Abstract
An acute lung injury represents a continuum of injury that may arise from a number of primary insults. When it is present, it may progress due to the trauma from mechanical ventilation, a finding that has led to an intense debate over the optimal ventilator management. Moreover, it has been demonstrated that mechanical ventilation per se, even in the absence of a preexisting lung injury, may lead to the development of ventilator-induced lung injury (VILI). The association between positive pressure mechanical ventilation and lung injury has fostered the concepts of barotrauma, volutrauma, atelectrauma, and biotrauma and led to the clinical development of “lung-protective ventilation,” which has led to a significant improvement in outcomes. Several theories have attempted to explain the mechanistic basis of VILI. The stretched-pore hypothesis suggested that vascular distention may open the endothelial intercellular junctions, thus increasing fluid and protein leak and leading to a compromised lung function. The stress failure hypothesis proposes that pressure-induced tensile failure of capillary endothelium and basement membrane may result in hemorrhage and fluid leak. The stretch-recoil hypothesis introduced the concept that active cellular components are involved in the development of VILI. In the current chapter, ventilator-induced lung injury is examined as it relates to the pathophysiological changes beyond direct airway trauma. The role of lung-related factors such as stress, strain, and lung inhomogeneity will be examined, as well as extra-parenchymal factors and factors more directly related to mechanical ventilation (such as tidal volume, driving pressure, respiratory rate, inspiratory-to-expiratory ratio and flow). The recently proposed, unifying theory of mechanical power will also be presented and discussed.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
13.1 Introduction
The vast majority of critically ill patients undergo invasive mechanical ventilation (MV) during their stay in the intensive care unit, and patients with ARDS are almost invariably managed by invasive mechanical ventilation. Despite extensive research over nearly half a century, no effective pharmacological therapies exist for ARDS, and supportive care with mechanical ventilation remains the cornerstone of treatment [1]. Indeed, mechanical ventilation, per se, does not substitute the function of the lungs: indeed, it is a substitute for the activity of respiratory muscles. Moreover, mechanical ventilation is a procedure that aims to improve the gas exchange, and, since it does not act either on the etiology or on the pathophysiology of ARDS, it is a measure to buy time for healing to take place [2]. On the other side, mechanical ventilation is not devoid of side effects and, namely, the hemodynamic instability secondary to the increased intrathoracic pressures and the mechanical trauma to the lung structure. Indeed, mechanical ventilation can further damage the lung, activating a biological inflammatory response and promoting the development of the so-called ventilator-induced lung injury (VILI). The present chapter will focus on the latter aspect, i.e., VILI. The classic distinction among factors related to the lung parenchyma, factors related to the mechanical ventilator, and extrapulmonary factors will be employed to classify the causes of VILI. The recently introduced theory of mechanical power, as a unifying hypothesis for all the mechanical ventilator-associated causes, will also be presented and discussed.
13.2 The Concept of VILI
VILI arises from repeated application of high mechanical forces that either directly tear a weak tissue or initiate a signaling process that culminates in a pro-inflammatory state [3], in the context of an altered lung and in the presence of extrapulmonary factors which may potentially increase the damage. Soon after the times in which invasive mechanical ventilation was effectively introduced as a supportive therapy, i.e., the 1952 polio epidemic in Denmark, the potential harm from mechanical ventilation was noted and started to raise concerns, as the term “respirator lung syndrome” [4] was used to label the injury observed in ventilated patients. It was then discovered how mechanical ventilation itself could cause a structural damage to the lung, characterized by diffuse alveolar infiltrates and hyaline membranes that were found on postmortem examination [5], although the major factor causing injury was thought to be the high fractional concentrations of oxygen used in many ventilated patients.
Webb and Tierney [6] conducted one of the first comprehensive studies in intact animals, unambiguously demonstrating that mechanical ventilation can cause pulmonary edema. In their seminal investigation, the authors ventilated rats with very high peak airway pressures (and therefore overdistention) and zero positive end-expiratory pressure (PEEP). Hypoxemia developed in the animals, and postmortem examination revealed perivascular and alveolar edema. Edema did not develop in animals that underwent ventilation with the same peak airway pressure but with the addition of a PEEP of 10 cm of water, showing an interaction between overdistention and low end-expiratory lung volume with respect to lung injury.
Although the term used throughout this chapter is VILI, the mechanisms of injury are related to factors which can also occur during spontaneous ventilation. Indeed, in their proof-of-concept investigation, Mascheroni et al. [7] injected sodium salicylate into the cisterna magna of spontaneously breathing, otherwise healthy sheep, causing a marked increase in minute ventilation and alveolar overdistention with each breath. All the animals developed hypoxemia, along with an increased respiratory elastance and severe morphologic pulmonary alterations at postmortem examination, consistent with lung injury commonly observed during mechanical ventilation. Indeed, such effects did not develop in animals that were similarly treated with sodium salicylate, but underwent controlled ventilation which prevented unsafe lung stretching. Hence, a better term than VILI might be ventilation-induced lung injury. Nevertheless, experimental evidence provides consistent laboratory observations and clinical trials regarding the factors which, alone or in conjunction, lead to the development of VILI. As a consequence of adverse patterns of ventilation, both airway and alveolar injury occur, causing a damage that prevails in anatomically dependent zones. Indeed, VILI can resemble ARDS itself, and it is often difficult to diagnose in humans because its appearance can be similar to the underlying disease for which MV was instituted [8].
The consequences of our better understanding of the mechanisms related to VILI are significant in terms of lives saved. Indeed, the incidence and mortality of ARDS have declined steadily over the past decades. A pivotal study by Li et al. [9] found that the decline in the incidence was primarily due to a decrease in nosocomial ARDS. Moreover, as documented by the first trial of extracorporeal membrane oxygenation, the mortality rate of patients with ARDS was close to 90% in the late 1970s [10]. Mortality in studies of ARDS has then fallen impressively from 48 to 59% between 1983 and 1991 to 25–26% since 2000 [11], and data from patients enrolled in the ARDS Network randomized controlled trials document a further significant trend toward improvement in mortality during the following period [12]. It is tempting to believe that, among the several major advances in critical care practice, the widespread use of lung-protective ventilation and a reduced incidence of VILI may significantly have contributed to this trend. Indeed, although it still remains unclear how inflammatory mediators exert their detrimental effects on distal organs, experimental studies and clinical trials in ARDS have shown that the application of protective ventilator strategies is associated with decreased serum cytokine levels [13], decreased extrapulmonary organ dysfunction [14], and decreased mortality [15].
13.3 Factors Related to Development of VILI
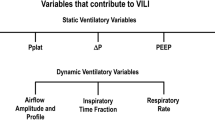
For an injury secondary to mechanical ventilation to develop, an interaction among different factors need to occur, in particular between what the ventilator delivers to the lung parenchyma and how the lung parenchyma accepts it, that is, the combined action of mechanical forces, lung pathoanatomy, and non-ventilatory characteristics [16]. In other words, one can identify factors related to the mechanical ventilator (i.e., the way that pressures and volumes are delivered), as well as factors related to the lung (such as decreased lung dimensions, increased lung inhomogeneity, presence of stress risers, and cyclic collapse and decollapse). Dynamic characteristics, such as respiratory frequency, flow rate, and strain rate, have recently been emphasized as key determinants of whether the “static” variables may or may not inflict injury [17, 18]. In addition to direct structural damage, mechanical stretch can trigger a complex array of inflammatory mediators associated with activation of the immune response, further adding to injury and potentially causing remote injury to other organs, which may result in multiple system organ dysfunction and ultimately in death; this is termed “biotrauma” [19]. Moreover, extrapulmonary factors such as perfusion, pH, gas tensions, and temperature may play a role in the development of VILI.
