Abstract
The role of the venous system is to return blood to the heart under low pressure conditions, compared with the arterial system. In humans the haemodynamics of venous flow is significantly influenced by postural changes, due to venous compliance, and an understanding of the physics associated with changes in hydrostatic pressure in the veins informs discussion of the biomechanics of the venous system.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Learning outcomes-
1.
Describe the role of the venous circulation in providing storage capacity within the circulation.
-
2.
Describe the variation in compliance of the veins with transmural pressure and the implications of this on the resistance to flow as the veins collapse.
-
3.
Describe the features of venous compliance which allow the veins to act as a blood reservoir.
-
4.
Describe the role of the muscle pumps of the lower limb and the respiratory pump in returning blood from the legs to the heart and the importance of venous valves in this process.
-
5.
Describe how the distribution of venous valves varies throughout the circulation.
-
6.
Describe how changes in posture lead to changes in venous volume with attention to the associated timescales.
-
7.
Define what is meant by venous insufficiency and state complications associated with the condition.
-
8.
Describe the applications of B-mode and Doppler ultrasound in diagnosis of venous disease.
-
9.
Describe the features that characterise varicose veins.
-
10.
Describe the nature of deep vein thrombosis (DVT) and the factors associated with increased risk of DVT.
The role of the venous system is to return blood to the heart under low pressure conditions, compared with the arterial system. In humans the haemodynamics of venous flow is significantly influenced by postural changes, due to venous compliance, and an understanding of the physics associated with changes in hydrostatic pressure in the veins informs discussion of the biomechanics of the venous system. This chapter presents key concepts associated with the role of the venous system in the circulation, how these relate to normal physiological conditions and how these processes may be altered under abnormal conditions.
7.1 Properties and Function of the Venous System
A schematic representation of the venous circulation, focusing on the larger vessels, is provided in Fig. 7.1. In all regions of the body the anatomy of the venous system becomes more complex as the vessel caliber becomes smaller, terminating in branching networks, often mirroring the anatomy of the arterial circulation.
Schematic representation of the circulation, arteries are shown in red, veins in blue. Reproduced from Wikipedia; https://commons.wikimedia.org/wiki/File:Circulatory_System_en.svg. This image is in the public domain and was authored by Mariana Ruiz Villarreal
These networks are designed to return blood from organ systems and musculature and the complexity of the venous network is particularly pronounced in the peripheral circulation (i.e. hands, feet and cerebral circulation). In general the anatomy of the venous circulation is more variable than the arterial circulation between individuals, particularly in the extremities. This variability may arise from the inherent redundancy associated in the mechanisms for venous return, which are discussed in more detail in the following sections. This aspect of venous anatomy poses particular challenges when considering the biomechanics of the venous circulation in detail for individual subjects, rather than typical behaviour of the overall system.
7.1.1 Venous Composition and Compliance
An important function of the venous circulation is to provide storage capacity within the circulatory loop, typically 60–80 % of the total blood volume is stored within the venous system depending on both posture and activity (Meissner et al. 2007). The storage capacity of the veins arises from the compliance of the vessels, which is related to their geometry, material properties, influence of the surrounding tissue and variation in transmural pressure, defined as the difference between the internal and external pressures acting on the vein.
The vein wall is thinner than that of its companion artery and contains less smooth muscle. Under physiological pressure loading the diameter of the venous lumen is larger than that of neighbouring arteries, particularly in peripheral vessels. The elastic modulus of veins has been shown to vary considerably with vessel location, exhibiting a similar stiffening response to arteries with increase in pressure loading (Wesley et al. 1975). For a particular value of elastic modulus simple linear measures of vessel compliance (Eq. 7.2) predict higher compliance in the venous circulation due to the larger diameter and thinner wall of the veins.
where R is the vessel radius, h the wall thickness and E the Young’s modulus of the vessel wall. The increase in compliance arises from the higher circumferential stress in a larger, thinner vessel at a given pressure.
In addition to the contribution from passive mechanical properties the pressure–area response of the veins is determined by active processes including metabolic control and pressure and flow-mediated changes in venous tone (Monos et al. 1995).
7.1.2 Vessel Collapse and Nonlinear Pressure–Area Relationship
The linear approximation of Eq. 7.2 neglects the large changes in compliance of the veins which arise over the range of transmural pressures experienced by these vessels. When transmural pressure becomes negative, the compliance of the veins is nonlinear as a result of changes in geometry of the vessel cross-section. Under negative transmural pressure the vein does not remain circular in cross-section, becoming elliptical or adopting a dumbbell shape. The form of the vessel cross section is determined by the support conditions with different forms of response observed in vessels surrounded by muscular tissue (e.g. deep calf veins) than in those with less supporting tissue (e.g. vena cava).
