220–244.
Passingham, R. E. (1996). Attention to action. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 351(1346), 1473–1479.
Peyser, J. M., Rao, S. M., LaRocca, N. G., & Kaplan, E. (1990). Guidelines for neuropsychological research in multiple sclerosis. Archives of Neurology, 47(1), 94–97.
Pichierri, G., Wolf, P., Murer, K., & de Bruin, E. D. (2011). Cognitive and cognitive-motor interventions affecting physical functioning: A systematic review. BMC Geriatrics, 11, 29.
Pilutti, L. A., Lelli, D. A., Paulseth, J. E., Crome, M., Jiang, S., Rathbone, M. P., et al. (2011). Effects of 12 weeks of supported treadmill training on functional ability and quality of life in progressive multiple sclerosis: A pilot study. Archives of Physical Medicine and Rehabilitation, 92(1), 31–36.
Plotnik, M., Giladi, N., & Hausdorff, J. M. (2009). Bilateral coordination of gait and Parkinson’s disease: The effects of dual tasking. Journal of Neurology, Neurosurgery, and Psychiatry, 80(3), 347–350.
Plotnik, M., & Hausdorff, J. M. (2008). The role of gait rhythmicity and bilateral coordination of stepping in the pathophysiology of freezing of gait in Parkinson’s disease. Movement Disorders, 23(Suppl. 2), S444–S450.
Radford, K., Lincoln, N., & Lennox, G. (2004). The effects of cognitive abilities on driving in people with Parkinson’s disease. Disability and Rehabilitation, 26(2), 65–70.
Rao, S. M., Leo, G. J., Ellington, L., Nauertz, T., Bernardin, L., & Unverzagt, F. (1991). Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology, 41(5), 692–696.
Robinson, K., Dennison, A., Roalf, D., Noorigian, J., Cianci, H., Bunting-Perry, L., et al. (2005). Falling risk factors in Parkinson’s disease. NeuroRehabilitation, 20(3), 169–182.
Rochester, L., Baker, K., Hetherington, V., Jones, D., Willems, A. M., Kwakkel, G., et al. (2010). Evidence for motor learning in Parkinson’s disease: Acquisition, automaticity and retention of cued gait performance after training with external rhythmical cues. Brain Research, 1319, 103–111.
Rowe, J., Stephan, K. E., Friston, K., Frackowiak, R., Lees, A., & Passingham, R. (2002). Attention to action in Parkinson’s disease: Impaired effective connectivity among frontal cortical regions. Brain, 125(Pt 2), 276–289.
Rubenstein, T. C., Giladi, N., & Hausdorff, J. M. (2002). The power of cueing to circumvent dopamine deficits: A review of physical therapy treatment of gait disturbances in Parkinson’s disease. Movement Disorders, 17(6), 1148–1160.
Rubenstein, L. Z., & Josephson, K. R. (2006). Falls and their prevention in elderly people: What does the evidence show? The Medical Clinics of North America, 90(5), 807–824.
Rubinsztein, D. C. (2006). The roles of intracellular protein-degradation pathways in neurodegeneration. Nature, 443(7113), 780–786.
Schaafsma, J. D., Giladi, N., Balash, Y., Bartels, A. L., Gurevich, T., & Hausdorff, J. M. (2003). Gait dynamics in Parkinson’s disease: Relationship to Parkinsonian features, falls and response to levodopa. Journal of the Neurological Sciences, 212(1–2), 47–53.
Schenkman, M., & Butler, R. B. (1989). A model for multisystem evaluation treatment of individuals with Parkinson’s disease. Physical Therapy, 69(11), 932–943.
Schwenk, M., Zieschang, T., Oster, P., & Hauer, K. (2010). Dual-task performances can be improved in patients with dementia: A randomized controlled trial. Neurology, 74(24), 1961–1968.
Sheridan, P. L., Solomont, J., Kowall, N., & Hausdorff, J. M. (2003). Influence of executive function on locomotor function: Divided attention increases gait variability in Alzheimer’s disease. Journal of American Geriatrics Society, 51(11), 1633–1637.
Shine, J. M., Matar, E., Bolitho, S. J., Dilda, V., Morris, T. R., Naismith, S. L., et al. (2012). Modeling freezing of gait in Parkinson’s disease with a virtual reality paradigm. Gait Posture, 38(1), 104–108.
Shine, J. M., Matar, E., Ward, P. B., Bolitho, S. J., Gilat, M., Pearson, M., et al. (2013). Exploring the cortical and subcortical functional magnetic resonance imaging changes associated with freezing in Parkinson’s disease. Brain, 136(Pt 4), 1204–1215.
Shine, J. M., Naismith, S. L., Palavra, N. C., Lewis, S. J., Moore, S. T., Dilda, V., et al. (2013). Attentional set-shifting deficits correlate with the severity of freezing of gait in Parkinson’s disease. Parkinsonism & Related Disorders, 19(3), 388–390.
Shine, J. M., Ward, P. B., Naismith, S. L., Pearson, M., & Lewis, S. J. (2011). Utilising functional MRI (fMRI) to explore the freezing phenomenon in Parkinson’s disease. Journal of Clinical Neuroscience, 18(6), 807–810.
