Abstract
Because of their ubiquitous distribution and high level of cross-reactivity, profilins and polcalcins are classified as panallergens. To date, 43 profilin and 15 polcalcin allergens have been identified. Panallergens frequently cause a pattern of multiple sensitizations in skin prick tests. Moreover, IgE specific for a number of biologically unrelated allergen sources exist. These sensitizations and cross-reactivities are usually irrelevant and, only sporadically, do panallergens represent clinically relevant major allergens. On rare occasions, severe allergic reactions to food have been observed among profilin-allergic patients. Pronounced sensitization to polcalcins may possibly be linked to an elevated risk of asthma. Moreover, panallergens affect the analytical specificity of pollen and food allergen extracts in skin prick tests and in IgE-based diagnosis. Thus, sensitization toward panallergens resembles an important indication to complement allergy diagnosis with source-related, species-specific marker major allergens. These marker allergens contribute significantly to the analytical specificity necessary for identifying the disease-eliciting allergen sources for allergen-specific immunotherapy.
This article is based on a publication of the authors published in 2012 in the Allergo Journal (Hauser M, Wallner M, Ferreira F, Mahler V, Kleine-Tebbe J (2012): Das Konzept der Pollen-Panallergerne. Allergo J 21: 291–293) which has now been updated, extended, and translated as a book chapter.
The authors gratefully thank Dr. Steve Love, PhD, Laguna Niguel, CA, USA, for reading the manuscript, helpful suggestions, and editorial assistance with the English translation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Because of their ubiquitous distribution and their high level of cross-reactivity, profilins and polcalcins are classified as panallergens. To date, 43 profilin and 15 polcalcin allergens have been identified as allergens (for review see also Matricardi et al. 2016). Profilins are actin-binding proteins, which explain their functionality in many essential cellular processes. They can be identified in various plant-derived foods, pollen, and latex. Polcalcins are expressed exclusively in pollen, and, as indicated by the name, they function in the regulation of intracellular Ca++ levels.
In skin prick tests, panallergens frequently cause a pattern of multiple sensitizations. Moreover, IgE specific for a variety of biologically unrelated allergen sources exists. These sensitizations and cross-reactivities are usually irrelevant, and only in rare cases panallergens do represent clinically relevant major allergens.
In some clinical reports of profilin-allergic patients, especially those with grass or weed pollen allergies in areas with high pollen exposure, severe allergic reactions toward certain foods (e.g., melon) have been observed. Pronounced sensitization to polcalcins could possibly be linked to an elevated risk of asthma (i.e., in cedar or cypress pollen-allergic individuals). Moreover, panallergens also affect the analytical specificity of pollen and food allergen extracts in skin prick tests and IgE-based diagnosis. Sensitization to panallergens (i.e., Bet v 2 or Ph p 12), which are accompanied by multiple reactions toward biologically unrelated pollen extracts (i.e., in skin prick tests), requires further allergy diagnosis with source-related, species-specific marker major allergens (i.e., Bet v 1, Ole e 1, Phl p 1/Phl p5, Art v 1, or Amb a 1). These marker allergens contribute significantly to the analytical specificity necessary for identifying the disease-eliciting allergen sources (tree, grass, or weed pollen) used for allergen-specific immunotherapy (AIT).
2 Allergen Nomenclature
Because of their ubiquitous distribution and high structural similarity, panallergens are responsible for widespread cross-reactions, even between botanically unrelated plant species. Profilins as well as polcalcins (Ca++-binding proteins found in pollen) are generally classified as panallergens. Numerous molecules belonging to the families of profilins and polcalcins have already been identified and described as allergens. Due to their fundamental roles in cell function, these proteins are highly conserved and widely distributed. While the occurrence of polcalcins is restricted to tree, grass, and weed pollen, profilins have been identified in pollen, plant-derived foods (fruits, vegetables, legumes, nuts), and latex, but also in animal organisms.
3 Structure and Function of Profilins
Profilins are ubiquitous, cytosolic proteins present in all eukaryotic cells. Despite a relatively variable amino acid sequence and polypeptide chain length, the structure of profilins is highly conserved. This provides the molecular basis for high serologic cross-reactivity. Structurally, the center of the molecule is a compact beta-sheet which is surrounded by alpha-helices (Fig. 3.1a). Profilins are actin-binding proteins and can also bind other ligands, such as phosphoinositides or poly-L-proline. Phosphoinositides constitute only a small fraction of cellular phospholipids; however they control many essential processes during the life of a cell. These lipids regulate ion channels and vesicular transport and are capable of modulating lipid metabolism via a close interplay with lipid transfer proteins (Balla 2013). This suggests a role of profilins in processes such as endo- and exocytosis, as well as intracellular signaling.
