Abstract
Polytrauma that includes the central nervous system presents a challenge to both surgical and neurocritical care teams as optimal fluid administration during resuscitation must facilitate hemostasis and restore intravascular volume, without worsening the secondary brain injury. Care must be taken to avoid edema systemically, as well as to the injured brain and its already compromised microvasculature and blood brain barrier. Fluid balance is an important consideration as well as the type of fluid administered. In addition to hyperosmolar agents, other fluids and adjunctive therapies such as platelets and fresh frozen plasma have emerged as options with both systemic and neuroprotective benefits. Evaluating resuscitation in traumatic brain injury is complex, and intracranial pressure along with cerebral perfusion pressure management alone may not be adequate to significantly impact clinical outcomes. Robust clinical trials must be designed so that the promising therapies that have emerged from preclinical studies can be adequately translated and evaluated with clinically relevant and measurable outcomes.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Traumatic brain injury
- Blood brain barrier
- Hypertonic saline
- Colloids
- Fresh frozen plasma
- Platelets
- Intracranial pressure
- Brain tissue oxygenation
- Microdialysis
- Cell therapy
Introduction
Polytrauma that includes the central nervous system, especially cases involving traumatic brain injury (TBI) presents a challenge to both surgical and neurocritical care teams due to potential competing interests during the resuscitative period. Trauma resuscitation involves the infusion of fluids to help decrease bleeding, reverse and prevent coagulopathy, support cardiovascular integrity in order to maintain organ, tissue, and cellular function. Recently these goals have been met while decreasing edema formation. In the brain, the blood brain barrier (BBB) normally maintains immunologic privilege as well as tight autoregulatory fluid control. However, following TBI, BBB dysfunction leads to vasogenic and cytotoxic edema, which contributes to intracranial hypertension [1]. TBI in return has been shown to have systemic implications in physiology such respiratory compromise as well as derangements in the hypothalamic pituitary adrenal axis such as acute glucocorticoid deficiency and diabetes insipidus [2]. This chapter will discuss current practices as well as preclinical and clinical studies aiming to answer the question about the optimal fluid resuscitation strategy.
In trauma patients without TBI, resuscitation goals include relatively low mean arterial, urine output and central venous pressure until definitive hemostasis is obtained, reversal of coagulopathy as well as the clearing of a base deficit. These “hypotensive” goals are utilized until definitive hemostasis is obtained, usually within 2–3 h of admission. In neurocritical care, adequate cerebral perfusion is paramount, with goal pressures of at least 60 mmHg, achieved by balancing intracranial pressure (ICP) and systemic mean arterial pressure of at least 90 mmHg. Especially early in the resuscitation of a polytrauma patient, it is obvious that these goals may seem contradictory. Intracranial pressure is reduced in a tiered fashion, with first tier treatments typically including sedation, establishing an ICP threshold, cerebral perfusion monitoring, neuromuscular blockade, cerebral spinal fluid (CSF) drainage, and hyperosmolar therapy [3]. Second tier treatments include hyperventilation, barbiturates for pharmacological coma with electroencephalogram monitoring for burst suppression, hypothermia, and surgical decompression. Mean arterial pressure is commonly supported by the use of vasoactive pressors norepinephrine and phenylephrine because they have the least effect on cerebral vasomotor tone, but overaggressive hypertension may increase the risk of acute respiratory distress syndrome [4]. Up to one-third of TBI patients have abnormal cerebral autoregulation. As the result of the loss of cerebral autoregulation, cerebral blood flow and capillary hydrostatic pressure increases, exacerbating edema and ICP. CSF circulation and clearance of metabolites is also impaired following TBI.
Fluid Balance
Only a handful of clinical studies have been designed to specifically address trauma resuscitation and fluid balance in cases that include traumatic brain injury , and none have found any association to benefits of fluid balance management and neurologic outcome [5]. Inferences have been made from other studies such as the North American Brain Injury Study: Hypothermia II (NABIS:H II) suggested that the higher incidence of intracranial hypertension was likely associated with resuscitation in the first 96 h aimed at countering hypotension encountered during the hypothermic protocol. Adjusting for injury severity, TBI patients were shown to have modestly increased odds of death after receiving resuscitative intravenous fluids in the prehospital setting. A retrospective cohort TBI study examined total fluid balance over the first 10 days of intensive care admission and the association with refractory intracranial hypertension despite first tiered therapies (defined as ICP >20 for 30 min or ICP >15 for 15 min in patients status post decompressive craniectomy). The study found that there was no difference between cumulative fluid in patients that did or did not develop refractory intracranial hypertension [6].