To examine the mechanics of venous collapse the vein can be considered a thin-walled elastic cylinder. The initial circular cross-section of the vein will deform to adopt a non-circular cross section under a uniform pressure load, as illustrated in Fig. 7.2. This arises from the elastic instability of the system and the pressure at which this occurs can be obtained through consideration of small deformations of the tube and a linear analytical approach (Fung 1997), which predicts that the vein will adopt a non-circular form at the transmural pressure given by Eq. 7.3.
where p e is the external pressure, p the internal pressure and ν is the Poisson’s ratio of the vessel wall. Extension of the analysis of this deformation into the post-buckling regime was undertaken by Flaherty et al. (1972) using numerical integration. This analysis captures the self-contact of the cylinder and the rapid changes in cross-sectional area that occur with increase in pressure following the initial buckling response. Figure 7.3 illustrates these effects through the solution of a finite element model of a thin cylinder under uniform pressure load. This analysis recognizes the finite thickness of the cylinder and captures the variation of the stress across the wall.
Finite element model of a thin-walled cylinder under uniform pressure loading. The deformation demonstrates the initial buckling of the cylinder (a) and subsequent collapse leading to self-contact (e) and further contact with increasing pressure along the plane of symmetry. The contours in these plots show the equivalent strain values
The response of the finite element model demonstrates significant changes in the geometry of the cross-section as the transmural pressure becomes negative. It should be noted that these deformations arise from nonlinear geometric effects in this analysis and that the strain within the cylinder is relatively low throughout the deformation. These effects are distinct from the nonlinearities observed in both the arterial and venous pressure/area relationship under positive transmural pressure resulting from the nonlinear mechanical response of the vessel to loading due to the vessel wall constituents. For more complex analysis of the deformation of thin-walled elastic tubes, including 3D deformation effects and fluid-structure interaction, the reader is referred to more detailed reports (Grotberg and Jensen 2004).
The results of such analyses provide a description of the nonlinear pressure–area response (compliance) of the venous system, which is generally handled through the definition of a “tube-law” to describe this behaviour. The typical form of an analytical tube-law is shown in Fig. 7.4 along with the response of the vessel computed using the finite element approach for two vessel thicknesses (h/R = 0.1 and 0.05). The equation for the tube-law is given below, with K p the bending stiffness of the vessel, A the cross-sectional area and A0 the area at zero pressure:
From Fig. 7.4 it is clear that, as the transmural pressure becomes increasingly negative, small changes in pressure result in large changes in cross-sectional area. This allows the vein to act as a blood reservoir without large increases in venous pressure. With further decrease in transmural pressure the compliance of the vessel reduces, due to the self-contact illustrated in Fig. 7.3e, f which correspond to normalized pressure of −4.86 and −25 respectively.
7.1.3 Resistance to Flow and Supercritical Flow in Collapsed Veins
In addition to the nonlinear form of the pressure–area response, it is also evident that the effective resistance of the vein will change significantly during the collapse phase. As a result, regions of vein which are collapsed present a high resistance to flow, which provides a dynamic mechanism for flow limitation. This effect is clear from Fig. 7.3 where the flow travels through a small gap and viscous losses are high in the collapsed state (d–f) compared to flow within the vessel as the transmural pressure increases (a–c). This effect is also observed in the operation of a Starling resistor, originally used to control flow rates within a heart-lung machine.
More complex behaviour is observed under conditions where the local speed u of the blood within the vein, exceeds the speed c of propagation of waves along the vessel. Due to significant variations in both cross-sectional area and local compliance of the vein, which determines the wavespeed, it is possible to transition between subcritical (u < c) and supercritical (u > c) flows within a single vein. Detailed analysis of the implications of these effects has been examined using a 1D numerical model under steady flow conditions (Shapiro 1977).
As wavespeed decreases with increase in compliance, supercritical flow becomes more likely in conditions when the veins are partially collapsed, this occurs in the jugular vein and the superior vena cava when in the standing position and in the superficial circulation when the limb is raised above heart level, as described in Sect. 7.2.4.
