Abstract
In recent years, elastosonography (ES) has become an important application in the study of the musculotendinous apparatus [1–4]; in fact, this method permits both a qualitative and quantitative evaluation of the elasticity properties of soft tissues and its alteration in traumatic lesions and degenerative pathology. In the field of rheumatology, in particular, it adds a complementary diagnostic element to the standard imaging studies represented by ultrasound (US) and magnetic resonance imaging (MRI). ES can therefore be considered a tool which provides additional and important information regarding certain functional characteristics of musculotendinous tissues.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
In recent years, elastosonography (ES) has become an important application in the study of the musculotendinous apparatus [1–4]; in fact, this method permits both a qualitative and quantitative evaluation of the elasticity properties of soft tissues and its alteration in traumatic lesions and degenerative pathology. In the field of rheumatology, in particular, it adds a complementary diagnostic element to the standard imaging studies represented by ultrasound (US) and magnetic resonance imaging (MRI). ES can therefore be considered a tool which provides additional and important information regarding certain functional characteristics of musculotendinous tissues.
When pressure is applied to a tissue surface, the force of compression is transmitted to the underlying tissue, producing a change in the mechanical stress of the tissue which will vary based on the tissue consistency: less change in rigid tissue and more in elastic tissue.
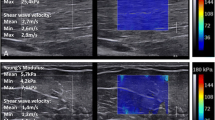
The elastosonographic methods, differentiated by modalities of force application to the tissue and modalities of measurement and visualization of the tissue response, are of two types: quantitative (shear wave imaging) and qualitative (strain imaging).
Shear wave ES evaluates the velocity of the transversal wave that is generated by the passage of the excitation wave, expressed as a number relative to the elasticity module.
Strain ES evaluates the deformation of the tissue along the propagation axis of the beam by means of analysis of the RF signal along each line of scanning, with a color-coded representation of the information where, by convention, red corresponds to elastic tissue, green to moderately elastic tissue, and blue to rigid tissue.
Both methods are used for the study of musculotendinous structures, though strain ES allows for a more immediate evaluation and better adapts itself to the structures in the region of interest.
In fact, it’s a peculiarity that muscles and tendons have elastographic characteristics which differ not only from region to region but also based on the resting state or tension and/or contraction. Therefore, an elastographic study of musculotendinous structures is always a dynamic-type study.
Furthermore, it’s important to be familiar with the elastographic aspect of normal muscular and tendon structures, both in the static and dynamic phases, in order to recognize the variations caused by different pathological conditions.
Strain ES is performed with dedicated equipment using a linear transducer with which manual compressions and relaxations are applied in a vertical direction with a homogeneous and regular force which is quantified by an indicator on the screen.
Visualization of the tissue under examination occurs in real time using a double window on the monitor, which allows evaluation of the aspect both in basal condition and during elastosonography, with scans done parallel and perpendicular to the long axis of the tissue. The results are shown in a chromatic scale where blue represents maximum rigidity and red the maximum elasticity, passing through intermediate values going from light blue to green to yellow. This chromatic box, partially transparent, is superimposed on the basal ultrasound image, with the possibility to sample in regions of interest (ROI) the values of the ratio between pathological tissue and healthy tissue, adding therefore a quantitative evaluation to the exam.
Some authors use a “spacer” between the transducer and the skin to make the pressure exerted on the tissues more homogeneous and regular and also to reduce artifacts, especially in anatomical regions with irregular surfaces [3, 5].
Each tissue has, in normal conditions, mechanical properties and therefore a characteristic elasticity coefficient, which can undergo change in pathological conditions.
ES can be indicated when the ultrasound study is inconclusive, highlighting different elasticity between healthy and pathological tissue, especially when confronted with pain symptom when the ultrasound exam does not find any significant morphostructural tissue changes.
Healthy tissue and pathological tissue can, in fact, have the same echogenicity; it is this lack of tissue contrast that doesn’t permit the recognition of alterations in certain pathological conditions [2, 6].