Crystalloids Versus Colloids
Crystalloids have long been first line therapy for resuscitating the trauma patient but the pattern of distribution of specific crystalloid products has implications on the degree of interstitial edema. Colloids such as albumin have the potential of raising intravascular oncotic pressure, thereby reducing interstitial edema to tissues such as the brain. However, studies such as the Saline versus Albumin Fluid Evaluation (SAFE) trial found that the clinical effect of colloids such as albumin have been much less than estimated [7]. Ad hoc subgroup analysis of the SAFE TBI trial found that the use of albumin was associated with increased treatment intensity in order to control ICP [8]. Reviewers of the SAFE trial have suggested that the albumin was either leaking into the brain interstitial tissue thereby exacerbating the edema or that the albumin solution was slightly hypoosmotic compared to normal saline [9]. In another study, albumin combined with neutral or a slightly negative fluid balance was associated with low mortality in severe TBI, but was associated with high rates respiratory failure [10]. To date, other colloids including synthetics have not produced convincing evidence to alter clinical practice.
Hyperosmolar Therapy
Hyperosmolar therapy includes mannitol, which is administered at 0.5–1 g/kg and produces effect within 15–30 min. This can be administered every 6 h to a target serum osmolaritiy of 310–320 Osm/L. In addition to lowering the intracranial pressure , mannitol also has been shown to improve cerebral blood flow (CBF) [11]. 23 % hypertonic saline can be used for hyperacute ICP elevations and for herniation syndromes and can reduce the ICP by up to 50 % within minutes and produce a durable response over hours [12].
Osmotic agents, including mannitol and hypertonic saline have been shown to be well tolerated and effective in the reduction of intracranial hypertension, but to date, no study has shown improved survival nor improved neurological outcomes. While both mannitol and hypertonic saline are both considered first tiered therapies, the dosing and administration practices vary between and within institutions and thus the power of systematic reviews are limited [13]. The Saline versus Albumin Fluid Evaluation Translation of Research Into Practice Study (SAFE TRIPS) trial was a global cross-sectional study that looked at 391 intensive care units and found that the choice of resuscitative fluid varied considerably and was associated more with local practice then the clinical scenario [14].
In the case of the trauma patient with polytrauma, hypertonic saline has found applications in reducing bowel edema in damage control surgery. In a retrospective study, the use of 3 % sodium chloride at 30 mL/h as maintenance fluid compared to isotonic fluids at 125 mL/h in damage control laparotomies was associated with 100 % primary fascial closure by day 7 compared to 76 % with isotonic fluids (p = 0.010). Retrospective studies have suggested that mannitol and hypertonic saline boluses (23.4 %) are equivalent in reducing ICP [15]. It is evident however, that in practice, the use of mannitol has become more limited to situations where quick reductions in ICP is required as the potential for diuresis complications are more prevalent than with hypertonic saline [16]. Rapid diuresis in the hypovolemic polytrauma patient can be especially deleterious, causing precipitous drops in blood pressure. Thus in theory, hypertonic saline can be considered one of the optimal fluids to be administered in a scenario of a patient with TBI undergoing damage control laparotomy. Although hypertonic saline is a common agent used for intracranial hypertension, patients experience worsening of their hypocoagulability and hyper-fibrinolysis, which may complicate the initial resuscitation of patients with polytrauma [17–19]. In a randomized control study evaluating single 250 mL bolus administration of 7.5 % saline, 7.5 % saline/6 % dextran, or normal saline in the prehospital setting for severe TBI patients not in hypovolemic shock, no differences were seen in 6 month Extended Glasgow Outcome Scale scores or disability rating scores. A follow-up study examining the same prehospital strategy of treating severe TBI patients with hypovolemic shock also did not show any differences in 28 day survival (although the study was stopped early due to increased early mortality in a subset of hypertonic saline and hypertonic saline/dextran groups that did not receive packed red blood cells in the first 24 h).