7.1.4 Venous Return
Venous return is defined as the volume of blood returning to the right atrium from the systemic venous circulation. Maintaining venous return is important for obvious reasons to ensure that blood is continuously available to prime the pulmonary circulation thus, in turn, providing oxygenated blood to the left ventricle. The storage capacity of the venous system and the subtle relationship between pressure and volume within the veins allows the venous system to act as a ‘buffer’, regulating levels of venous return under transient changes in cardiac output.
Total venous return is determined by a number of contributing factors including; the pressure gradient between the peripheral veins and the right atrium, the resistance of the venous vascular bed, the influence of transient muscle pump activation (in particular the calf muscle pump) and the effects of the respiratory pump. As discussed above, the resistance of the venous bed can be strongly nonlinear due to the increased resistance of collapsed vascular segments, this is particularly notable in the abdomen during collapse of the vena cava under changes of abdominal pressure (Wallace et al. 2010). The mechanisms underlying the calf muscle pump and respiratory pump are discussed in more detail in the following sections. Both pumping mechanisms rely on the presence of venous valves.
7.1.5 Calf Muscle Pump
During exercise, increased cardiac output requires an associated increase in venous return. Augmentation of venous return from the legs is achieved through the action of the foot, calf and thigh muscle pumps, allowing venous return to be enhanced beyond the level associated with the pressure gradient between the legs and the heart. The anatomy of the calf muscle pump, which provides the most significant contribution, is shown in Fig. 7.5. The calf pump is formed by the action of the gastrocnemius and soleus muscles which contract and force blood out of the deep veins of the calf (anterior tibial, posterior tibial and peroneal veins) which drain into the popliteal vein at the knee.
The presence of competent venous valves within the lower limb ensures that blood ejected from the calf during muscle contraction is not able to return to the calf under the influence of gravity when the muscle relaxes. The refilling of the deep veins is achieved through inflow from the arterial circulation and from flow between the superficial and deep venous systems which is facilitated by the perforating veins. These vessels extend through the fascia to connect the deep and superficial venous circulation. Uni-directional flow from the superficial to the deep veins is dependent on the presence of valves within the perforating veins.
The physiological action of the calf muscle pump has informed design of prophylaxis to reduce incidence of DVT following surgery. This involves the use of an external cuff to apply intermittent compression to the calf, mimicking the contraction and relaxation of the calf muscle. Understanding of the mechanics associated with the transfer of pressure from the surface of the calf to the veins is important to predict the degree of collapse of the deep veins.
Numerical analysis combined with anatomical characterisation using magnetic resonance imaging (MRI) has provided a methodology to examine this behaviour in detail (Narracott et al. 2009). Figure 7.6a illustrates the deformation of the calf caused by inflation of an external cuff assessed using MRI and simulated using the finite element approach. The deep veins and arteries are arranged with two veins either side of a single artery and are identified as labelled in the figure.
a MRI image of calf following cuff inflation. The solid white outline shows the calf outline prior to cuff inflation, the mesh overlaid on the MRI image shows the finite element model of the calf following application of the cuff pressure. The deep veins and arteries are arranged with two veins either side of a single artery. b Collapse of deep vessels of the calf during cuff inflation, data is shown for six of the vessels labelled in a
Whilst MRI provides useful information on the overall calf deformation it is less effective for assessing the detail of vein collapse. This is due to the relatively low spatial resolution of the images and the fact that during the time required to acquire the image (order several minutes) refilling of the vein may occur due to arterial inflow. B-mode ultrasound imaging can be used to dynamically visualize the collapse of the veins during cuff inflation but the depth of the vessels makes this approach challenging. The importance of considering the anatomy of the calf is clear in this case, as the tibia and fibula influence the transfer of pressure from the surface of the calf to the deep vessels, resulting in less collapse of the anterior tibial veins, as shown in Fig. 7.6b.
Other applications of these techniques include study of the influence of continuous elastic compression on wall shear stress with the deep veins (Downie et al. 2008) and the effect of active muscular contraction on venous collapse (Rohan et al. 2015).
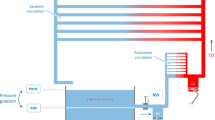
7.1.6 The Respiratory Pump
The respiratory pump enhances venous return through changes in pressure within the abdomen and the thorax. During inspiration the pressure decreases in the thorax and increases in the abdomen. These changes in pressure compress the vena cava in the abdomen and, as the vena cava does not possess valves, blood is expelled from the abdomen to the thorax and the extremity. Both the presence of valves in the veins of the legs and the decrease in thoracic pressure promote flow towards the heart. During expiration the pressure reduces in the abdomen and increases in the thorax. The pressure on the vena cava is reduced and refilling occurs as the valves below the abdomen open, priming the vena cava prior to further inspiration. As the pressure in the thorax is below atmospheric throughout the respiratory cycle, the vena cava is not compressed within this region.
