Abstract
Popliteal artery aneurysms may be amenable to endovascular treatment with a stent graft. This chapter describes indications, essential steps, variations, and complications of this procedure. It provides a detailed template operative note for the procedure.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Indications
-
Asymptomatic popliteal artery aneurysm greater than 2 cm in diameter in the presence of suitable anatomy
-
Symptomatic popliteal artery aneurysm in the presence of suitable anatomy
Essential Steps
-
1.
Preoperative evaluation by CT angiography to determine suitable anatomy (2 cm landing zones and preferably two tibial vessel runoff).
-
2.
Antegrade percutaneous access of the ipsilateral common femoral artery or under local anesthesia expose the ipsilateral superficial femoral artery.
-
3.
Place a 5-French sheath.
-
4.
Obtain an angiogram to further document the suitable anatomy.
-
5.
Exchange the 5-French sheath into an 8-French sheath.
-
6.
Anticoagulate with intravenous heparin 75–100 IU/kg to keep ACT greater than 250 s.
-
7.
Evaluate the landing zones if intravascular ultrasound (IVUS) is available.
-
8.
Advance a glide wire into a tibial artery and then exchange into a stiff straight wire (260 cm).
-
9.
Obtain another angiogram with the stiff wire through the aneurysm and reassess the anatomy.
-
10.
Select the desired dimensions of the endoprosthesis (upsizing by 10 % and avoid excessive upsizing to prevent infolding of the graft).
-
11.
Mark the desired landing zones distally and proximally on the screen and using bony landmarks or roadmap.
-
12.
Introduce the endoprosthesis to the desired location.
-
13.
Obtain another angiogram to reconfirm desired landing location.
-
14.
Deploy the endoprosthesis.
-
15.
Remove the delivery system.
-
16.
Perform balloon angioplasty to mold/iron the endoprosthesis at the landing sites.
-
17.
Completion angiogram to check for endoleak or the need for another extension.
-
18.
Remove the sheath and close the puncture site with a closure device if performed percutaneously or with interrupted Prolene sutures if performed using an open superficial femoral artery exposure.
Note These Variations
-
Proper patient selection based on suitable anatomy is essential to the success of the procedure. If poor distal runoff or short landing zones, or presence of significant compression symptoms, an open repair is preferable especially if the patient is not a high medical risk for open procedure.
-
Access to the femoral vessel may be performed percutaneously or through an open approach. Due to the large-sized sheath, an open exposure of the superficial femoral artery under local anesthesia allows easy access and closure of the puncture side. If a percutaneous approach is used, a closure device should be considered for closing the puncture side to avoid excessive manual compression that may occlude the endoprosthesis or cause groin complications.
-
Various stent grafts and endoprostheses are available on the market.
-
It is preferable to avoid using multiple endoprostheses. However, if there is significant discrepancy between the diameter of the distal landing zone and the proximal landing zone, two stents grafts may be needed. The distal endoprosthesis is first deployed. The second endoprosthesis is then docked inside the distal with a good 2- to 3-cm overlap.
-
The patient is usually started on dual antiplatelet therapy with aspirin and clopidogrel prior to the procedure. Clopidogrel is usually maintained for 3 months postoperatively and aspirin indefinitely.
Complications
-
Thrombosis of endoprosthesis
-
Endoleak
-
Distal embolization
-
Bleeding
-
Gangrene
Template Operative Dictation
Preoperative Diagnosis
Asymptomatic ___-cm popliteal aneurysm/symptomatic ___-cm popliteal aneurysm with right/left leg-disabling claudication. Right/left foot rest pain. Right/left foot/toe ulcerations/gangrene
Procedure
Endovascular repair of right/left popliteal artery aneurysm using a _____ Viabahn/Fluency/other endoprostheses
Postoperative diagnosis
Same
Indications
The patient is a ___-year-old male/female with an asymptomatic ___-cm popliteal aneurysm/a symptomatic ___-cm popliteal aneurysm with right/left leg-disabling claudication, right/left foot rest pain, right/left foot/toe ulcerations/gangrene.