Other Crystalloids
Investigators have also explored the use of lactate containing solutions and sodium bicarbonate in small clinical studies. Lactate is a preferred energy substrate in TBI, increasing cerebral blood flow and in a small study, reduced intracranial hypertension to a similar degree as equimolar mannitol [20]. Half molar sodium lactate was applied in a randomized double blinded study versus normal saline and was found to significantly reduce the number of elevated ICP episodes as well as total fluid and chloride balance over the first 48 h post TBI [21]. Equiosmolar 8.4 % sodium bicarbonate was investigated in a small, randomized trial versus 5 % hypertonic sodium chloride and was found to have equal reductions in ICP [22]. The use of sodium bicarbonate may reduce the incidence of hyperchloremic metabolic acidosis commonly seen with repeated doses of hypertonic sodium chloride and may provide an advantage in critically ill trauma patients where acidosis already exists [23].
Blood Products
Blood products are increasingly becoming a standard addition to the trauma resuscitation algorithm starting in certain cases in the prehospital setting [24]. Optimal resuscitation using blood products has been shown through the Prospective Observational Multicenter Major Trauma Transfusion (PROMMITT) and Pragmatic Randomized Optimal Platelet and Plasma Ratios (PROPPR) studies to be best performed using balanced red cells, fresh frozen plasma (FFP) and platelets . Many leading trauma centers now use plasma as the primary resuscitation fluid in hypovolemic trauma patients. These centers are also placing this approach into the prehospital environment [25]. Of interest in TBI is the potential therapeutic benefit of FFP due to the known endotheliopathy that occurs in trauma. One TBI population that may particularly benefit from FFP is the pediatric population, which is prone to developing coagulopathy following injury than adults and also demonstrate acute phase dysregulation of fluid and electrolyte balance [26].
Plasma repairs the systemic endothelial injury and dysfunction that leads to coagulation disturbances and inflammation [27]. This protective property has been shown in the pulmonary endothelium as well as in studies on platelet function, and thus may play an important role in treating the endothelial dysfunction that occurs following TBI at the level of the blood brain barrier [28]. Compared to normal saline, FFP has been shown to cause less activation of coagulation, natural anticoagulation, and endothelial systems in porcine polytrauma models of TBI [29].
Initial porcine studies by the Alam group comparing FPP, 6 % hetastarch and normal saline in a combined controlled TBI and hemorrhage model (mimicking the polytrauma patient) demonstrated superiority of FFP over 6 % hetastarch and normal saline in reducing lesion size and edema. The volume of normal saline required to resuscitate the animals was three times that of FFP [30]. Further studies demonstrated decreased excitotoxicty through decreased levels of glutamate and glycerol as well as improved energetics with higher levels of mitochondrial pyruvate dehydrogenase complex activity with FFP resuscitation compared to normal saline [31]. More recently, the investigators were also able to demonstrate improved levels of brain oxygenation, cerebral perfusion pressure and endothelial nitric oxide synthase [32].
The roles of blood products such as FFP and component factors become critical with the increased incidence of trauma patients arriving on anticoagulation including warfarin, clopidogrel and others. The reversal of anticoagulation is often part of the initial resuscitation process and may be even more essential to survival in TBI patients than non-TBI trauma patients [33]. Investigators have suggested that the use of recombinant factor VIIa can reduce the amount of FFP required and may help reduce length of stay and intensive care required in the coagulopathic TBI patient [34]. In the most challenging cases where direct thrombin inhibitors such as Dabigatran, Etexilate are not easily reversed, monitoring with thrombelastography and treatments such as activated prothrombin complex concentrates, recombinant factor VIIa and other factors may need to be employed, along with possible emergency dialysis [35, 36].
