Abstract
This chapter examines physiological responses to variations in environmental pressure and physical effects of pressure. High pressure also has an effect on action of drugs on the human body. Effects of high-pressure environments are described on various systems of the body, particularly the nervous system. Hearing and vestibular functions, as well as taste sensation, are impaired under high pressure. In addition to detailing effects on specific body systems, the symptoms and treatments related to a variety of pressure-induced medical conditions are presented.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Complications of diving
- Decompression sickness
- Diver’s headache
- Diver’s vertigo
- Diving medicine
- Environmental pressure
- High-pressure neurological syndrome
- Middle ear damage in diving
- Nitrogen narcosis
- Pressure and action of drugs
Physical Effects of Pressure
When human beings descend beneath the surface of the sea, they are subjected to tremendous pressure increases. To keep the thorax from collapsing, air must be supplied under high pressure, which exposes the blood in the lungs to extremely high alveolar gas pressures. This is known as hyperbarism. Workers in caissons, for example, must work in pressurized areas.
Relation of Sea Depth to Pressure. A vertical column of sea water 33 ft (~10 m) high exerts the same absolute pressure as that of the atmosphere at sea level (760 mmHg, as measured by a mercury barometer) and referred to as 1 ATA or 1.013 bar. Therefore, a person 33 ft beneath the surface of the sea is exposed to a pressure of 2 ATA (1 ATA caused by the weight of the water and 1 ATA by the air above the water) and a dive to 66 ft involves exposure to pressure of 3 ATA. Studies in diving medicine may refer to a dive to so many feet or the diver being subjected to so many ATA or bar. Similar terms are used to describe simulations in hyperbaric chambers.
Effect of Depth on Volume of Gases. Boyle’s law states that the volume to which a given quantity of gas is compressed is inversely proportional to the pressure. Thus, 1.0 L of air at sea level is compressed to 0.5 L at 10 m (33 ft).
The effects of pressure on the human body vary according to the following factors:
-
Total pressure
-
Duration of exposure to pressure
-
State of activity of the diver resting or exercising
-
Temperature
-
Drugs in the body
-
Gas mixtures used
-
Rate of descent
Effects of Pressure on Various Systems of the Body
Hematological and Biochemical Effects
A 14-day exposure to 5.2 % oxygen and nitrogen at pressure of 4 ATA has been shown to cause hemoconcentration with slight elevation of Hb, Hct, RBC, plasma proteins, and cholesterol because of a decrease of plasma volume with diuresis. Loss of intracellular fluid has been observed, but this reverses partially during the postexposure period. Weight loss has been observed in divers compressed to 49.5 ATA (488 msw) in He-oxygen environments. This loss was shown to be 3.7–10.2 kg in 14 days of hyperbaric exposure.
Diuresis occurs in practically all saturation dives and is associated with natriuresis at pressures greater than 31 ATA. Three mechanisms may be involved in the development of this diuresis:
-
1.
Inhibition of ADH release
-
2.
Inhibition of tubular reabsorption of NA+ (pressure inhibits active transcapillary transport of NA+)
-
3.
Inhibition of hydrostatic action of ADH on the tubules
Fluid loss induced by diving and/or weightlessness might also add substantially to the pressure-induced diuresis. Because the sense of thirst is impaired in hyperbaric environments, and the resultant fluid imbalance reduces performance of divers, countermeasures against fluid loss should be taken during operational saturation diving.
Effect on Ammonia Metabolism
Long-term exposure to hyperbaric conditions has been shown to increase blood urea in US Navy divers. This is interpreted as evidence of hyperammonemia because urea is formed with ammonia buffering.
Effect on Blood Cells and Platelets
Increase of neutrophils, blood platelets, and fibrinogen concentration in the blood plasma immediately after diving is of temporary character, being a typical reaction observed during diving. The values usually return to normal spontaneously. Environmental stress such as cold water may contribute to platelet activation, which plays an important role in the pathogenesis of prethrombotic states and thus may be responsible for decompression illness during compressed air diving.
