Abstract
This section provides a comprehensive procedural report for endovascular treatment of popliteal aneurysm procedure with up-to-date explanatory notes, synopsis of the indications and contraindications, and potential complications in an organized and practical format.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
INTRODUCTION
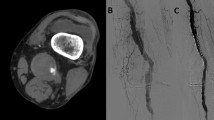
Popliteal Artery Aneurysms (PAAs) are the most prevalent type of peripheral arterial aneurysms, accounting for 70–80 % of all peripheral aneurysms. The current gold standard of PAA repair is ligation or resection of the aneurysm along with saphenous vein bypass. In high-risk patients or in those with no suitable vein conduit, another treatment option is endovascular exclusion of the aneurysm with covered stents. This approach provides shorter operative times, shorter hospital stays, and lower perioperative morbidity with a reported patency rate approximating 70 % at 6 years.
POSSIBLE COMPLICATIONS [1]
-
Access site bleeding
-
Arterial injury
-
Access vessel thrombosis
-
Distal embolization
-
Worsening limb ischemia
-
Contrast induced nephropathy
-
Iatrogenic injury to nearby neurovascular structures
PREPROCEDURAL ASSESSMENT AND PLANNING
-
History, indications, and physical examination (Appendix 1 in Chap. 149 ). Document indications of the procedure, lower extremity pulses, and vital signs.
-
Evaluation of diagnostic imaging studies to determine the relevant vascular anatomy and assess the access site
-
Periprocedural management of coagulation status (Appendices 2 in Chap. 150 and 3 in Chap. 151 )
-
Antibiotic prophylaxis: Perioperative antibiotics are recommended [5] (Appendices 4 in Chap. 152 and 5 in Chap. 153 )
-
Imaging modality for guidance: Fluoroscopy; combined with ultrasound for arterial puncture
-
Positioning: Supine
-
Patient preparation:
-
Start intravenous fluids the night before angiography in order to ensure adequate hydration, combined with effective monitoring of fluid status
-
Insert a urinary catheter or ask the patient to void before the procedure depending on the estimated time of the procedure
-
Considerations for patients with specific diseases or conditions, patients on specific medications or patients with history of multiple comorbidities: consult with the referring clinician, and obtain subspecialty consultation as needed
-
PROCEDURE NOTE
-
Procedure: Endovascular Treatment of right/left popliteal aneurysm
-
Staff: [_]
-
Fellow: [_]
-
Resident: [_]
-
Clinical Information: Describe history and list indications
-
Allergies: No known drug allergy/Allergic to (specify)
-
Anesthesia: Local anesthesia/Monitored conscious sedation
-
Medications: List any relevant medications used
-
Contrast Material: (_) mL of [type] contrast material was used for intra-arterial injection
-
Field: Sterile
-
Procedure Classification: Clean
-
Position: Supine
-
Monitoring: Intravenous access was secured and vitals were continuously monitored by nursing staff/anesthesia team throughout the procedure
-
Total fluoroscopy time: (_) minutes
-
Cumulative radiation dose: (_) mGy
Description of Procedure:
The risks, benefits, alternatives, and the procedure itself were explained to the patient/patient’s Power of Attorney/legal guardian, and informed written consent was obtained. The site of the procedure was identified and marked. Time out was performed to confirm the correct patient, procedure, and site.
The groin area was prepped and draped in the usual sterile manner. After infiltrating the skin with 1 % Lidocaine, and using ultrasound guidance, the right/left common femoral artery was accessed retrogradely with a micropuncture kit and the position of the microwire was confirmed by fluoroscopy. A small nick in the skin was done using an 11 blade and the microsheath was exchanged with a (_)-French sheath over an exchange wire. A (_)-inch glidewire was advanced into the abdominal aorta. A (_)-French pigtail catheter/Omni flush catheter was advanced over the wire to the abdominal aorta and angiographic runs of the aorto-iliac and bilateral proximal femoral arteries were then performed. Next, a (_)-French [type] catheter was used to maneuver the glide wire into the contralateral common iliac artery down to the femoral artery and the catheter was advanced over it and parked in the distal external iliac artery. Selective contralateral lower extremity angiography was performed confirming the presence and location of the popliteal aneurysm. The glidewire was advanced to the level of the aneurysm and down to the tibio-peroneal trunk and was then exchanged with a (_)-French Bentson wire/stiff Glidewire/Amplatz wire over the catheter. Unfractionated heparin was infused to achieve a therapeutic ACT level and then the short (_)-French sheath was exchanged for a long (_) cm, (_)-French Flexor/Ansel Sheath with its tip parked in the distal superficial femoral artery.