Despite the presence of valves between the abdomen and the periphery, the influence of respiration on venous flow within the lower limbs has been demonstrated using Doppler ultrasound measurements to characterise the frequency of transient changes in flow rate in the common femoral vein (Abu-Yousef et al. 1997).
7.2 The Role of Venous Valves
The venous valves form during development of the cardiovascular system, initially as a bulging in the endothelial layer of the vein wall which covers the valve leaflet surface. The form of the valve is shown, as a longitudinal section, in Fig. 7.7. When developed, the valve leaflet consists of a thin elastic layer on the luminal surface and underlying collagen with very little connective tissue. Smooth muscle cells are only found in the valvular agger, where the valve attaches to the vein wall (Gottlob and May 1986).
7.2.1 Valve Geometry
Unlike the aortic valve, most venous valves are composed of two valve leaflets (bicuspid), although occasionally tricuspid valves have been observed. In addition to the valve leaflets the valve geometry often also features a pronounced sinus region similar to the aortic sinus, the valve sinus can be visualized during imaging studies such as contrast MR studies or X-ray venograms. The extent of the valve sinus is determined by the unstressed geometry of the vessel wall in this region and the distension of the sinus due to changes in transmural pressure, as the venous wall in the sinus region is thinner than other locations, making it more distensible (Kampmeier and La Fleur Birch 1927).
7.2.2 Valve Locations and Incidence
Valves are found within all components of the venous system (superficial, deep and perforating veins) and in general the number of valves increases from the central circulation to the peripheral circulation of the arms and legs.
The vena cava is reported to be without valves, with valves observed infrequently in the common iliac vein and more frequently in the external and internal iliac veins. Most subjects are observed to have a valve in the femoral vein and the popliteal vein is also reported to contain one or more valves. There is a significant increase in the number of valves in the deep veins below the knee, with at least 8 valves reported in the posterior and anterior tibial and peroneal veins (Gottlob and May 1986). The veins of the upper limb are also reported to contain a significant number of valves (Iimura et al. 2003). This increase in valves towards the periphery is associated with the importance of the skeletal muscle pump in the peripheral circulation.
7.2.3 Dynamic Valve Behaviour
Detailed descriptions of venous valve function in vivo are scarce due to the challenges in imaging the dynamic structure of the valve due to the thinness of the valve leaflets, the relatively small size of the valve and the tissue thickness between the skin and the deep veins. B-mode ultrasound imaging has provided data to characterise valve function in relation to changes in haemodynamics (Lurie et al. 2002, 2003; Nam et al. 2012). This data demonstrates distinct phases to valvular motion, including opening, closing and resting phases. It is notable that the valve leaflets undergo oscillatory motion during the ‘resting phase’ when the volume flow through the valve region is constant, this effect is similar to the observations of self-excited oscillations which occur during steady flow through compliant tubes, due to the strongly coupled interaction between the solid and fluid mechanics in such systems. The valve leaflets do not open fully to the vein wall, resulting in a reduction in the diameter of the vessel as shown in transverse cross-section in Fig. 7.8a. This local stenosis results in velocity augmentation through the valve and fluid recirculation in the valve sinus as shown in Fig. 7.8b. The vortices which form within the valve sinus whilst the valve is open result in a region of recirculating blood, which has implications for the development of valvular thrombosis.
The response of the valve under various physiological loading conditions has been described by Lurie et al. (2002); the loading includes normal respiration and simulated walking in both standing and recumbent positions. Such observations highlight the variability of venous haemodynamics and the changes in the nature of venous flow that occur within individual vascular compartments. The compliance of the venous system acts to reduce the influence of such variability on the overall form of the venous return. Observations of valve motion during quiet respiration along with reports of contraction of the musculature, even during quiet standing, and the influence of this effect on valve motion (Nam et al. 2012), demonstrates the sensitivity of the valves to changes in pressure and flow. Regular valve motion is considered to act as a protective mechanism against the formation of thrombosis behind the valve leaflets.
7.2.4 Influence of Postural Changes
Due to the distensibility of the venous system, changes in hydrostatic pressure lead to significant changes in venous volume. This effect is illustrated in Fig. 7.9 which shows the superficial veins of the hand in three positions (at the level of the head, at the level of the heart and below heart level).