13.4 Lung-Dependent Factors of VILI: Stress, Strain, and Stress Raisers
The logical sequence of events in progression of VILI caused by inappropriate mechanical ventilation would seem to be mechanical damage to pulmonary tissue caused by excess stress- induced strain as the primary injury, followed by biotrauma in response to physical damage caused by excessive strain [20, 21]. Gattinoni’s group applies engineering concepts as a novel approach to analyze the pathologic impact of mechanical ventilation on normal pulmonary tissue and to determine what adjustments in the mechanical breath can block progressive acute lung injury and thus reduce ARDS incidence [22, 23]. In their most recent paper, their goal was to identify the volumetric threshold for VILI and determine if PEEP was directly or indirectly protective in normal pigs [24]. Unlike many experiments in which the role of tidal volume (TV), plateau pressure (P plat), and PEEP were correlated with VILI, the authors analyzed the mechanism of VILI under two main categories with two respective subcategories: (1) global strain (dynamic and static strain) and (2) energy load (dynamic and static) within the volumetric constraints of the lung, which is the inspiratory capacity.
Strain is the response to an applied stress, which in the case of the lung are TV and PEEP. Thus, global strain is the result of TV + PEEP volume. Dynamic strain is the amount the volume change caused by the TV over the functional residual capacity (FRC), and static strain is the volume change from PEEP over the FRC. Global energy load is a combination of the static component due to PEEP (conceptually equivalent to potential energy) and the dynamic cyclic component due to the driving pressure, defined as TV above PEEP (conceptually equivalent to kinetic energy).
Stress and strain are frequently used terms to describe the effect of external force acting on a subject. Stress is defined as the internal distribution of forces per unit of area of a specific material by an external force. The resulting change in shape of the material by the stress applied is called strain. Lung stress describes the distribution of forces due to PEEP and tidal volume, whereas strain describes the resulting change in lung volume. Calculations of strain require measurements of FRC. Traditional FRC measurements needed tracer gases such as helium, and expensive and bulky equipment [25] and modern device use the nitrogen multiple breath washout technique [26]. For the calculation of stress, the specific elastance should be known, or transpulmonary pressure measurements are required.
Ultimately, this mechanical insult results in the release of inflammatory mediators that exacerbate the primary mechanical damage resulting in a secondary biotrauma as mentioned above [27]. These studies are supported by physiological evidence that high static strain, which should be sufficient to cause overdistension-induced tissue damage, is benign unless this strain is dynamic [28]. However, if PEEP is reduced, thereby creating excessive dynamic strain, significant lung damage will occur at the identical peak static strain. Thus, it appears that dynamic strain, or atelectrauma, is the primary mechanical mechanism of injury to the pulmonary parenchyma. Volutrauma is also important because it can cause stress failure in small airways leading to pneumothoraces, but it does not cause pulmonary edema or histopathology to the pulmonary parenchyma.
More recently, another mechanical VILI mechanism has been identified. Evidence has shown that the damage to the pulmonary parenchyma can be caused by heterogeneous ventilation, which occurs at the junction between collapsed or edema-filled alveoli and air-inflated alveoli [29]. This heterogeneity causes stress concentrators that can significantly magnify the amount of alveolar and alveolar duct strain for any given stress and thus appears to be another mechanism of mechanical injury to the pulmonary tissue [30]. The main pathological cause for both heterogeneous ventilation and altered alveolar and small airway mechanics is airway flooding with edema fluid and altered surfactant function. Ventilator-induced loss of surfactant function exacerbates edema formation [31]. This leads to alveolar instability, which increments in vascular permeability, causing more edema and deactivating more surfactant in a cycle that repeats until established ARDS is recognized [32]. However, if a mechanical breath can be preemptively applied to maintain homogeneous lung ventilation (eliminate stress concentrators) and prevent alveolar collapse and reopening during ventilation (eliminate dynamic strain), it would ameliorate all components of the pathological tetrad and theoretically reduce ARDS incidence. Thus, physiological evidence suggests that progressive VILI may be blocked by applying a preemptive mechanical breath directed to maintain homogeneous lung inflation and not allowing alveoli to collapse during expiration.
13.5 Ventilator-Dependent Factors
It is now known, in general terms, that the mechanisms of VILI are alveolar overdistension (volutrauma), alveolar instability leading to alveolar collapse and reopening with each breath (atelectrauma), and the secondary inflammation caused by these mechanical injuries which is known as biotrauma [9].
Times ago, Lachmann [33] proposed that the optimal lung-protective strategy would be to “open the lung and keep it open.” He hypothesized that heterogeneous lung inflation, which is a hallmark of ARDS pathology, plays a major role in driving mechanical ventilation-induced progressive acute lung injury. The corollary to this hypothesis is that keeping the lung open would result in a homogeneously ventilated lung, minimizing VILI and reducing ARDS mortality. If the approach of opening the ARDS lung and keeping it open can significantly reduce injury, then protective mechanical ventilation should be applied early in patients at a high risk of developing ARDS, in an attempt to “never let the lung collapse” and significantly reduce ARDS incidence [34]. As we will see in the next paragraphs, barotrauma, volutrauma, atelectrauma, and biotrauma are considered as undisputable truth and represent the background for the development and universal acceptance of the so-called lung-protective strategy.
13.5.1 Barotrauma and Volutrauma
Barotrauma was the first to be recognized as a form of stress at rupture, leading to pneumothorax, pneumoperitoneum, pneumomediastinum, and subcutaneous emphysema [35]. Although most frequently encountered in patients with the ARDS, it can occur in any patient receiving mechanical ventilation [14]. In addition, barotrauma can occur in patients with a wide range of underlying pulmonary conditions (i.e., asthma, chronic obstructive pulmonary disease, interstitial lung disease, pneumocystis pneumonia). In clinical medicine, barotrauma is used to describe the manifestations of extra-alveolar air during mechanical ventilation. Early descriptions of barotrauma refer to rupture of the lung after forceful exhalation against a closed glottis [27]. Although nonmechanically ventilated patients may have barotrauma, most cases occur in patients receiving mechanical ventilation.
The clinical presentation can vary, ranging from absent symptoms with the subtle radiographic findings of pulmonary (or perivascular) interstitial emphysema to respiratory distress or cardiac arrest due to a large tension pneumothorax [36]. Other manifestations include subcutaneous emphysema, pneumopericardium, pneumomediastinum, and even pneumoperitoneum, singly or in combination. Barotrauma was once the most frequent and easily recognized complication of mechanical ventilation. It is now evident, however, that barotrauma represents only one of the mechanisms underlying the broad category of VILI. As the term suggests, the lung injury associated with barotrauma is mediated by increased alveolar pressures.