3D ribbon structures of (a) allergenic profilins and (b) allergenic polcalcins. The accession numbers of the protein database (PDB, www.rcsb.org) are given in parentheses. Alpha-helices are depicted in red, beta-sheets in yellow, and unordered structures in green. Bound Ca++ are indicated by yellow spheres
Profilins regulate actin polymerization and, thus, cell mobility and are, therefore, also involved in cell separation, cell elongation, outgrowth of pollen tube or root hairs, and rapid cytoplasmic streaming (Hauser et al. 2010). Consequently, profilin-deficient plants display phenotypes of dwarfism or reduced fruit setting (Le et al. 2006).
Additionally, 50 ligands of profilins have been identified, suggesting that profilins are key regulators of molecular processes of complex intracellular networks (Witke 2004). Profilins share the property of binding to poly-L-proline with prolyl hydroxylases. It was this binding property that led to the initial identification of profilins as contaminants during purification of prolyl hydroxylase enzymes (Tanaka and Shibata 1995). Now, however, poly-L-proline is successfully used to purify allergenic profilins (Wopfner et al. 2008).
The strongly IgE cross-reactive profilins represent cytosolic proteins with conserved structures, found in all eukaryotic cells. They regulate actin polymerization and are involved in the control of multiple molecular processes within intracellular networks.
4 Relevance of Profilins
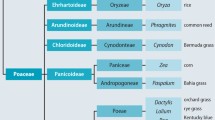
In 1991, Bet v 2 was identified as the first allergenic profilin in birch pollen (Valenta et al. 1991). Since then, a series of tree, grass, and weed pollen profilins as well as profilins from plant-derived foods and latex have been described as allergens (reviewed also in Matricardi et al. 2016). At present, 43 allergenic profilins have officially been acknowledged by the WHO/IUIS allergen nomenclature subcommittee (Fig. 3.2), including 20 profilin allergens from pollen and latex and 23 profilins from foods (www.allergen.org).
List of cross-reactive allergenic profilins officially acknowledged by the WHO/IUIS allergen nomenclature subcommittee (Photos were obtained from www.fotolia.com)
Sensitization rates to pollen profilin allergens are, in general, highly related to geography, with 5–40 % of the allergic population affected. In Germany, sensitization rates of 10–15 % have been reported. IgE to Phl p 12 was observed in 23 % of a large Italian children’s cohort. The prevalence, being associated with sensitizations to grass and olive pollen major allergens, declined from northern to southern Italy (Asero et al. 2015). Sensitization rates to mugwort (Art v 4) and ragweed (Amb a 8) profilins among weed pollen-allergic patients in Italy were about 20 %, while Austrian weed pollen allergics showed sensitization rates of 45–50 % (Wopfner et al. 2008). On average, sensitization to pollen profilins is around 30 %, while certain weed pollen, e.g., from Chenopodium album (white goosefoot) or Mercurialis annua (annual mercury) but also the pollen from date palm (Phoenix dactylifera), evoke sensitization rates to profilins of more than 50 % (Asturias et al. 2005; Barderas et al. 2004; Vallverdu et al. 1997).
Profilins have also been identified as potential allergens in plant foods; 70–90 % of melon- and orange-allergic patients are sensitized to profilins. However, most food profilins have been described as minor allergens with sensitization rates below 50 %. Depending on the study, between 12 and 42 % of latex-allergic patients have been found to be sensitized to profilin (Santos and van Ree 2011).
5 Sensitization to Profilins
The high IgE cross-reactivity of profilins from different allergen sources (i.e., pollen and fruits) is based on the highly conserved three-dimensional structure of the molecules. Interestingly, sensitization to food profilins is restricted to pollen sensitized atopic individuals. IgE epitopes of profilins are dependent on the proper conformation of the allergens. Thus, antibodies cannot bind to denatured or structurally modified proteins. Profilins are heat labile and unstable in the presence of digestive enzymes (Hauser et al. 2010; Rodriguez-Perez et al. 2003).
Inhibition experiments revealed that pollen profilins could effectively inhibit IgE binding to food profilins. However, the opposite was only partially the case. These results, combined with the fact that profilins are quite susceptible to proteolytic degradation, suggest that pollen profilins are the primary sensitizers of profilin allergies. This hypothesis is further supported by studies, which have demonstrated a relation of IgE antibodies to birch and grass pollen profilins with IgE against profilins from hazelnut or various fruits of the Rosaceae family (e.g., strawberry Fra a 4, apple Mal d 4, cherry Pru av 4, almond Pru du 4, peach Pru p 4, or pear Pyr c 4) (Hauser et al. 2010; van Ree et al. 1995). In addition, association of birch and mugwort pollen allergies with reactions to celery or carrot and also the so-called ragweed-banana-melon syndrome were connected to profilin sensitization (Hauser et al. 2010).