The change in pressure in the vein is given by:
where h is the vertical distance from the reference position, g is the gravitational constant and ρ is the density of blood. The distension of the vein is noticeable under this magnitude of pressure variation. It is evident that the vessel is not collapsed when the hand is at the level of the heart, as the venous pressure is higher than that of the right atrium due to the pressure gradient required to sustain venous return from the periphery. These effects are also reported for veins in the deep circulation under changes in elevation of the leg (Cirovic et al. 2006). Variation in distensibility of the superficial and deep systems arises from the variation in support conditions of the vein as the deep veins do not collapse in the same manner, due to the support of the surrounding muscular tissue.
The hydrostatic pressure does not develop instantaneously upon change in posture, as fluid shifts are required to establish the hydrostatic pressure gradient, which will be impeded by venous valve closure. The changes described above are therefore the steady state conditions once the hydrostatic pressure gradient has developed. The timescale for establishment of the hydrostatic pressure when moving from sitting to standing is of the order 20 s (Pollack and Wood 1949). Similar effects are observed during walking which produces a transient reduction in the pressure within the veins as blood is expelled from the calf. When walking stops the pressure gradually increases to the value associated with the hydrostatic column due to refilling from the arterial circulation.
7.3 Biomechanics of Venous Disease
7.3.1 Venous Insufficiency
Venous insufficiency is defined as the lack of reduction of pressure in the deep veins of the lower limb during exercise and is associated with a range of complications which present clinical symptoms associated with poor venous return from the lower limb. Whilst clinical gradings have been developed to report the severity of disease, the underlying causes of poor venous return can be hard to assess. Chronic venous insufficiency can result in complications including ulceration, oedema and fibrosis (Meissner et al. 2007). Ultrasound imaging has become widely used as a tool to aid understanding of such vascular complications and diagnosis of the cause of venous insufficiency.
B-mode ultrasound can be used to assess venous anatomy and undertake vein mapping in the lower limb. This can be helpful to identify anatomical features in an individual which contribute to poor venous return including congenital absence of valves, valve incompetence and outflow obstruction. Doppler ultrasound is employed to assess the direction of flow during clinical tests and can provide quantitative measures of haemodynamics. This technique is used to assess the magnitude of reflux in the venous system following manual calf compression, muscle pump activation or the valsalva maneuver. Assessment along the length of a vein aids identification of specific valve sites associated with reflux, which can be used to target intervention. Kotani et al. (2007) report the use of M-mode ultrasound to assess the variation of valve geometry and examine valve incompetence demonstrating clear visualization of the incomplete closure of the valve leaflets.
7.3.2 Varicose Veins
The aetiology of varicose veins remains unclear as a number of mechanisms have been suggested to contribute to the eventual tortuosity of the superficial venous circulation which characterises the pathology. These include the failure or absence of valves leading to distension of the vein wall and alteration of the mechanical properties of the vein wall due to changes in the wall constituents. The biomechanical implications of increase of collagen concentration and reduced elasticity of the vein have been demonstrated using a finite element approach (Badel et al. 2013). This demonstrates the development of vessel tortuosity and the strong dependence of this effect on the axial pre-stretch of the vein.
7.3.3 Deep Vein Thrombosis
DVT is the development of thrombus within the deep veins, typically of the calf or thigh. DVT is often asymptomatic, if symptoms occur they include swelling of the limb and change in skin pigmentation. The most severe outcomes arise when the thrombus detaches from the vein and travels through the circulation. If the thrombus occludes the pulmonary arterial circulation, restricting blood from reaching the lungs, this results in a potentially fatal pulmonary embolism.
Post-mortem studies have indicated a tendency for DVT to form at venous valve sites. This has been linked to the generation of vortices within the valve sinus (Lurie et al. 2003; Karino and Motomiya 1984) whilst the valve remains in the open configuration, resulting in the recirculation of blood constituents and the potential for cellular damage due to the avascular nature of the valve leaflets and resulting reduction in PO2 tension (Malone and Agutter 2006). The biological response to this injury includes platelet aggregation and clot formation behind the valve leaflets.
The potential for thrombus formation is increased during periods of prolonged inactivity, such as long haul air travel or bed-rest following surgery, when the transient action of the muscle and respiratory pumps may not be sufficient to open and close the valves. These links between the biomechanics of valve function and the action of the muscle pump have led to the development of intermittent compression techniques to replicate the muscle pump and reduce DVT incidence in surgical patients, as described earlier.