Other Considerations
In the effort to move resuscitation to the prehospital setting, investigators have studied the potential of “on demand” versions of plasma and red cells. Lyophilized plasma product was found to be just as effective as FFP preclinical swine models of combined TBI and hemorrhagic shock [37]. The hemoglobin based oxygen carrier HBOC-201 was found to improve cerebral perfusion pressure and brain tissue oxygen versus lactated ringers [38, 39]. While some high volume centers in the US have placed liquid plasma and RBCs on their helicopters, the dried plasma products will facilitate wide spread adoption. Although increasing oxygenation should theoretically protect the injured brain, a recent randomized trial found that neither the administration of erythropoietin nor establishing a transfusion threshold of 10 g/dL resulted in any improvements in a dichotomized Glasgow Outcome Scale at 6 months post TBI [40]. Additionally, the incidence of venous thromboembolisms increased in the treated groups. In the design of such studies, the choice of the outcome measure may need to be tailored to the proposed mechanism of the treatment in order to find clinically significant and relevant associations.
Neurocritical Care Targets of Resuscitation
The monitoring and treatment of ICP is a major target in the treatment of TBI. However, controversy exists in the impact of ICP directed therapy on outcomes. The multicentered, randomized Benchmark Evidence from South American Trials: Treatment of Intracranial Pressures (BEST TRIP) study reported no difference in functional/cognitive outcome, mortality, median ICU stay, and serious adverse events between maintaining ICP at or below 20 mmHg to imaging and clinical examination alone [41, 42]. Critics of the trial argue that the study varied from established guidelines and did not specifically look into ICP monitor use for the management of intracranial hypertension, thereby limiting external validity and generalizability. The average ICP during the acute neurointensive period has been used as an early target for therapy in hopes that this indicator could correlate with long-term outcome. However, studies have reported that average ICP during the first 48 h do not correlate with 6-month functional nor neuropsychological outcomes [43]. Some suggest that, these studies generally do not reflect continuous monitoring trends, number of spikes and waveforms, and are thus likely limited by design. Despite these findings, recent evidence looking specifically at large databases and studies following the Brain Trauma Foundation (BTF) guidelines suggest that ICP monitoring contributed to improved outcomes [44–47].
The debate regarding ICP monitoring and outcome has led investigators to seek additional, multimodal approaches to guide resuscitation for the injured brain and include brain oxygen monitoring and microdialysis . Poor short-term outcome is associated with hypoxia measured by pBrO2 (partial pressure of oxygen in brain tissue) independent of elevated ICP, low CPP, and injury severity [48]. Studies have suggested that pBrO2 directed therapy can lead to improved Glasgow Outcome Scores (GOS) at 6 months versus standard ICP directed management [49]. The multicentered Phase II Brain Tissue Oxygen Monitoring in Traumatic Brian Injury (BOOST 2) trial, will further evaluate whether pBrO2 levels below the critical threshold of 20 mmHg can be reduced with monitoring, in addition to the evaluation of safety, feasibility and GOS extended scores 6 months post injury. Despite the potential benefits of an additional metabolic indicator of resuscitation, judicial use of monitoring equipment may be necessary as using pBrO2 monitors have also been shown in a study to be associated with higher cumulative fluid balance, vasopressor use, pulmonary edema and refractory intracranial hypertension [6].
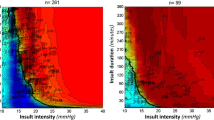
Microdialysis has the ability to provide information regarding the metabolic status of penumbral brain tissue, and includes real-time glucose, lactate, glycerol, and glutamate measurements although robust randomized clinical trials have not yet been pursued. Studies have suggested that metabolic derangements can be detected by microdialysis prior to increases in ICP [50]. Investigators have also demonstrated that metabolic crisis, defined by brain glucose <0.8 mmol/L and lactate/pyruvate ratio > 25 can occur at an incidence of 74 % despite adequate resuscitation and controlled ICP [51].
While the use of pBrO2 monitoring and microdialysis has not been widely adopted in clinical use, these two devices provide investigators valuable tools beyond simple ICP measurements when evaluating emerging therapeutics. Combined microdialysis and positron emission tomography in patients following severe TBI demonstrated that metabolic crisis can even be present without cerebral ischemia as measured by oxygen extraction fraction and cerebral venous oxygen content [52].
