Abstract
Human papillomaviruses (HPVs) are a necessary cause of anogenital squamous cell carcinomas (SCC) and a subgroup of head and neck SCC, i.e., those originating in the oropharynx. The key events in high-risk HPV (HRHPV)-associated neoplastic progression include persistent infection, deregulated expression of virus early genes in basal epithelial cells, local immune suppression and the accumulation of chromosomal alterations. Evidence for these events particularly comes from studies of uterine cervical carcinogenesis; primary premalignant HRHPV-positive lesions of the head and neck mucosa are seldomly detected. Integration of virus DNA into host chromosomes is considered an important driver of carcinogenesis and observed in 40 up to 90 % of uterine cervical SCC (UCSCC) and oropharyngeal SCC (OPSCC), dependent on the integration detection method used and HRHPV type. In OPSCC, > 90 % HPV-positive tumors are infected with HPV16. Ten up to 60 % of HPV-positive tumors thus contain extrachromosomal (episomal) virus. In this chapter, causes and consequences of HPV integration are summarized from the literature, with special focus on the site of HPV integration in the cellular genome, and its effect on expression of viral oncogenes (particularly E6 and E7), on human (tumor) gene expression and on deregulation of cell proliferation, apoptosis and cell signaling pathways. Also data on DNA methylation, viral load and clinical outcome in relation to HPV integration are provided.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Human papillomavirus
- HPV
- Head and neck squamous cell carcinoma (HNSCC)
- Oropharyngeal carcinoma
- Tonsillar carcinoma
- Viral integration
- E2
- E6
- E7
- FISH
- PCR
- NGS
- Tumor genes
1 Human Papillomaviruses and Their Life Cycle
Human papillomaviruses (HPVs) are non-enveloped viruses, containing circular double-stranded DNA of approximately 8 kb. They are highly epitheliotropic and can infect both mucosal and cutaneous epithelia. The HPV family is classified into 5 genera and subdivided into 31 species and 120 types (zur Hausen 2002; Bernard et al. 2010). Each type is defined as a complete papillomavirus genome, whose L(ate) 1 gene nucleotide sequence is at least 10 % different from that of any other known type. I will focus here on the mucosal HPV types. Fifteen HPV types belonging to the α genus are linked to the development of malignant epithelial lesions, i.e., the so-called high-risk (HR) HPVs, including HPV16 and HPV18 which are found in ~50 % and ~20 % of uterine cervical malignancies, respectively (WHO IARC Monographs 2007). HPV16 is also the predominant type in oropharyngeal carcinomas (OPSCC) (Olthof et al. 2012). Differences in the capacity to deregulate cellular protein function by viral oncogenes E6 and E7 account for the carcinogenic properties of HRHPV in comparison with low-risk (LR) HPVs. LRHPV types, such as HPV6 and HPV11, are often found in benign mucosal lesions (e.g., anogenital and laryngeal papillomas) and are only sporadically associated with carcinomas (Olthof et al. 2012; Huebbers et al. 2013; Mooren et al. 2014).
To date, most information on the initiation of HPV-associated mucosal disease comes from studies on uterine cervical carcinogenesis, because patients with head and neck lesions containing HRHPV usually present with advanced disease and only seldomly with primary premalignant lesions (Mooren et al. 2014). The following events are more or less generally accepted to occur during the HPV life cycle (for reviews, see zur Hausen 2002; Woodman et al. 2007; Olthof et al. 2012, Groves and Coleman 2015 and references therein) (Fig. 1a):
-
(1)
HPV tends to target the multilayered keratinocyte layers of the epidermis for infection and reproduction. In particular, the virus prefers to target functional epithelial appendages, such as hair follicles, several glands including salivary glands in the oral cavity and tonsillar crypts, as well as sites where stratified epithelium abuts columnar epithelium, such as in the uterine cervical transformation zone. These vulnerable sites lack the highly structured barrier function of the epithelium and have the heighted presence of epithelial reserve cells/stem cells (Egawa et al. 2015).
-
(2)
HPV infects the basal cell layer of stratified epithelia via epithelial wounding/microlesions.
-
(3)
Viral entry of cells requires active cell division and studies with HPV16 suggest that the L1 capsid protein binds to heparan sulfate proteoglycans (HSPGs) on segments of the basement membrane, which are exposed at sites of (micro)injury. Furthermore, the virion binds to α6 integrins, which initiate further intracellular signaling events. Binding to HSPGs induces conformational changes, L2 cleavage and binding of the exposed L2 N terminus to a newly identified L2-specific receptor, the annexin A2 heterotetramer. Subsequently, clathrin-, caveolin-, lipid raft-, flotillin-, cholesterol- and dynamin-independent endocytosis of HPV16 occurs (Schiller et al. 2010; Raff et al. 2013).
-
(4)
Infection is associated with HPV early gene E1 and E2 expression and low-level amplification of the HPV episome (circular, extrachromosomal DNA). E2 furthermore binds to mitotic spindles enabling viral DNA partitioning during cell division (Van Tine et al. 2004a).
-
(5)
Infected cells replicate and move into parabasal epithelial layers. E6 and E7 expression suppress differentiation and promote re-entering the cell cycle.
-
(6)
Infected cells move to the upper epithelial layers, replicate their viral genome to high copy number and express E4 and the late genes L1 and L2 allowing encapsulation of episomes into infectious virus particles and shedding from the cornified surface. Recognizable lesions that are going through these usually non-neoplastic productive HPV infections are classified as low-grade intraepithelial lesion (LSIL) or cervical intraepithelial neoplasia 1 (CIN1). These lesions often regress due to the action of the immune system.
