Abstract
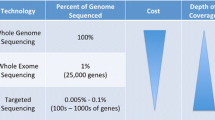
Molecular studies of endometrial cancer have evolved with the tools available to researchers: the methods for measuring nucleic acids, protein expression, and combinations thereof. Today “molecular genetic analysis” implies a broad range of indirect and direct tests that yield molecular phenotypes or genotypes, immunotypes, or signatures that were not conceived of when the histologic and biologic heterogeneity was first fully acknowledged.
We will provide a historical perspective on molecular genetic studies of endometrial cancers focusing on candidate genes and how early foundational research shaped both our understanding of the disease and current research directions. Examples of direct tests (mutation, DNA methylation, and/or protein expression) will be provided along with examples of indirect tests that have been and continue to be central to endometrial cancer molecular biology, such as DNA content or microsatellite instability analysis. We will highlight clinically relevant examples of molecular phenotyping and direct evaluation of candidate genes that integrate direct and indirect testing as part of routine patient care. This is not intended to be an exhaustive review but rather an overview of the progress that has been made and how early work is shaping current molecular, clinical, and biologic studies of endometrial cancer.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Endometrial cancer was for many years the red-headed stepchild of oncology: unwanted and neglected. Clinically focused research has led to improved detection and treatments. Molecular biologists, however, gave little attention to endometrial cancer at the time molecular tools first became available. This is somewhat surprising in light of the high incidence of endometrial cancer and the remarkable increase in the number of cases associated with the use of unopposed estrogens in the 1970s. The strong link between excess estrogen and risk for development of endometrial cancer did, however, provide a solid biologic framework for correlative and descriptive molecular studies. Researchers began to formulate and test hypotheses regarding the influence of steroid hormones and their receptors on endometrial cancer biology.
Initial molecular studies of endometrial cancer were largely based on observations from other cancer types (endometrial cancer remained a “me-too” subject of investigation). The candidate gene/candidate pathway approach nonetheless yielded important insights into the pathobiology of endometrial carcinoma. Over the past two decades it has become evident that the molecular complexity of these cancers is among the highest of common tumor types studied to date. Indeed the molecular heterogeneity is consistent with the histologic and clinical variability recognized today. The rapid evolution of methods for molecular biology and informatics continues to change the perception of endometrial cancer, and its ever rising incidence has garnered the attention of epidemiologists, health care providers, and health care economists (see Chaps. 1 and 2).
DNA Content Studies
Among the earliest molecular studies of endometrial cancers were DNA content analyses that began more than 60 years ago [1]. In 1902 Theodor Boveri proposed that chromosomal defects account for cancerous phenotypes [2]. Observational studies from the 1950s and 1960s proved that the total nucleic acid content of tumor cells can differ from nonmalignant cells. Aneuploidy, referring to abnormalities in the number of chromosomes, is a “mutator phenotype” [3, 4]. It was recognized early on in the study of endometrial cancers, and the clinical diagnostic and prognostic significance of DNA content has been explored repeatedly. DNA content analysis is an indirect test that can be used to measure what is referred to as a chromosomal instability (CIN) phenotype [5]. Mauland, Wik and Salvesen [6] have recently reviewed the clinical value of DNA content assessment in endometrial cancer focusing on DNA content as a potential prognostic and predictive maker. Despite more than two decades of investigation and numerous reports on positive association between abnormalities in tumor cell DNA content and factors known to portend poor outcome, the prognostic and predictive value of DNA ploidy in endometrial cancers remains controversial [7–9]. Prospective evaluation of the prognostic and predictive value of aneuploidy is ongoing. It is conceivable that an indirect test such as DNA content measurement might be replaced by what are potentially more resolving and more powerful copy number loss or gain analyses. It is equally possible that DNA ploidy assessment combined with direct tests for mutations, epigenetic marks, changes in transcription, and altered protein expression will come to the forefront of endometrial cancer management.
DNA Mismatch Repair (MMR): Molecular Phenotyping and Direct Assessment of Candidate Genes
Endometrioid endometrial cancers have one of the highest incidences of mismatch repair (MMR) defects in human cancers studied to date. Loss of DNA MMR is associated with an easily recognized tumor phenotype, microsatellite instability (MSI) . MSI is a result of somatic strand slippage mutations that have been referred to as replication errors [10, 11]. MSI analysis provides a convenient way of assessing the MMR status of tumors and falls into the category of indirect testing. When the tumor phenotype was first noted in familial colon cancers members of the conserved mutS, mutH, and mutL families were immediately recognized as candidate genes [12]. Loss of function alleles in mutS, mutH, and mutL genes in bacteria and yeast were known to lead to an accumulation of strand slippage mutations [13, 14]. In 1993, with the discovery of germline mutations in patients with familial/inherited colon cancer [15, 16], direct testing for MMR defects became possible and candidate genes were credentialed as causative factors. It was immediately obvious that carriers of MMR mutations had increased risk for endometrial cancer as well as colon cancer. This in turn spurred both direct and indirect testing for MMR defects in sporadic endometrial cancers and direct testing of candidate genes: MSI and mutation analyses. Immunohistochemistry (IHC) studies directly testing for loss of MMR proteins in tumors proceeded rapidly.
The initial studies focusing on the mutation status of candidates, specifically the MLH1, MSH2, MSH6, and PMS2 genes, were disappointing. Few MSI-positive tumors had mutations [17, 18]. However, methylation of MLH1 regulatory sequences, initially seen in colon cancers with MSI, was found in the majority of MSI-positive endometrial cancers and rarely in tumors with normal MMR (no MSI or so-called microsatellite stable (MSS) tumors) [19, 20]. Aberrant MLH1 methylation was linked to epigenetic silencing of MLH1 based on MLH1 protein measured by IHC: tumors with methylation failed to express MLH1 [20]. MLH1 promoter methylation thus became a direct test for a cause of MMR deficiency. Work by a number of groups confirmed methylation of MLH1 is frequent in tumors with MSI and that germline or somatic mutations in MLH1, MSH2, and PMS2 were seen at low frequency [17, 21, 22].
Although MMR defects associated with epigenetic silencing of MLH1 are seen frequently in endometrial cancers, the precise mechanisms by which MLH1 is silenced remain a matter of uncertainty. One factor contributing to MLH1 silencing is sequence variation at or near the MLH1 locus. Again, a candidate gene approach was pursued to test the hypothesis. In 2007, Chen and colleagues [23] provided evidence for heritable predisposition to epigenetic silencing of MLH1. A single nucleotide polymorphism in the 5′ untranslated regions (rs1800734) was shown to be associated with aberrant methylation of MLH1 in both endometrial and colon cancers using a nested case study design. The finding has been confirmed in several other cohorts [24, 25]. Subsequent work in colon cancer further suggested that variation in the MLH1 locus at rs1800734 might in fact be a low penetrance risk allele [26]. The same association with risk has also been reported for endometrial cancer [27]. It is noteworthy that association with aberrant methylation was recently reported in peripheral blood cells [28]. This discovery has important implications for normal aging and tumorigenesis.
The study of MMR defects and endometrial tumorigenesis began as a “me too” analysis. Endometrial cancers were underappreciated or seen as a minor component of the inherited colon cancer syndromes. Today endometrial cancer is recognized as a hallmark of inherited MMR deficiency and Lynch syndrome eponym has been adopted to reflect colon, endometrial, and other tumor risk [29]. The high frequency of MMR defects (tumor MSI) in endometrial cancer spurred a range of molecular studies. One of the candidate MMR genes, MSH6, had been considered to play a minor role in inherited susceptibility to colon cancer. MSH6’s possible causative role in endometrial cancer came to prominence with a report on MSH6 mutation in a family with Lynch syndrome in which several members were affected by endometrial cancer [30]. In 2004, a search for MSH6 mutation in endometrioid cancers revealed frequent germline MSH6 mutations [31]. The finding was confirmed in a second cohort shortly thereafter [32]. Today, alterations in MSH6 are recognized as perhaps the most frequent cause of inherited endometrial cancer and clinical testing for germline MSH6 mutation has been implemented widely for endometrial cancer patients with suspected Lynch syndrome.