It is important to recognize that lung involvement in persons with ARDS is heterogeneous and that some portions of the lungs are more adversely affected than others. This involvement can lead to misdistribution of mechanically delivered tidal volume, with some alveoli subjected to more distention than others. Pressures between adjacent alveoli may initially equilibrate, but alveolar pressures eventually increase, creating a pressure gradient between the alveoli and adjacent sheath. This gradient may result in rupture of the alveoli adjacent to the perivascular sheath and proximal dissection into the mediastinum (i.e., interstitial emphysema) [37]. In this circumstance, alveolar air is further decompressed by dissecting along lines of least resistance. These pathways include subcutaneous tissues, where the air produces subcutaneous emphysema, or along tissue planes, resulting in pneumopericardium, pneumoperitoneum, or subpleural air cysts. In the mediastinum, air can track along tissue planes, creating a pneumomediastinum, whereas increased pressures that rupture through the mediastinal pleura produce a pneumothorax. This is the most dreaded manifestation of barotrauma, and continued accumulation of air during mechanical ventilation can progress to a tension pneumothorax, sometimes with catastrophic consequences [38]. In view of the preceding description, alveolar overdistention is the key element in the development of barotrauma. In this sense, “barotrauma” is a misnomer, because the term suggests the presence of elevated pressures in its pathogenesis. Current concepts suggest that high tidal volume ventilation produces the alveolar disruption that triggers the aforementioned chain of events.
Therefore, VILI seen with high tidal volume is most accurately termed “volutrauma” [3], and it has been the basis for recent clinical trials that have established a low tidal volume approach to mechanical ventilation. On the other hand, transalveolar pressure, a measure of alveolar distention, provides another indication of the risk of barotrauma. The concept is the same, with overdistended alveoli leading to disruption in the alveolar epithelium and decompression of air as previously outlined. Although there has been some debate about the primary force that causes injury, both volume and pressure are two sides of the same coin – the transpulmonary pressure, the difference between airway pressure (P aw) and pleural pressure (P pl) [39]. In fact, the airway pressure is the pressure required to distend to the same extent not only the lung but also the chest wall. When the chest wall is free to expand, the pleural pressure is relatively low but high airway pressures are now associated with high transpulmonary pressures that may lead to a lung structural damage. In other words, for a given airway pressure, the development of VILI will depend on the resulting transpulmonary pressure. Chiumello et al. [20] recently demonstrated that a specific lung elastance is present in subjects with healthy lungs as well as in patients with ARDS. This means that even during lung injury, barotraumas (stress) and volutrauma (strain) bear the same constant relationship observed in normal subjects. The distinction between volutrauma and barotrauma then vanishes where at the cellular level, stretching the lung beyond its capacity ruptures alveolar cell membranes [40], and the resulting cell death induces inflammation. Moreover, subtler injuries to the cytoskeleton or extracellular matrix trigger inflammation through intracellular signals [41].
13.5.2 Atelectrauma and PEEP Effects
The second mechanism of injury, cyclic changes in non-aerated lung, was deduced from the observation of lung injury during ventilation with low end-expiratory lung volume (EELV) or in the absence of PEEP. In this case, the mechanisms at the cellular level are less clear. Air bubbles flowing through a collapsed or fluid-filled airway might induce damage to the epithelium by VILI consists of tissue damage and a biological response resulting from the application of inappropriate mechanical forces to the lung parenchyma [42].
Parenchymal stability resulting from the interplay of respiratory parameters such as tidal volume, PEEP, or respiratory rate can explain the results of different clinical trials and experimental studies that do not fit with the classic barotraumas/volutrauma model. A consequence of low EELV can be a heterogeneous lung where that the forces exerted on alveolar walls or septa in the interfaces between collapsed and aerated lung tissues can be amplified, leading to cell injury [43]. The application of PEEP is almost invariably associated with a decrease in VILI in different experimental models of lung injury, such as high TV ventilation or surfactant depletion [44, 45]. The focus of investigative attention regarding VILI has been on the individual tidal cycle – as defined by PEEP and tidal volume. However, it stands to reason that the number of damaging cycles delivered per unit time (closely correlated with minute ventilation, independently of mode) would accentuate the injury inflicted by the individual tidal cycle [46].
PEEP tends to reduce the number of lung units placed at high risk by critical junctional interfaces between expanding and reluctantly expanding tissues. For the same tidal volume, PEEP also elevates the mean airway pressure and with it the average tissue stress. In the absence of compensatory recruitment or reduction in tidal volume, PEEP therefore also tends to increase right ventricular afterload. Without a simultaneous reduction in driving pressure, raising PEEP will place the lung at higher risk for stretch-related injury. Tidal volume itself may not injure the ventilated lung, but rather, the causative variable relates to the ratio of the tidal volume to the capacity of the lung to accept it [47]. The transalveolar pressure and the swings of transalveolar pressure (transalveolar driving pressure) determine the damaging energy forces imparted to delicate tissue [48].
Experimental designs combining high PEEP with low TV make it impossible to clarify the contributions of each factor to the outcome. In intact lungs PEEP reduces VILI. One study showed that adding PEEP in intact rats ventilated with very high TV could reduce injury [44], and a randomized trial showed in patients without lung injury that ventilation with PEEP did not worsen outcome, but improved oxygenation and decreased the risk of ventilator-associated pneumonia [49]. The effect of TV on healthy lungs is also controversial. A classic experiment from Mascheroni and colleagues [7] demonstrated that, even in spontaneously breathing animals, chemically induced hyperventilation could trigger substantial lung damage. This work highlights the importance of tissue deformation, represented by increased transpulmonary pressures, even during negative pressure ventilation (absence of high alveolar pressure, more homogeneous inflation).
Low EELV has proved safe in both animals and patients, and this approach has sometimes been termed permissive atelectasis. In a recent study using an isolated lung model, Fanelli and colleagues [50] demonstrated that permissive atelectasis caused the same amount of lung injury as the open lung strategy and only subtle differences in apoptosis and ultrastructural changes favoring the open lung strategy. In the clinical setting, mortality rates in descriptive studies for patients managed with a low-pressure strategy are similar to those in clinical trials [51]. Taken together, these data contradict the volutrauma/atelectrauma model, suggesting that other mechanisms could be responsible for VILI.
13.5.3 Biotrauma
The concepts of VILI already discussed are based on the biophysical injury induced when applied forces cause mechanical destruction of the anatomical lung structure. Alveolar overdistention, lung strain (the associated deformation of a structure to an external load in relation to its resting state), and atelectasis are key inciting features of VILI. However, numerous studies have demonstrated that there can be a more subtle form of injury, with release of various mediators into the lung, pulmonary recruitment of leukocytes, and local initiation of inflammatory processes. This biological response to mechanical forces has been called “biotrauma” [19, 27]. The biotrauma hypothesis postulates that the circulating mediators can cause local lung injury, and if they translocate into the systemic circulation, they may lead to distal organ dysfunction and death [52]. One of the pioneristic papers that investigated the effects of mechanical ventilation in an animal model [13] found that isolated nonperfused rat lungs ventilated for 2 h with large tidal volumes without PEEP had large increases in lavage concentrations of tumor necrosis factor (TNF)-a, interleukin (IL)-1b, IL-6, and macrophage inflammatory peptide 2. The potential for ventilation-induced inflammation in humans was examined in patients with ARDS who were randomized to receive traditional or lung-protective ventilation [14]. BAL and plasma concentrations of several pro-inflammatory cytokines were lower in patients receiving protective ventilation, as were other indices of plasma and alveolar fluid inflammation, compared with patients receiving traditional tidal volumes and lower PEEP.