In a study of 106 grass pollen-allergic children, including 50 sensitized to grass pollen panallergens and latex, a positive correlation between sensitization to the profilins Phl p 12 and Hev b 8 was reported; however, the authors did not find evidence for clinical relevance of this cross-reactivity (Casquete-Roman et al. 2012). Despite the fact that profilins are highly cross-reactive in vitro, the clinical relevance of this cross-reactivity is controversial. Thus, only some of the profilin-sensitized patients develop allergic symptoms (Matricardi et al. 2016). These allergic reactions are usually mild among pollen-allergic patients, and only in rare cases of food-allergic individuals may severe allergic reactions be triggered (Hauser et al. 2010; Santos and van Ree 2011).
To date, 43 allergenic profilins have been identified in pollen, plant foods, and latex. In Germany, 10–15 % of pollen-allergic patients display sensitization toward profilins; worldwide, the prevalence of profilin sensitization varies from 5 to 40 %. These sensitization rates can be considerably higher with some allergenic food profilins.
6 Structure and Function of Polcalcins
In addition to parvalbumin (Kühn et al. 2012), polcalcins (monomer 8–9 kDa) constitute the majority of allergenic calcium-binding proteins. However, calcium-binding allergens have not only been identified in food and pollen but also in house dust mite, cockroach, and cattle. Consistent with the name, the expression of polcalcins is restricted to pollen. Characteristic to polcalcins is the EF-hand domain, a helix-loop-helix structure which can bind calcium thus forming the dominant structural motif of the mostly alpha-helical proteins. Binding of calcium changes and stabilizes the structure of polcalcins, which concomitantly increases the interactions with IgE antibodies (Kühn et al. 2012). Based on the number of EF-hand motifs, at least three types of polcalcins can be distinguished:
-
1.
Allergens with two calcium-binding domains (i.e., alder Aln g 4, ragweed Amb a 9, mugwort Art v 5, or birch Bet v 4)
-
2.
Allergens with three calcium-binding domains (i.e., ragweed Amb a 10, and birch Bet v 3)
-
3.
Allergens with four calcium-binding domains (i.e., Jun o 4 from prickly juniper or Ole e 8 from olive)
Moreover, polcalcins may occur as monomeric units (Bet v 4) or form dimeric structures (i.e., Phl p 7 from timothy grass or Che a 3 from white goosefoot) (Verdino et al. 2008). Recently, it has been reported that also the per se monomeric Bet v 4 can form reversible dimers or oligomers in a temperature-dependent manner (Magler et al 2010). However, the exact biological role of polcalcins still remains elusive. Due to their localization in pollen and their ability to regulate intracellular calcium levels, it has been suggested that polcalcins play a crucial role in pollen tube outgrowth (Wopfner et al. 2007).
7 Relevance of Polcalcins
For calcium-binding proteins, two distinct conformations can be distinguished:
-
The closed calcium-free (apo)structure
-
The open calcium-bound (holo)form
The latter has been reported to be more stable and shows stronger IgE reactivity. Polcalcins are highly cross-reactive allergens with a sensitization prevalence ranging from 5 to 10 % among pollen-allergic patients (Hauser et al. 2010). Similar to profilins, the clinical relevance of polcalcin sensitization seems highly dependent on geographic factors as well as the allergen source itself. Thus, it has been reported that the sensitization rates to the polcalcins Art v 5 from mugwort and Amb a 9 and 10 from ragweed were, as expected, approximately 10 % in an Austrian cohort, but in an Italian population, reached almost 30 % (Wopfner et al. 2008).
Among all allergenic polcalcins, Phl p 7 from timothy grass pollen is the most cross-reactive molecule. Thus, it can be used as a marker to identify multiple pollen cross-reactivities. The increased IgE binding capacity of Phl p 7 could be a consequence of the dimeric structure of the allergen. This can be explained by the fact that monomeric polcalcins are very small proteins with a molecular weight of 8 kDa. Considering that an antibody epitope covers an area of approximately 1000 Å2 on the surface of a protein (Mirza et al. 2000), an effective IgE cross-linking by the simultaneous binding of multiple IgE antibodies on the surface of such a small protein seems unlikely. However, comparative IgE-binding studies of Phl p 7 dimers with other polcalcins such as monomeric Bet v 4 from birch pollen or the likewise dimeric Che a 3 from white goosefoot are lacking (Tinghino et al. 2002). To date, 15 allergenic polcalcins have officially been acknowledged by the WHO/IUIS allergen nomenclature subcommittee (www.allergen.org) (Fig. 3.3).