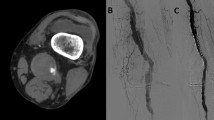
Preoperative evaluation revealed a right/left popliteal aneurysm with a patent popliteal artery and good tibial runoff and reconstitution of the anterior tibial/posterior tibial/peroneal artery. The landing zones were deemed appropriate for endovascular treatment.
The risks and benefits of endovascular aneurysm repair and alternatives with bypass and nonoperative management were explained to the patient, who elected to undergo endovascular intervention.
Description of Procedure
The procedure was performed under local monitored anesthesia. The patient was placed supine on the operating table. The arms were tucked in/placed at 80°. Normal bony prominences were padded. Time-outs were performed using both preinduction and pre-incision safety checklist to verify correct patient, procedure, site, and additional critical information prior to beginning the procedure. The anesthesia team placed appropriate lines. A Foley catheter was placed under sterile technique. The patient’s lower abdomen and both lower extremities were circumferentially prepped and draped in the usual sterile fashion. Preoperative antibiotics were administered prior to skin incision. The patient has been on dual antiplatelet therapy with aspirin and clopidogrel.
Alternative 1: Using a Seldinger technique and under ultrasound guidance, the common femoral artery was punctured in an antegrade manner. The wire was advanced into the superficial femoral artery. The micropuncture sheath was then exchanged into a size 5-French sheath.
Alternative 2: The skin over the course of the proximal superficial femoral artery was infiltrated with 1 % lidocaine. A 7-cm longitudinal incision was performed over the upper thigh and deepened through the subcutaneous tissue and fat. The superficial femoral artery was identified along the lower border of the sartorius muscle and was dissected for a 5-cm segment. Using Seldinger technique, a 5-French sheath was inserted.
Angiography through the sheath was performed delineating the location of the aneurysm and its proximal and distal landing zones. The anatomy appeared to be appropriate for endovascular graft treatment. The patient was given 75–100 IU of heparin intravenously to keep the activated clotting time (ACT) greater than 250 s. The 5-French sheath was exchanged for a size 8-French sheath. The intravascular ultrasound IVUS was introduced, and the landing zones were evaluated and confirmed to be appropriate. The superficial femoral artery/popliteal artery diameter was measured proximal and distal to the aneurysm. A glide wire was then introduced and manipulated through the aneurysm and advanced to the tibial arteries. The wire was then exchanged to an 260-cm Amplatz/straight tip stiff wire. A repeat angiogram was then performed with the stiff wire in place. The proximal and distal landing zones were marked using a Glow ′N Tell tape/erasable marker on the screen/bony landmarks. The appropriate size stent graft was selected. A size ____mm × ____cm Viabahn/Fluency graft was then introduced over the wire to the area of the aneurysm. The stent graft was then placed at the appropriate location. After an additional angiogram was performed to further confirm the appropriate position, the stent graft was deployed. The delivery system was then removed. A size ____mm × ____cm balloon was then used to mold each landing zone to maximize the apposition of the graft against the arterial wall. The balloon was then removed. An angiography was then performed and revealed proper placement with no evidence of any type I endoleak. There was no need for any additional extension limbs.
Alternative 1: The sheath was then removed and a closure device (Perclose) was used to close the puncture side.
Alternative 2: The sheath was removed, and the puncture hole in the superficial femoral artery was closed with interrupted 5-0 Prolene sutures. The wound was then closed with 3-0 absorbable sutures (Vicryl) for the subcutaneous tissue and 4-0 absorbable subcuticular sutures (Monocryl) for the skin.
A debriefing checklist was completed to share information critical to postoperative care of the patient.
The patient tolerated the procedure well and was transferred to the recovery room in good condition with excellent distal pulses and no complications.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Hoballah, J.J. (2017). Endovascular Treatment of Popliteal Artery Aneurysm. In: Hoballah, J., Scott-Conner, C., Chong, H. (eds) Operative Dictations in General and Vascular Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-44797-1_245
Download citation
DOI: https://doi.org/10.1007/978-3-319-44797-1_245
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-44795-7
Online ISBN: 978-3-319-44797-1
eBook Packages: MedicineMedicine (R0)