The main concept of these observations is that the healthy lung is a homogeneously ventilated organ that is structurally resistant to mechanical damage during ventilation. The shared walls of each alveolus with a two-fiber support system (i.e., the axial system anchored to the hilum and extending into the alveolar ducts and the peripheral system anchored to the visceral pleura distending into the central portion of the lung) are structurally very stable and resistant to either overdistension or collapse. As mentioned before, the concept of this alveolar interdependence was first introduced by Mead [43] and describes the structural mechanisms by which alveoli resist either collapse or hyperinflation. In addition, they also demonstrated how heterogeneous collapse of alveoli created stress concentrators in the areas between open and collapsed alveoli. These stress concentrators greatly amplify the mechanical damage to tissue in the transitional zone between open and collapsed or edema-filled alveoli [31].
Figure 13.1 summarizes the different pathophysiologic steps of lung injury developing as a consequence of barotrauma/volutrauma, atelectrauma, and biotrauma. Table 13.1 summarizes the most relevant studies which investigated the pathophysiology of VILI.
From barotrauma/volutrauma to biotrauma. Ventilator-induced lung injury progresses from the primary mechanical injury to secondary atelectrauma, encouraged by both barotrauma and volutrauma. Atelectrauma resulting from alveolar interdependence is showed in panel 3, where at the interface between collapsed/consolidated (A) and overdistended lung units, the tissue may be injured by excessive shear stress and stretching caused by the uneven expansion of surrounding zone (C). Panel 4 shows the stress concentration between an air-filled and edematous alveolus (a model of forces between air-filled and air-filled alveoli where all forces are in balance – A; a model of forces between an air-filled and edematous alveolus where a greater pressure drop across the alveolar interface causing and excessive strain). The progression of lung damage is seen through inflammatory mediators (panel 5), eventually resulting in distal tissue damage. Mechanical stretch impairs alveolar epithelial integrity, causing a loss of tight junction structure and cell attachment associated with a production of pro-inflammatory cytokines
13.6 Mechanical Power
Very recently, a new way of looking at the ventilator side of VILI, i.e., the mechanical power, has been introduced [18] . According to this approach, every ventilator component already known to be associated with the development of VILI (tidal volume, driving pressure, respiratory rate, inspiratory-to-expiratory ratio and flow), with the addition of the effect of PEEP, contributes, each one to his proper extent, to the total amount of energy delivered to the respiratory system (and hence to the lung). The mechanical power concept does not introduce any new component to the field of ventilator-related causes of VILI; instead, it proposes and validates a mathematical description of machine power responsive to the relative contributions of its bedside-adjustable components. Starting from the classical equation of motion, an equation was developed that enables to calculate the mechanical power by some easily obtainable ventilator variables [53]. In fact, the initial trigger of stress and strain is the force applied to the lung extracellular matrix times its displacement, which equals the product of pressure times delta-volume. The cyclic energy loads applied at a given frequency (power) then triggers the development of VILI, which may be seen in this context as a sort of “fatigue” of the extracellular matrix [24]. If the lung is subject to an “excess” of energy, the unrecovered energy may be expected to be sufficient to break the molecular bonds of the polymers of the extracellular matrix [54, 55], to detach endothelial [56] and epithelial [57] cells from the basement membrane, and to fracture the capillary walls [58]. Alteration of the extracellular matrix, combined with capillary micro-fractures, may then activate an inflammatory reaction [59] and micro-hemorrhage, leading to the extracellular edema typical of VILI.
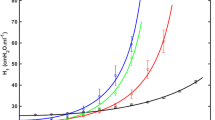
Indeed, the tidal change in lung volume is associated with a cyclic energy load delivered by the ventilator to the respiratory system. The energy load to the respiratory system (Fig. 13.2) is composed of a static component, due to PEEP and PEEP volume (conceptually equivalent to potential energy), and a dynamic cyclic component, due to driving pressure and tidal volume above PEEP (conceptually equivalent to kinetic energy), plus the additional, resistive and inertial component generated by the pressure spent for gas movement, the surface tension forces, and tissue resistances to motion. Energy is equal to the pressure applied times the change in volume, summed along the inspiratory volume-pressure curve. In contrast, once PEEP is applied, no further cyclic energy load is imposed on the system, as the volume is constant. As a matter of fact, PEEP plays a complex role in the context of the energy provided by the ventilator, as it provides increased continuous tension to the extracellular matrix which then accumulates potential energy. Further energy is added when cyclic tidal ventilation is superimposed to reach a given end-inspiratory volume. Therefore, if the end-inspiratory volume is the same, with or without PEEP, the energy is lower in the presence of PEEP than without it. Computed in this way, the energy/power load provided a single explanation of the different phenomena related to development of VILI.
Mechanical power and mechanical power equation. Mechanical energy provided during tidal ventilation and graphical representation of the power equation. The graphic is composed of a triangle on the lower left-hand side of the image, representing the elastic static component, i.e., the energy delivered just once when PEEP is applied, and of a larger trapezoid, representing the elastic dynamic component, whose area equals the elastic energy delivered at each tidal breath, to which a parallelogram is added on the right, representing the resistive component
In a recent paper, Gattinoni et al. [60] demonstrated how the “power equation,” as derived from the classical equation of motion with the addition of PEEP (while inertial forces were neglected), proved to yield comparable values of mechanical power when compared to data obtained experimentally through the pressure–volume curve analysis. The advantage of such a mathematical description of the mechanical power is that it enables the quantification of the relative contribution of its different components, thus allowing to anticipate the effects of their changes.
As far as mechanical ventilation is provided with PEEP, the static energy to reach the PEEP volume corresponds to the triangle equal to 1/2 × PEEP × PEEP volume. However, this energy is provided only once (as long as the same amount of PEEP is maintained), since during tidal ventilation the PEEP volume equals zero. However, in the presence of PEEP, more energy is required to inflate the lung. The energy needed for TV to reach P plat corresponds to the trapezoid equal to (peak pressure − PEEP) × TV/2 + (PEEP × TV).
From the classical equation of motion in which PEEP is also considered [61], at any given time, the pressure (P) in the whole respiratory system is equal to
where E rs is the respiratory system elastance, R aw is the total respiratory system resistance, and V i is the inspiratory flow.
The energy provided by the ventilator per breath can be calculated by multiplying each pressure in the motion equation by the volume variation (i.e., TV); after substituting V i with TV/T insp (the inspiratory time) and then expressing T insp as a function of respiratory rate (RR) and inspiratory-to-expiratory (I:E) ratio and converting the value to J/min, the following equation may be derived:
In the same paper [60], the authors demonstrated how, both in patients with healthy lungs and in patients with ARDS, the mechanical power measured directly through the pressure–volume curve analysis was strictly correlated with the one computed via the power equation.