Shumway-Cook, A., Woollacott, M., Kerns, K. A., & Baldwin, M. (1997). The effects of two types of cognitive tasks on postural stability in older adults with and without a history of falls. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 52(4), M232–M240.
Stuss, D. T., & Alexander, M. P. (2000). Executive functions and the frontal lobes: A conceptual view. Psychological Research, 63(3–4), 289–298.
Thaut, M. H., McIntosh, G. C., Rice, R. R., Miller, R. A., Rathbun, J., & Brault, J. M. (1996). Rhythmic auditory stimulation in gait training for Parkinson’s disease patients. Movement Disorders, 11(2), 193–200.
The Panel on Prevention of Falls in Older Persons American Geriatrics Society and British Geriatrics Society. (2011). Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society, 59(1), 148–157.
Tinetti, M. E., Speechley, M., & Ginter, S. F. (1988). Risk factors for falls among elderly persons living in the community. The New England Journal of Medicine, 319(26), 1701–1707.
Tomassini, V., Johansen-Berg, H., Jbabdi, S., Wise, R. G., Pozzilli, C., Palace, J., et al. (2012). Relating brain damage to brain plasticity in patients with multiple sclerosis. Neurorehabilitation and Neural Repair, 26(6), 581–593.
Toole, T., Maitland, C. G., Warren, E., Hubmann, M. F., & Panton, L. (2005). The effects of loading and unloading treadmill walking on balance, gait, fall risk, and daily function in Parkinsonism. NeuroRehabilitation, 20(4), 307–322.
van Iersel, M. B., Kessels, R. P., Bloem, B. R., Verbeek, A. L., & Olde Rikkert, M. G. (2008). Executive functions are associated with gait and balance in community-living elderly people. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 63(12), 1344–1349.
Van Wegen, E., Lim, I., de Goede, C., Nieuwboer, A., Willems, A., Jones, D., et al. (2006). The effects of visual rhythms and optic flow on stride patterns of patients with Parkinson’s disease. Parkinsonism & Related Disorders, 12(1), 21–27.
Verghese, J., Buschke, H., Viola, L., Katz, M., Hall, C., Kuslansky, G., et al. (2002). Validity of divided attention tasks in predicting falls in older individuals: A preliminary study. Journal of the American Geriatrics Society, 50(9), 1572–1576.
Vitorio, R., Pieruccini-Faria, F., Stella, F., Gobbi, S., & Gobbi, L. T. (2010). Effects of obstacle height on obstacle crossing in mild Parkinson’s disease. Gait & Posture, 31(1), 143–146.
Weerdesteyn, V., Rijken, H., Geurts, A. C., Smits-Engelsman, B. C., Mulder, T., & Duysens, J. (2006). A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology, 52(3), 131–141.
Weinshenker, B. G. (1994). Natural history of multiple sclerosis. Annals of Neurology, 36(Suppl.), S6–S11.
Winstein, C. J. (1990). Designing practice for motor learning: Clinical implications. Paper presented at II STEP Conference, 1990.
Wood, B. H., Bilclough, J. A., Bowron, A., & Walker, R. W. (2002). Incidence and prediction of falls in Parkinson’s disease: A prospective multidisciplinary study. Journal of Neurology, Neurosurgery, and Psychiatry, 72(6), 721–725.
Woollacott, M., & Shumway-Cook, A. (2002). Attention and the control of posture and gait: A review of an emerging area of research. Gait & Posture, 16(1), 1–14.
Wu, T., & Hallett, M. (2005). A functional MRI study of automatic movements in patients with Parkinson’s disease. Brain, 128(Pt 10), 2250–2259.
Yogev, G., Giladi, N., Peretz, C., Springer, S., Simon, E. S., & Hausdorff, J. M. (2005). Dual tasking, gait rhythmicity, and Parkinson’s disease: Which aspects of gait are attention demanding? The European Journal of Neuroscience, 22(5), 1248–1256.
Yogev, G., Plotnik, M., Peretz, C., Giladi, N., & Hausdorff, J. M. (2006). Gait asymmetry in patients with Parkinson’s disease and elderly fallers: When does the bilateral coordination of gait require attention? Experimental Brain Research, 177(3), 336–346.
Yogev-Seligmann, G., Giladi, N., Brozgol, M., & Hausdorff, J. M. (2012). A training program to improve gait while dual tasking in patients with Parkinson’s disease: A pilot study. Archives of Physical Medicine and Rehabilitation, 93(1), 176–181.
Yogev-Seligmann, G., Hausdorff, J. M., & Giladi, N. (2008). The role of executive function and attention in gait. Movement Disorders, 23(3), 329–342.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Mirelman, A., Deutsch, J.E., Hausdorff, J.M. (2014). Virtual Reality Augmented Training for Improving Walking and Reducing Fall Risk in Patients with Neurodegenerative Disease. In: Weiss, P., Keshner, E., Levin, M. (eds) Virtual Reality for Physical and Motor Rehabilitation. Virtual Reality Technologies for Health and Clinical Applications. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0968-1_8
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0968-1_8
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0967-4
Online ISBN: 978-1-4939-0968-1
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)