List of allergenic polcalcins acknowledged by the WHO/IUIS allergen nomenclature subcommittee (Photos were obtained from www.fotolia.com)
Polcalcins are Ca++-binding proteins, but their expression is restricted to pollen. As mentioned in detail above, the number of Ca++-binding motifs is used to distinguish three types of allergenic polcalcins. The allergens are highly cross-reactive, inducing sensitization rates between 5 and 10 % among pollen-allergic patients.
8 Diagnosis of Relevant Multi-Sensitizations to Pollen
As panallergens, polcalcins and profilins are responsible for multiple pollen sensitizations; profilins are additionally associated with cross-reactivities of pollen, plant foods and latex (Raulf-Heimsoth and Rihs 2011).
Problems in the specific diagnosis of pollen sensitizations are induced by both profilins and polcalcins because of their high degree of similarity as well as their potential to evoke clinically relevant cross-reactivities. Thus, they reduce the analytical specificity of allergen extracts and interfere with specific allergy diagnosis:
-
In skin prick tests, there can be a characteristic pattern of multiple sensitizations to a variety of botanically distinct or even unrelated pollen sources.
-
In individual cases, pollen extracts would lead to unexpected results (e.g., hazel and alder positive but birch negative skin prick test) suggesting a different context (as, for instance, Bet v 1-mediated cross-reactivity).
-
Concomitant sensitizations to profilins and polcalcins may induce positive test results in any of the tested pollen extracts (in skin prick tests as well as in specific IgE tests using allergen extracts).
-
Reactions to food plants with a high profilin content (i.e., melon, banana, citrus fruits, tropical fruits, cucumbers, or various vegetables) aside from the typical Bet v 1 homologous foods would serve as an additional indication of a profilin sensitization (Kleine-Tebbe et al. 2010).
In that event, it is recommended to test the sensitization to a (recombinant) member of either of the two panallergens, such as:
-
IgE specific to the timothy grass polcalcin Phl p 7 (recommended panallergen) or the birch polcalcin Bet v 4
-
IgE specific to the timothy grass profilin Phl p 12 or the birch pollen profilin Bet v 2 (both suitable as panallergens)
An affordable alternative is the simultaneous panallergen detection in specific IgE assays, which are available either as a combination of profilin/polcalcin from birch pollen (t221) or grass pollen (g214, ImmunoCAP, Thermo Fisher). However, this will not allow the discrimination between the two panallergens.
In conclusion, panallergens may cause multiple sensitizations against biologically unrelated allergen sources in skin prick tests as well as in specific IgE tests with allergen extracts. Frequently, these sensitizations remain without symptoms and are therefore considered irrelevant, although clinically relevant cross-reactivities may occur.
9 Component-Resolved Diagnosis of Panallergen Sensitizations
With a positive test result for a profilin, polcalcin, or both panallergens, neither skin prick tests nor IgE-based assays with allergen extracts allow a reliable determination of the allergen source. Specific allergy diagnosis with allergen extracts is impossible under those circumstances. Thus, for the exact determination of the sensitizing pollen source, species-specific marker allergens are mandatory (Fig. 3.4) for the correct extract selection for AIT.
Propeller model of cross-reactivity between pollen allergens. Propeller blades: species-specific, genuine marker allergens; propeller center: highly cross-reactive panallergens. In case of allergic sensitization to the panallergens profilin and/or polcalcin (propeller center), extract-based allergy diagnosis does not allow a precise determination of the allergen source. Tree, grass, and weed pollen sensitization can only be verified via specific sensitization tests (i.e., specific IgE determination) using genuine marker allergens
10 Clinical Relevance of Panallergens
Panallergen-allergic patients are usually only sensitized to the major allergens of the particular allergen source (i.e., Bet v 1 from birch or Phl p 1/Phl p 5 from timothy grass) and not the whole panel of major allergens from all allergen sources. Similarly, for extract-based diagnosis, clinical relevance is only indicated when the patients show appropriate symptoms. However, based on the pollen extracts available for the diagnosis of panallergens (profilin, polcalcin), this is very difficult to determine, since minor allergens are frequently underrepresented in commercial pollen extracts (Focke et al. 2009).
Persistent moderate symptoms during the whole pollen season could indicate a sensitization to panallergens. Conjunctival provocation tests with profilin-containing extracts (i.e., date pollen, ALK-Abelló, Spain) induce positive reactions in some of the affected patients (Tehrani et al. 2011). Moreover, a sensitization to panallergens can be an indication of the severity of the allergy.
Studies with children elucidated the typical sequence of allergic sensitization to various proteins of an allergen source. Allergic sensitization is triggered by a so-called initiator allergen (i.e., Phl p 1 for timothy grass). With progressing sensitization, additional allergens will be recognized by the immune system in a distinct order. First, the major allergens followed by the minor allergens of the source, i.e., grass pollen Phl p 4 and Phl p 5, followed by Phl p 2, Phl p 6, and Phl p 11; thereafter, sensitization to the panallergens Phl p 12 (profilin) and Phl p 7 (polcalcin) can be observed (Hatzler et al. 2012).