Molecular testing of endometrial tumors is used in the triage for genetic testing for germline mutations . A combination of indirect and direct testing has been recommended: MSI, MMR IHC, MLH1 promoter methylation, and mutation analysis [33, 34]. Universal testing of MMR defects has been recommended by gynecologic oncology in an effort to identify patients with Lynch syndrome [35].
The link between MLH1 epigenetic silencing and endometrial tumorigenesis was firmly established in the late 1990s. The importance of loss of MMR in the initiation of endometrial cancer, be it due to inherited mutation in the context of Lynch syndrome or epigenetic silencing in sporadic endometrial cancers, was clear. In colorectal cancers, loss of MMR (MSI phenotype) was shown to be prognostic and ultimately predictive of outcome [36–38]. The discoveries in colon cancer led to similar analyses in endometrial cancer. Despite many published studies, some showing that MSI is associated with improved outcomes, others suggesting an association with reduced survival, and still other showing no effect, it is still unclear if tumor MSI is a prognostic marker. It has been suggested that both clinical heterogeneity and how MMR status is assessed and categorized (molecular lumping of indirect phenotyping of MMR status as normal or defective) may explain the differences among the different studies [39]. Bilbao-Sieyro and colleagues [40] have argued that lumping tumors into two groups, MSI-positive and MSS ignores the long appreciated variation and DNA content (ploidy) that could confound outcome studies.
The similarities and differences in MMR defects in endometrial and colon cancer have helped shape our understanding of the role MMR plays in cancer susceptibility, tumor initiation, and tumor progression. Inherited MSH6 mutations are far more common in endometrial cancer patients than colon cancer patients. On the surface this could be taken to mean that MSH6 is the guardian of the endometrial epithelium genome, and by extension its role in colonic epithelium less critical. However, loss of MMR due to epigenetic silencing of MLH1 is the most common cause of defective MMR in both colon and endometrial cancers and it is nearly twice as frequent in endometrial cancers than colon cancers. Clearly MMR defects help drive endometrial tumorigenesis. Molecular studies of uterine cancers focused on MMR defects will continue to rely on both direct and indirect testing methods. The Cancer Genome Atlas for uterine cancers [41] recognizes MMR deficiency as a defining feature of one of the major molecularly defined classes of endometrial cancer: tumors that have MSI and many more somatic mutations than their MMR normal counterparts. The genomic landscape of endometrial cancers is discussed in greater detail in Chap. 5.
Steroid Hormone Receptors
Aberrant steroid hormone signaling has been implicated in endometrial tumorigenesis for over a half century [42–44]. Early studies exploring the relationship between hormone receptor status and clinical parameters relied largely on radiolabeled ligand binding assays. Absence of estrogen receptor (ER) and progesterone receptor (PR) has been associated with high tumor grade, advanced stage, metastasis, and recurrence [45–48]. Today it is widely accepted that estrogen excess is associated with risk for the development of endometrial cancer [49, 50], progesterone can have antitumor activities [51, 52], and absence of the receptors on tumors appears to be associated with poor outcomes for endometrial cancer patients [53].
A major technical advance is the study of steroid hormone receptors in endometrial cancer came in 1986 when Budwit-Novotny and colleagues [54] described the use of monoclonal antibodies to detect ER and PR in tissue samples. IHC methods made it possible to distinguish between glandular and stromal expression and to determine the subcellular localization of the receptors [55, 56]. IHC analysis could also be used to conveniently study large numbers of tumors. IHC confirmed earlier reports that reduced steroid hormone receptor expression is associated with factors that portend poor outcomes in endometrial cancer patients including advanced stage, high tumor grade, advanced patient age, and presence of lymphovascular space invasion [57–61]. There are many reports on the potential prognostic significance of ER and PR expression in endometrial cancers, but to date there have been no prospective, well-controlled IHC studies [53, 62–65].
Advances in molecular biology have repeatedly changed the prism through which hormone receptors are viewed. Gene cloning and new tools for molecular biology have shown how very complex steroid hormone signaling is in normal tissues and in disease. Early IHC expression studies in endometrial cancer did not account for the multiple ER and PR protein isoforms, nor did they consider ER and PR cofactors. It is clear that estrogen, progesterone, and their receptors all play critical roles in endometrial cancer biology. In some regards it appears that the more we know, the less we understand.
There are two estrogen receptor genes, ESR1 and ESR2, encoding ERα and ERβ, respectively [66, 67]. Work in many different systems has led to general acceptance that ERβ acts to oppose the actions of the canonical ERα isoform in normal tissues in breast, ovarian, and endometrial cancers [68–70]. The complexity of ERα and ERβ gene regulation makes receptor analysis in primary tissue specimens extremely challenging. Although both the alpha and beta forms bind estrogen responsive elements, they recruit different cofactors to regulate different targets or have opposite effects on the same targets [71–74]. At least three ERα and five ERβ isoforms exist and all of these are likely to play unique roles in hormone signaling [75, 76].
A single PGR gene exists that encodes at least seven transcripts with three established isoforms, PR-A, PR-B, and the less well-studied PR-C, along with several possible other isoforms [77–80]. Like ERα and ERβ, PR-A and PR-B have distinct molecular targets.
Candidate Tumor Suppressors and Oncogenes
TP53
The tumor suppressor gene TP53 is the most frequently mutated gene in human cancers [81]. TP53’s role in endometrial cancer has been a subject of investigation for over two decades using indirect tests (testing for allelic deletion) or direct tests for mutations or overexpression of TP53 protein. Today it is known that TP53 is mutated in over 90 % of serous endometrial cancers and is infrequently mutated in low grade endometrioid endometrial tumors [41]. However, early studies did not always make clear distinctions between type I and type II endometrial cancers or histologically different tumors as the existence of distinctive biology was not yet established.
In 1991, Okamoto and colleagues [82] first reported on TP53 abnormalities in endometrial cancers. They tested 24 tumors for evidence of loss of heterozygosity (LOH) using Southern blot-based restriction fragment length polymorphism (RFLP) analysis with a panel of 57 markers representing all chromosomes. Five tumors had LOH on the short arm of chromosome 17 involving TP53. Using single strand conformation analysis and Sanger sequencing of variants, Okamoto and colleagues [82] went on to demonstrate two of these five cases with LOH also harbored TP53 mutations as would be expected for a classical “two-hit” tumor suppressor. In the same year, it was reported that TP53 mutations were common in endometrial cancer cell lines [83]. TP53 expression measured by IHC and indicative of TP53 mutations was observed in 21 % of endometrial cancers studied by Kohler and colleagues [84]. Collectively, the analyses in the early 1990s described earlier firmly established a role for TP53 in a subset of endometrial cancers.
The relationship between TP53 mutation and pathologic features was further explored by Enomoto et al. [85] who assessed TP53 mutation and LOH as well as KRAS mutations in endometrial cancer and atypical hyperplasia samples. TP53 alterations were seen in ~25 % of samples, including atypical hyperplasias, with a higher rate of TP53 defects in grade 3 endometrioid endometrial cancers than in grade 1 or 2 tumors. TP53 and KRAS mutation tended to be mutually exclusive, which provided some early insights into the existence of molecularly distinct subgroups of endometrial tumors [85].
In an effort to determine if TP53 mutations occur as early events in endometrial tumorigenesis, Kohler and colleagues investigated simple, complex, and atypical endometrial hyperplasia and carcinomas for mutations using single-strand conformational variant (SSCV) analysis coupled with direct sequencing. No mutations were identified in the hyperplasias, including 41 atypical hyperplasia specimens, and based on these findings the authors postulated that TP53 mutation is a late event in endometrial tumorigenesis [86]. The study by Kohler and colleagues [86] did not include endometrial intraepithelial carcinoma or endometrial glandular dysplasia specimens, the putative precursors of serous endometrial carcinoma. Sherman et al. [87] reported findings for TP53 expression (IHC status) in broad range of endometrial specimens including benign endometrium, atypical endometrial hyperplasia and endometrial intraepithelial carcinoma samples, as well as endometrioid, clear cell, and serous carcinomas. They noted positive TP53 staining (indicative of TP53 defects) for most endometrial intraepithelial carcinoma, clear cell, and serous samples. In contrast, only 20 % of endometrioid samples were positive, and all atypical endometrial hyperplasia and benign endometrium samples were negative. This study helped to establish that TP53 mutation is indeed an early and frequent event in serous and clear cell endometrial carcinomas, and that mutations were less common in endometrioid tumors and rare in the histologically defined precursors of endometrioid cancer [87]. Recent studies that rely on more sensitive methods have confirmed an increasing frequency of TP53 abnormalities with progression from normal endometrium through endometrial glandular dysplasia and endometrial intraepithelial carcinoma to serous carcinoma [88].