In the musculoskeletal field, the preliminary results in the study of tendinopathy and muscle disorders are encouraging [4].
Tendinopathies are frequent in athletes, but they are not easily treatable due to their multifactor etiology [7].
The alterations that tendons undergo, regarding both clinical findings, constituting thickening, and anatomopathological findings, are well known [8].
Continuous microtrauma, overload, and vascular alterations cause tissue damage which has repercussions on the elasticity of the fibrillary architecture [3].
ES has been used in some work groups to compare the behavior of healthy tendons with pathological ones in the rotator cuff, the elbow [9], and the Achilles tendon [8, 10, 11], with satisfying results in comparison to basal ultrasound.
Some authors have demonstrated that ES has detected alterations of the elastosonographic characteristics of tendons both in symptomatic and asymptomatic patients [10, 11]; this finding implies that this new method, combined with basal ultrasound, can increase the diagnostic accuracy given that it can detect alterations very early.
Healthy tendons and, in particular, the Achilles tendon, which is easy to study because of its size and location, have an elastosonographic pattern which is prevalently blue, expression of a certain rigidity and scarce deformability [10, 11].
In geriatric patients, however, the Achilles tendon has a prevalently green color with traces of blue, while when it’s the site of tendinopathy, the color is predominately red due to the reduced consistency [4].
The supraspinatus tendon, according to the same author, has an analogous chromatic pattern in the same clinical conditions.
This finding has been confirmed by other authors who compared elastosonographic findings with those of magnetic resonance imaging which is the gold standard, highlighting a good sensitivity of ES [12].
ES has been used in the diagnosis of fatty degeneration of the rotator cuff with similar results also in this case with magnetic resonance imaging [12], demonstrating a reduced elasticity of the tendons in atrophy and providing useful information regarding prognosis and treatment.
Interesting applications have emerged in the study of synovial pathology where some authors were able to differentiate inflammatory synovial pathology from infectious synovial pathology, demonstrating a reduction in elasticity with predominant red color in areas with inflammatory disease in comparison to infectious complications, which present as areas of greater consistency with a green color [4].
An area of great interest is that of ES in the study of muscle tissue in different pathological conditions such as inflammation, trauma, and the rarer congenital dystrophies [13, 14].
Normal muscle tissue presents a chromatic pattern which is prevalently green. In this field, the exam of choice is magnetic resonance imaging, but the agreement that some authors have found between this method and ES could, in the future, lead to the substitution of MRI with ES due to MRI’s limitations of claustrophobia, pacemakers, surgical clips, and higher cost [15].
In our study we used ES in muscle lesions following direct and indirect trauma, at a time interval of up to 6 months after the trauma, to allow for healing time in widespread lesions.
The criteria of inclusion are the traumatic event and pain.
We compared findings of basal ultrasound exam, ES, clinical examination, and MRI, which is considered the gold standard [16].
ES was able to demonstrate persistence of alterations even when basal ultrasound became normalized and allowed to correctly interpret the dynamics of tissue repair and eventual complications in the follow-up leading to the potential of the method to indicate the correct therapy or to modify the therapy enacted in order not to risk further damage.
The use of ES has also been extended to the study of space-occupying lesions of the skeletal muscle system in an attempt to characterize the tissue: confronted with the poor attendibility of the quantitative elastographic findings, the qualitative findings, expressed as a color-coded map, are useful in differentiating benign forms from malignant forms [17].
Preliminary studies of angiomatous lesions and of neurofibromatosis have shown an ES color pattern which is predominantly red for angiomas due to their soft consistency and predominantly green for neurofibromas due to their more rigid tissue structure [4].
ES has also been evaluated for carpal tunnel syndrome: the elasticity of the median nerve is decreased in pathological conditions with a blue chromatic pattern [18, 19].
ES has some limits; mainly it is operator dependent and therefore difficult to reproduce the findings; regarding this, it is indispensable to pay attention to the indicative scales on the screen during pressure application to the tissues during the examination.