References
Abu-Yousef MM, Mufid M, Woods KT, Brown BP, Barloon TJ. Normal lower limb venous Doppler flow phasicity: is it cardiac or respiratory? Am J Roentgenol. 1997;169:1721–5.
Badel P, Rohan CP, Avril S. Finite element simulation of buckling-induced vein tortuosity and influence of the wall constitutive properties. J Mech Behav Biomed Mater. 2013;26:119–26.
Cirovic S, Walsh C, Fraser WD, Gulino A. Venous filling and elastance in the calf positioned above and below heart level. Aviat Space Env Med. 2006;77:1009–14.
Downie SP, Raynor SM, Firmin DN, Wood NB, et al. Effects of elastic compression stockings on wall shear stress in deep and superficial veins of the calf. Am J Physiol Heart Circ Physiol. 2008;294:H2112–20.
Flaherty JE, Keller JB, Rubinow SI. Post buckling behavior of elastic tubes and rings with opposite sides in contact. SIAM J Appl Math. 1972;23:446–55.
Fung YC. Biomechanics. New York: Springer New York; 1997.
Gottlob R, May R. Venous valves. Vienna: Springer Vienna; 1986.
Grotberg JB, Jensen OE. Biofluid mechanics in flexible tubes. Ann Rev Fluid Mech. 2004;36:121–47.
Iimura A, Nakamura Y, Itoh M. Anatomical study of distribution of valves of the cutaneous veins of adult’s limbs. Ann Anat. 2003;185:91–5.
Kampmeier OF, La Fleur Birch C. The origin and development of the venous valves, with particular reference to the saphenous district. Am J Anat. 1927;38:451–499.
Karino T, Motomiya M. Flow through a venous valve and its implication for thrombus formation. Thromb Res. 1984;36:245–57.
Kotani A, Hirano Y, Yasuda C, Ishikawa K. A new ultrasonographic technique for diagnosing deep venous insufficiency–imaging and functional evaluation of venous valves by ultrasonography with improved resolution. Int J Cardiovasc Imaging. 2007;23:493–500.
Lurie F, Kistner RL, Eklof B. The mechanism of venous valve closure in normal physiologic conditions. J Vasc Surg. 2002;35:713–7.
Lurie F, Kistner RL, Eklof B, Kessler D. Mechanism of venous valve closure and role of the valve in circulation: a new concept. J Vasc Surg. 2003;38:955–61.
Malone PC, Agutter PS. The aetiology of deep venous thrombosis. Quart J Med. 2006;99:581–93.
Meissner MH, Moneta G, Burnand K, Gloviczki P, et al. The hemodynamics and diagnosis of venous disease. J Vasc Surg. 2007;46:4S–24S.
Monos E, Berczi V, Nadasy G. Local control of veins: biomechanical, metabolic, and humoral aspects. Physiol Rev. 1995;75:611–66.
Nam KH, Yeom E, Ha H, Lee SJ. Velocity field measurements of valvular blood flow in a human superficial vein using high-frequency ultrasound speckle image velocimetry. Int J Cardiovasc Imaging. 2012;28:69–77.
Narracott AJ, John GW, Morris RJ, Woodcock JP, Hose DR, Lawford PV. A validated model of calf compression and deep vessel collapse during external cuff inflation. IEEE Trans Biomed Eng. 2009;56:273–280.
Pollack AA, Wood EH. Venous pressure in the saphenous vein at the ankle in man during exercise and changes in posture. J Appl Physiol. 1949;1:649–62.
Rohan PY, Badel P, Lun B, Rastel D, Avril S. Prediction of the biomechanical effects of compression therapy on deep veins using finite element modelling. Ann Biomed Eng. 2015;43:314–24.
Shapiro AH. Steady flow in collapsible tubes. J Biomech Eng. 1977;99:126–47.
Wallace DJ, Allison M, Stone MB. Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med. 2010;17:96–9.
Wesly RL, Vaishnav RN, Fuchs JC, Patel DJ, Greenfield JC. Static linear and nonlinear elastic properties of normal and arterialized venous tissue in dog and man. Circ Res. 1975;37:509–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Narracott, A.J. (2017). The Venous System. In: Hoskins, P., Lawford, P., Doyle, B. (eds) Cardiovascular Biomechanics. Springer, Cham. https://doi.org/10.1007/978-3-319-46407-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-46407-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-46405-3
Online ISBN: 978-3-319-46407-7
eBook Packages: MedicineMedicine (R0)