-
(7)
In ~5 % of cases, infections may become persistent (lesions classified as high-grade SIL, or CIN 2/3) leading to local immune suppression, accumulation of chromosome alterations in the infected host cells (Southern et al. 2001; Hopman et al. 2004, 2006), deregulated expression of HPV early genes and consequently reduced virus production. 0.3–1.2 % of initial infections will eventually progress to invasive cancer (WHO 2014).
a Schematic overview of HPV infection and integration during the development of HPV-positive tumors (modified from Woodman et al. 2007; Cornet et al. 2015). HPV is thought to access the basal cells through micro lesions in the squamous cell epithelium. Following infection, the early HPV genes E1, E2, E4, E5, E6 and E7 are expressed and the viral DNA replicates from episomal DNA. In the upper layers of the epithelium, the viral genome is replicated further, and the late genes L1 and L2, and E4 are expressed. L1 and L2 allow encapsulation of the viral genomes to form progeny virions in the nucleus. The shed virus can then initiate a new infection. In the transition to (micro)invasive cancer, viral DNA often integrates in 1 or more copies into the host genomic DNA, with often associated loss or disruption of E2, and subsequent upregulation of E6 and E7 oncogene expression. LCR, long control region. b The subsequent upregulation of E6 and E7 oncoproteins results in deregulation of cell signaling pathways, which, among others, leads to increased cellular proliferation and inhibition of apoptosis (modified from Olthof et al. 2012; Groves and Coleman 2015). c Multiple mechanisms by which HPV integration into the host genome may directly lead to deregulation of the key cellular tumor suppressor genes and proto-oncogenes (modified from Rusan et al. 2015)
2 Mechanisms Involved in and Approaches to Detect HPV Integration
Persistent infection may also result in integration of the HRHPV genome or parts thereof into the host genome. Although in premalignant CIN lesions the time and frequency of integration has been heavily debated, it is now believed that it occurs relatively late in the progression of high-grade dysplasia to (micro)invasive anogenital carcinomas (Klaes et al. 1999; Hopman et al. 2004; Vinokurova et al. 2008; Rusan et al. 2015). HPV16 integration could also be detected in OPSCC and in tumor adjacent dysplasia in some of these cases (Hafkamp et al. 2003; Mooren et al. 2014). So far, in situ localization of a persistent HRHPV infection in the oropharynx/palatine tonsils has been extremely difficult to find and detect in the normal population (Klingenberg et al. 2010), and analysis of tissue biopsies of a population with a high chance of HPV infection (e.g., people having many sex partners, oral sex or who are immunosuppressed) is probably required to successfully identify such infections. In contrast, LRHPV infections are easy to detect, for example in laryngeal papillomas, but in these cases viral integration is a seldom finding (Huebbers et al. 2013; Mooren et al. 2014).
Because viral integration requires the breakage of both the viral and the host DNA, the integration rate is believed to be linked to the levels of DNA damage (Chen et al. 2014). DNA damage can be caused by both endogenous and exogenous factors, including inflammation induced either by the virus itself (E6 and E7 expression) or by co-infections with other agents (both resulting in production of excessive amounts of reactive oxygen and nitrate species), environmental agents and other factors (Wei et al. 2009; Lace et al. 2015; Visalli et al. 2016). In this respect, the activation of DNA damage repair mechanisms as well as the accumulation of chromosomal alterations may also contribute to the viral integration process (Southern et al. 2001; Hopman et al. 2004, 2006).
In uterine cervical squamous cell carcinomas (UCSCC), which are HPV positive in 95–100 % of cases, different HRHPV types tend to integrate at different frequencies, such as HPV16 at 50–80 %, HPV18 at >90 %, HPV31 and −33 at 15–40 % and HPV45 at > 80 % (Wentsenzen et al. 2004; Vinokurova et al. 2008; Olthof et al. 2012; Groves and Coleman 2015). In OPSCC HPV, positivity range from 20 to 90 % in different studies and depend among others on the geographical location, sample preparation and detection methods used (Olthof et al. 2012). 90–95 % of virus-positive OPSCC are infected with HPV16, and integration percentages range between 40 and 80 % dependent on the methods used to identify integrated HPV.
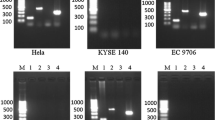
Along with the many HPV detection methods available to date (Snijders et al. 2010), a number of approaches have been developed to specifically detect integrated HPV. On the one hand, approaches have been designed to only identify integration events that are transcriptionally active detecting virus–host fusion transcripts, such as RNA in situ hybridization (ISH) (Van Tine et al. 2004b), 3′ RACE–PCR [also known as “Amplification of Papillomavirus Oncogene Transcripts” (APOT) PCR] (Klaes et al. 1999; Lace et al. 2011; Olthof et al. 2014, 2015; Vojtechova et al. 2016) and RNASeq (Akagi et al. 2014; Ojesina et al. 2014; Parfenov et al. 2014; Hu et al. 2015). On the other hand, procedures have been used to detect integrated HPV genomes (regardless of their transcriptional activity), including DNA (F)ISH (Cooper et al. 1991; Hopman et al. 2004; Hafkamp et al. 2008), Southern blotting (Cullen et al. 1991; Cooper et al. 1991; Vojtechova et al. 2016), detection of integrated papillomavirus sequences (DIPS) PCR (Luft et al. 2001; Peter et al. 2010; Huebbers et al. 2013; Li et al. 2013; Olthof et al. 2014, 2015), restriction-site PCR (Thorland et al. 2000), quantitative PCR (Peitsaro et al. 2002; Nagao et al. 2002; Ziegert et al. 2003) and DNASeq (Xu et al. 2013; Akagi et al. 2014; Parfenov et al. 2014, Chandrani et al. 2015; Hu et al. 2015). These analyses have contributed significantly to our current knowledge on the frequency of HPV integration in UCSCC and OPSCC and its impact on cancer development and progression as well as on viral (onco)gene and human gene expression. However, all these assays also have their (dis)advantages and differ in their detection sensitivities, which have to be taken into account when comparing reported data and generating general conclusions on these issues (below).