TP53 was one of the first candidate genes studied as a prognostic marker in endometrial cancer. Several reports suggested association between mutation status and/or positive IHC staining and features associated with poor outcome including nonendometrioid histology, advanced stage, and high grade [84, 89–91]. Subsequent studies of larger cohorts revealed TP53 status is not an independent marker of poor outcome in multivariable analyses that included histologic subtype as a confounding variable [92–95]. It is noteworthy that the rates of TP53 mutation in endometrioid cancers reported in early studies tend to be higher than what has been reported in recent years. Possible explanations for the higher mutation rates in early studies are sample bias to larger and/or higher stage and grade tumors and misclassification of nonendometrioid tumors as TP53-mutated endometrioid endometrial cancers [41].
PTEN
The PTEN tumor suppressor is the most frequently mutated gene in endometrial cancer. Its existence and importance in endometrial cancers was first suggested by the results of deletion mapping studies (indirect tests for tumor suppressor function). Allelic loss/deletion of the genomic region including the PTEN locus was recognized in endometrial cancers several years before the PTEN gene was cloned. In 1994, Jones and colleagues reported on loss of heterozygosity (LOH) studies in endometrial cancers with a panel of 29 microsatellite markers distributed across the genome as part of an effort to map the location of tumor suppressors. More than a third of tumors had deletion of 10q [96]. The finding of frequent 10q deletion in endometrial cancers was subsequently confirmed and the minimum region of deletion mapped to 10q23-26 [97]. In 1997 the PTEN gene, a novel tumor suppressor mapping to 10q23, was cloned and shown to be mutated in a range of malignancies [98, 99]. Following the initial discovery, Kong et al. examined mutation (direct testing) and LOH status of PTEN in a panel of endometrial, colorectal, gastric, and pancreatic carcinomas [100]. They found that mutation and LOH were seen infrequently in colorectal, gastric, and pancreatic tumors. However, among the endometrial cancers tested, 48 % showed LOH and 55 % were mutated, with most mutations resulting in clear loss of function [100]. The Kong et al. study provided the first evidence that PTEN is frequently mutated in endometrial cancers and strongly suggested that PTEN is the 10q tumor suppressor for which there is strong selection for deletion in endometrial cancers.
Around the same time, Tashiro et al. examined a panel of endometrioid endometrial cancers , serous endometrial cancer, ovarian cancer, and cervical carcinomas and found that mutation in PTEN is specific to endometrioid endometrial cancers [101]. A follow-up study confirmed that PTEN mutations are much more frequent in endometrioid than serous or clear cell endometrial cancers [102]. PTEN became the most commonly mutated tumor suppressor gene in endometrial cancers, and endometrial cancers garnered a great deal of attention by geneticists and cancer biologists interested in PTEN.
A potential link between PTEN mutation and MMR status was established shortly after the PTEN gene was discovered. MSI-positive tumors appeared to have more frequent PTEN mutation. Furthermore, it was initially reported that outcomes were better for women with PTEN mutant tumors [102]. Mutter and colleagues determined that PTEN defects occur early in tumorigenesis by analyzing cancers and precancers [103]. It was subsequently shown that PTEN lesions might precede MMR defects, which were previously established as occurring early in the development of endometrial cancers [104]. With the advent or antibodies for immunohistochemical analysis of PTEN expression and direct testing for defects, the Mutter lab confirmed that loss of PTEN protein is observed in some normal endometrial glands. They speculated that concurrent loss of PTEN and additional critical regulators of development may be necessary for malignant transformation [105]. Given the high frequency of both mutation and deletion of PTEN in endometrial cancers, it was not surprising that a search for epigenetic silencing of PTEN was undertaken. It has been reported that PTEN can also be inactivated through promoter methylation [106], but how frequently this occurs is uncertain and further methylation studies in endometrial cancers using additional methods are warranted [107].
Because PTEN mutation is an early event in tumorigenesis many groups have investigated the utility of PTEN staining in precancerous lesions to predict progression to carcinoma. Several studies suggest that there is a stepwise decrease in PTEN expression between normal endometrium, precancerous lesions (endometrial intraepithelial neoplasia and complex atypical hyperplasia), and endometrial cancer [103, 105, 108–111]. A large study by Lacey et al. published in 2008, on the other hand, found that PTEN IHC is not useful for predicting progression of atypical endometrial hyperplasia to endometrioid endometrial cancer [112]. Similar reports have found that PTEN negativity in endometrial intraepithelial neoplasia is not sufficient to predict malignant transformation, although combining PTEN status with nuclear atypia increases prediction sensitivity and specificity [113, 114]. The inconsistent findings are likely attributable to etiologic heterogeneity and the reliability of the tests used.
Traditional approaches to molecular genetic analysis include generation and characterization of genetically modified animals. The functional consequences of in vivo PTEN loss were first examined in 1999 by Podsypanina and colleagues who developed a knockout mouse model and observed that the Pten+/− heterozygous animals developed neoplasms in the endometrium, as well as liver, prostate, GI tract, thyroid, and thymus [115]. By 6 months of age, 100 % of Pten+/− mice exhibited endometrial hyperplasia, providing evidence to the importance of PTEN in this tissue [116]. Early studies combining in vivo loss of PTEN with other genetic alterations in cancer-associated genes determined that loss of tumor suppressors such as INK4a/ARF [117], MLH1 [118], and MIG6 [119] accelerated hyperplastic growth and led to development of carcinomas. In contrast, loss of the Akt oncogene in Pten+/− mice was found to be protective, particularly in the endometrium [120]. The Pten +/− mouse model was later used to show in vivo that loss of PTEN leads to elevated Akt activation and a subsequent increase in ER signaling that drives endometrial hyperplasia/carcinoma [121]. Interestingly, neonatal estrogen exposure was also found to be protective against endometrial hyperplasia [122]. Interest in endometrial cancer and research investments in endometrial tumorigenesis grew remarkably when PTEN’s role in endometrial tumorigenesis was appreciated. The endometrium became a model system in which to study perturbed signaling.
In 2008, Diakoku et al. developed an inducible uterine-specific homozygous Pten knockout using a PR (progesterone receptor) (Cre+/−) Pten(fl/fl) system. At the time a conditional knock out was state of the art, but today it is a traditional approach in mouse genetic analysis. Diakoku and colleagues demonstrated that homozygous deletion of Pten led to development of carcinomas with 100 % penetrance and early onset [123]. The model has been subsequently used to further investigate other common genetic events in endometrial cancers in vivo, in the absence of Pten. These studies have shown that endometrial carcinogenesis can be accelerated through mutational activation of Pik3ca [124], loss of Apc [125], loss of Cdh1 [126], and loss of Lkb1 [127], and that knockout of Grp78 prevents carcinoma development [128]. Today the “one gene at a time” approach for mouse models for endometrial cancer seems particularly daunting given how many genes have been implicated based on candidate gene studies alone.