Recently, in a secondary analysis of patients enrolled in two previously published randomized controlled trials [62], Guerin and colleagues [63] found how mechanical power (computed as DP × TV × RR, where DP is the airway driving pressure) was higher in ARDS non-survivors than in survivors. A dose–response effect was found, with higher values of power associated with increased mortality, and a threshold of 12 J/min was identified, which was associated with significant distinct probabilities of survival. Despite the equation proposed by the authors is simpler than that derived from the equation of motion, it represents only the product of respiratory rate times twice the dynamic energy component due to tidal volume, thus neglecting both the role of PEEP and that of the resistive load.
Since VILI originates from the interaction between the mechanical power transferred to the ventilable lung parenchyma and the anatomo-pathological characteristics of the latter, it is possible that different combinations of the components of mechanical power, resulting in a value greater than a given threshold, may produce similar damage. This was recently confirmed by animal experiments in which different combinations of tidal volume and respiratory rate were applied to detect the threshold for VILI [18]. The authors found how up to a mechanical power of approximately 12 J/min, the computed tomography scans showed mostly isolated densities, whereas when mechanical power was above the 12 J/min threshold, all piglets developed whole-lung edema.
Since airway pressure represents the pressure applied to the respiratory system as a whole, its interpretation is influenced by alterations in the mechanical properties of the chest wall [20, 64]; a more informative parameter could be the computation of the mechanical power selectively applied to the lung, either via the transpulmonary pressure–volume curve analysis or via a rearrangement of the equation of motion. The mechanical power delivered to the lung (POWERl) implies the use of the transpulmonary pressure (P l) instead of airway pressure at P plat and at PEEP. The relationship between P l and P aw (either P plat or PEEP) is expressed by P l = P aw × (E l/E rs), where E l is the elastance of the lung [65].
Therefore, substituting in the equation:
Eventually, it must be stressed that the mechanical power is just one part of the problem. The other part is represented by the lung’s conditions. The same mechanical power may have different effects depending on dimensions of the lung, the presence of inhomogeneity, the extent of the stress risers, and the vessels’ filling state, all factors which condition an uneven distribution of the delivered energy. Therefore, to be clinically meaningful, the mechanical power must be normalized, at least to the lung volume [66].
13.7 Extra-Parenchymal Factors
Nonmechanical background factors have repeatedly been proven important in the process of VILI generation, and, for any given ventilation pattern that applies potentially damaging stress, they may determine whether or not VILI is expressed [67]. These background factors, which may synergize with each other, include the preinjury and inflammatory state, the temperature at which ventilation occurs [68, 69], the amplitudes of vascular pressures and flows [56, 70], PaCO2/pH [71, 72], and FiO2 [73, 74].
In an experimental study aimed at investigating whether thermal stress could modulate the development of VILI, Suzuki et al. [68] randomized three groups of anesthetized rabbits to be ventilated for 2 h at core body temperatures of 33, 37, or 41° while ventilated with a noninjurious or a potentially injurious strategy. The hyperthermic group compared with the hypothermic animals developed a significantly higher degree of hypoxia and had increased lung edema and an altered pressure–volume relationship. To correct for potential effects arising from cardiac output fluctuations or from extrapulmonary organs, an isolated lung model was used for a confirmatory study, with similar findings. In a similarly designed study on rats, Akinci et al. [69] found how concomitant hyperthermia increased systemic inflammatory response, as assessed by higher levels of serum chemokines and cytokines, and a worse histology, during an injurious, high-pressure ventilation strategy.
Despite the great majority of studies of VILI which have specifically investigated the airspace mechanics, i.e., factors as tidal volume, plateau pressure, and PEEP, one must consider that the pulmonary alveolus is an interface between gas and blood. Indeed, because the intraluminal pressures applied to the airway epithelium also impact on the vascular endothelium, the potential for pressures and flows within blood vessels to influence the development and/or evolution of VILI has also been taken into account. The vascular structure of the pulmonary circulation is composed of both intra-alveolar and extra-alveolar vessels, whose behavior during lung inflation is fundamentally different. In fact, inflation compresses wall-embedded capillaries but dilates extra-alveolar microvessels. Under the high-permeability conditions of ARDS, even small increases in pulmonary microvascular pressure lead to increased edema formation. Moreover, unlike in health tissue in which the blood–gas barrier is intact, there is no clear pressure threshold for edema formation in the lung tissue of ARDS patients [75]. It is a well-known phenomenon that mechanical forces that tear the delicate alveolar–capillary membrane can originate on either side of the boundary, when the application of adverse ventilatory patterns to previously healthy lungs not only causes formation of proteinaceous edema, but it also stimulates neutrophil aggregation and hemorrhage [76]. The complementary issue, that is, the vascular contribution to VILI, was investigated in a series of studies conducted by the group of Marini using isolated, ventilated, and perfused lungs. When isolated rabbit lungs were exposed to perfusion levels that were equivalent to greater or less than the normal resting blood flow of in vivo animals, while ventilated with airway pressures that proved damaging in vivo, the authors demonstrated that perfusion amplitude contributed to the reduced lung compliance and promoted both lung edema and hemorrhage [77]. In a subsequent experiment [78], the authors found a significant relationship between the magnitude of pulmonary arterial pressure and the length of time over which it was sustained with the extent of VILI. Subsequent studies showed how lungs exposed to cyclic elevations in pulmonary artery pressure in the absence of ventilation formed less edema and exhibited less perivascular and alveolar hemorrhage than did ventilated lungs exposed to similar peak and mean pulmonary artery pressures and mean airway pressure [70]. Taken together, the studies demonstrated that when the mechanical stresses of the tidal cycle are high, an increase in precapillary vascular pressure or a reduction in postcapillary vascular pressure each could influence the severity of VILI inflicted by an unchanging adverse pattern of ventilation [56]. These observations imply that the gradient of transalveolar vascular pressure may be instrumental in inflicting damage when airway stresses are high. Figure 13.3 shows the possible mechanisms by which hemodynamic parameters may induce or exacerbate VILI.
In an attempt to reduce the total amount of stress delivered by the mechanical ventilator, a strategy of reduced minute ventilation has long ago been suggested [79], which was generally associated with increased carbon dioxide retention and hypercapnic acidosis. Indeed, experiments by Sinclair and coworkers [80] and by Broccard and colleagues [81] strongly indicate that the generation of hypercapnic acidosis may exert a protective effect on the severity of VILI. More recent preclinical data still confirm the protective effects of therapeutic hypercapnia initiated concurrently with injurious ventilation in an in vivo model of VILI [72]. The beneficial effects of such hypercapnic acidosis in reducing the extent of VILI are increasingly well understood and include attenuation of lung neutrophil recruitment, pulmonary and systemic cytokine and eicosanoid concentrations, cell apoptosis, and oxygen-derived and nitrogen-derived free radical injury [71].