3 Identification of HPV Integration Sites in the Human Genome
Identification of sites in the human cellular genome where HPV integration events occur is a longstanding field of interest in HPV research. Molecular studies have provided evidence that often 1 and sometimes >1 integration site(s) can be detected in UCSCC and OPSCC (Hopman et al. 2004; Hafkamp et al. 2008; Peter et al. 2010; Mooren et al. 2013; Akagi et al. 2014; Ojesina et al. 2014; Parfenov et al. 2014; Hu et al. 2015). HPV integration sites appear to be distributed all over the human genome in both UCSCC and OPSCC, and lie often within, or close to, fragile sites (Wentsenzen et al. 2004; Akagi et al. 2014; Ojesina et al. 2014; Olthof et al. 2014, 2015; Parfenov et al. 2014; Hu et al. 2015). Furthermore, a number of cytogenetic bands have been identified as integration hotspots, including 3q28, 4q13.3, 8q24.21, 13q22.1 and 17q21.2 accounting for integration sites of >20 % of UCSCC analyzed (Schmitz et al. 2012; Olthof et al. 2014; Chandrani et al. 2015). In addition, Parfenov et al. (2014) and Hu et al. (2015) reported that integration in both UCSCC and OPSCC is often in regions of microhomology (1–10 bp) among the viral and host genome, indicating that fusion between viral and human DNA may have occurred by microhomology-mediated DNA repair pathways. Most frequently integration is detected into genic regions and to a lesser extent in miRNA regions. Parfenov et al. (2014) reported that in 54 % of OPSCC HPV integrated into a known gene (e.g., RAD51B), and in 17 % within 20 kb of a gene. Similarly, Olthof et al. identified in 29 OPSCC 37 HPV16 integration sites, 27 of which were in known or predicted genes, including 17 with a known role in tumorigenesis, such as BCL2, FANCC, HDAC2 and TP63. Hu et al. (2015) reported integration hot spots (range 4.9–9.7 %) in POU5F1B, FHIT, KLF12, KLF5, LRP1B, LEPREL1, HMGA2, DLG2 and SEMA3D, whereas Ojesina et al. (2014) found virus breakpoints in MYC, ERBB2, TP63, FANCC, RAD51B and CEACAM5, both in UCSCC. Also in 7 often used HPV16-positive HNSCC cell lines 2–7 integration sites per nucleus were identified, with integration in genes (DIAPH2, TP63, C9orf156) and intergenic regions (Olthof et al. 2014). Akagi et al. (2014) were able to confirm these observations in cell lines as well as primary tumor specimens and, moreover, found that sites of integration cluster near sites of structural alterations (amplifications, deletions) in the genome. These findings have also been described previously for UCSCC (Lockwood et al. 2007; Peter et al. 2010; Ojesina et al. 2014). As a result, Akagi et al. (2014) proposed a viral genome looping model to explain HPV-driven amplifications and rearrangements that occur at sites of integration, which may be further propagated throughout the genome. It consists of the following steps: (1) host genome and viral episome are nicked, (2) linear HPV genome integrates in cellular genome, (3) circular DNA containing both host and viral sequences is formed, (4) this template is amplified by rolling circle amplification and (5) integrated concatemers of viral–host sequences are generated that might spread further in the genome. Indeed, in the HPV16-positive HNSCC cell lines described by Olthof et al. (2015), FISH experiments provided evidence for multiplication and translocation events of chromosomes harboring integrated viral DNA sequences as well as genomic instability. It should be noted, however, that the looping model is particularly based on analysis of tumor cell lines, which might also have accumulate additional chromosomal alterations induced by long-term cultivation. It would be interesting to compare the used cell lines with early passages and the primary tumor tissue to examine this in more detail.
Taken together, these data suggest that HPV integration is not simply a random event, but rather has a preference for less protected and more accessible chromosomal regions such as transcribed tumor genes and fragile sites. It will be interesting to further explore (1) whether integration takes place in genes, which are highly expressed during carcinogenesis or (2) whether integration itself is rather random but may affect the expression of interrupted genes or (3) whether both may occur simultaneously. In this respect, Kraus Christiansen et al. (2015) recently reported that integration sites seem to coincide with DNA that is transcriptionally active in mucosal epithelium, as judged after relating data of integration sites to DNase hypersensitivity and H3K4me3 methylation. These results might point to integration being rather an early event in carcinogenesis than a late product of chromosomal instability, which is in agreement with data of Hopman et al. (2006) showing that integration already can occur in diploid CIN lesions.
4 Consequences of Viral Integration: Viral Gene Expression
In vitro studies have suggested that HPV integration events occur in cells that also contain non-integrated episomes resulting in repression of integrant-derived transcription of E6 and E7 by expression of the E2 transcriptional regulator from the episome (Bechtold et al. 2003; Pett et al. 2006; Groves and Coleman 2015). Only after episome clearance, for example by a host anti-virus response (Herdman et al. 2006), an upregulated expression of E6 and E7 oncoproteins from the integrated viral DNA might be detected, which leads to a selective growth advantage over cells harboring episomal DNA (Jeon and Lambert 1995). There is, however, discussion on the height of the E6 and E7 expression levels and how they are exactly regulated in HPV-positive lesions. The general view is that viral DNA often integrates in 1 or more copies into the host genomic DNA (see above). During this process, the viral episome is most often opened within the E2 open reading frame (preferential site of integration), frequently leading to deletion of E4 and E5 and part of E2 and L2 (zur Hausen 2002; Wentsenzen et al. 2004; Olthof et al. 2012). Olthof et al. and Parfenov et al. (2014) also detected disruption of the viral episome in the E1 gene, which also leads to E2 loss. The subsequent upregulation of E6 and E7 oncoproteins results in deregulation of cell signaling pathways, which, among others, leads to increased cellular proliferation and inhibition of apoptosis and finally to a transformed cell state (zur Hausen 2002; Ganguly and Parihar 2009; Moody and Laimins 2010; Pim and Banks 2010; Olthof et al. 2012) (Fig. 1b). Transformation is continuously dependent upon E6/E7 expression and can be reversed by the reintroduction of E2 (Adams et al. 2014) or by downregulation of E6/E7 using short-hairpin RNAs (Rampias et al. 2009). HPV breakpoints have also been mapped outside the E2 and E1 open reading frame (Akagi et al. 2014; Hu et al. 2015), most frequently in the L1 and L2 genes. In these cases, however, methylation of the E2-binding sites in the LCR promotor, preventing E2 to bind to the LCR promotor, might be responsible for de-repression of E6 and E7 expression (Reuschenbach et al. 2015). This might also be the case in tumors that harbor multiple copies of the HPV genome in stretches or concatenates in the human genome (Olthof et al. 2014; Groves and Coleman 2015). Another possibility might be that viral gene expression is influenced by nearby cellular regulatory sequences (Rusan et al. 2015).