The use of tumor PTEN protein expression to predict patient outcome and/or response to therapy has been extensively studied over the past 15 years. Complete loss of PTEN protein and RNA (direct tests) occurs in many patient samples, although the reported percentage of PTEN negative tumors varies between 7 and 65 %, depending on the methods used and patient population investigated [9, 129–131]. The frequent involvement of a gene, such as PTEN, in endometrial cancer makes it an attractive candidate for therapeutics, but based on frequency alone, an unlikely prognostic marker. An early report by Mutter et al. described reduced PTEN protein compared to normal endometrium in most cancers investigated and 13 of 33 cases had no immunodetectable protein [103]. A similar report from Salvesen et al. found that 20 % of EC tumors examined had loss of PTEN, and in their study PTEN negativity was associated with metastasis [9]. Still another study showed that PTEN negative tumors tend to be less well differentiated than PTEN-expressing EECs [132]. The high frequency of PTEN abnormalities combined with the many different mutations that coexist with PTEN defects explains why clear pictures regarding PTEN status and clinical features have failed to emerge. A subgroup of PTEN negative tumors that also lack p27 are well differentiated and have favorable outcome [133]. Recent comprehensive mutation studies that include PTEN and other candidates show consistent high frequency of PTEN mutation or deletion in endometrioid tumors, plus or minus other common and rare mutations: these next-generation studies reflect what we began to learn by studying one candidate at a time, then combinations. Studying PTEN alone, as was done in early studies, gave mixed results as might be expected. PTEN negativity was associated with poor outcome [131, 134, 135] but there are clear contrasting reports [136, 137]. Among advanced stage patients, PTEN negativity is associated with favorable response to chemotherapy, and although this was first reported over a decade ago, PTEN status has never been used in the clinic to direct treatment strategies [138, 139]. The candidate gene PTEN is undeniably important in endometrial cancer. At present the prognostic and predictive significance of PTEN defects in endometrial cancer is entirely unknown.
KRAS
The ras family of oncogenes is frequently mutated in cancers [140, 141]. Most mutations inhibit ras GTPase activity, resulting in constitutively active ras and activation of the downstream PI3-kinase and MAP-kinase pathways. The potential role for ras family members in endometrial cancer was first investigated more than a quarter of a century ago using immunohistochemistry [142, 143]. Direct testing for the known activating mutations followed [144, 145].
Ras mutations in endometrial cancers typically are in KRAS, with much less frequent involvement of NRAS and HRAS [146, 147].
KRAS mutations were first identified using PCR and dot plot hybridization mutational screening for a small number of tumors, half of which harbored KRAS mutations [145]. Shortly thereafter KRAS mutation was implicated as an early event in endometrial tumorigenesis based on the observation that some endometrial hyperplasias carried KRAS mutations [146]. With advances in methods for mutation testing, specifically PCR amplification of tumor DNAs and allele specific oligomer dot-blot hybridization, it was possible to analyze larger numbers of specimens and to interrogate additional base substitutions. Duggan and colleagues tested KRAS codons 12 and 13 for mutations in 60 endometrial cancers (a sizeable number of specimens at the time) and found that mutations were present in both the carcinomas and surrounding atypical hyperplasia [148]. The use of UV radiation fractionation to interrogate the mutation status of precancerous cells firmly established a role for KRAS early in endometrial tumorigenesis [148]. Additional early studies on ras mutation status in smaller numbers of cases provided a wide range of mutation frequency for KRAS ranging from 10 % for primary tumors to 64 % for cell lines [147, 149, 150].
There were early reports on differences in KRAS mutation frequency in different histologic subtypes of endometrial cancer: differences in the methods for mutation detection and histological classification of tumors likely explain some of the apparently contradictory findings for early studies. The overall consensus is that KRAS mutations are infrequent in nonendometrioid cancers. KRAS mutations, predominantly involving codon 12, are present in ~20 % of endometrioid tumors with no clear difference in mutation frequencies in tumors with intact mismatch repair and MSI-positive tumors [34, 41, 151–154].
Aberrant ras activity could provide therapeutic opportunities in endometrial cancer and although ras mutations were among the first defects described, the finding has not translated to new therapies. Pharmacologically, direct targeting of the ras family remains elusive [155], although recent efforts have shown some promise [156, 157]. The use of molecules targeting downstream ras effectors (e.g., mTOC1/2, PI3-kinase, AKT) has been explored in preclinical models and clinical trials [158]. Activation of ras in endometrial cancers may ultimately factor into treatment and even prevention strategies.
FGFR2
Members of fibroblast growth factor receptor (FGFR) family (FGFRs 1–4) play important roles in development, normal cellular processes, and pathophysiology [159]. The FGFRs are classic multifunctional receptor tyrosine kinases for which combinations of receptor isoforms and multiple ligands afford tremendous functional diversity. FGFRs activate the ras, src, and PI3-kinase pathways [160]. Kinome screens (mutation analysis of a large number of kinases) were undertaken in cancer cell lines and a variety of primary cancers with the goal of identifying druggable targets [161–163]. The FGFRs were recognized as potential oncogenes, but largely lacking cancer associations. FGFR2, however, became a candidate oncogene/drug target for endometrial cancers when mutations were identified in uterine cancer cell lines (http://www.sanger.ac.uk/genetics/CGP/CellLines). Mutations in FGFR2 were first reported in primary endometrial cancers in 2007 [164]. The majority of alterations seen in endometrial cancers are missense mutations that have previously been characterized as causative germline mutations in patients with congenital craniofacial developmental disorders (S525W and N550K as two examples) [164]. Activation of ras signaling appears to mediate the oncogenicity of FGFR2 mutations [165, 166] and not surprisingly KRAS and FGFR2 mutations are nearly mutually exclusive. The therapeutic implications for activating FGFR2 mutations in endometrial cancer were recognized by both cancer biologists and developmental biologist [167, 168]. Efficacy of FGFR2 inhibition was shown in endometrial cancer cell lines using the FGFR/VEGF inhibitor PD173074 as a single agent [165, 169] and in combination with doxorubicin and paclitaxel [170]. FGFR2 thus became a viable target for therapeutic intervention in endometrial cancers: the candidate gene from a cell line screen was confirmed by simple mutation analysis in primary tumors and drug testing in cells lines. Years of work in other experimental systems, driven in large part by the importance of FGFR2 mutations in human congenital malformation syndromes, paved the way for clinical trials in endometrial cancer using anti-FGFR agents. What, if any clinical benefit for endometrial cancer patients will come from FGFR2 inhibitor remains to be determined. The importance of discovery of FGFR2 activation is nonetheless important. It has further highlighted the roles of multiple signaling axes in endometrial cancers and has prompted questions regarding the function that FGFR signaling plays in the normal endometrium, precancerous endometrium, and in frank carcinoma.
Combinations of Molecular Defects Explain the Biology
Early genetic studies in endometrial cancer were performed one gene/one factor at a time. The findings from those early studies have provided both conceptual and biological frameworks for multifactor molecular approaches currently being used to characterize endometrial cancers. The idiom nanos gigantum humeris insidentes (discovering truth by building on previous discoveries) seems particularly apt as we begin to adopt “next-generation” technologies for molecular analysis of endometrial cancers. The increasing resolution for the cancer cell genomic landscape will have meaning only if we look back to where we have come from. Doubtless some of the giants we have already discovered (PTEN, MMR defects, steroid hormones, and their receptors and others) will provide important vantage points as we seek to understand the genomic complexity of individual tumors and endometrial cancers in general.
References
Sandritter W. Nucleic acid content of different neoplasms; adenocarcinomata, renal, thyroid, liver carcinoma and liver sarcoma. Frankf Z Pathol. 1952;63:432–46.
Harris H. Concerning the origin of malignant tumours by Theodor Boveri. Translated and annotated by Henry Harris. Preface. J Cell Sci. 2008;121 Suppl 1:v–vi.
Lengauer C, Kinzler KW, Vogelstein B. Genetic instability in colorectal cancers. Nature. 1997;386:623–7.
Loeb LA. Mutator phenotype may be required for multistage carcinogenesis. Cancer Res. 1991;51:3075–9.
McClelland SE, Burrell RA, Swanton C. Chromosomal instability A composite phenotype that influences sensitivity to chemotherapy. Cell Cycle. 2009;8:3262–6.
Mauland KK, Wik E, Salvesen HB. Clinical value of DNA content assessment in endometrial cancer. Cytometry B Clin Cytom. 2014;86:154–63.
Moberger B, Auer G, Forsslund G, et al. The prognostic significance of DNA measurements in endometrial carcinoma. Cytometry. 1984;5:430–6.
Auer G, Eriksson E, Azavedo E, et al. Prognostic significance of nuclear DNA content in mammary adenocarcinomas in humans. Cancer Res. 1984;44:394–6.