Future Directions
The solution to effective resuscitation for the polytrauma patient with TBI will likely be in the form of a multimodal approach that will include FFP, hyperosmolar agents, as well as other emerging fluid options such as lactate and hypertonic bicarbonate solutions and other therapeutic adjuncts. Optimizing resuscitation by decreasing blood loss and edema seems to be a reasonable approach. Clinical strategies have even included case reports where continuous renal replacement therapy was shown to normalize intracranial hypertension in TBI patients within 48 h of initiation through a hypothesized mechanism of gentle removal of fluid, solutes and inflammatory cytokines [53]. Preclinical studies have suggested that valproic acid can improve energetics, reduce lesion size, and edema [54]. Cell therapy with bone marrow derived mesenchymal stromal cells has been shown to inhibit inflammation and preserve vascular endothelial integrity in lungs after hemorrhagic shock and preserve vascular endothelial barrier proteins [55]. Clinical trials are underway in both pediatric and adult populations using autologous bone marrow derived mononuclear cells intravenously delivered within 48 h of injury [56, 57].
Controversy still exists in the extent of which ICP directed management impacts short and long-term outcomes, thus other strategies, new targets are necessary. Clinical trials should be designed to test therapies against clinically relevant outcome measures such as neurointensive length of stay, short and long-term neurocongitive outcomes and neuroimaging, in addition to standard long-term function. Neurophysiological outcomes, such as BBB dysfunction can be assessed by CSF-plasma albumin quotient and may be the key to validating and translating preclinical studies to the intensive care unit [58]. Even the amount of resuscitative fluid and adequacy on a per patient basis can be optimized. For example, limited transthoracic echocardiogram has been shown to be effective in guiding fluid resuscitation [59]. Also, plasma levels of longitudinal midregional pro-atrial naturetic peptide has been studied as a prognostic tool of GOS outcome at 6-months post injury [60].
Polytrauma that includes central nervous system injury and hemorrhagic shock presents a complicated challenge for trauma and neurocritical care teams during the resuscitative period. The choice of fluid administrated during the resuscitative period has direct impact to the central nervous system. The adequacy of resuscitation in regards to TBI must look beyond ICP and CPP management adherence to include clinically relevant indicators of outcome. To date, small studies and post hoc analysis have not yielded convincing support towards any single clinical management strategy. Although plasma and other fluids have emerged as effective agents in preclinical studies, robust clinical trials or retrospective studies using trauma registries must be designed to correlate preclinical physiologic as well as functional improvements to clinically measureable outcomes.
Today, trauma and neurocritical care teams must approach the TBI patient with coexisting hemorrhagic shock with a tailored approach, using multiple systemic and neuromonitoring modalities while applying judicious selection of resuscitative fluids. Balanced blood products should be given for hemorrhagic shock and early ICP monitoring established with frequent neurologic checks. The delay to ICP monitoring or neurosurgical intervention should be reduced. Retrospective studies suggest that hemorrhagic complications infrequently occur when international normalized ratio (INR) levels of 1.6 or less [61]. The increased usage of thrombelastography to assess the functional clotting status may reduce the delay that moderately elevated INR values causes to neurosurgical interventions [62]. Early stabilization of both systemic and cerebral endothelia with FFP may influence the course of resuscitation. The choice of additional resuscitative fluids may depend on the clinical scenario. FFP can be given when patients present with multiple derangements such as hypovolemia, coagulopathy, and possibly cerebral edema due to endothelial dysfunction of the BBB. Hyperosmolar agents can be used for episodes of intracranial hypertension, but can be beneficial when applied to counter systemic as well as cerebral edema in TBI patients undergoing damage control laparotomies. Other fluid options such as lactate and hypertonic bicarbonate solutions should be considered as additional therapies for neuroprotection if clinically indicated. These resuscitative efforts should ideally be directed using prospectively designed service guidelines and thoroughly captured for analysis.
References
Unterberg AW, Stover J, Kress B, Kiening KL. Edema and brain trauma. Neuroscience. 2004;129(4):1021–9 Epub 2004/11/25.
Hannon MJ, Crowley RK, Behan LA, O’Sullivan EP, O’Brien MM, Sherlock M, et al. Acute glucocorticoid deficiency and diabetes insipidus are common after acute traumatic brain injury and predict mortality. J Clin Endocrinol Metab. 2013;98(8):3229–37 Epub 2013/05/22.