It has been demonstrated in a study on 891 pollen-allergic patients from Spain that sensitization to grass pollen profilin correlates with the severity of the allergic disease (Barber et al. 2008). With certain pollens, e.g., Chenopodium album (white goosefoot), extraordinarily high sensitization rates of 55 % and 46 % to profilin and polcalcin, respectively, have been reported (Barderas et al. 2004). Another study, investigating the sensitization rates to Che a 2, reported that an exceedingly high 81 % of the patients had IgE against the profilin allergen. Thus, it seems necessary to include both panallergens Che a 2 and 3 in the component-resolved determination of goosefoot allergy sensitization patterns (Nouri et al. 2012). Quite high sensitization rates (47 %) have also been reported for the pollen profilins of Russian thistle (Salsola kali Sal k 4), 33 % for redroot pigweed (Amaranthus retroflexus Ama r 2), and 64 % for date palm (Phoenix dactylifera Pho d 2) (Assarehzadegan et al. 2010; Asturias et al. 2005; Tehrani et al. 2011).
Profilins may represent clinically relevant major allergens of certain plant-derived foods. Although profilins may sporadically evoke severe allergic reactions, such as gastrointestinal anaphylaxis, nausea, pruritus, or dyspnea, allergic symptoms are usually restricted to the oropharyngeal region. This is in accordance with the known degradation of profilins by digestive enzymes. The apple profilin Mal d 4, for instance, loses its IgE-binding properties within 10 s of pepsin treatment (Ma et al. 2006). This could also explain the generally mild oropharyngeal allergic symptoms elicited by melon, where profilin has been described as a major allergen (Rodriguez-Perez et al. 2003). Although food processing affects the allergenicity of profilins, it has been reported that cooking diminishes but does not abolish IgE binding to the celery profilin Api g 4 (Ballmer-Weber et al. 2002). It may be that heat treatment initially destroys IgE epitopes of the Api g 4, but that the cooling process might lead to a partial renaturation. In a case report of lychee allergy anaphylaxis induced by profilin, either fresh or canned lychee fruits were of comparable potency. As profilin was the only detectable allergen in lychee, the severe reactions were explained by the significant amount of profilin in the fruits (Santos and van Ree 2011).
In a Spanish study, grass pollen-allergic patients sensitized to profilin were exposed to purified profilin from date palm pollen (Pho d 2) in oral provocation tests using amounts from 0.074 to 740 μg. The study demonstrated that these quantities induced mild to severe allergic reactions, the latter with as little as 7.4 μg of Pho d 2 (Alvarado et al. 2014). The authors concluded that a high grass pollen exposure would eventually lead to a broad sensitization to multiple grass pollen allergens and that these patients would then be at risk for profilin-associated food allergies. In individual cases, sufficient amounts of the allergen could be absorbed via the mucosa to lead not only to oropharyngeal but also more severe systemic reactions.
11 Extract Selection for Allergen Immunotherapy (AIT)
The rare patients who are sensitized exclusively to pollen panallergens or minor pollen allergens are probably not suitable for AIT. Thus, before selecting an AIT extract for patients with a history of profilin and/or polcalcin sensitization, one should determine the specific IgE levels to the primary pollen major allergens (Fig. 3.4) to complement allergen-specific diagnosis.
The extent to which pollen AIT is less promising in those patients has only been examined retrospectively (Schmid-Grendelmeier 2010), but has not yet been investigated prospectively. Consider, for example, a pollen-allergic patient who shows only weak skin prick test reactivity to birch pollen extracts: If there is no sensitization to the major birch pollen allergen Bet v 1 but only to the birch pollen profilin Bet v 2, birch pollen AIT would seem to be contraindicated. In Central Europe, such patients are usually sensitized to the grass pollen profilin Phl p 12, leading to cross-reactivity with Bet v 2.
To avoid the undue cost of incorrect extract selection, patients in Central Europe (e.g., Austria and Switzerland, possibly a consequence of the high local prevalence of profilin sensitization) are routinely tested for sensitization to profilins and polcalcins prior to any extract-based AIT. In case of positive results, further tests with the respective major pollen allergens are performed (Pfaar et al. 2014).
Multiple positive results in skin prick tests and/or specific IgE tests with pollen extracts are usually indicative of panallergen sensitization. Thus, it is highly recommended that one investigates the influence of panallergens by molecule-based diagnosis using purified, natural, or recombinant major and minor allergens (Schmid-Grendelmeier 2010).