In contrast to this view, a study in primary keratinocytes immortalized with HPV16 genomes has shown that disruption of the E2 gene sequence upon viral integration does not result in increased expression of the viral E6 and E7 oncogenes (Lace et al. 2011). In addition, a publication by Häfner et al. (2008) using APOT-PCR has shown no correlation between the integration state of the viral genome and the expression of the viral gene E6 in a collection of 55 HPV16-positive UCSCC samples. Recently, Olthof et al. (2014, 2015) have provided evidence that also in 7 HPV-positive HNSCC cell lines as well as in 75 primary OPSCC HPV physical status (extrachromosomal episomes or host DNA integrated) does not affect the levels of viral E2, E6 and E7 gene transcripts. Therefore, constitutive rather than a high-level expression of viral oncogene transcripts appears to be required in HPV-related OPSCC, enough to ensure the viral oncogenes to consistently deregulate cellular proteins and cell signaling pathways, including cell proliferation (pRb pathway), apoptosis and DNA damage response (p53 pathway) (Wiest et al. 2002; zur Hausen 2002; Hafkamp et al. 2009; Leemans et al. 2011; Pim and Banks 2010; Rieckmann et al. 2013; Arenz et al. 2014) (Fig. 1b).
5 Consequences of Viral Integration: Human Gene Expression
Besides its promotion of stable viral gene expression and subsequent deregulation of cell signaling pathways, HPV integration may also confer a selective growth advantage to the host cells through a direct effect on the host genome (i.e., by affecting the key cellular genes). Olthof et al. (2014) had mRNA expression profiling data of 6 OPSCC with proven HPV16 integration in gene sequences, including the known tumor-related genes FANCC, HDAC2, SYNPO2 and TRAF3. Viral integration, however, did not lead to significantly different expression of the interrupted gene in comparison with OPSCC having integration in another DNA sequence or showing solely viral episomes. This is in contrast to a study of Huebbers et al. (2013) showing that integration of low-risk HPV6 in the AKR1C3 gene resulted in loss of gene expression in a laryngeal carcinoma. In this case, however, the other gene copy was lost in the tumor as shown by array CGH analyses. In the 6 OPSCC studied by Olthof et al. (2014), no loss or amplification of the chromosomal regions containing the virally interrupted genes has been detected by array CGH, indicating that one or more expressed gene copies are still present in these tumors, which can mask a possible effect of the integration on gene expression. On the other hand, this might also point to the fact that viral integration is not per se meant to deregulate the interrupted gene in the cell, as also can be concluded by the finding of HPV16 integrated in intergenic sequences of 10 OPSCC in this study.
In UCSCC, however, Ojesina et al. (2014) found significantly elevated host gene expression levels at sites of integration compared with expression levels of the same genes in tumors without integration. This was associated in a number of cases with copy number gains, but not at all sites, indicating that expression may also be driven by alternative mechanisms, such as the viral promotor of the integrant, other regulatory sequences and proteins, or decreased E6/E7 expression (Rusan et al. 2015).
Figure 1c shows several mechanisms by which HPV integration may directly affect gene expression, previously presented by Rusan et al. (2015), i.e., (1) integration in a tumor suppressor gene resulting in loss of gene function, (2) integration adjacent to an oncogene leading to gene amplification and expression or enhanced expression from the viral promotor and (3) intra- or interchromosomal rearrangements followed by altered expression of genes in involved regions. Examples of (1) are described above and may involve additional loss of the chromosome without the HPV integrant (Huebbers et al. 2013) or amplification or loss of gene components leading to truncated proteins, as has been found for the double-strand break DNA repair pathway gene RAD51B (Khoury et al. 2013; Ojesina et al. 2014; Parfenov et al. 2014). HPV integration upstream near or within the NR4A2 or MYC oncogenes in UCSCC and OPSCC are examples of (2) (Ferber et al. 2003; Wentsenzen et al. 2004; Ojesina et al. 2014; Parfenov et al. 2014), and examples of HPV insertion associated with chromosomal rearrangements, gene amplification and increased expression have been described by Akagi et al. (2014), Parfenov et al. (2014) and Olthof et al. (2015) involving the TP63 gene, a transcription factor with a role in epithelial development and highly expressed in squamous cell carcinomas (SCC).
In summary, recent as well as older literature has provided evidence that at least in a part of UCSCC and OPSCC HPV integration has a direct effect on the host genome and human gene expression, further underscored by recurrent integration events in specific genes. However, more studies are needed to fully explore the molecular mechanisms underlying human as well as viral gene expression as a result of HPV integration in anogenital and head and neck cancers.
6 HPV Integration in Relation to Viral Load, Methylated Genes and Outcome
A number of studies have examined other parameters in relation to HPV integration, although different methods have been used to determine the viral physical status. Olthof et al. (2014) examined whether tumors with episomal virus have a higher viral load than those with integration as determined by APOT and/or DIPS-PCR. For this purpose qPCR was performed on 73 OPSCC samples. Viral load ranged from 3.4 × 10−6 up to 97 HPV DNA copies per cell. When comparing the average viral load in cases with or without integration, no significant differences were seen (7 vs. 8.5 HPV DNA copies/cell). Furthermore, no correlation was found between the mean log2 expression levels of the viral genes E2, E6 or E7 and the viral load. This was also the case in 7 HPV16-positive HNSCC cell lines containing 2–7 integration sites, in which the viral load ranged from 1-739 HPV DNA copies/referencee gene (Beta-globin) copy (Olthof et al. 2015).