Sakellaridis N, Pavlou E, Karatzas S, Chroni D, Vlachos K, Chatzopoulos K, et al. Comparison of mannitol and hypertonic saline in the treatment of severe brain injuries. J Neurosurg. 2011;114(2):545–8 Epub 2010/11/23.
Frattalone AR, Ling GS. Moderate and severe traumatic brain injury: pathophysiology and management. Neurosurg Clin N Am. 2013;24(3):309–19 Epub 2013/07/03.
Gantner D, Moore EM, Cooper DJ. Intravenous fluids in traumatic brain injury: what’s the solution? Curr Opin Crit Care. 2014;20(4):385–9 Epub 2014/07/01.
Fletcher JJ, Bergman K, Blostein PA, Kramer AH. Fluid balance, complications, and brain tissue oxygen tension monitoring following severe traumatic brain injury. Neurocrit Care. 2010;13(1):47–56 Epub 2010/04/09.
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. New Engl J Med. 2004;350(22):2247–56 Epub 2004/05/28.
Cooper DJ, Myburgh J, Heritier S, Finfer S, Bellomo R, Billot L, et al. Albumin resuscitation for traumatic brain injury: is intracranial hypertension the cause of increased mortality? J Neurotrauma. 2013;30(7):512–8 Epub 2012/12/01.
Van Aken HK, Kampmeier TG, Ertmer C, Westphal M. Fluid resuscitation in patients with traumatic brain injury: what is a SAFE approach? Curr Opin Anaesthesiol. 2012;25(5):563–5 Epub 2012/07/25.
Rodling Wahlstrom M, Olivecrona M, Nystrom F, Koskinen LO, Naredi S. Fluid therapy and the use of albumin in the treatment of severe traumatic brain injury. Acta anaesthesiologica Scandinavica. 2009;53(1):18–25. Epub 2008/10/24.
Scalfani MT, Dhar R, Zazulia AR, Videen TO, Diringer MN. Effect of osmotic agents on regional cerebral blood flow in traumatic brain injury. Journal of critical care. 2012;27(5):526 e7–12. Epub 2011/12/20.
Kesinger MR, Nagy LR, Sequeira DJ, Charry JD, Puyana JC, Rubiano AM. A standardized trauma care protocol decreased in-hospital mortality of patients with severe traumatic brain injury at a teaching hospital in a middle-income country. Injury. 2014;45(9):1350–4 Epub 2014/05/28.
Mortazavi MM, Tubbs RS, Riech S, Verma K, Shoja MM, Zurada A, et al. Anatomy and pathology of the cranial emissary veins: a review with surgical implications. Neurosurgery. 2012;70(5):1312–8; discussion 8–9. Epub 2011/12/01.
Finfer S, Liu B, Taylor C, Bellomo R, Billot L, Cook D, et al. Resuscitation fluid use in critically ill adults: an international cross-sectional study in 391 intensive care units. Critical care. 2010;14(5):R185. Epub 2010/10/19.
Ware ML, Nemani VM, Meeker M, Lee C, Morabito DJ, Manley GT. Effects of 23.4 % sodium chloride solution in reducing intracranial pressure in patients with traumatic brain injury: a preliminary study. Neurosurgery. 2005;57(4):727–36; discussion-36. Epub 2005/10/22.
Rhoney DH, Parker D Jr. Considerations in fluids and electrolytes after traumatic brain injury. Nutr Clin Pract: Off Publ Am Soc Parenter Enteral Nutr. 2006;21(5):462–78 Epub 2006/09/26.
Delano MJ, Rizoli SB, Rhind SG, Cuschieri J, Junger W, Baker AJ, et al. Pre-Hospital Resuscitation of Traumatic Hemorrhagic Shock with Hypertonic Solutions Worsen Hypo-Coagulation and Hyper-Fibrinolysis. Shock. 2015. Epub 2015/03/19.
Bulger EM, May S, Brasel KJ, Schreiber M, Kerby JD, Tisherman SA, et al. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA. 2010;304(13):1455–64 Epub 2010/10/07.
Bulger EM, May S, Kerby JD, Emerson S, Stiell IG, Schreiber MA, et al. Out-of-hospital hypertonic resuscitation after traumatic hypovolemic shock: a randomized, placebo controlled trial. Ann Surg. 2011;253(3):431–41 Epub 2010/12/24.