In component-resolved diagnosis for the selection of pollen extracts for AIT in patients with panallergen sensitization, the major allergens include the following depending on the geographic region:
-
Bet v 1 (major birch pollen allergen: sensitization marker for birch, hazel, alder, beech, and oak pollen allergies)
-
Cup a 1 (major cypress pollen allergen, marker for sensitization to cypress pollen) or closely related
-
Jun a 1 (major mountain cedar pollen allergen, marker for sensitization to cedar pollen)
-
Ole e 1 (major olive pollen allergen: sensitization marker for olive and ash pollen allergies)
-
Phl p 1 and Phl p 5 (major grass pollen allergens: sensitization markers for grass and rye pollen allergies)
-
Art v 1 (major mugwort pollen allergen)
-
Amb a 1 (major ragweed pollen allergen)
12 Conclusions from a Clinical Perspective
Allergy diagnosis based on pollen extracts (skin prick tests, specific IgE tests) is impeded by the fact that, worldwide, 5–40 % of pollen-allergic patients are sensitized to the highly cross-reactive panallergens, profilin and polcalcin. Such sensitization/cross-reactivity patterns do not induce false-positive test results, but are usually clinically irrelevant. Only rarely does sensitization to profilins and polcalcins evoke clinically relevant allergic reactions, e.g., after the ingestion of profilin-rich foods such as melon, tomato, orange, or various tropical fruits.
Molecule-based diagnosis and specific IgE tests against single pollen allergens represent a targeted approach to determining sensitization to important major and minor allergens. The clinical relevance of such sensitization profiles needs to be carefully evaluated by linkage to the associated symptoms. In case of ambiguity, provocation tests are indicated to aid in selecting AIT extracts for pollen-allergic patients.
References
Alvarado MI, Jimeno L, De La Torre F, Boissy P, Rivas B, Lazaro M, Barber D. Profilin as a severe food allergen in allergic patients overexposed to grass pollen. Allergy. 2014;69(12):1610–6. Epub 2014/08/16.
Asero R, Tripodi S, Dondi A, Di Rienzo Businco A, Sfika I, Bianchi A, Candelotti P, Caffarelli C, Povesi Dascola C, Ricci G, Calamelli E, Maiello N, Miraglia Del Giudice M, Frediani T, Frediani S, Macrì F, Moretti M, Dello Iacono I, Patria MF, Varin E, Peroni D, Comberiati P, Chini L, Moschese V, Lucarelli S, Bernardini R, Pingitore G, Pelosi U, Tosca M, Cirisano A, Faggian D, Plebani M, Verga C, Matricardi PM; Italian Pediatric Allergy Network (I-PAN). Prevalence and Clinical Relevance of IgE Sensitization to Profilin in Childhood: A Multicenter Study. Int Arch Allergy Immunol. 2015;168:25–31.
Assarehzadegan MA, Amini A, Sankian M, Tehrani M, Jabbari F, Varasteh A. Sal k 4, a new allergen of Salsola kali, is profilin: a predictive value of conserved conformational regions in cross-reactivity with other plant-derived profilins. Biosci Biotechnol Biochem. 2010;74:1441–6.
Asturias JA, Ibarrola I, Fernandez J, Arilla MC, Gonzalez-Rioja R, Martinez A. Pho d 2, a major allergen from date palm pollen, is a profilin: cloning, sequencing, and immunoglobulin E cross-reactivity with other profilins. Clin Exp Allergy. 2005;35:374–81.
Balla T. Phosphoinositides: tiny lipids with giant impact on cell regulation. Physiol Rev. 2013;93:1019–137.
Ballmer-Weber BK, Hoffmann A, Wuthrich B, Luttkopf D, Pompei C, Wangorsch A, Kastner M, Vieths S. Influence of food processing on the allergenicity of celery: DBPCFC with celery spice and cooked celery in patients with celery allergy. Allergy. 2002;57:228–35.
Barber D, de la Torre F, Feo F, Florido F, Guardia P, Moreno C, Quiralte J, Lombardero M, Villalba M, Salcedo G, Rodriguez R. Understanding patient sensitization profiles in complex pollen areas: a molecular epidemiological study. Allergy. 2008;63:1550–8.
Barderas R, Villalba M, Pascual CY, Batanero E, Rodriguez R. Profilin (Che a 2) and polcalcin (Che a 3) are relevant allergens of Chenopodium album pollen: isolation, amino acid sequences, and immunologic properties. J Allergy Clin Immunol. 2004;113:1192–8.
Casquete-Roman E, Rosado-Gil T, Postigo I, Guisantes JA, Fernandez M, Torres HE, Martinez-Quesada J. Profilin cross-reactive panallergen causes latex sensitization in the pediatric population allergic to pollen. Ann Allergy Asthma Immunol. 2012;109:215–9.