Salvesen HB, Akslen LA. Molecular pathogenesis and prognostic factors in endometrial carcinoma. APMIS. 2002;110:673–89.
Ionov Y, Peinado MA, Malkhosyan S, et al. Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis. Nature. 1993;363:558–61.
Parsons R, Li GM, Longley MJ, et al. Hypermutability and mismatch repair deficiency in RER+ tumor cells. Cell. 1993;75:1227–36.
Aaltonen LA, Peltomaki P, Leach FS, et al. Clues to the pathogenesis of familial colorectal cancer. Science. 1993;260:812–6.
Levinson G, Gutman GA. High frequencies of short frameshifts in poly-CA/TG tandem repeats borne by bacteriophage M13 in Escherichia coli K-12. Nucleic Acids Res. 1987;15:5323–38.
Strand M, Prolla TA, Liskay RM, et al. Destabilization of tracts of simple repetitive DNA in yeast by mutations affecting DNA mismatch repair. Nature. 1993;365:274–6.
Fishel R, Lescoe MK, Rao MR, et al. The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell. 1993;75:1027–38.
Leach FS, Nicolaides NC, Papadopoulos N, et al. Mutations of a mutS homolog in hereditary nonpolyposis colorectal cancer. Cell. 1993;75:1215–25.
Katabuchi H, van Rees B, Lambers AR, et al. Mutations in DNA mismatch repair genes are not responsible for microsatellite instability in most sporadic endometrial carcinomas. Cancer Res. 1995;55:5556–60.
Kowalski LD, Mutch DG, Herzog TJ, et al. Mutational analysis of MLH1 and MSH2 in 25 prospectively-acquired RER+ endometrial cancers. Genes Chromosomes Cancer. 1997;18:219–27.
Esteller M, Levine R, Baylin SB, et al. MLH1 promoter hypermethylation is associated with the microsatellite instability phenotype in sporadic endometrial carcinomas. Oncogene. 1998;17:2413–7.
Simpkins SB, Bocker T, Swisher EM, et al. MLH1 promoter methylation and gene silencing is the primary cause of microsatellite instability in sporadic endometrial cancers. Hum Mol Genet. 1999;8:661–6.
Kobayashi K, Matsushima M, Koi S, et al. Mutational analysis of mismatch repair genes, hMLH1 and hMSH2, in sporadic endometrial carcinomas with microsatellite instability. Jpn J Cancer Res. 1996;87:141–5.
Basil JB, Swisher EM, Herzog TJ, et al. Mutational analysis of the PMS2 gene in sporadic endometrial cancers with microsatellite instability. Gynecol Oncol. 1999;74:395–9.
Chen H, Taylor NP, Sotamaa KM, et al. Evidence for heritable predisposition to epigenetic silencing of MLH1. Int J Cancer. 2007;120:1684–8.
Raptis S, Mrkonjic M, Green RC, et al. MLH1–93G > A promoter polymorphism and the risk of microsatellite-unstable colorectal cancer. J Natl Cancer Inst. 2007;99:463–74.
Allan JM, Shorto J, Adlard J, et al. MLH1–93G > A promoter polymorphism and risk of mismatch repair deficient colorectal cancer. Int J Cancer. 2008;123:2456–9.
Whiffin N, Broderick P, Lubbe SJ, et al. MLH1-93G > A is a risk factor for MSI colorectal cancer. Carcinogenesis. 2011;32:1157–61.
Poplawski T, Sobczuk A, Sarnik J, et al. Polymorphism of DNA mismatch repair genes in endometrial cancer. Exp Oncol. 2015;37:44–7.
Savio AJ, Lemire M, Mrkonjic M, et al. MLH1 region polymorphisms show a significant association with CpG island shore methylation in a large cohort of healthy individuals. PLoS One. 2012;7:e51531.
Watson P, Lynch HT. Extracolonic cancer in hereditary nonpolyposis colorectal cancer. Cancer. 1993;71:677–85.
Wijnen J, De Leeuw W, Vasen H, et al. Familial endometrial cancer in female carriers of MSH6 germline mutations. Nat Genet. 1999;23:142–4.
Goodfellow PJ, Buttin BM, Herzog TJ, et al. Prevalence of defective DNA mismatch repair and MSH6 mutation in an unselected series of endometrial cancers. Proc Natl Acad Sci U S A. 2003;100:5908–13.
Hampel H, Frankel W, Panescu J, et al. Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res. 2006;66:7810–7.
Buchanan DD, Tan YY, Walsh MD, et al. Tumor mismatch repair immunohistochemistry and DNA MLH1 methylation testing of patients with endometrial cancer diagnosed at age younger than 60 years optimizes triage for population-level germline mismatch repair gene mutation testing. J Clin Oncol. 2014;32:90–100.
Goodfellow P, Billingsley CC, Lankes H, et al. Combined MSI, MLH1 methylation analysis and IHC for Lynch syndrome screening for 1002 endometrial cancers from GOG210: an NRG Oncology/Gynecologic Oncology Group study. J Clin Oncol. 2015;33(36):4301–8.
Lancaster JM, Powell CB, Chen LM, et al. Society of Gynecologic Oncology statement on risk assessment for inherited gynecologic cancer predispositions. Gynecol Oncol. 2015;136:3–7.
Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med. 2003;349:247–57.
Kim GP, Colangelo LH, Wieand HS, et al. Prognostic and predictive roles of high-degree microsatellite instability in colon cancer: a National Cancer Institute-National Surgical Adjuvant Breast and Bowel Project Collaborative Study. J Clin Oncol. 2007;25:767–72.
Sargent DJ, Marsoni S, Monges G, et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol. 2010;28:3219–26.
Diaz-Padilla I, Romero N, Amir E, et al. Mismatch repair status and clinical outcome in endometrial cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2013;88:154–67.
Bilbao-Sieyro C, Ramirez R, Rodriguez-Gonzalez G, et al. Microsatellite instability and ploidy status define three categories with distinctive prognostic impact in endometrioid endometrial cancer. Oncotarget. 2014;5:6206–17.
Kandoth C, Schultz N, Cherniack AD, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73.
Larson JA. Estrogens and endometrial carcinoma. Obstet Gynecol. 1954;3:551–72.
Meissner WA, Sommers SC, Sherman G. Endometrial hyperplasia, endometrial carcinoma, and endometriosis produced experimentally by estrogen. Cancer. 1957;10:500–9.
Brush MG, Taylor RW, King RJ, et al. The uptake and metabolism of (6,7-3H)oestrediol by human endometrial carcinoma tissue in vivo and in vitro. J Endocrinol. 1968;41:12–3.
McCarty Jr KS, Barton TK, Fetter BF, et al. Correlation of estrogen and progesterone receptors with histologic differentiation in endometrial adenocarcinoma. Am J Pathol. 1979;96:171–83.
Kauppila A, Kujansuu E, Vihko R. Cytosol estrogen and progestin receptors in endometrial carcinoma of patients treated with surgery, radiotherapy, and progestin. Clinical correlates. Cancer. 1982;50:2157–62.
Kauppila AJ, Isotalo HE, Kivinen ST, et al. Prediction of clinical outcome with estrogen and progestin receptor concentrations and their relationships to clinical and histopathological variables in endometrial cancer. Cancer Res. 1986;46:5380–4.
Liao BS, Twiggs LB, Leung BS, et al. Cytoplasmic estrogen and progesterone receptors as prognostic parameters in primary endometrial carcinoma. Obstet Gynecol. 1986;67:463–7.
Siiteri PK. Steroid hormones and endometrial cancer. Cancer Res. 1978;38:4360–6.
Henderson BE, Ross RK, Pike MC, et al. Endogenous hormones as a major factor in human cancer. Cancer Res. 1982;42:3232–9.
Lentz SS, Brady MF, Major FJ, et al. High-dose megestrol acetate in advanced or recurrent endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol. 1996;14:357–61.
Thigpen JT, Brady MF, Alvarez RD, et al. Oral medroxyprogesterone acetate in the treatment of advanced or recurrent endometrial carcinoma: a dose-response study by the Gynecologic Oncology Group. J Clin Oncol. 1999;17:1736–44.