Changes in the Respiratory System and Blood Gases
Breathing mixtures with normal oxygen content at pressures up to 60 bar produces moderate changes in respiration, compared with the pattern of respiration at normal ambient pressure. At pressures from 80 to 100 bar, oxygen transport is likely to be compromised by changes in hemoglobin affinity. Breathing of high concentrations of oxygen (pO2 over 500 mbar) causes retention of CO2 in the tissues, which leads to hyperventilation. However, if the subject is exercising, reduced chemoreceptor activity leads to impaired alveolar ventilation.
Rapid changes in environmental pressure produce an inequality between inspiratory and expiratory volumes; compression causes hypercapnia while decompression causes hypocapnia. The following influence the respiratory effects of pressure:
-
Position of the diver. The upright position causes less dyspnea than the prone position.
-
Physical activity, which increases the tendency for CO2 accumulation.
-
Gas density. The higher the density of the gas mixture breathed, the greater the airway resistance is; it therefore requires more energy to breathe denser mixtures.
If the diver uses a face mask, the breathing gas should provide a static lung load of approximately 0 to +10 cm of water (0–0.01 ATA) regardless of the diver’s orientation in the water.
The increased ventilation observed in experimental animals breathing He-oxygen mixtures at extremely high pressures (up to 10 MPa) is responsible for fatigue of the respiratory muscles and may lead to ventilatory failure.
Adaptation has been shown to occur during a 14-day exposure to a high nitrogen pressure environment of 4 ATA with naturally inspired oxygen tensions. This modification of respiratory control is exemplified by a diminished ventilatory response to CO2. The diminished response is more likely related to the density of respiratory gas than to the narcotic influence of the respired nitrogen.
Multiple diving exposures affect both the vital capacity and the forced rotatory flow rate of smaller lung volumes. This is evidence for the narrowing of the airways that may be secondary to diving-induced loss of elasticity of the lung tissue. Longitudinal studies of lung function in oxygen divers have shown that substantial exposure to elevated oxygen partial pressure while diving is not associated with an accelerated decline in lung function. Factors other than hyperoxia (e.g., venous gas microemboli and altered breathing gas characteristics) may account for the long-term effects that have been found in professional divers.
Hypoxic states usually do not occur in divers, but the response of divers to hypoxia is the same as that of nondivers. The effects of repeated acute exposures to breathing 100 % oxygen at pressure—such as those encountered during oxygen diving—may affect the peripheral oxygen chemosensors.
Effects on the Cardiovascular System
Exposure to hyperbaric environments has been shown to cause a variety of disturbances in the electrical activity of the mammalian heart. Arrhythmias under these conditions are considered to be the result of an increase in parasympathetic tone. Increased hydrostatic pressure also decreases excitability and conduction through direct effects on the myocardial cell membrane. Hyperbaric exposure alters cardiac excitation–contraction coupling in anesthetized cats during He-oxygen dives to 305 msw. Some conclusions of the studies of the effects of moderate hyperbaric exposure on the rat heart are as follows:
• Cardiac contractility is increased during hyperbaric exposures despite administration of calcium and sodium channel blockers, thus reducing the possibility of involvement of these channels in the mechanism of this effect. Starling’s mechanism or neurotransmitter involvement was also excluded.
-
Repeated hyperbaric exposures causes hypertrophy of the heart.
-
Left ventricular pressure increased at 5 bar and the degree of rise varied with the breathing gases used.
-
Heart rate remained unchanged in all normoxic experiments.
Doppler-echocardiographic studies in healthy divers indicate that circulating gas bubbles are associated with cardiac changes, suggesting a right ventricular overload and an impairment of ventricular diastolic performance. Postdive humoral and hematologic changes are consistent with the hypothesis that “silent” gas bubbles may damage pulmonary endothelium and activate the reactive systems of the human body.