Alternatively a small cutdown under local anesthesia was used to expose the proximal superficial femoral artery. The artery was punctured antegradely and a size 8–9 French sheath was introduced.
Another angiogram was done through the sheath allowing for measurement of the aneurysm dimensions. Over the stiff wire, a (_) mm diameter-(_) mm long Viabahn/Fluency covered stent was advanced and positioned across the aneurysm. The self-expanding stent was deployed allowing for a 2 cm landing zone. A follow up angiogram showed complete exclusion of the aneurysm with adequate runoff to the foot ( alternatively, if the measured length to be stented exceeds the length of one stent graft, another stent is placed with an overlap zone between stent grafts of at least 3 cm ). After obtaining all the necessary images, the procedure was concluded. The long sheath was exchanged for a short one. An ACT level was measured and then the sheath was pulled and manual compression held for 20 min/a [type] closure device was used to achieve adequate hemostasis. A dry compression dressing was applied. The patient had palpable pulses/Doppler signals over the pedal vessels.
The patient was then transferred to the recovery room in a stable condition. Staff was present for the entire procedure.
-
Intra-Procedure Findings: List all relevant radiologic findings.
-
Immediate Complications: None encountered during or directly after the procedure. List the complications if any.
Post-Procedure Plan [3]:
-
Keep patient complete bed rest with the right/left leg extended for (_) hours.
-
Check the puncture site for any bleeding or hematoma formation every 15 min for 1 h, then every 30 min for 4 h; inform interventional radiology team if any complications are observed.
-
Lower extremity neurovascular checks every hour.
-
Resume diet and previous orders as needed and if not otherwise contraindicated.
-
Continue adequate intravenous hydration and monitor fluid (intake-output) status.
-
Check complete blood count, creatinine and blood urea nitrogen on the day following the procedure or as clinically indicated.
Impression:
-
Endovascular treatment of left/right popliteal aneurysm as described above.
-
The patient tolerated the procedure well and left the interventional unit in a stable condition.
-
The patient was unstable and the procedure was canceled/terminated prematurely.
-
List any other relevant of important information/finding.
Abbreviations
- PAAs:
-
Popliteal Artery Aneurysms
References
Trinidad-Hernandez M, Ricotta JJ 2nd, Gloviczki P, Kalra M, Oderich GS, Duncan AA, et al. Results of elective and emergency endovascular repairs of popliteal artery aneurysms. J Vasc Surg. 2013;57(5):1299–305.
Garg K, Rockman CB, Kim BJ, Jacobowitz GR, Maldonado TS, Adelman MA, et al. Outcome of endovascular repair of popliteal artery aneurysm using the Viabahn Endoprosthesis. J Vasc Surg. 2012;55(6):1647–53.
Pulli R, Dorigo W, Fargion A, Pratesi G, Innocenti AA, Angiletta D, et al. Comparison of early and midterm results of open and endovascular treatment of popliteal artery aneurysms. Ann Vasc Surg. 2012;26(6):809–18.
Midy D, Berard X, Ferdani M, Alric P, Brizzi V, Ducasse E, et al. A retrospective multicenter study of endovascular treatment of popliteal artery aneurysm. J Vasc Surg. 2010;51(4):850–6.
Venkatesan AM, Kundu S, Sacks D, Wallace MJ, Wojak JC, Rose SC, et al. Practice guidelines for adult antibiotic prophylaxis during vascular and interventional radiology procedures. J Vasc Interv Radiol. 2010;21(11):1611–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Aboul Hosn, M. (2016). Endovascular Treatment of Popliteal Aneurysm. In: Taslakian, B., Al-Kutoubi, A., Hoballah, J. (eds) Procedural Dictations in Image-Guided Intervention. Springer, Cham. https://doi.org/10.1007/978-3-319-40845-3_124
Download citation
DOI: https://doi.org/10.1007/978-3-319-40845-3_124
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40843-9
Online ISBN: 978-3-319-40845-3
eBook Packages: MedicineMedicine (R0)