At present, the imaging of the mechanical properties and of the elasticity of the tissues has arrived at a high technical level of development to make it clinically useful [20–22].
However, large-scale studies are necessary to define the indications and the role of the method in the diagnostic work-up of musculotendinous pathology, either as an exam associated with the basal ultrasound exam or as a substitute for less comfortable and more costly exams.
1 Image Gallery
(a) Grayscale axial scan (left) of the anterior rectus femoris shows a normal muscle aspect; at sonoelastography (right), an altered intrinsic elasticity with intramuscular stiffer areas (blue dot arrow) mixed with softer ones (red dot arrow) in patient with anterior thigh pain without trauma. (b) Contralateral healthy side. (c) MRI: SET2W and fat suppression images show a normal muscle aspect
(a) Grayscale axial images of the semimenbranosus and semitendinosus muscle (right): a post-traumatic intramuscular hyperechoic longitudinal area and corresponding elastogram (left) in neutral thigh position. The presence of a red oblique area between the muscles means a partial fluid collection. (b) Axial T2 W: fluid collection well defined with MRI
(a) Grayscale axial image (left): partial quadriceps muscular rupture 10 days after trauma which appears like a hypo-anechoic round area; on the right a very soft aspect of the hemorrhage. (b) The contrast-enhanced US (CEUS) evidences the muscular lesion like a black round area without vascularization. (c) The lesion after 1 month appears stiff (green/blue) at sonoelastography due to the reparative process
(a, b) Grayscale axial (a) and longitudinal (b) images of the rectus femoris muscle (left): a post-traumatic intramuscular anechoic interfascial area. The corresponding elastogram (right) in neutral thigh position shows a red soft area that means a fluid interfascial collection and a soft aspect of the muscle because of the hemorrhage. (c) The MRI axial T2 fat suppression image confirms the interfascial liquid and the intramuscular hemorrhage
(a, b) Grayscale longitudinal (a) and axial (b) scan of fluid homogeneous post-traumatic subcutaneous collection in the anterior tibial region on the left. At the sonoelastography (right), the collection appears as a typical red-green-blue aspect, like a cyst lesion. (c, d) Coronal T2FS (c) and axial T2 (d) view confirm the fluid collection
(a) Grayscale longitudinal image of the normal anterior tibial tendon (right) and corresponding elastogram (left) in neutral ankle position. The tendons appear homogeneously stiff (green-yellow), with no distinct soft (red) areas. (b) Grayscale longitudinal image of the normal Achilles tendon (left) and corresponding elastogram (right) in extension position. The tendons appear homogeneously stiff (green/blue)
Grayscale longitudinal image of the anterior tibial tendon (right) and corresponding elastogram (left) in neutral ankle position. Clinically the patient had difficulty to dorsiflexion. The tendon appears enlarged and inhomogeneous in grayscale with a prevalence of blue and green area with few red spots in superficial portion during the elastography: soft area alternating with areas of low elasticity which demonstrate small partial-thickness tear in tendinosis
(a) Grayscale sonographic image reveals swelling and intratendinous hypoechogenicity in common extensor tendon origin in patient with lateral elbow pain. (b) Color Doppler sonographic image shows increased vascularity epicondylitis. (c) MRI T2 FS coronal view shows a hyperintensity area in the proximal insertion of the common extensor tendon. (d) The elastosonography reveals a diffuse red-coded area in symptomatic common extensor tendon
(a) Longitudinal grayscale of the patellar tendon: the tendon appears thick and inhomogeneous with a small calcification in the proximal deep portion. (b) At the elastosonography the tendon reveals homogeneous increased elasticity in case of tendinopathy. (c) MRI sagittal view T2FSW (d) and T1SEW (c) images shows high signal intensity at the enthesis due to tendinosis
(a, b) Grayscale longitudinal plane of the plantar fascial (a) and color (b). The plantar fascia appears ticked and hypoechoic in the insertion, in the intermediate and distal portion without spots of color. (c) Sonoelastography evidences focused softening of the plantar fascia in the intermediate region