The increased environmental pressure seems responsible for the hemodynamic rearrangement causing reduction of cardiac output seen in diving humans because most of the changes are observed during diving (Marabotti et al. 2009). Left ventricular diastolic function changes suggest a constrictive effect on the heart possibly accounting for cardiac output reduction. Breath holding (BH) induces progressive left ventricular (LV) enlargement both in air and whole-body immersion, associated with reduced LV ejection fraction and progressive hindrance to diastolic filling (Marabotti et al. 2013). For a similar apnea duration, SaO2 decreased less during immersed BH, indicating an O2-sparing effect of diving, suggesting that interruption of apnea was not triggered by a threshold critical value of blood O2 desaturation.
Changes in the Endocrine System
The following changes in the endocrine function can occur as a result of hyperbaric exposures exceeding 4 ATA (30 msw) while breathing 6.2 % nitrogen in oxygen:
-
Increase in the circulating levels of epinephrine, norepinephrine, and dopamine.
-
Decrease in ADH secretion without a change in aldosterone excretion.
-
Severe hyperbaric conditions associated with deep dives have a profound effect on male reproductive function due to fall in the quality of semen and oligozoospermia.
-
Decrease of thyroxine levels in the blood.
-
Increase in the insulin and angiotensin I level in plasma.
-
Increase in the circulating concentration of atrial naturetic factor (ANF, a diuretic hormone). This may explain the diuresis observed in divers.
The endocrine reactions as well as the accompanying reductions in cognitive performance in divers, however, may be the result of emotional reactions to the dive rather than the direct effect of nitrogen narcosis.
Effect on the Skeletal System
Dysbaric osteonecrosis is a type of avascular necrosis caused by ischemia and subsequent infarction of bone. This usually involves the head of the femur. The disruption of blood flow in bone has been attributed to the formation of nitrogen bubbles as a result of diving, but blood pressure at the femoral head has been shown to be reduced by prolonged exposure to compressed air. Dysbaric osteonecrosis has been reported in 25 % of workers who perform in high-pressure environments (Cimsit et al. 2007).
Effects of High-Pressure Environments on the Nervous System
Neuropsychological Effects
Scuba diving was shown to have adverse long-term neuropsychological effects only when performed in extreme conditions, i.e., cold water, with >100 dives per year, and maximal depth <40 m. Deterioration of both mental and motor function has been reported in dives to 10 and 13 ATA—while breathing air and at rest. Hyperbaric air at 7 ATA does not impair short-term or long-term memory in test subjects, but, long-term memory is impaired at 10 ATA although it recovers on switching to an 80/20 He-oxygen mixture.
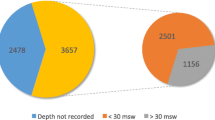
Non-saturation construction divers may not reveal clear evidence of neuropsychological deficit due to repeated diving but the prolonged reaction time can be ascribed to extensive non-saturation diving. Middle-aged divers who are exposed to critical depths of >60 msw have navigational problems and the number of brain lesions detected on MRI can be related to the number of hyperbaric exposures. There is a belief among occupational divers that a “punch drunk” effect is produced by prolonged compressed air diving. Most of the studies on this topic have serious limitations in statistical analysis and use of control groups. Dementia is recognized as a complication of severe hypoxia, cerebral embolism, or cerebral decompression sickness, but temporary neurological insults experienced by divers breathing compressed air cannot be translated into hard evidence of brain damage.
Nitrogen Narcosis
Behnke noted in 1935 that humans subjected to compressed air >5 ATA exhibited symptoms similar to alcohol intoxication. As the symptoms were immediate in onset and did not occur when He-oxygen mixtures were used, Behnke concluded that nitrogen was the causal agent. Since then many investigators have studied this phenomenon which Cousteau calls “l’ivresse des grandes profondeurs” or “rapture of the depths.” The symptoms of nitrogen narcosis are euphoria, dulled mental ability, difficulty in assimilating facts, and quick decision-making.