The deleterious effects of hyperoxygenation are increasingly being recognized in several fields of intensive care medicine [82], to the extent that less aggressive approaches to oxygen supply have recently been suggested, even to not providing any supplemental oxygen, in several acute care settings, such as resuscitation of asphyxiated newborns, during acute myocardial infarction or after stroke or cardiac arrest [83]. Indeed, a recent trial showed how a conservative protocol for oxygen therapy vs conventional therapy resulted in lower mortality in a heterogeneous population of mechanically ventilated critically ill patients [84]. Experimental evidence points to the detrimental role of hyperoxia as a contributing factor to the development of VILI. In a laboratory investigation aimed at assessing whether hyperoxia could exacerbate lung injury caused by an injurious mechanical ventilation strategy, Sinclair and colleagues [73] found how hyperoxic animals, as compared to normoxic ones, had significantly reduced oxygenation and increased lung injury scores. Hyperoxia also significantly increased alveolar–capillary permeability and polymorphonuclear leukocytes and inflammatory mediator concentrations in bronchoalveolar lavage fluid. Similar results were found by Li et al. [74], who investigated the mechanisms regulating the interaction between injurious ventilation and hyperoxia. In their experiments, the authors found how the addition of hyperoxia to an unsafe ventilation strategy increased lung cytokine production, neutrophil infiltration by upregulation of the cytokine macrophage inflammatory protein-2, and apoptotic cell death through activation of the JNK and ERK1/2 pathways.
In conclusion, the vascular/metabolic/oxidative environment of the lung tissue at the onset of major mechanical stress has repeatedly shown to be influential in the VILI development process. Lowering ventilatory and cardiovascular demands – thereby reducing both minute ventilation and the vascular pressure gradient across the lung – are potentially important therapeutic targets when attempting to avoid VILI. It seems rational then to suggest a reduction in oxygen demand and ventilation requirement as a component of a comprehensive “lung-protective” strategy [67]. Indeed, reducing the ventilation requirement simultaneously allows reduction of driving pressures or ventilating frequencies. Because cardiac output also declines in response to lower oxygenation demands, the pulmonary microvascular blood flow gradient is lessened, thereby potentially reducing VILI risk.
References
Fan E, Needham DM, Stewart TE (2005) Ventilatory management of acute lung injury and acute respiratory distress syndrome. JAMA 294(22):2889–2896. doi:10.1001/jama.294.22.2889
Gattinoni L, Quintel M (2016) Is mechanical ventilation a cure for ARDS? Intensive Care Med 42(5):916–917. doi:10.1007/s00134-016-4266-y
Dreyfuss D, Soler P, Basset G, Saumon G (1988) High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 137(5):1159–1164. doi:10.1164/ajrccm/137.5.1159
Nash G, Blennerhassett JB, Pontoppidan H (1967) Pulmonary lesions associated with oxygen therapy and artificial ventilation. N Engl J Med 276(7):368–374. doi:10.1056/NEJM196702162760702
Avignon PD, Lindahl J, Werneman H (1956) Causes of death. Acta Medica Scand Suppl 316:111–113
Webb HH, Tierney DF (1974) Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 110(5):556–565. doi:10.1164/arrd.1974.110.5.556
Mascheroni D, Kolobow T, Fumagalli R, Moretti MP, Chen V, Buckhold D (1988) Acute respiratory failure following pharmacologically induced hyperventilation: an experimental animal study. Intensive Care Med 15(1):8–14
Fan E, Villar J, Slutsky AS (2013) Novel approaches to minimize ventilator-induced lung injury. BMC Med 11:85. doi:10.1186/1741-7015-11-85
Uhlig U, Uhlig S (2011) Ventilation-induced lung injury. Compr Physiol 1(2):635–661. doi:10.1002/cphy.c100004
Zapol WM, Snider MT, Hill JD, Fallat RJ, Bartlett RH, Edmunds LH, Morris AH, Peirce EC 2nd, Thomas AN, Proctor HJ, Drinker PA, Pratt PC, Bagniewski A, Miller RG Jr (1979) Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA 242(20):2193–2196
Bernard GR (2005) Acute respiratory distress syndrome: a historical perspective. Am J Respir Crit Care Med 172(7):798–806. doi:10.1164/rccm.200504-663OE
Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD (2009) Recent trends in acute lung injury mortality: 1996-2005. Crit Care Med 37(5):1574–1579. doi:10.1097/CCM.0b013e31819fefdf
Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS (1997) Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest 99(5):944–952. doi:10.1172/JCI119259
Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer JM, Brienza A, Bruno F, Slutsky AS (1999) Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 282(1):54–61
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network (2000). N Engl J Med 342(18):1301–1308. doi:10.1056/NEJM200005043421801
Marini JJ, Jaber S (2016) Dynamic predictors of VILI risk: beyond the driving pressure. Intensive Care Med 42(10):1597–1600. doi:10.1007/s00134-016-4534-x
Protti A, Maraffi T, Milesi M, Votta E, Santini A, Pugni P, Andreis DT, Nicosia F, Zannin E, Gatti S, Vaira V, Ferrero S, Gattinoni L (2016) Role of strain rate in the pathogenesis of ventilator-induced lung edema. Crit Care Med 44(9):e838–e845. doi:10.1097/CCM.0000000000001718
Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, Cammaroto A, Brioni M, Montaruli C, Nikolla K, Guanziroli M, Dondossola D, Gatti S, Valerio V, Vergani GL, Pugni P, Cadringher P, Gagliano N, Gattinoni L (2016) Mechanical power and development of ventilator-induced lung injury. Anesthesiology 124(5):1100–1108. doi:10.1097/ALN.0000000000001056
Tremblay LN, Slutsky AS (2006) Ventilator-induced lung injury: from the bench to the bedside. Intensive Care Med 32(1):24–33. doi:10.1007/s00134-005-2817-8
Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, Tallarini F, Cozzi P, Cressoni M, Colombo A, Marini JJ, Gattinoni L (2008) Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med 178(4):346–355. doi:10.1164/rccm.200710-1589OC
Tremblay LN, Slutsky AS (2005) Pathogenesis of ventilator-induced lung injury: trials and tribulations. Am J Physiol Lung Cell Mol Physiol 288(4):L596–L598. doi:10.1152/ajplung.00438.2004