Focke M, Marth K, Valenta R. Molecular composition and biological activity of commercial birch pollen allergen extracts. Eur J Clin Invest. 2009;39:429–36.
Hatzler L, Panetta V, Lau S, Wagner P, Bergmann RL, Illi S, Bergmann KE, Keil T, Hofmaier S, Rohrbach A, Bauer CP, Hoffman U, Forster J, Zepp F, Schuster A, Wahn U, Matricardi PM. Molecular spreading and predictive value of preclinical IgE response to Phleum pratense in children with hay fever. J Allergy Clin Immunol. 2012;130:894–901 e5.
Hauser M, Roulias A, Ferreira F, Egger M. Panallergens and their impact on the allergic patient. Allergy Asthma Clin Immunol. 2010;6:1.
Kleine-Tebbe J, Balmer-Weber B, Breiteneder H, Vieths S. Bet v 1 und Homologe – Verursacher der Baumpollenallergie und birkenpollenassoziierter Kreuzreaktionen. Allergo J. 2010;19:462–4.
Kühn A, Radauer C, Swoboda I, Kleine-Tebbe J. Molekulare Diagnostik der Fischallergie: Parvalbumine und andere Allergene. Allergo J. 2012;21:16–8.
Le LQ, Mahler V, Lorenz Y, Scheurer S, Biemelt S, Vieths S, Sonnewald U. Reduced allergenicity of tomato fruits harvested from Lyc e 1-silenced transgenic tomato plants. J Allergy Clin Immunol. 2006;1180:1176–83.
Ma Y, Zuidmeer L, Bohle B, Bolhaar ST, Gadermaier G, Gonzalez-Mancebo E, Fernandez-Rivas M, Knulst AC, Himly M, Asero R, Ebner C, van Ree R, Ferreira F, Breiteneder H, Hoffmann-Sommergruber K. Characterization of recombinant Mal d 4 and its application for component-resolved diagnosis of apple allergy. Clin Exp Allergy. 2006;36:1087–96.
Magler I, Nuss D, Hauser M, Ferreira F, Brandstetter H. Molecular metamorphosis in polcalcin allergens by EF-hand rearrangements and domain swapping. FEBS J. 2010;277:2598–610.
Matricardi PM, Kleine-Tebbe J, Hoffmann HJ, Valenta R, Hilger C, Hofmaier S, Aalberse RC, Agache I, Asero R, Ballmer-Weber B, Barber D, Beyer K, Biedermann T, Biló MB, Blank S, Bohle B, Bosshard PP, Breiteneder H, Brough HA, Caraballo L, Caubet JC, Crameri R, Davies JM, Douladiris N, Ebisawa M, Eigenmann PA, Fernandez-Rivas M, Ferreira F, Gadermaier G, Glatz M, Hamilton RG, Hawranek T, Hellings P, Hoffmann-Sommergruber K, Jakob T, Jappe U, Jutel M, Kamath SD, Knol EF, Korosec P, Kuehn A, Lack G, Lopata AL, Mäkelä M, Morisset M, Niederberger V, Nowak-Wezgrzyn AH, Papadopoulos NG, Pastorello EA, Pauli G, Platts-Mills T, Posa D, Poulsen LK, Raulf M, Sastre J, Scala E, Schmid JM, Schmid-Grendelmeier P, van Hage M, van Ree R, Vieths S, Weber R, Wickman M, Muraro A, Ollert M. EAACI molecular allergology user’s guide. Pediatr Allergy Immunol. 2016;27 Suppl 23:1–250.
Mirza O, Henriksen A, Ipsen H, Larsen JN, Wissenbach M, Spangfort MD, Gajhede M. Dominant epitopes and allergic cross-reactivity: complex formation between a Fab fragment of a monoclonal murine IgG antibody and the major allergen from birch pollen Bet v 1. J Immunol. 2000;165:331–8.
Nouri HR, Sankian M, Vahedi F, Afsharzadeh D, Rouzbeh L, Moghadam M, Varasteh A. Diagnosis of Chenopodium album allergy with a cocktail of recombinant allergens as a tool for component-resolved diagnosis. Mol Biol Rep. 2012;39:3169–78.