Many suggestions have been made to explain the narcotic effects of inert gases, but the most satisfactory explanation seems to be the degree of lipid solubility. Auditory evoked potential studies have been used to assess the degree of narcosis induced by diving and indicate that nitrogen is the major cause of compressed air narcosis and that oxygen does not have a synergistic effect with nitrogen. Some of the noble gases, which have been substituted for nitrogen, also tend to cause some narcosis, but to a much lesser degree. Nitrogen and a raised CO2 tension in the tissues as a result of hypoventilation and impaired CO2 elimination are the causes of narcosis, but they can also cause a deterioration in the performance of the affected diver. Increasing the oxygen partial pressure and the density of the breathing mixture causes retention of the carbon dioxide in the cerebral tissues and synergistically potentiates the nitrogen narcosis.
Most of these studies were carried out under hyperbaric conditions although nitrous oxide is known to be an inducer of narcosis at atmospheric pressure as well. Animal experimental studies indicate that nitrous oxide could be considered as a normobaric model of hyperbaric narcosis.
Effects of anesthetics and high-pressure nitrogen can be compared. Conventional anesthetics, including inhalational agents and inert gases, such as xenon and nitrous oxide, interact directly with ion channel neurotransmitter receptors. However, there is no evidence that nitrogen, which only exhibits narcotic potency at increased pressure, may act by a similar mechanism; rather nitrogen at increased pressure might interact directly with the GABAA receptor. Repetitive exposures to nitrogen narcosis produce a sensitization of postsynaptic N-methyl D-aspartate receptors on dopaminergic cells, related to a decreased glutamatergic input in substantia nigra pars compacta (Lavoute et al. 2008). Consequently, successive nitrogen narcosis exposures disrupt ion channel receptor activity revealing a persistent nitrogen-induced neurochemical change underlying the pathologic process.
Diving deeper than 100 m cannot be done breathing air, as the nitrogen contained in such a mixture becomes narcotic at pressures greater than 6 ATA. In order to avoid nitrogen narcosis, mixtures of helium and oxygen (heliox) are used, and this permits dives beyond 100 m.
High-Pressure Neurological Syndrome
This subject has been reviewed in detail elsewhere (Jain 1994, 2016). High-pressure neurological syndrome (HPNS) is a condition encountered in deep diving beyond a depth of 100 m which is made possible by breathing of special gas mixtures such as helium and oxygen (heliox). It is characterized by neurological, psychological, and electroencephalographic abnormalities. Clinical features of HPNS have been reviewed by several authors and can be summarized as follows:
Symptoms
-
Headache
-
Vertigo
-
Nausea
-
Fatigue
-
Euphoria
Neurological signs
-
Tremors
-
Postural sway
-
Opsoclonus
-
Myoclonus
-
Dysmetria
-
Hyperreflexia
-
Sleep disorders
-
Drowsiness
-
Convulsions (only in experimental animals)
Neuropsychiatric
-
Memory impairment
-
Cognitive deficits
-
Psychoses
Pathophysiology of HPNS
HPNS is primarily a result of excessive atmospheric pressure on different structures in the central nervous system (CNS). The rate of compression influences the manifestations of HPNS; a faster rate of compression increases the intensity of HPNS and decreases the pressure threshold for the onset of symptoms. The manifestations persist during a stay at a constant depth and decrease during decompression. The symptoms usually subside after the pressure is normalized, but some of these, such as lethargy, may linger on for days. In some cases, complaints such as memory disturbances take several months to resolve. Eventually, all of the divers who experience only HPNS recover. There is no evidence of permanent neurological sequelae or histopathological changes in the brain resulting from HPNS.
Intraspecies and interspecies variations of high-pressure neurological syndrome exist. There appears to be a genetic basis for adaptation to high-pressure neurological syndrome. Some individuals are more susceptible than others to development of the syndrome as a whole, or manifest various symptoms at different pressures. A single mutation in 3′UTR (untranslated region) of vacuolar protein sorting gene 52 (Vps52) is associated with greater than 60 % of the seizure risk difference between the high- and low-risk seizure susceptibility strains of mice (McCall 2011). By gene homology with human VPS52, this mutation may be considered a risk factor for seizures on exposure to high pressure.