Protti A, Cressoni M, Santini A, Langer T, Mietto C, Febres D, Chierichetti M, Coppola S, Conte G, Gatti S, Leopardi O, Masson S, Lombardi L, Lazzerini M, Rampoldi E, Cadringher P, Gattinoni L (2011) Lung stress and strain during mechanical ventilation: any safe threshold? Am J Respir Crit Care Med 183(10):1354–1362. doi:10.1164/rccm.201010-1757OC
Protti A, Andreis DT, Monti M, Santini A, Sparacino CC, Langer T, Votta E, Gatti S, Lombardi L, Leopardi O, Masson S, Cressoni M, Gattinoni L (2013) Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med 41(4):1046–1055. doi:10.1097/CCM.0b013e31827417a6
Protti A, Andreis DT, Milesi M, Iapichino GE, Monti M, Comini B, Pugni P, Melis V, Santini A, Dondossola D, Gatti S, Lombardi L, Votta E, Carlesso E, Gattinoni L (2015) Lung anatomy, energy load, and ventilator-induced lung injury. Intensive Care Med Exp 3(1):34. doi:10.1186/s40635-015-0070-1
Hewlett AM, Hulands GH, Nunn JF, Minty KB (1974) Functional residual capacity during anaesthesia. I: methodology. Br J Anaesth 46(7):479–485
Olegard C, Sondergaard S, Houltz E, Lundin S, Stenqvist O (2005) Estimation of functional residual capacity at the bedside using standard monitoring equipment: a modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg 101(1):206–212, table of contents. doi:10.1213/01.ANE.0000165823.90368.55
Tremblay LN, Slutsky AS (1998) Ventilator-induced injury: from barotrauma to biotrauma. Proc Assoc Am Physicians 110(6):482–488
Nieman GF, Satalin J, Andrews P, Habashi NM, Gatto LA (2016) Lung stress, strain, and energy load: engineering concepts to understand the mechanism of ventilator-induced lung injury (VILI). Intensive Care Med Exp 4(1):16. doi:10.1186/s40635-016-0090-5
Cressoni M, Cadringher P, Chiurazzi C, Amini M, Gallazzi E, Marino A, Brioni M, Carlesso E, Chiumello D, Quintel M, Bugedo G, Gattinoni L (2014) Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 189(2):149–158. doi:10.1164/rccm.201308-1567OC
Cressoni M, Gallazzi E, Chiurazzi C, Marino A, Brioni M, Menga F, Cigada I, Amini M, Lemos A, Lazzerini M, Carlesso E, Cadringher P, Chiumello D, Gattinoni L (2013) Limits of normality of quantitative thoracic CT analysis. Crit Care 17(3):R93. doi:10.1186/cc12738
Bilek AM, Dee KC, Gaver DP (1985) 3rd (2003) mechanisms of surface-tension-induced epithelial cell damage in a model of pulmonary airway reopening. J Appl Physiol 94(2):770–783. doi:10.1152/japplphysiol.00764.2002
Albert RK, Keniston A, Baboi L, Ayzac L, Guerin C (2014) Prone position-induced improvement in gas exchange does not predict improved survival in the acute respiratory distress syndrome. Am J Respir Crit Care Med 189(4):494–496. doi:10.1164/rccm.201311-2056LE
Lachmann B (1992) Open up the lung and keep the lung open. Intensive Care Med 18(6):319–321
Nieman GF, Gatto LA (1985) Habashi NM (2015) impact of mechanical ventilation on the pathophysiology of progressive acute lung injury. J Appl Physiol 119(11):1245–1261. doi:10.1152/japplphysiol.00659.2015
Kumar A, Pontoppidan H, Falke KJ, Wilson RS, Laver MB (1973) Pulmonary barotrauma during mechanical ventilation. Crit Care Med 1(4):181–186
Ioannidis G, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, Lampaki S, Kioumis I, Pitsiou G, Papaiwannou A, Karavergou A, Katsikogiannis N, Sarika E, Tsakiridis K, Korantzis I, Zarogoulidis K, Zarogoulidis P (2015) Barotrauma and pneumothorax. J Thorac Dis 7(Suppl 1):S38–S43. doi:10.3978/j.issn.2072-1439.2015.01.31
Tagliabue M, Casella TC, Zincone GE, Fumagalli R, Salvini E (1994) CT and chest radiography in the evaluation of adult respiratory distress syndrome. Acta Radiol 35(3):230–234
Marini JJ, Culver BH (1989) Systemic gas embolism complicating mechanical ventilation in the adult respiratory distress syndrome. Ann Intern Med 110(9):699–703
Dos Santos CC (1985) Slutsky AS (2000) invited review: mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol 89(4):1645–1655
Vlahakis NE, Hubmayr RD (2005) Cellular stress failure in ventilator-injured lungs. Am J Respir Crit Care Med 171(12):1328–1342. doi:10.1164/rccm.200408-1036SO
Ridge KM, Linz L, Flitney FW, Kuczmarski ER, Chou YH, Omary MB, Sznajder JI, Goldman RD (2005) Keratin 8 phosphorylation by protein kinase C delta regulates shear stress-mediated disassembly of keratin intermediate filaments in alveolar epithelial cells. J Biol Chem 280(34):30400–30405. doi:10.1074/jbc.M504239200
Muscedere JG, Mullen JB, Gan K, Slutsky AS (1994) Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 149(5):1327–1334. doi:10.1164/ajrccm.149.5.8173774
Mead J, Takishima T, Leith D (1970) Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 28(5):596–608
Valenza F, Guglielmi M, Irace M, Porro GA, Sibilla S, Gattinoni L (2003) Positive end-expiratory pressure delays the progression of lung injury during ventilator strategies involving high airway pressure and lung overdistention. Crit Care Med 31(7):1993–1998. doi:10.1097/01.CCM.0000070401.65534.F9
Steinberg JM, Schiller HJ, Halter JM, Gatto LA, Lee HM, Pavone LA, Nieman GF (2004) Alveolar instability causes early ventilator-induced lung injury independent of neutrophils. Am J Respir Crit Care Med 169(1):57–63. doi:10.1164/rccm.200304-544OC
Hotchkiss JR Jr, Blanch L, Murias G, Adams AB, Olson DA, Wangensteen OD, Leo PH, Marini JJ (2000) Effects of decreased respiratory frequency on ventilator-induced lung injury. Am J Respir Crit Care Med 161(2 Pt 1):463–468. doi:10.1164/ajrccm.161.2.9811008
Chiumello D, Carlesso E, Brioni M, Cressoni M (2016) Airway driving pressure and lung stress in ARDS patients. Crit Care 20:276. doi:10.1186/s13054-016-1446-7
Chiumello D, Chidini G, Calderini E, Colombo A, Crimella F, Brioni M (2016) Respiratory mechanics and lung stress/strain in children with acute respiratory distress syndrome. Ann Intensive Care 6(1):11. doi:10.1186/s13613-016-0113-0
Manzano F, Fernandez-Mondejar E, Colmenero M, Poyatos ME, Rivera R, Machado J, Catalan I, Artigas A (2008) Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med 36(8):2225–2231. doi:10.1097/CCM.0b013e31817b8a92
Fanelli V, Mascia L, Puntorieri V, Assenzio B, Elia V, Fornaro G, Martin EL, Bosco M, Delsedime L, Fiore T, Grasso S, Ranieri VM (2009) Pulmonary atelectasis during low stretch ventilation: "open lung" versus "lung rest" strategy. Crit Care Med 37(3):1046–1053. doi:10.1097/CCM.0b013e3181968e7e
Page B, Vieillard-Baron A, Beauchet A, Aegerter P, Prin S, Jardin F (2003) Low stretch ventilation strategy in acute respiratory distress syndrome: eight years of clinical experience in a single center. Crit Care Med 31(3):765–769. doi:10.1097/01.CCM.0000055402.68581.DC