Ichai C, Armando G, Orban JC, Berthier F, Rami L, Samat-Long C, et al. Sodium lactate versus mannitol in the treatment of intracranial hypertensive episodes in severe traumatic brain-injured patients. Intensive Care Med. 2009;35(3):471–9 Epub 2008/09/23.
Ichai C, Payen JF, Orban JC, Quintard H, Roth H, Legrand R, et al. Half-molar sodium lactate infusion to prevent intracranial hypertensive episodes in severe traumatic brain injured patients: a randomized controlled trial. Intensive Care Med. 2013;39(8):1413–22 Epub 2013/06/12.
Bourdeaux CP, Brown JM. Randomized controlled trial comparing the effect of 8.4 % sodium bicarbonate and 5 % sodium chloride on raised intracranial pressure after traumatic brain injury. Neurocrit Care. 2011;15(1):42–5 Epub 2011/02/08.
Bourdeaux C, Brown J. Sodium bicarbonate lowers intracranial pressure after traumatic brain injury. Neurocrit Care. 2010;13(1):24–8 Epub 2010/04/28.
Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62(2):307–10 Epub 2007/02/14.
Holcomb JB, Donathan DP, Cotton BA, Del Junco DJ, Brown G, Wenckstern TV, et al. Prehospital Transfusion of Plasma and Red Blood Cells in Trauma Patients. Prehospital Emerg Care: Official J National Assoc EMS Phys National Assoc State EMS Directors. 2015;19(1):1–9 Epub 2014/06/17.
Redmond C, Lipp J. Traumatic brain injury in the pediatric population. Nutr Clinl Pract.: Off Publ Am Soc Parenter Enteral Nutr. 2006;21(5):450–61 Epub 2006/09/26.
Holcomb JB, Pati S. Optimal trauma resuscitation with plasma as the primary resuscitative fluid: the surgeon’s perspective. Hematol/Educ Program Am Soc Hematol Am Soc Hematol Educ Program. 2013;2013:656–9 Epub 2013/12/10.
Sillesen M, Johansson PI, Rasmussen LS, Jin G, Jepsen CH, Imam A, et al. Fresh frozen plasma resuscitation attenuates platelet dysfunction compared with normal saline in a large animal model of multisystem trauma. J Trauma Acute Care Surg. 2014;76(4):998–1007 Epub 2014/03/26.
Dekker SE, Sillesen M, Bambakidis T, Jin G, Liu B, Boer C, et al. Normal saline influences coagulation and endothelial function after traumatic brain injury and hemorrhagic shock in pigs. Surgery. 2014. Epub 2014/06/24.
Jin G, DeMoya MA, Duggan M, Knightly T, Mejaddam AY, Hwabejire J, et al. Traumatic brain injury and hemorrhagic shock: evaluation of different resuscitation strategies in a large animal model of combined insults. Shock. 2012;38(1):49–56 Epub 2012/05/12.
Hwabejire JO, Imam AM, Jin G, Liu B, Li Y, Sillesen M, et al. Differential effects of fresh frozen plasma and normal saline on secondary brain damage in a large animal model of polytrauma, hemorrhage and traumatic brain injury. The journal of trauma and acute care surgery. 2013;75(6):968–74; discussion 74–5. Epub 2013/11/22.
Imam A, Jin G, Sillesen M, Dekker SE, Bambakidis T, Hwabejire JO, et al. Fresh frozen plasma resuscitation provides neuroprotection compared to normal saline in a large animal model of traumatic brain injury and polytrauma. J Neurotrauma. 2015;32(5):307–13 Epub 2014/08/26.
Ott MM, Eriksson E, Vanderkolk W, Christianson D, Davis A, Scholten D. Antiplatelet and anticoagulation therapies do not increase mortality in the absence of traumatic brain injury. J Trauma. 2010;68(3):560–3 Epub 2010/01/13.
Stein DM, Dutton RP, Kramer ME, Scalea TM. Reversal of coagulopathy in critically ill patients with traumatic brain injury: recombinant factor VIIa is more cost-effective than plasma. J Trauma. 2009;66(1):63–72; discussion 3-5. Epub 2009/01/10.