High pressure differentially affects ionic currents of eight specific N-methyl-d-aspartate receptor subtypes generated by the co-expression of GluN1-1a or GluN1-1b with 1 of the 4 GluN2(A–D) subunits. A further study reports that eight GluN1 splice variants, when co-expressed with GluN2A, mediate different ionic currents at normal and high pressure of 45 atm, indicating that both GluN1 and GluN2 subunits play a critical role in determining N-methyl-d-aspartate receptor currents under normal and high-pressure conditions (Bliznyuk et al. 2015). Because of the differential spatial distribution of various N-methyl-d-aspartate receptor subtypes in the CNS, these data offer an explanation for the mechanism governing the complex signs and symptoms of high-pressure neurological syndrome as well as for the long-term health sequelae of repetitive deep dives by professional divers.
Sensitivity of the nervous system to high pressures may be compensated by a physiological adaptive response. Synaptic depression that requires less transmitter turnover may serve as an energy-saving mechanism when enzymes and membrane pumps activity are slowed down at pressure. Lethargy and fatigue, as well as reduction in cognitive and memory functions, are compatible with this state. Maladaptation to high pressure may lead to a pathophysiological response, i.e., HPNS. Some of the neurological signs may be an unmasking of previously silent brain lesions as a result of DCS. Various neurological manifestations appear at different depths. Tremor is seen at 200–300 m, myoclonus at 300–500 m, and EEG abnormalities are noted at 200–400 m.
Psychotic-like episodes in divers exposed to high pressure have been attributed to either the HPNS, confinement in pressure chamber, the subject’s personality, or the addition of nitrogen or hydrogen to the basic helium-oxygen breathing mixture used for deep diving. Alternatively, it is suggested that these disorders are in fact paroxysmal narcotic symptoms that result from the sum of the individual narcotic potencies of each inert gas in the breathing mixture. This hypothesis has been tested against a variety of lipid solubility theories of narcosis and the results clearly support the hypothesis that there are cellular interactions between inert gases at raised pressure and pressure itself.
Role of Neurotransmitters in the Pathogenesis of HPNS
Various neurotransmitters and amino acids have been implicated in the pathogenesis of HPNS: GABA, dopamine, serotonin (5-HT), acetylcholine, and glutamate. Conclusions from various studies on this subject are:
-
Various neurological and behavioral disturbances of HPNS are regulated by different mechanisms in the same areas of the brain.
-
Neurotransmitter interactions in HPNS differ in various parts of the brain.
-
The biochemical substrates for epileptic and HPNS-associated convulsions are different, for example, adenosine compounds protect against epilepsy but not against HPNS seizures.
The motor symptoms of HPNS are attributed to changes in neural excitability at spinal and midbrain levels. Serotonin may be implicated in hyperbaric spinal cord hyperexcitability. Quinolinic acid and kynurenine are metabolites of 5-HT that have been proposed as endogenous convulsants. The precise balance between these two may be an important determinant of onset of HPNS.
The clinical features of serotonin syndrome are changes in mental status, restlessness, myoclonus, hyperreflexia, shivering, and tremor. Behavioral changes in rats exposed to pressure resemble serotonin syndrome and are consistent with the activation of 5-HT receptor subtype 1A.
Prevention and Management of HPNS
Measures for the prevention and management of HPNS are as follows:
-
Reduction of the speed of compression
-
Modifications and additions to breathing gas mixtures: addition of nitrogen or hydrogen to heliox
-
Anesthetics
-
Barbiturates
-
Anticonvulsant drugs
-
Non-anesthetic compounds
A promising pharmacological approach is based on the resemblance of HPNS to serotonin syndrome. 5-HT1A receptor antagonists may provide a promising approach to prevent HPNS.
Headaches in Divers
Headaches in divers are uncommon include benign causes such as exertion, cold stimulus, migraine, and tension as well as serious causes such as decompression sickness, air embolism, and otic or paranasal sinus barotrauma. Inadequate ventilation of compressed gases can lead to carbon dioxide accumulation, cerebral vasodilatation, and headache. Rarely cerebral aneurysm rupture is associated with barotrauma. It is unclear whether volume expansion of trapped air, the blood pressure increase associated with barotrauma, or systemic vasodilation causes an aneurysm to rupture in this situation. Correct diagnosis and appropriate treatment require a careful history and neurologic examination as well as an understanding of the unique physiologic stresses of the subaquatic environment.