Pfaar O, Bachert C, Bufe A, Buhl R, Ebner C, Eng P, Friedrichs F, Fuchs T, Hamelmann E, Hartwig-Bade D, Hering T, Huttegger I, Jung K, Klimek L, Kopp MV, Merk H, Rabe U, Saloga J, Schmid-Grendelmeier P, Schuster A, Schwerk N, Sitter H, Umpfenbach U, Wedi B, Wöhrl S, Worm M, Kleine-Tebbe J. Guideline on allergen-specific immunotherapy in IgE-mediated allergic diseases – S2k Guideline of the German Society for Allergology and Clinical Immunology (DGAKI), the Society for Pediatric Allergy and Environmental Medicine (GPA), the Medical Association of German Allergologists (AeDA), the Austrian Society for Allergy and Immunology (ÖGAI), the Swiss Society for Allergy and Immunology (SGAI), the German Society of Dermatology (DDG), the German Society of Oto-Rhino-Laryngology, Head and Neck Surgery (DGHNO-KHC), the German Society of Pediatrics and Adolescent Medicine (DGKJ), the Society for Pediatric Pneumology (GPP), the German Respiratory Society (DGP), the German Association of ENT Surgeons (BV-HNO), the Professional Federation of Paediatricians and Youth Doctors (BVKJ), the Federal Association of Pulmonologists (BDP) and the German Dermatologists Association (BVDD). Allergo J Int. 2014;23:282–319. doi:10.1007/s40629-014-0032-2.
Raulf-Heimsoth M, Rihs HP. Latexallergene: Sensibilisierungsquellen und Einzelallergenprofile erkennen. Allergo J. 2011;20:241–3.
Rodriguez-Perez R, Crespo JF, Rodriguez J, Salcedo G. Profilin is a relevant melon allergen susceptible to pepsin digestion in patients with oral allergy syndrome. J Allergy Clin Immunol. 2003;111:634–9.
Santos A, Van Ree R. Profilins: mimickers of allergy or relevant allergens? Int Arch Allergy Immunol. 2011;155:191–204.
Schmid-Grendelmeier P. Recombinant allergens. For routine use or still only science? Hautarzt. 2010;61:946–53.
Tanaka M, Shibata H. Poly(L-proline)-binding proteins from chick embryos are a profilin and a profilactin. Eur J Biochem. 1995;151:291–7.
Tehrani M, Sankian M, Assarehzadegan MA, Falak R, Noorbakhsh R, Moghadam M, Jabbari F, Varasteh A. Identification of a new allergen from Amaranthus retroflexus pollen, Ama r 2. Allergol Int. 2011;60:309–16.
Tinghino R, Twardosz A, Barletta B, Puggioni EM, Iacovacci P, Butteroni C, Afferni C, Mari A, Hayek B, Di Felice G, Focke M, Westritschnig K, Valenta R, Pini C. Molecular, structural, and immunologic relationships between different families of recombinant calcium-binding pollen allergens. J Allergy Clin Immunol. 2002;109:314–20.
Valenta R, Duchene M, Pettenburger K, Sillaber C, Valent P, Bettelheim P, Breitenbach M, Rumpold H, Kraft D, Scheiner O. Identification of profilin as a novel pollen allergen; IgE autoreactivity in sensitized individuals. Science. 1991;253:557–60.
Vallverdu A, Garcia-Ortega P, Martinez J, Martinez A, Esteban MI, de Molina M, Fernandez-Tavora L, Fernandez J, Bartolome B, Palacios R. Mercurialis annua: characterization of main allergens and cross-reactivity with other species. Int Arch Allergy Immunol. 1997;112:356–64.
van Ree R, Fernandez-Rivas M, Cuevas M, van Wijngaarden M, Aalberse RC. Pollen-related allergy to peach and apple: an important role for profilin. J Allergy Clin Immunol. 1995;95:726–34.
Verdino P, Barderas R, Villalba M, Westritschnig K, Valenta R, Rodriguez R, Keller W. Three-dimensional structure of the cross-reactive pollen allergen Che a 3: visualizing cross-reactivity on the molecular surfaces of weed, grass, and tree pollen allergens. J Immunol. 2008;180:2313–21.
Witke W. The role of profilin complexes in cell motility and other cellular processes. Trends Cell Biol. 2004;14:461–9.
Wopfner N, Dissertori O, Ferreira F, Lackner P. Calcium-binding proteins and their role in allergic diseases. Immunol Allergy Clin North Am. 2007;27:29–44.
Wopfner N, Gruber P, Wallner M, Briza P, Ebner C, Mari A, Richter K, Vogel L, Ferreira F. Molecular and immunological characterization of novel weed pollen pan-allergens. Allergy. 2008;63(7):872–81.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wallner, M., Ferreira, F., Hofer, H., Hauser, M., Mahler, V., Kleine-Tebbe, J. (2017). The Concept of Pollen Panallergens: Profilins and Polcalcins. In: Kleine-Tebbe, J., Jakob, T. (eds) Molecular Allergy Diagnostics. Springer, Cham. https://doi.org/10.1007/978-3-319-42499-6_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-42499-6_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42498-9
Online ISBN: 978-3-319-42499-6
eBook Packages: MedicineMedicine (R0)