In two studies, methylation of human genes as well as E2-binding sites in the HPV LCR DNA, respectively, were examined and compared with the HPV integration status of head and neck cancers. In the first study, Parfenov et al. (2014) showed that DNA methylation profiles are distinct for HPV-positive tumors with integration than for those without integration. Differentially methylated genes included the tumor suppressors BARX2 and IRX4, and the oncogenes SIM2 and CTSE. The mechanism by which integration alters the methylation profile, however, remains to be elucidated (Rusan et al. 2015). In the second study, Reuschenbach et al. (2015) detected differential methylation levels in the HPV16 (LCR) E2-binding sites E2BS3 and E2BS4 depending on the viral DNA physical status, i.e., (1) complete methylation (>80 %) associated with the presence of integrated HPV genomes with an intact E2 gene; (2) intermediate methylation levels (20–80 %) with predominantly episomal HPV genomes with intact E2; and (3) no methylation (<20 %) with a disrupted E2 gene. Patients with high methylation levels tended to have a worse 5-year overall survival compared with patients with intermediate methylation (hazard ratio: 3.23). The authors therefore concluded that further studies are warranted to determine whether the E2BS methylation status may represent a prognostic marker.
A number of studies analyzed if tumors with HPV integration show a worse outcome as compared to tumors with episomal virus present. Parfenov et al. (2014) explored in primary head and neck cancers whether HPV integration was associated with clinical outcome or other clinical features (anatomic site, tumor stage, age, smoking status), but did not find significant associations. An explanation could be the relatively small sample size of the study. Vojtechova et al. (2016) recently analyzed a series of 186 tonsillar carcinomas showing integration in 43 % of cases as assessed by E2 mRNA mapping, which in a subset of tumors corresponded to APOT and Southern blotting data. These authors also did not find a statistically significant difference in disease-specific survival between patients with HPV-positive integrated vs. extrachromosomal/mixed forms of the virus. Finally, in cervical cancer patients treated with radiotherapy, Shin et al. (2014) found a trend toward decreased disease-free survival in patients with only HPV integrated forms versus patients with both integrated and episomal HPV. In conclusion, further studies are required to elucidate the relationship between HPV physical status (integrated vs. episomal vs. mixed integrated/episomal) and survival in both OPSCC and UCSCC.
Taken together, HPV integration affects both the viral and host genome, which may lead to deregulation of viral oncoproteins, critical cellular (cancer) genes as well as changes in DNA methylation, transcription and accumulation of chromosomal alterations (see also chapter “Molecular patterns and biology of HPV associated HNSCC” by Brakenhoff RH, Wagner S, Klussmann JP). More genome-wide studies with larger tumor series are necessary to further explore viral integration events, their impact on genomic alterations and the clinical implications of these findings.
References
Adams AK, Wise-Draper TM, Wells SI (2014) Human papillomavirus induced transformation in cervical and head and neck cancers. Cancers 6:1793–1820 doi:10.3390/cancers6031793
Akagi K, Li J, Broutian TR, Padilla-Nash H, Xiao W, Jiang B, Rocco JW, Teknos TN, Kumar B, Wangsa D, He D, Ried T, Symer DE, Gillison ML (2014) Genomewide analysis of HPV integration in human cancers reveals recurrent, focal genomic instability. Genome Res 24:185–199
Arenz A, Ziemann F, Mayer C, Wittig A, Dreffke K, Preising S, Wagner S, Klussmann JP, Engenhart-Cabillic R, Wittekindt C (2014) Increased radiosensitivity of HPV-positive head and neck cancer cell lines due to cell cycle dysregulation and induction of apoptosis. Strahlenther Onkol 190:839–846
Bechtold V, Beard P, Raj K (2003) Human papillomavirus type 16 E2 protein has no effect on transcription from episomal viral DNA. J Virol 77:2021–2028
Bernard HU, Burk RD, Chen Z et al (2010) Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology 401:70–79
Chandrani P, Kulkarni V, Iyer P, Upadhyay P, Chaubal R, Das P, Mulherkar R, Singh R, Dutt A (2015) NGS-based approach to determine the presence of HPV and their sites of integration in human cancer genome. Br J Cancer 112:1958–1965
Chen Y, Williams V, Filippova M, Filippov V, Duerksen-Hughes P (2014) Viral carcinogenesis: factors inducing DNA damage and viral integration. Cancers 6:2155–2186. doi:10.3390/cancers6042155
Cooper K, Herrington CS, Stickland JE, Evans MF, McGee JO (1991) Episomal and integrated human papillomavirus in cervical neoplasia shown by non-isotopic in situ hybridisation. J Clin Pathol 44:990–996
Cornet I, Kaanders JHAM, Kremer B, Speel EJM (2015) Hoofdhalskanker en HPV: hoe op maat te behandelen? Kanker Breed 7:26–29
Cullen AP, Reid R, Campion M, Lörincz AT (1991) Analysis of the physical state of different human papillomavirus DNAs in intraepithelial and invasive cervical neoplasm. J Virol 65:606–612