Central Nervous System Lesions in Divers
Decompression sickness is described in Chap. 10. Hyperintense lesions of the subcortical white matter seen on MRI are more common in amateur divers than in normal controls. These results differ from studies on saturation divers who have fewer such lesions than control subjects, even though neurological manifestations are more common among divers. Professional saturation diving involves breathing of helium/oxygen mixtures rather than compressed air as in the case of amateur divers. It is possible that MRI lesions in amateur divers are due to intravascular gas microbubbles. The only direct evidence for this is the demonstration by fluorescein angiography of pathological changes in the retinal microvasculature of divers even when they have not experienced decompression sickness.
Microbubble Damage to the Blood–Brain Barrier
Myelin damage has been discovered at the autopsy of divers with no recorded incidence of neurological decompression syndrome during life. Hyalinization of cerebral vessels has also been described in divers. Subtle neuropsychological changes in divers have not always been correlated with any pathology in the brain.
It has been proposed that as divers undergo decompression, microbubbles (15 ± 5 mm) pass the pulmonary filter into the cerebral arterial circulation and impair the blood–brain barrier, leading to extravasation of protein and focal cerebral edema (James and Hills 1988). This can account for the myelin damage and cerebral vascular pathology in divers.
Effect of Pressure on the Peripheral Nerve Conduction Velocity
Moderate pressure has been shown to increase nerve conduction velocity and amplitude in experimental animals, whereas high pressures depress these parameters. Various studies of nerve conduction velocities of divers at depth have concluded:
-
There is no significant correlation between slow sensory conduction and hyperbaric pressure.
-
Distal motor latencies increase with increases in hyperbaric pressure as well as with decreases in ambient temperature.
-
The effect of pressure is independent of the temperature.
-
No significant changes were detected in the main nerve trunk proximal to the wrist, or in the F-wave response.
-
The effect on peripheral nerves may contribute to the reduced work capacity of divers at depth.
-
Effect of hyperbaric pressure on autonomic nerve functions.
Autonomic nerve functions under severe hyperbaric pressure has been evaluated by measuring heart rate variability (HRV) and catecholamine excretion rate to assess sympathetic and parasympathetic tone in normal volunteers in submarine experimental facilities simulating conditions 330 m below sea level. There was significant negative correlation between HRV and urinary catecholamine levels. Evaluation of autonomic nerve functions under hyperbaric conditions by measuring HRV was shown to be a useful method. Thus, the present results indicate that the autonomic nerve functions of people who work under deep-sea conditions can be evaluated adequately by measuring HRV.
Hearing and Vestibular Impairment in Hyperbaric Environments
Hearing loss in professional divers is well known. A general etiological classification of hearing loss that is associated with hyperbaric environments is shown in Table 3.1. The hearing threshold in water appears to be 20–60 dB higher than in air. In the hyperbaric chamber, application of pressure on the middle ear or the external ear causes temporary impairment of hearing—especially in the low frequency range. At 4–11 ATA in hyperbaric air, the threshold of hearing is raised to 30–40 dB—proportional to the pressure. In a heliox environment at 31 ATA, the hearing loss does not exceed 30–40 dB. Conclusions of studies on this subject are:
-
Humans with patent Eustachian tubes, exposed to hyperbaric heliox conditions, develop a conductive hearing loss related to depth.
-
After exposure at a depth of 600 ft for several days, there is less variation in the hearing levels and a greater loss in the lower frequencies.
-
Sensory-neural auditory functions, as measured by sensory acuity levels and frequency differences, are not altered by hyperbaric heliox exposures up to 19.2 ATA.
-
The conductive hearing loss is assumed to be the result of an increased impedance of the middle ear transformer in the denser atmosphere plus an upward shift in resonance frequency of the ear in a helium atmosphere.