Werner HM, Salvesen HB. Current status of molecular biomarkers in endometrial cancer. Curr Oncol Rep. 2014;16:403.
Budwit-Novotny DA, McCarty KS, Cox EB, et al. Immunohistochemical analyses of estrogen receptor in endometrial adenocarcinoma using a monoclonal antibody. Cancer Res. 1986;46:5419–25.
Snijders MP, De Goeij AF, Koudstaal J, et al. Is immunohistochemical analysis of oestrogen and progesterone receptors in endometrial carcinoma superior to the radioligand binding assay? J Pathol. 1990;161:129–35.
Segreti EM, Novotny DB, Soper JT, et al. Endometrial cancer: histologic correlates of immunohistochemical localization of progesterone receptor and estrogen receptor. Obstet Gynecol. 1989;73:780–5.
Gehrig PA, Van Le L, Olatidoye B, et al. Estrogen receptor status, determined by immunohistochemistry, as a predictor of the recurrence of stage I endometrial carcinoma. Cancer. 1999;86:2083–9.
Carcangiu ML, Chambers JT, Voynick IM, et al. Immunohistochemical evaluation of estrogen and progesterone receptor content in 183 patients with endometrial carcinoma. Part I: clinical and histologic correlations. Am J Clin Pathol. 1990;94:247–54.
Chambers JT, Carcangiu ML, Voynick IM, et al. Immunohistochemical evaluation of estrogen and progesterone receptor content in 183 patients with endometrial carcinoma. Part II: correlation between biochemical and immunohistochemical methods and survival. Am J Clin Pathol. 1990;94:255–60.
Kleine W, Maier T, Geyer H, et al. Estrogen and progesterone receptors in endometrial cancer and their prognostic relevance. Gynecol Oncol. 1990;38:59–65.
Pertschuk LP, Masood S, Simone J, et al. Estrogen receptor immunocytochemistry in endometrial carcinoma: a prognostic marker for survival. Gynecol Oncol. 1996;63:28–33.
Miyamoto T, Watanabe J, Hata H, et al. Significance of progesterone receptor-A and -B expressions in endometrial adenocarcinoma. J Steroid Biochem Mol Biol. 2004;92:111–8.
Sakaguchi H, Fujimoto J, Hong BL, et al. Drastic decrease of progesterone receptor form B but not A mRNA reflects poor patient prognosis in endometrial cancers. Gynecol Oncol. 2004;93:394–9.
Shabani N, Kuhn C, Kunze S, et al. Prognostic significance of oestrogen receptor alpha (ERalpha) and beta (ERbeta), progesterone receptor A (PR-A) and B (PR-B) in endometrial carcinomas. Eur J Cancer. 2007;43:2434–44.
Jongen V, Briet J, de Jong R, et al. Expression of estrogen receptor-alpha and -beta and progesterone receptor-A and -B in a large cohort of patients with endometrioid endometrial cancer. Gynecol Oncol. 2009;112:537–42.
Mosselman S, Polman J, Dijkema R. ER beta: identification and characterization of a novel human estrogen receptor. FEBS Lett. 1996;392:49–53.
Klinge CM. Estrogen receptor interaction with estrogen response elements. Nucleic Acids Res. 2001;29:2905–19.
Leygue E, Dotzlaw H, Watson PH, et al. Expression of estrogen receptor beta1, beta2, and beta5 messenger RNAs in human breast tissue. Cancer Res. 1999;59:1175–9.
Rutherford T, Brown WD, Sapi E, et al. Absence of estrogen receptor-beta expression in metastatic ovarian cancer. Obstet Gynecol. 2000;96:417–21.
Thomas C, Gustafsson JA. The different roles of ER subtypes in cancer biology and therapy. Nat Rev Cancer. 2011;11:597–608.
Waters KM, Safe S, Gaido KW. Differential gene expression in response to methoxychlor and estradiol through ERalpha, ERbeta, and AR in reproductive tissues of female mice. Toxicol Sci. 2001;63:47–56.
Lindberg MK, Moverare S, Skrtic S, et al. Estrogen receptor (ER)-beta reduces ERalpha-regulated gene transcription, supporting a “ying yang” relationship between ERalpha and ERbeta in mice. Mol Endocrinol. 2003;17:203–8.
Frasor J, Barnett DH, Danes JM, et al. Response-specific and ligand dose-dependent modulation of estrogen receptor (ER) alpha activity by ERbeta in the uterus. Endocrinology. 2003;144:3159–66.
Bjornstrom L, Sjoberg M. Mechanisms of estrogen receptor signaling: convergence of genomic and nongenomic actions on target genes. Mol Endocrinol. 2005;19:833–42.
Moore JT, McKee DD, Slentz-Kesler K, et al. Cloning and characterization of human estrogen receptor beta isoforms. Biochem Biophys Res Commun. 1998;247:75–8.
Poola I, Speirs V. Expression of alternatively spliced estrogen receptor alpha mRNAs is increased in breast cancer tissues. J Steroid Biochem Mol Biol. 2001;78:459–69.
Kastner P, Krust A, Turcotte B, et al. Two distinct estrogen-regulated promoters generate transcripts encoding the two functionally different human progesterone receptor forms A and B. EMBO J. 1990;9:1603–14.
Wei LL, Gonzalez-Aller C, Wood WM, et al. 5'-Heterogeneity in human progesterone receptor transcripts predicts a new amino-terminal truncated “C”-receptor and unique A-receptor messages. Mol Endocrinol. 1990;4:1833–40.
Wei LL, Miner R. Evidence for the existence of a third progesterone receptor protein in human breast cancer cell line T47D. Cancer Res. 1994;54:340–3.
Samalecos A, Gellersen B. Systematic expression analysis and antibody screening do not support the existence of naturally occurring progesterone receptor (PR)-C, PR-M, or other truncated PR isoforms. Endocrinology. 2008;149:5872–87.
Petitjean A, Achatz MI, Borresen-Dale AL, et al. TP53 mutations in human cancers: functional selection and impact on cancer prognosis and outcomes. Oncogene. 2007;26:2157–65.
Okamoto A, Sameshima Y, Yamada Y, et al. Allelic loss on chromosome 17p and p53 mutations in human endometrial carcinoma of the uterus. Cancer Res. 1991;51:5632–5.
Yaginuma Y, Westphal H. Analysis of the p53 gene in human uterine carcinoma cell lines. Cancer Res. 1991;51:6506–9.
Kohler MF, Berchuck A, Davidoff AM, et al. Overexpression and mutation of p53 in endometrial carcinoma. Cancer Res. 1992;52:1622–7.
Enomoto T, Fujita M, Inoue M, et al. Alterations of the p53 tumor suppressor gene and its association with activation of the c-K-ras-2 protooncogene in premalignant and malignant lesions of the human uterine endometrium. Cancer Res. 1993;53:1883–8.
Kohler MF, Nishii H, Humphrey PA, et al. Mutation of the p53 tumor-suppressor gene is not a feature of endometrial hyperplasias. Am J Obstet Gynecol. 1993;169:690–4.
Sherman ME, Bur ME, Kurman RJ. p53 in endometrial cancer and its putative precursors: evidence for diverse pathways of tumorigenesis. Hum Pathol. 1995;26:1268–74.
Jia L, Liu Y, Yi X, et al. Endometrial glandular dysplasia with frequent p53 gene mutation: a genetic evidence supporting its precancer nature for endometrial serous carcinoma. Clin Cancer Res. 2008;14:2263–9.
Tsuda H, Hirohashi S. Frequent occurrence of p53 gene mutations in uterine cancers at advanced clinical stage and with aggressive histological phenotypes. Jpn J Cancer Res. 1992;83:1184–91.
Reinartz JJ, George E, Lindgren BR, et al. Expression of p53, transforming growth factor alpha, epidermal growth factor receptor, and c-erbB-2 in endometrial carcinoma and correlation with survival and known predictors of survival. Hum Pathol. 1994;25:1075–83.
Inoue M, Okayama A, Fujita M, et al. Clinicopathological characteristics of p53 overexpression in endometrial cancers. Int J Cancer. 1994;58:14–9.
Ito K, Watanabe K, Nasim S, et al. Prognostic significance of p53 overexpression in endometrial cancer. Cancer Res. 1994;54:4667–70.