Egawa N, Egawa K, Griffin H, Doorbar J (2015) Human papillomaviruses; epithelial tropisms and the development of neoplasia. Viruses 7:3863–3890
Ferber MJ, Thorland EC, Brink AA, Rapp AK, Phillips LA, McGovern R, Gostout BS, Cheung TH, Chung TK, Fu WY, Smith DI (2003) Preferential integration of human papillomavirus type 18 near the c-myc locus in cervical carcinoma. Oncogene 22:7233–7242
Ganguly N, Parihar SP (2009) Human papillomavirus E6 and E7 oncoproteins as risk factors for tumorigenesis. J Biosci 34:113–123
Groves IJ, Coleman N (2015) Pathogenesis of human papillomavirus-associated mucosal disease. J Pathol 235:527–538
Hafkamp HC, Speel EJM, Haesevoets A, Bot FJ, Dinjens WNM, Ramaekers FCS, Hopman AHN, Manni JJ (2003) A subset of head and neck squamous cell carcinomas exhibits integration of HPV 16/18 DNA and overexpression of p16INK4A and p53 in the absence of mutations in exons 5–8. Int J Cancer 107:394–400
Hafkamp HC, Manni JJ, Haesevoets A, Voogd AC, Schepers M, Bot FJ, Hopman AHN, Ramaekers FCS, Speel EJM (2008) Marked differences in survival rate between smokers and non-smokers with HPV 16-associated tonsillar carcinomas. Int J Cancer 122:2656–2664
Hafkamp HC, Mooren JJ, Claessen SHM, Klingenberg B, Voogd AC, Bot FJ, Klussmann JP, Hopman AHN, Manni JJ, Kremer B, Ramaekers FCS, Speel EJM (2009) P21Cip1/WAF1 expression is strongly associated with HPV-positive tonsillar carcinoma and a favorable prognosis. Modern Pathol 22:686–698
Häfner N, Driesch C, Gajda M, Jansen L, Kirchmayr R, Runnebaum IB, Dürst M (2008) Integration of the HPV16 genome does not invariably result in high levels of viral oncogene transcripts. Oncogene 27:1610–1617
Herdman MT, Pett MR, Roberts I, Alazawi WO, Teschendorff AE, Zhang XY, Stanley MA, Coleman N (2006) Interferon-β treatment of cervical keratinocytes naturally infected with human papillomavirus 16 episomes promotes rapid reduction in episome numbers and emergence of latent integrants. Carcinogenesis 27:2341–2353
Hopman AHN, Smedts F, Dignef W, Ummelen M, Sonke G, Mravunac M, Vooijs GP, Speel EJM, Ramaekers FCS (2004) Transition of high grade cervical intraepithelial neoplasia to micro-invasive carcinoma is characterized by integration of HPV 16/18 and numerical chromosome abnormalities. J Pathol 202:23–33
Hopman AHN, Theelen W, Hommelberg P, Kamps MA, Herrington CS, Morrison LE, Speel EJM, Smedts F, Ramaekers FCS (2006) Genomic integration of oncogenic HPV and gain of the Human Telomerase Gene TERC at 3q26 are strongly associated events in the progression of uterine cervical dysplasia to invasive cancer. J Pathol 210:412–419
Hu Z, Zhu D, Wang W, Li W, Jia W, Zeng X, Ding W, Yu L, Wang X, Wang L, Shen H, Zhang C, Liu H, Liu X, Zhao Y, Fang X, Li S, Chen W, Tang T, Fu A, Wang Z, Chen G, Gao Q, Li S, Xi L, Wang C, Liao S, Ma X, Wu P, Li K, Wang S, Zhou J, Wang J, Xu X, Wang H, Ma D (2015) Genome-wide profiling of HPV integration in cervical cancer identifies clustered genomic hot spots and a potential microhomology-mediated integration mechanism. Nat Genet 47:158–163
Huebbers CU, Preuss SF, Kolligs J, Vent J, Stenner M, Wieland U, Silling S, Drebber U, Speel EJM, Klussmann JP (2013) Integration of HPV6 and downregulation of AKR1C3 expression mark malignant transformation in a patient with juvenile-onset laryngeal papillomatosis. PLoS ONE 8(2):e57207. doi:10.1371/journal.pone.0057207
Jeon S, Lambert PF (1995) Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: implications for cervical carcinogenesis. Proc Natl Acad Sci USA 92:1654–1658
Khoury JD, Tannir NM, Williams MD, Chen Y, Yao H, Zhang J, Thompson EJ, Network TCGA, Meric-Bernstam F, Medeiros LJ, Weinstein JN, Su X (2013) Landscape of DNA virus associations across human malignant cancers: analysis of 3,775 cases using RNA-Seq. J Virol 87:8916–8926
Klaes R, Woerner SM, Ridder R, Wentzensen N, DuerstM Schneider A, Lotz B, Melsheimer P, von Knebel Doeberitz M (1999) Detection of high-risk cervical intraepithelial neoplasia and cervical cancer by amplification of transcripts derived from integrated papillomavirus oncogenes. Cancer Res 59:6132–6136
Klingenberg B, Hafkamp HC, Haesevoets A, Manni JJ, Slootweg PJ, Weissenborn SJ, Klussmann JP, Speel EJM (2010) p16INK4A overexpression is frequently detected in tumor-free tonsil tissue without association with HPV. Histopathology 56:957–967
Kraus Christiansen I, Kjetil Sandve G, Schmitz M, Dürst M, Hovig E (2015) Transcriptionally active regions Are the Preferred Targets for Chromosomal HPV Integration in Cervical Carcinogenesis. PLoS ONE 10(3):e0119566. doi:10.1371/journal.pone.0119566
Lace MJ, Anson JR, Klussmann JP, Wang DH, Smith EM, Haugen TH, Turek LP (2011) Human papillomavirus type 16 (HPV-16) genomes integrated in head and neck cancers and in HPV-16-immortalized human keratinocyte clones express chimeric virus cell mRNAs similar to those found in cervical cancers. J Virol 85:1645–1654
Lace MJ, Anson JR, Haugen TH, Dierdorff JM, Turek LP (2015) Interferon treatment of human keratinocytes harboring extrachromosomal, persistent HPV-16 plasmid genomes induces de novo viral integration. Carcinogenesis 36:151–159
Leemans CR, Braakhuis BJ, Brakenhoff RH (2011) The molecular biology of head and neck cancer. Nat Rev Cancer 11:9–22