Flexor tendons tenosynovitis in pregnant woman who had onset of pain. (a) US power axial scan of flexor tendons in the volar region of the hand: an evident anechoic area is visualized around the tendons which are increased in size as a result of edematous changes. (b) The anechoic area appears at elastosonography very soft and means an abundant effusion in the sheath
Pigmented villonodular synovitis (PVNS). (a) Real-time sonoelastography view (right) and B mode image (left) in 74-year-old patient with pain and swelling of the wrist. Hypertrophied synovium shows predominant firm to soft nature, which is represented by predominant red color with patchy blue areas: (b) MRI gradient echo in sagittal plane confirms a heterogeneous synovial mass with decreased signal intensity caused by hemosiderin
(a, b) US grayscale longitudinal view (a) and axial view (b) show a heterogeneous mass next to the bone in tibial fracture in patient with pain and fever. (c) At elastosonography the lesion appears almost completely blue with a small superficial component of high elasticity: the lesion was a localized collection of pus and inflammation
Lymphangioma. (a) Grayscale (left) shows in the groin an oval-shaped mass anechoic between the fascia and subcutaneous tissue; at elastosonography (right), the lesion shows a cyst-like aspect (red-green-blue). (b) The mass evidences at CEUS a rich vascularization because of a lot of white spots inside. (c, d) MRI on axial SET1 and SET2W shows a liquid multiloculated mass with thin septa inside
Lipoma. Grayscale longitudinal images (left) of a little elliptical subcutaneous mass parallel to the skin surface hyperechoic relative to the adjacent muscle which contains linear echogenic lines; at elastography (right), the subcutaneous lipomas have a typical horizontally oriented striated pattern which is characterized as tricolor (blue, green-yellow, and red)
Sebaceous cyst. B mode image (left) in longitudinal scan of subcutaneous mass, hypo-anechoic, inhomogeneous, with sharp margins and enhanced through-transmission deep to the lesion with refractive shadowing at the edges; real-time sonoelastography (right) shows a stiff and moderate elasticity in the mass due to different content of the cyst
Myxoid liposarcoma. (a) Longitudinal grayscale and color show an oval hypoechoic mass with regular edges and with some vessels inside. (b) The lesion studied with CEUS evidences a rich heterogeneous vascularization. (c) At sonoelastography in longitudinal view, the mass appears almost completely stiff. (d) MRI SET1 coronal plane image after intravenous gadolinium administration shows nonenhancing tissue central with peripheral enhancement. (e) MRI SET2 axial plane image shows a hyperintense lesion
Dermatofibrosarcoma protuberans (DFSP). (a) US color shows a huge hypoechoic hynomogeneous mass in the anterior region of the thigh with some vessels inside. (b) At CEUS the mass appears completely full of vessels. (c) The biopsy procedure. (d) At elastosonography the lesion appears very stiff in the half deep portion and with high elasticity in the other superficial part
Neuroendocrine carcinoma. (a) Grayscale axial view (left) shows a homogeneous hypoechoic mass in the groin which at elastosonography (right) evidences a moderate elasticity with a layer of low elasticity in superficial region. (b) At CEUS the lesion shows some vessel in the middle region. (c) MRI T1W axial image shows low enhancement of the lesion. (d) MRI T2 fat suppression shows inhomogeneous high signal
Giant cell tumor of tendon sheath (nodular tenosynovitis) in woman with a slightly painful finger mass. (a) Grayscale longitudinal view of the volar region of the hand shows a lobulated and well-defined, hypoechoic lesion around the tendon. (b) Corresponding elastosonography shows the lesion as a mosaic of various levels of stiffness over the normal tendon which is blue
(a, b) Grayscale axial (a) and longitudinal (b) view of the median nerve at the proximal carpal tunnel level evidences the enlargement of the median nerve cross-sectional area. The nerve is hypoechoic with a reduced fascicular pattern. (c, d) At sonoelastography in axial (c) and longitudinal view (d), the nerve appears significantly stiffer in patients with carpal tunnel syndrome
References
Varghese T, et al. Tradeoffs in elastographic imaging. Ultrason Imaging. 2001;23(4):216–48.