Slutsky AS, Tremblay LN (1998) Multiple system organ failure. Is mechanical ventilation a contributing factor? Am J Respir Crit Care Med 157(6 Pt 1):1721–1725. doi:10.1164/ajrccm.157.6.9709092
Tonetti T, Cressoni M, Collino F, Maiolo G, Rapetti F, Quintel M, Gattinoni L (2017) Volutrauma, Atelectrauma, and mechanical power. Crit Care Med 45(3):e327–e328. doi:10.1097/CCM.0000000000002193
Parker JC, Breen EC (1985) West JB (1997) high vascular and airway pressures increase interstitial protein mRNA expression in isolated rat lungs. J Appl Physiol 83(5):1697–1705
Pelosi P, Rocco PR (2008) Effects of mechanical ventilation on the extracellular matrix. Intensive Care Med 34(4):631–639. doi:10.1007/s00134-007-0964-9
Marini JJ, Hotchkiss JR, Broccard AF (2003) Bench-to-bedside review: microvascular and airspace linkage in ventilator-induced lung injury. Crit Care 7(6):435–444. doi:10.1186/cc2392
Budinger GR, Sznajder JI (2006) The alveolar-epithelial barrier: a target for potential therapy. Clin Chest Med 27(4):655–669; abstract ix. doi:10.1016/j.ccm.2006.06.007
West JB (2013) Fragility of pulmonary capillaries. J Appl Physiol (1985) 115(1):1–15. doi:10.1152/japplphysiol.00229.2013
O'Neill LA (2005) TLRs play good cop, bad cop in the lung. Nat Med 11(11):1161–1162. doi:10.1038/nm1105-1161
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, Protti A, Gotti M, Chiurazzi C, Carlesso E, Chiumello D, Quintel M (2016) Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 42(10):1567–1575. doi:10.1007/s00134-016-4505-2
Marini JJ, Crooke PS 3rd (1993) A general mathematical model for respiratory dynamics relevant to the clinical setting. Am Rev Respir Dis 147(1):14–24. doi:10.1164/ajrccm/147.1.14
Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guerin C, Prat G, Morange S, Roch A (2010) Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 363(12):1107–1116. doi:10.1056/NEJMoa1005372
Guerin C, Papazian L, Reignier J, Ayzac L, Loundou A, Forel JM (2016) Effect of driving pressure on mortality in ARDS patients during lung protective mechanical ventilation in two randomized controlled trials. Crit Care 20(1):384. doi:10.1186/s13054-016-1556-2
Cortes GA, Marini JJ (2013) Two steps forward in bedside monitoring of lung mechanics: transpulmonary pressure and lung volume. Crit Care 17(2):219. doi:10.1186/cc12528
Chiumello D, Cressoni M, Colombo A, Babini G, Brioni M, Crimella F, Lundin S, Stenqvist O, Gattinoni L (2014) The assessment of transpulmonary pressure in mechanically ventilated ARDS patients. Intensive Care Med 40(11):1670–1678. doi:10.1007/s00134-014-3415-4
Gattinoni L, Pesenti A (2005) The concept of "baby lung". Intensive Care Med 31(6):776–784. doi:10.1007/s00134-005-2627-z
Marini JJ (2015) Advances in the support of respiratory failure: putting all the evidence together. Crit Care 19(Suppl 3):S4. doi:10.1186/cc14722
Suzuki S, Hotchkiss JR, Takahashi T, Olson D, Adams AB, Marini JJ (2004) Effect of core body temperature on ventilator-induced lung injury. Crit Care Med 32(1):144–149. doi:10.1097/01.CCM.0000098857.14923.44
Akinci OI, Celik M, Mutlu GM, Martino JM, Tugrul S, Ozcan PE, Yilmazbayhan D, Yeldandi AV, Turkoz KH, Kiran B, Telci L, Cakar N (2005) Effects of body temperature on ventilator-induced lung injury. J Crit Care 20(1):66–73
Hotchkiss JR Jr, Blanch L, Naveira A, Adams AB, Carter C, Olson DA, Leo PH, Marini JJ (2001) Relative roles of vascular and airspace pressures in ventilator-induced lung injury. Crit Care Med 29(8):1593–1598
Curley G, Kavanagh BP, Laffey JG (2010) Hypocapnia and the injured brain: more harm than benefit. Crit Care Med 38(5):1348–1359. doi:10.1097/CCM.0b013e3181d8cf2b
Peltekova V, Engelberts D, Otulakowski G, Uematsu S, Post M, Kavanagh BP (2010) Hypercapnic acidosis in ventilator-induced lung injury. Intensive Care Med 36(5):869–878. doi:10.1007/s00134-010-1787-7
Sinclair SE, Altemeier WA, Matute-Bello G, Chi EY (2004) Augmented lung injury due to interaction between hyperoxia and mechanical ventilation. Crit Care Med 32(12):2496–2501
Li LF, Liao SK, Ko YS, Lee CH, Quinn DA (2007) Hyperoxia increases ventilator-induced lung injury via mitogen-activated protein kinases: a prospective, controlled animal experiment. Crit Care 11(1):R25. doi:10.1186/cc5704
Brigham KL, Woolverton WC, Blake LH, Staub NC (1974) Increased sheep lung vascular permeability caused by pseudomonas bacteremia. J Clin Invest 54(4):792–804. doi:10.1172/JCI107819
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157(1):294–323. doi:10.1164/ajrccm.157.1.9604014
Broccard AF, Hotchkiss JR, Kuwayama N, Olson DA, Jamal S, Wangensteen DO, Marini JJ (1998) Consequences of vascular flow on lung injury induced by mechanical ventilation. Am J Respir Crit Care Med 157(6 Pt 1):1935–1942. doi:10.1164/ajrccm.157.6.9612006
Broccard AF, Hotchkiss JR, Suzuki S, Olson D, Marini JJ (1999) Effects of mean airway pressure and tidal excursion on lung injury induced by mechanical ventilation in an isolated perfused rabbit lung model. Crit Care Med 27(8):1533–1541
Hickling KG, Henderson SJ, Jackson R (1990) Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med 16(6):372–377
Sinclair SE, Kregenow DA, Lamm WJ, Starr IR, Chi EY, Hlastala MP (2002) Hypercapnic acidosis is protective in an in vivo model of ventilator-induced lung injury. Am J Respir Crit Care Med 166(3):403–408. doi:10.1164/rccm.200112-117OC
Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller MD (2001) Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164(5):802–806. doi:10.1164/ajrccm.164.5.2007060
Asfar P, Singer M, Radermacher P (2015) Understanding the benefits and harms of oxygen therapy: response to comments by Akca. Intensive Care Med 41(10):1875. doi:10.1007/s00134-015-3995-7
Sjoberg F, Singer M (2013) The medical use of oxygen: a time for critical reappraisal. J Intern Med 274(6):505–528. doi:10.1111/joim.12139
Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, Morelli A, Antonelli M, Singer M (2016) Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA 316(15):1583–1589. doi:10.1001/jama.2016.11993
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Umbrello, M., Formenti, P. (2017). Ventilator-Induced Lung Injury. In: Chiumello, D. (eds) Acute Respiratory Distress Syndrome. Springer, Cham. https://doi.org/10.1007/978-3-319-41852-0_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-41852-0_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41850-6
Online ISBN: 978-3-319-41852-0
eBook Packages: MedicineMedicine (R0)