Soong R, Knowles S, Williams KE, et al. Overexpression of p53 protein is an independent prognostic indicator in human endometrial carcinoma. Br J Cancer. 1996;74:562–7.
Geisler JP, Geisler HE, Wiemann MC, et al. p53 expression as a prognostic indicator of 5-year survival in endometrial cancer. Gynecol Oncol. 1999;74:468–71.
Stelloo E, Bosse T, Nout RA, et al. Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol. 2015;28(6):836–44.
Jones MH, Koi S, Fujimoto I, et al. Allelotype of uterine cancer by analysis of RFLP and microsatellite polymorphisms: Frequent loss of heterozygosity on chromosome amrs 3p, 9q, 10q, and 17p. Genes Chromosomes Cancer. 1994;9:119–23.
Peiffer SL, Herzog TJ, Tribune DJ, et al. Allelic loss of sequences from the long arm of chromosome 10 and replication errors in endometrial cancers. Cancer Res. 1995;55:1922–6.
Li J, Yen C, Liaw D, et al. PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast and prostate cancer. Science. 1997;275:1943–7.
Steck PA, Pershouse MA, Jasser SA, et al. Identification of a candidate tumour suppressor gene, MMAC1, at chromosome 10q23.3 that is mutated in multiple advanced cancers. Nat Genet. 1997;15:356–62.
Kong D, Suzuki A, Zou TT, et al. PTEN1 is frequently mutated in primary endometrial carcinomas. Nat Genet. 1997;17:143–4.
Tashiro H, Blazes MS, Wu R, et al. Mutations in PTEN are frequent in endometrial carcinoma but rare in other common gynecological malignancies. Cancer Res. 1997;57:3935–40.
Risinger JI, Hayes K, Maxwell GL, et al. PTEN mutation in endometrial cancers is associated with favorable clinical and pathologic characteristics. Clin Cancer Res. 1998;4:3005–10.
Mutter GL, Lin MC, Fitzgerald JT, et al. Altered PTEN expression as a diagnostic marker for the earliest endometrial precancers. J Natl Cancer Inst. 2000;92:924–30.
Zhou XP, Kuismanen S, Nystrom-Lahti M, et al. Distinct PTEN mutational spectra in hereditary non-polyposis colon cancer syndrome-related endometrial carcinomas compared to sporadic microsatellite unstable tumors. Hum Mol Genet. 2002;11:445–50.
Monte NM, Webster KA, Neuberg D, et al. Joint loss of PAX2 and PTEN expression in endometrial precancers and cancer. Cancer Res. 2010;70:6225–32.
Salvesen HB, MacDonald N, Ryan A, et al. PTEN methylation is associated with advanced stage and microsatellite instability in endometrial carcinoma. Int J Cancer. 2001;91:22–6.
Zysman MA, Chapman WB, Bapat B. Considerations when analyzing the methylation status of PTEN tumor suppressor gene. Am J Pathol. 2002;160:795–800.
Sobczuk A, Smolarz B, Romanowicz-Makowska H, et al. MMAC/PTEN gene expression in endometrial cancer: RT-PCR studies. Pol J Pathol. 2006;57:137–40.
Norimatsu Y, Moriya T, Kobayashi TK, et al. Immunohistochemical expression of PTEN and beta-catenin for endometrial intraepithelial neoplasia in Japanese women. Ann Diagn Pathol. 2007;11:103–8.
Kapucuoglu N, Aktepe F, Kaya H, et al. Immunohistochemical expression of PTEN in normal, hyperplastic and malignant endometrium and its correlation with hormone receptors, bcl-2, bax, and apoptotic index. Pathol Res Pract. 2007;203:153–62.
Sarmadi S, Izadi-Mood N, Sotoudeh K, et al. Altered PTEN expression; a diagnostic marker for differentiating normal, hyperplastic and neoplastic endometrium. Diagn Pathol. 2009;4:41.
Lacey Jr JV, Mutter GL, Ronnett BM, et al. PTEN expression in endometrial biopsies as a marker of progression to endometrial carcinoma. Cancer Res. 2008;68:6014–20.
Baak JP, Van Diermen B, Steinbakk A, et al. Lack of PTEN expression in endometrial intraepithelial neoplasia is correlated with cancer progression. Hum Pathol. 2005;36:555–61.
Pavlakis K, Messini I, Vrekoussis T, et al. PTEN-loss and nuclear atypia of EIN in endometrial biopsies can predict the existence of a concurrent endometrial carcinoma. Gynecol Oncol. 2010;119:516–9.
Podsypanina K, Ellenson LH, Nemes A, et al. Mutation of Pten/Mmac1 in mice causes neoplasia in multiple organ systems. Proc Natl Acad Sci U S A. 1999;96:1563–8.
Stambolic V, Tsao MS, Macpherson D, et al. High incidence of breast and endometrial neoplasia resembling human Cowden syndrome in pten+/- mice. Cancer Res. 2000;60:3605–11.
You MJ, Castrillon DH, Bastian BC, et al. Genetic analysis of Pten and Ink4a/Arf interactions in the suppression of tumorigenesis in mice. Proc Natl Acad Sci U S A. 2002;99:1455–60.
Wang H, Douglas W, Lia M, et al. DNA mismatch repair deficiency accelerates endometrial tumorigenesis in Pten heterozygous mice. Am J Pathol. 2002;160:1481–6.
Kim TH, Franco HL, Jung SY, et al. The synergistic effect of Mig-6 and Pten ablation on endometrial cancer development and progression. Oncogene. 2010;29:3770–80.
Chen ML, Xu PZ, Peng XD, et al. The deficiency of Akt1 is sufficient to suppress tumor development in Pten+/- mice. Genes Dev. 2006;20:1569–74.
Vilgelm A, Lian Z, Wang H, et al. Akt-mediated phosphorylation and activation of estrogen receptor alpha is required for endometrial neoplastic transformation in Pten+/- mice. Cancer Res. 2006;66:3375–80.
Begum M, Tashiro H, Katabuchi H, et al. Neonatal estrogenic exposure suppresses PTEN-related endometrial carcinogenesis in recombinant mice. Lab Invest. 2006;86:286–96.
Daikoku T, Hirota Y, Tranguch S, et al. Conditional loss of uterine Pten unfailingly and rapidly induces endometrial cancer in mice. Cancer Res. 2008;68:5619–27.
Joshi A, Miller Jr C, Baker SJ, et al. Activated mutant p110alpha causes endometrial carcinoma in the setting of biallelic Pten deletion. Am J Pathol. 2015;185:1104–13.
van der Zee M, Jia Y, Wang Y, et al. Alterations in Wnt-beta-catenin and Pten signalling play distinct roles in endometrial cancer initiation and progression. J Pathol. 2013;230:48–58.
Lindberg ME, Stodden GR, King ML, et al. Loss of CDH1 and Pten accelerates cellular invasiveness and angiogenesis in the mouse uterus. Biol Reprod. 2013;89:8.
Cheng H, Liu P, Zhang F, et al. A genetic mouse model of invasive endometrial cancer driven by concurrent loss of Pten and Lkb1 Is highly responsive to mTOR inhibition. Cancer Res. 2014;74:15–23.
Lin YG, Shen J, Yoo E, et al. Targeting the glucose-regulated protein-78 abrogates Pten-null driven AKT activation and endometrioid tumorigenesis. Oncogene. 2015;34(43):5418–26.
Yaginuma Y, Yamashita T, Ishiya T, et al. Abnormal structure and expression of PTEN/MMAC1 gene in human uterine cancers. Mol Carcinog. 2000;27:110–6.
Oh WK, George DJ, Kantoff PW. Rapid rise of serum prostate specific antigen levels after discontinuation of the herbal therapy PC-SPES in patients with advanced prostate carcinoma: report of four cases. Cancer. 2002;94:686–9.
Uegaki K, Kanamori Y, Kigawa J, et al. PTEN-positive and phosphorylated-Akt-negative expression is a predictor of survival for patients with advanced endometrial carcinoma. Oncol Rep. 2005;14:389–92.