Li H, Yang Y, Zhang R, Cai Y, Yang X, Wang Z, Li Y, Cheng X, Ye X, Xiang Y, Zhu B (2013) Preferential sites for the integration and disruption of human papillomavirus 16 in cervical lesions. J Clin Virol 56:342–347
Lockwood WW, Coe BP, Williams AC, MacAuley C, Lam WL (2007) Whole genome tiling path aray CGH analysis of segmental copy number alterations in cervical cancer cell lines. Int J Cancer 120:436–443
Luft F, Klaes R, Nees M, Dürst M, Heilmann V, Melsheimer P, von Knebel Doeberitz M (2001) Detection of integrated papillomavirus sequences by ligation-mediated PCR (DIPS-PCR) and molecular characterization in cervical cancer cells. Int J Cancer 92:9–17
Moody CA, Laimins LA (2010) Human papillomavirus oncoproteins: pathways to transformation. Nat Rev Cancer 10:550–560
Mooren JJ, Kremer B, Claessen SMH, Voogd AC, Bot FJ, Klussmann JP, Huebbers CU, Hopman AHN, Ramaekers FCS, Speel EJM (2013) Chromosome stability in tonsillar squamous cell carcinomas is associated with HPV 16 integration and indicates a favourable prognosis. Int J Cancer 132:1781–1789
Mooren JJ, Gultekin SE, Straetmans JM, Haesevoets A, Peutz-Kootstra CJ, Huebbers CU, Dienes HP, Wieland U, Ramaekers FC, Kremer B, Speel EJ, Klussmann JP (2014) P16(INK4A) immunostaining is a strong indicator for high-risk-HPV-associated oropharyngeal carcinomas and dysplasias, but is unreliable to predict low-risk-HPV-infection in head and neck papillomas and laryngeal dysplasias. Int J Cancer 134:2108–2117
Nagao S, Yoshinouchi M, Miyagi Y, Hongo A, Kodama J, Itoh S, Kudo T (2002) Rapid and sensitive detection of physical status of human papillomavirus type 16 DNA by quantitative real-time PCR. J Clin Microbiol 40:863–867
Ojesina AI, Lichtenstein L, Freeman SS, Pedamallu CS, Imaz-Rosshandler I, Pugh TJ, Cherniack AD, Ambrogio L, Cibulskis K, Bertelsen B, Romero-Cordoba S, Treviño V, Vazquez-Santillan K, Guadarrama AS, Wright AA, Rosenberg MW, Duke F, Kaplan B, Wang R, Nickerson E, Walline HM, Lawrence MS, Stewart C, Carter SL, McKenna A, Rodriguez-Sanchez IP, Espinosa-Castilla M, Woie K, Bjorge L, Wik E, Halle MK, Hoivik EA, Krakstad C, Gabiño NB, Gómez-Macías GS, Valdez-Chapa LD, Garza-Rodríguez ML, Maytorena G, Vazquez J, Rodea C, Cravioto A, Cortes ML, Greulich H, Crum CP, Neuberg DS, Hidalgo-Miranda A, Escareno CR, Akslen LA, Carey TE, Vintermyr OK, Gabriel SB, Barrera-Saldaña HA, Melendez-Zajgla J, Getz G, Salvesen HB, Meyerson M (2014) Landscape of genomic alterations in cervical carcinomas. Nature 506:371–375
Olthof NC, Straetmans JMJAA, Snoeck R, Ramaekers FCS, Kremer B, Speel EJM (2012) Next generation treatment strategies for HPV-related head and neck squamous cell carcinomas: where do we go? Rev Med Virol 22:88–105
Olthof NC, Speel EJM, Kolligs J, Haesevoets A, Henfling M, Ramaekers FCS, Preuss SF, Drebber U, Wieland U, Silling S, Lam WL, Vucic EA, Kremer B, Klussmann JP, Huebbers CU (2014) Comprehensive analysis of HPV 16 integration in OSCC reveals no significant impact of physical status on viral oncogene and virally disrupted human gene expression. PLoS ONE 9(2):e88718. doi:10.1371/journal.pone.0088718
Olthof NC, Huebbers CU, Kolligs J, Henfling M, Ramaekers FC, Cornet I, van Lent-Albrechts JA, Stegmann AP, Silling S, Wieland U, Carey TE, Walline HM, Gollin SM, Hoffmann TK, de Winter J, Kremer B, Klussmann JP, Speel EJM (2015) Viral load, gene expression and mapping of viral integration sites in HPV16-associated HNSCC cell lines. Int J Cancer 136:E207–E218
Parfenov M, Pedamallu CS, Gehlenborg N, Freeman SS, Danilova L, Bristow CA, Lee S, Hadjipanayis AG, Ivanova EV, Wilkerson MD, Protopopov A, Yang L, Seth S, Song X, Tang J, Ren X, Zhang J, Pantazi A, Santoso N, Xu AW, Mahadeshwar H, Wheeler DA, Haddad RI, Jung J, Ojesina AI, Issaeva N, Yarbrough WG, Hayes DN, Grandis JR, El-Naggar AK, Meyerson M, Park PJ, Chin L, Seidman JG, Hammerman PS, Kucherlapati R, Network Cancer Genome Atlas (2014) Characterization of HPV and host genome interactions in primary head and neck cancers. Proc Natl Acad Sci U S A 111:15544–15549
Peitsaro P, Johansson B, Syrjanen S (2002) Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J Clin Microbiol 40:886–891
Peter M, Stransky N, Couturier J, Hupe P, Barillot E, de Cremoux P, Cottu P, Radvanyi F, Sastre-Garau X (2010) Frequent genomic structural alterations at HPV insertion sites in cervical carcinoma. J Pathol 221:320–330
Pett MR, Herdman MT, Palmer RD, Yeo GS, Shivji MK, Stanley MA, Coleman N (2006) Selection of cervical keratinocytes containing integrated HPV16 associates with episome loss and an endogenous antiviral response. Proc Natl Acad Sci USA 103:3822–3827
Pim D, Banks L (2010) Interaction of viral oncoproteins with cellular target molecules: infection with high-risk vs low-risk human papillomaviruses. APMIS 118:471–493
Raff AB, Woodham AW, Raff LM, Skeate JG, Yan L, Da Silva DM, Schelhaas M, Kast WM (2013) The evolving field of human papilloma virus receptor research: a review of binding and entry. J Virol 87:6062–6072
Rampias T, Sasaki C, Weinberger P, Psyrri A (2009) E6 and E7 gene silencing and transformed phenotype of human papillomavirus 16-positive oropharyngeal cancer cells. J Natl Cancer Inst 101:412–423