Frey H. Realtime elastography: a new ultrasound procedure for the reconstruction of tissue elasticity. Radiologe. 2003;43(10):850–5.
Klauser AS, et al. Sonoelastography: musculoskeletal applications. Radiology. 2014;272(3):622–33.
Lalitha P, et al. Musculoskeletal applications of elastography: a pictorial essay of our initial experience. Korean J Radiol. 2011;12(3):365–75.
Kjaer S, et al. EULAR 2011. London.
Niitsu M, et al. Muscle hardness measurement by using ultrasound elastography: a feasibility study. Acta Radiol. 2011;52:99–105.
Kannus P, Natri A. Etiology and pathophysiology of tendon ruptures in sports. Scand J Med Sci Sports. 1997;7(2):107–12.
Sconfienza LM, et al. Sonoelastography in the evaluation of painful Achilles tendon in amateur athletes. Clin Exp Rheumatol. 2010;28(3):373–8.
De Zordo T, et al. Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. AJR Am J Roentgenol. 2009;193(1):180–5.
De Zordo T, et al. Real-time sonoelastography: findings in patients with symptomatic achilles tendons and comparison to healthy volunteers. Ultraschall Med. 2010;31(4):394–400.
De Zordo T, et al. Real-time sonoelastography findings in healthy Achilles tendons. AJR Am J Roentgenol. 2009;193(2):W134–8.
Schreiber V, et al. Real-time sonoelastography in rotator cuff imaging and comparison to magnetic resonance imaging as gold standard. RSNA. 2009.
Drakonaki EE, Allen GM. Magnetic resonance imaging, ultrasound and real-time ultrasound elastography of the thigh muscles in congenital muscle dystrophy. Skeletal Radiol. 2010;39(4):391–6.
Monetti G, Minafra P. Elastosonography in the evaluation of the post-traumatic muscular pathology Musculoskeletal Ultrasound Society Meeting, Paris. 2007.
Adler RS, Garofalo G. Ultrasound in the evaluation of the inflammatory myopathies. Curr Rheumatol Rep. 2009;11(4):302–8.
De Marchi A, et al. EUROSON 2012. Madrid. 2012.
Park SK, et al. Diagnostic performance of ultrasound elastography in the evaluation of benign and malignant soft tissue tumors. RSNA. 2013.
Miyamoto H, et al. Carpal tunnel syndrome: diagnosis by means of median nerve elasticity- improved diagnostic accuracy of US with sonoelastography. Radiology. 2014;270:481–6.
Orman G, et al. Ultrasound elastographic evaluation in the diagnosis of tunnel carpal syndrome: initial findings ultrasound. Med Biol. 2013;39:1184–9.
Wells PN, Liang HD. Medical ultrasound: imaging of soft tissue strain and elasticity. J R Soc Interface. 2011;8(64):1521–49.
Brandenburg JE, et al. Ultrasound elastography: the new frontier in direct measurement of muscle stiffness. Arch Phys Med Rehabil. 2014;95(11):2207–19.
Eby SF, et al. Validation of shear wave elastography in skeletal muscle. J Biomech. 2013;46(14):2381–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Cammarota, T., De Marchi, A., Pozza, S. (2017). Musculoskeletal. In: Clevert, DA., D'Onofrio, M., Quaia, E. (eds) Atlas of Elastosonography. Springer, Cham. https://doi.org/10.1007/978-3-319-44201-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-44201-3_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-44199-3
Online ISBN: 978-3-319-44201-3
eBook Packages: MedicineMedicine (R0)