Kimura F, Watanabe J, Hata H, et al. PTEN immunohistochemical expression is suppressed in G1 endometrioid adenocarcinoma of the uterine corpus. J Cancer Res Clin Oncol. 2004;130:161–8.
Dellas A, Jundt G, Sartorius G, et al. Combined PTEN and p27kip1 protein expression patterns are associated with obesity and prognosis in endometrial carcinomas. Clin Cancer Res. 2009;15:2456–62.
Erkanli S, Kayaselcuk F, Kuscu E, et al. Expression of survivin, PTEN and p27 in normal, hyperplastic, and carcinomatous endometrium. Int J Gynecol Cancer. 2006;16:1412–8.
Athanassiadou P, Athanassiades P, Grapsa D, et al. The prognostic value of PTEN, p53, and beta-catenin in endometrial carcinoma: a prospective immunocytochemical study. Int J Gynecol Cancer. 2007;17:697–704.
Mackay HJ, Gallinger S, Tsao MS, et al. Prognostic value of microsatellite instability (MSI) and PTEN expression in women with endometrial cancer: results from studies of the NCIC Clinical Trials Group (NCIC CTG). Eur J Cancer. 2010;46:1365–73.
Akiyama-Abe A, Minaguchi T, Nakamura Y, et al. Loss of PTEN expression is an independent predictor of favourable survival in endometrial carcinomas. Br J Cancer. 2013;109:1703–10.
Kanamori Y, Kigawa J, Itamochi H, et al. PTEN expression is associated with prognosis for patients with advanced endometrial carcinoma undergoing postoperative chemotherapy. Int J Cancer. 2002;100:686–9.
Terakawa N, Kanamori Y, Yoshida S. Loss of PTEN expression followed by Akt phosphorylation is a poor prognostic factor for patients with endometrial cancer. Endocr Relat Cancer. 2003;10:203–8.
Fernandez-Medarde A, Santos E. Ras in cancer and developmental diseases. Genes Cancer. 2011;2:344–58.
Pylayeva-Gupta Y, Grabocka E, Bar-Sagi D. RAS oncogenes: weaving a tumorigenic web. Nat Rev Cancer. 2011;11:761–74.
Agnantis NJ, Spandidos DA, Mahera H, et al. Immunohistochemical study of ras oncogene expression in endometrial and cervical human lesions. Eur J Gynaecol Oncol. 1988;9:360–5.
Long CA, O’Brien TJ, Sanders MM, et al. ras oncogene is expressed in adenocarcinoma of the endometrium. Am J Obstet Gynecol. 1988;159:1512–6.
Lester DR, Cauchi MN. Point mutations at codon 12 of C-K-ras in human endometrial carcinomas. Cancer Lett. 1990;51:7–10.
Enomoto T, Inoue M, Perantoni AO, et al. K-ras activation in neoplasms of the human female reproductive tract. Cancer Res. 1990;50:6139–45.
Enomoto T, Inoue M, Perantoni AO, et al. K-ras activation in premalignant and malignant epithelial lesions of the human uterus. Cancer Res. 1991;51:5308–14.
Ignar-Trowbridge D, Risinger JI, Dent GA, et al. Mutations of the Ki-ras oncogene in endometrial carcinoma. Am J Obstet Gynecol. 1992;167:227–32.
Duggan BD, Felix JC, Muderspach LI, et al. Early mutational activation of the c-Ki-ras oncogene in endometrial carcinoma. Cancer Res. 1994;54:1604–7.
Fujimoto I, Shimizu Y, Hirai Y, et al. Studies on ras oncogene activation in endometrial carcinoma. Gynecol Oncol. 1993;48:196–202.
Boyd J, Risinger JI. Analysis of oncogene alterations in human endometrial carcinoma: prevalence of ras mutations. Mol Carcinog. 1991;4:189–95.
Sasaki H, Nishii H, Takahashi H, et al. Mutation of the Ki-ras protooncogene in human endometrial hyperplasia and carcinoma. Cancer Res. 1993;53:1906–10.
Swisher EM, Peiffer-Schneider S, Mutch DG, et al. Differences in patterns of TP53 and KRAS2 mutations in a large series of endometrial carcinomas with or without microsatellite instability. Cancer. 1999;85:119–26.
Lax SF, Kendall B, Tashiro H, et al. The frequency of p53, K-ras mutations, and microsatellite instability differs in uterine endometrioid and serous carcinoma: evidence of distinct molecular genetic pathways. Cancer. 2000;88:814–24.
Xiong J, He M, Jackson C, et al. Endometrial carcinomas with significant mucinous differentiation associated with higher frequency of k-ras mutations: a morphologic and molecular correlation study. Int J Gynecol Cancer. 2013;23:1231–6.
Sawyers CL. Finding and drugging the vulnerabilities of RAS-dependent cancers. Cell. 2009;137:796–8.
Ostrem JM, Peters U, Sos ML, et al. K-Ras(G12C) inhibitors allosterically control GTP affinity and effector interactions. Nature. 2013;503:548–51.
Maurer T, Garrenton LS, Oh A, et al. Small-molecule ligands bind to a distinct pocket in Ras and inhibit SOS-mediated nucleotide exchange activity. Proc Natl Acad Sci U S A. 2012;109:5299–304.
Slomovitz BM, Coleman RL. The PI3K/AKT/mTOR pathway as a therapeutic target in endometrial cancer. Clin Cancer Res. 2012;18:5856–64.
Carter EP, Fearon AE, Grose RP. Careless talk costs lives: fibroblast growth factor receptor signalling and the consequences of pathway malfunction. Trends Cell Biol. 2015;25: 221–33.
Teven CM, Farina EM, Rivas J, et al. Fibroblast growth factor (FGF) signaling in development and skeletal diseases. Genes Dis. 2014;1:199–213.
Stephens P, Edkins S, Davies H, et al. A screen of the complete protein kinase gene family identifies diverse patterns of somatic mutations in human breast cancer. Nat Genet. 2005;37:590–2.
Bardelli A, Parsons DW, Silliman N, et al. Mutational analysis of the tyrosine kinome in colorectal cancers. Science. 2003;300:949.
Ruhe JE, Streit S, Hart S, et al. Genetic alterations in the tyrosine kinase transcriptome of human cancer cell lines. Cancer Res. 2007;67:11368–76.
Pollock PM, Gartside MG, Dejeza LC, et al. Frequent activating FGFR2 mutations in endometrial carcinomas parallel germline mutations associated with craniosynostosis and skeletal dysplasia syndromes. Oncogene. 2007;26:7158–62.
Byron SA, Gartside MG, Wellens CL, et al. Inhibition of activated fibroblast growth factor receptor 2 in endometrial cancer cells induces cell death despite PTEN abrogation. Cancer Res. 2008;68:6902–7.
Taniguchi F, Harada T, Sakamoto Y, et al. Activation of mitogen-activated protein kinase pathway by keratinocyte growth factor or fibroblast growth factor-10 promotes cell proliferation in human endometrial carcinoma cells. J Clin Endocrinol Metab. 2003;88:773–80.
Shukla V, Coumoul X, Wang RH, et al. RNA interference and inhibition of MEK-ERK signaling prevent abnormal skeletal phenotypes in a mouse model of craniosynostosis. Nat Genet. 2007;39:1145–50.
Wilkie AO. Cancer drugs to treat birth defects. Nat Genet. 2007;39:1057–9.
Dutt A, Salvesen HB, Chen TH, et al. Drug-sensitive FGFR2 mutations in endometrial carcinoma. Proc Natl Acad Sci U S A. 2008;105:8713–7.
Byron SA, Loch DC, Pollock PM. Fibroblast growth factor receptor inhibition synergizes with Paclitaxel and Doxorubicin in endometrial cancer cells. Int J Gynecol Cancer. 2012;22:1517–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Walker, C.J., Goodfellow, P.J. (2017). Traditional Approaches to Molecular Genetic Analysis. In: Hedrick Ellenson, L. (eds) Molecular Genetics of Endometrial Carcinoma. Advances in Experimental Medicine and Biology, vol 943. Springer, Cham. https://doi.org/10.1007/978-3-319-43139-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-43139-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43137-6
Online ISBN: 978-3-319-43139-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)