Reuschenbach M, Huebbers CU, Prigge ES, Bermejo JL, Kalteis MS, Preuss SF, Seuthe IM, Kolligs J, Speel EJM, Olthof N, Kremer B, Wagner S, Klussmann JP, Vinokurova S, von Knebel Doeberitz M (2015) Methylation status of HPV16 E2-binding sites classifies subtypes of HPV-associated oropharyngeal cancers. Cancer 121:1966–1976
Rieckmann T, Tribius S, Grob TJ, Meyer F, Busch CJ, Petersen C, Dikomey E, Kriegs M (2013) HNSCC cell lines positive for HPV and p16 possess higher cellular radiosensitivity due to an impaired DSB repair capacity. Radiother Oncol 107:242–246
Rusan M, Li YY, Hammerman PS (2015) Genomic landscape of human papillomavirus-associated cancers. Clin Cancer Res 21:2009–2019
Schiller JT, Day PM, Kines RC (2010) Current understanding of the mechanism of HPV infection. Gynecol Oncol 118:S12–17
Schmitz M, Driesch C, Jansen L, Runnebaum IB, Durst M (2012) Non-random integration of the HPV genome in cervical cancer. PLoS ONE 7(6):e39632. doi:10.1371/journal.pone.0039632
Shin HJ, Joo J, Yoon JH, Yoo CW, Kim JY (2014) Physical status of human papillomavirus integration in cervical cancer is associated with treatment outcome of the patients treated with radiotherapy. PLoS ONE 9(1):e78995. doi:10.1371/journal.pone.0078995
Snijders PJF, Heideman DAM, Meijer CJLM (2010) Methods for HPV detection in exfoliated cell and tissue specimens. APMIS 118:520–528
Southern SA, Noya F, Meyers C, Broker TR, Chow LT, Herrington CS (2001) Tetrasomy is induced by human papillomavirus type 18 E7 gene expression in keratinocyte raft cultures. Cancer Res 61:4858–4863
Thorland EC, Myers SL, Persing DH, Sarkar G, McGovern RM, Gostout BS, Smith DI (2000) Human papillomavirus type 16 integrations in cervical tumors frequently occur in common fragile sites. Cancer Res 60:5916–5921
Van Tine BA, Dao LD, Wu SY, Sonbuchner TM, Lin BY, Zou N, Chiang CM, Broker TR, Chow LT (2004a) Human papillomavirus (HPV) origin-binding protein associates with mitotic spindles to enable viral DNA partitioning. Proc Natl Acad Sci U S A 101:4030–4035
Van Tine BA, Kappes JC, Banerjee NS, Knops J, Lai L, Steenbergen RD, Meijer CL, Snijders PJ, Chatis P, Broker TR, Moen PT Jr, Chow LT (2004b) Clonal selection for transcriptionally active viral oncogenes during progression to cancer. J Virol 78:11172–11186
Vinokurova S, Wentzensen N, Kraus I, Klaes R, Driesch C, Melsheimer P, Kisseljov F, Dürst M, Schneider A, von Knebel Doeberitz M (2008) Type-dependent integration frequency of human papillomavirus genomes in cervical lesions. Cancer Res 68:307–313
Visalli G, Riso R, Facciolà A, Mondello P, Caruso C, Picerno I, Di Pietro A, Spataro P, Bertuccio MP (2016) Higher levels of oxidative DNA damage in cervical cells are correlated with the grade of dysplasia and HPV infection. J Med Virol 88:336–344
Vojtechova Z, Sabol I, Salakova M, Turek L, Grega M, Smahelova J, Vencalek O, Lukesova E, Klozar J, Tachezy R (2016) Analysis of the integration of human papillomaviruses in head and neck tumours in relation to patients’ prognosis. Int J Cancer 138:386–395
Wei L, Gravitt PE, Song H, Maldonado AM, Ozbun MA (2009) Nitric oxide induces early viral transcription coincident with increased DNA damage and mutation rates in human papillomavirus-infected cells. Cancer Res 69:4878–4884
Wentzensen N, Vinokurova S, von Knebel Doeberitz M (2004) Systematic review of genomic integration sites of human papillomavirus genomes in epithelial dysplasia and invasive cancer of the female lower genital tract. Cancer Res 64:3878–3884
Wiest T, Schwarz E, Enders C, Flechtenmacher C, Bosch FX (2002) Involvement of intact HPV16 E6/E7 gene expression in head and neck cancers with unaltered p53 status and perturbed pRb cell cycle control. Oncogene 21:1510–1517
World Health Organization (2007) Human papillomaviruses: IARC Monographs on the evaluation of carcinogenic risks to humans. International Agency for Research on Cancer, Lyon
World Health Organization (2014) Cancers of the female reproductive organs. In: Stewart BW, Wild CP (eds) World cancer report 2014. Lyon, IARC, pp 465–481
Woodman CBJ, Collins SI, Young LS (2007) The natural history of cervical HPV infection. Nat Rev Cancer 7:11–22
Xu B, Chotewutmontri S, Wolf S, Klos U, Schmitz M, Dürst M, Schwarz E (2013) Multiplex identification of human papillomavirus 16 DNA integration sites in cervical carcinomas. PLoS ONE 8(6):e66693. doi:10.1371/journal.pone.0066693
Ziegert C, Wentzensen N, Vinokurova S, Kisseljov F, Einenkel J, Hoeckel M, Knebel Doeberitz M (2003) A comprehensive analysis of HPV integration loci in anogenital lesions combining transcript and genome-based amplification techniques. Oncogene 22:3977–3984
zur Hausen H (2002) Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer 2:342–350
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Speel, E.J.M. (2017). HPV Integration in Head and Neck Squamous Cell Carcinomas: Cause and Consequence. In: Golusiński, W., Leemans, C., Dietz, A. (eds) HPV Infection in Head and Neck Cancer. Recent Results in Cancer Research, vol 206. Springer, Cham. https://doi.org/10.1007/978-3-319-43580-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-43580-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43578-7
Online ISBN: 978-3-319-43580-0
eBook Packages: MedicineMedicine (R0)