Damage to the Middle Ear and Inner Ear in Diving
The pressure changes that are encountered in diving can cause damage to the ear in at least three distinctly different ways:
-
1.
Middle ear barotrauma of descent
-
2.
Middle ear barotrauma as a manifestation of pulmonary barotrauma during ascent
-
3.
Inner ear barotrauma
Middle ear barotrauma occurs during descent when there is a failure to equalize the middle ear and the ambient pressures by means of the Eustachian tube. When this occurs, there may be bleeding in the middle ear and even rupture of the ear drum. Forceful autoinflation of the middle ear (Valsalva maneuver) during descent may cause rupture of the round window membrane and leakage of perilymph into the middle ear. Damage to the inner ear may occur by decompression sickness, that is, release of dissolved nitrogen bubbles during ascent from a deep dive. It can lead to hearing loss and dizziness. This damage is usually unilateral and can be reversed with prompt recompression procedure, including HBO therapy. Barotrauma of the ear has been shown to be preventable by myringotomy (puncture of the tympanic membrane) before the dive.
Temporal bones of divers who died of unrelated causes, but had a history of barotrauma of the ears have been examined the. The classical findings, shown in Figs. 3.1 and 3.2, are very similar to experimental findings in monkeys subjected to barotrauma. New bone formation in the inner ear following decompression sickness may have been responsible for the late onset of hearing deficits.
(a, b) Middle and inner ears, left (top) and right (bottom) of a diver who died underwater from unknown causes. Left ear has the round window membrane (M) ripped (black arrow) and the middle ear is filled with blood (white arrow). C cochlea, A lateral ampullary crista, S footplate of stapes. Photos courtesy of Dr. K.E. Money, reproduced from Money et al. (1985)
Professional diving may cause a more rapid deterioration of high frequency hearing loss than is seen in the general population. An audiometric survey of abalone divers has shown that >60 % of them suffered from high frequency deafness unacceptable by the Australian standards. The hearing loss was unilateral in one-half of the cases and bilateral in the rest.
In experimental studies, minipigs subjected to a compression/decompression profile that was considered to be safe for compressed air workers showed that there was loss of hearing as well as loss of hair cells in the cochlea of all the compressed animals.
Vertigo and Diving
Because of the close anatomical relationship between the hearing organ and the vestibular apparatus, vestibular disorders like dizziness and vertigo are frequently associated with barotrauma of the ear. Inner ear barotraumas and decompression sickness may cause acute vestibular symptoms in divers. The result may be irreversible damage to the vestibular end organs or their central connections. An etiological classification of vertigo in divers is shown in Table 3.2.
In a survey of divers and nondiver controls, the prevalence of dizziness (28 %), spinning vertigo (14 %), and unsteady gait (25 %) was significantly higher in divers than controls (Goplen et al. 2007). These symptoms were strongly associated with a previous history of DCS, particularly Type I, which was reported by 61 % of the divers. Symptoms were less strongly associated with the number of dives. In divers with dizziness, the prevalence of abnormal postural sway, nystagmus, canal paresis, or pathological smooth pursuit was 32 %,9 %, 7 %, and 11 %, respectively. Among the reasons for the high prevalence of vestibular symptoms among the divers, the high exposure to DCS is probably an important factor.
Inert gas narcosis may lead to balance disturbances and nystagmus. Velocity of the slow component of the vestibular ocular reflex, as determined by electronystagmography (ENG) increases by 50 % after inhalation of 25 % nitrous oxide. Caloric tests conducted during saturation dives to 450 msw (4.6 mPa) while breathing trimix do not show any significant nystagmus upon ENG.
Taste Sensation Under High Pressure
Significant changes in taste sensation have been shown to occur on exposure to heliox at 18.6 ATA. These changes include:
-
Increased sensitivity to sweetness
-
Increased sensitivity to bitter taste
-
Decline of sour sensitivity
-
Decrease of salt sensitivity
Effect of High Pressure on Effect of Drugs
The efficiency of a number of drugs is affected by pressure—usually manifested as a decrease in activity—but the results may be unpredictable. High pressure has been reported to reduce the efficiency of drugs which act on cell membranes, such as anesthetics, tranquilizers, and narcotics. This effect is ascribed to the pressure changes affecting the cell membrane itself. The major enzyme involved in drug metabolism is cytochrome P-450 which is bound to the cell membrane. The effect of pressure on the membrane may be differential. The so-called pressure of anesthesia may be due to an antagonism, not only on a pharmacological level, but also on a physiological level via increased sensory feedback under high pressure.
Dimenhydrinate, an antihistamine, often is used by divers to control seasickness. Its effects in the hyperbaric environment have been poorly studied although decrements in learning were reported. Dimenhydrinate adversely affects mental flexibility and depth can impair memory. It is likely that these effects in combination increase the risk to scuba divers. Divers who suffer from severe seasickness may have to take dimenhydrinate to avoid the miseries of this condition, but they would be wise to incorporate extra margins of safety into planning dives.
Information on the manner in which high pressure affects the drug disposition in the body is scarce.
Conclusion
Important effects of pressure on the human body were reviewed in this chapter. This may be of interest to physicians who treat complications of diving with HBO. For those interested in diving medicine, several excellent texts are available including that by (Edmonds et al. 2015). The most important effect of high pressure is on the nervous system. This should be distinguished from oxygen toxicity. The major complication of diving and decompression sickness are discussed in Chap. 12; cerebral air embolization is described in Chap. 13.
References
Bliznyuk A, Aviner B, Golan H, Hollmann M, Grossman Y. The N-methyl-D-aspartate receptor’s neglected subunit—GluN1 matters under normal and hyperbaric conditions. Eur J Neurosci. 2015;42:2577–84.
Cimsit M, Ilgezdi S, Cimsit C, Uzun G. Dysbaric osteonecrosis in experienced dive masters and instructors. Aviat Space Environ Med. 2007;78:1150–4.
Edmonds C, Bennett M, Lippmann J, Mitchell S. Diving and subaquatic medicine. 5th ed. Boca Raton: CRC Press; 2015.
Goplen FK, Gr¢nning M, Irgens A, Sundal E, Nordahl SH. Vestibular symptoms and otoneurological findings in retired offshore divers. Aviat Space Environ Med. 2007;78:414–9.
Jain KK. High pressure neurological syndrome (HPNS). Acta Neurol Scand. 1994;90:45–50.
Jain KK. High pressure neurological syndrome. In: Greenamyre JT, editor. Medlink Neurology; 2016 (online).
James PB, Hills BA. Microbubbles damage the blood-brain barrier. Abstract 21. In: Proceedings of the XIV Annual meeting of the EUBS, Aberdeen, Scotland; 1988.
Lavoute C, Weiss M, Sainty JM, Risso JJ, Rostain JC. Post effect of repetitive exposures to pressure nitrogen-induced narcosis on the dopaminergic activity at atmospheric pressure. Undersea Hyperb Med. 2008;35:21–5.
Marabotti C, Scalzini A, Cialoni D, Passera M, L’Abbate A, Bedini R. Cardiac changes induced by immersion and breath-hold diving in humans. J Appl Physiol. 2009;106:293–7.
Marabotti C, Piaggi P, Menicucci D, Passera M, Benassi A, Bedini R, et al. Cardiac function and oxygen saturation during maximal breath-holding in air and during whole-body surface immersion. Diving Hyperb Med. 2013;43:131–7.
McCall RD. HPNS seizure risk: a role for the Golgi-associated retrograde protein complex. Undersea Hyperb Med. 2011;38(1):3–9.
Money KE, Buckingham IP, Calder IM, Johnson WH, King JD, Landolt JP, et al. Damage to the middle ear and the inner ear in underwater divers. Undersea Biomed Res. 1985;12:77–84.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Jain, K.K. (2017). Effects of Diving and High Pressure on the Human Body. In: Textbook of Hyperbaric Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-47140-2_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-47140-2_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-47138-9
Online ISBN: 978-3-319-47140-2
eBook Packages: MedicineMedicine (R0)