Solbeck S, Meyer MA, Johansson PI, Meyer AS, Cotton BA, Stensballe J, et al. Monitoring of dabigatran anticoagulation and its reversal in vitro by thrombelastography. Int J Cardiol. 2014;176(3):794–9 Epub 2014/08/27.
Pakraftar S, Atencio D, English J, Corcos A, Altschuler EM, Stahlfeld K. Dabigatran etixilate and traumatic brain injury: Evolving anticoagulants require evolving care plans. World J Clin Cases. 2014;2(8):362–6 Epub 2014/08/19.
Imam AM, Jin G, Sillesen M, Duggan M, Jepsen CH, Hwabejire JO, et al. Early treatment with lyophilized plasma protects the brain in a large animal model of combined traumatic brain injury and hemorrhagic shock. J Trauma Acute Care Surg. 2013;75(6):976–83 Epub 2013/11/22.
Teranishi K, Scultetus A, Haque A, Stern S, Philbin N, Rice J, et al. Traumatic brain injury and severe uncontrolled haemorrhage with short delay pre-hospital resuscitation in a swine model. Injury. 2012;43(5):585–93 Epub 2010/11/03.
White NJ, Wang X, Bradbury N, Moon-Massat PF, Freilich D, Auker C, et al. Fluid resuscitation of uncontrolled hemorrhage using a hemoglobin-based oxygen carrier: effect of traumatic brain injury. Shock. 2013;39(2):210–9 Epub 2013/01/18.
Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312(1):36–47 Epub 2014/07/25.
Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. New Engl J Med. 2012;367(26):2471–81 Epub 2012/12/14.
Melhem S, Shutter L, Kaynar A. A trial of intracranial pressure monitoring in traumatic brain injury. Critical Care. 2014;18(1):302. Epub 2014/02/04.
Badri S, Chen J, Barber J, Temkin NR, Dikmen SS, Chesnut RM, et al. Mortality and long-term functional outcome associated with intracranial pressure after traumatic brain injury. Intensive Care Med. 2012;38(11):1800–9 Epub 2012/09/27.
Alali AS, Fowler RA, Mainprize TG, Scales DC, Kiss A, de Mestral C, et al. Intracranial pressure monitoring in severe traumatic brain injury: results from the American College of Surgeons Trauma Quality Improvement Program. J Neurotrauma. 2013;30(20):1737–46 Epub 2013/06/05.
Gerber LM, Chiu YL, Carney N, Hartl R, Ghajar J. Marked reduction in mortality in patients with severe traumatic brain injury. J Neurosurg. 2013;119(6):1583–90 Epub 2013/10/09.
Talving P, Karamanos E, Teixeira PG, Skiada D, Lam L, Belzberg H, et al. Intracranial pressure monitoring in severe head injury: compliance with Brain Trauma Foundation guidelines and effect on outcomes: a prospective study. J Neurosurg. 2013;119(5):1248–54 Epub 2013/08/27.
Dawes AJ, Sacks GD, Cryer HG, Gruen JP, Preston C, Gorospe D, et al. Intracranial pressure monitoring and inpatient mortality in severe traumatic brain injury: A propensity score-matched analysis. J Trauma Acute Care Surg. 2015;78(3):492–501; discussion-2. Epub 2015/02/25.
Oddo M, Levine JM, Mackenzie L, Frangos S, Feihl F, Kasner SE, et al. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery. 2011;69(5):1037–45; discussion 45. Epub 2011/06/16.
Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009;111(4):672–82 Epub 2009/05/26.
Belli A, Sen J, Petzold A, Russo S, Kitchen N, Smith M. Metabolic failure precedes intracranial pressure rises in traumatic brain injury: a microdialysis study. Acta Neurochir. 2008;150(5):461–9; discussion 70. Epub 2008/04/19.
Stein NR, McArthur DL, Etchepare M, Vespa PM. Early cerebral metabolic crisis after TBI influences outcome despite adequate hemodynamic resuscitation. Neurocrit Care. 2012;17(1):49–57 Epub 2012/04/25.
Vespa P, Bergsneider M, Hattori N, Wu HM, Huang SC, Martin NA, et al. Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metabo: Official J Int Soc Cereb Blood Flow Metab. 2005;25(6):763–74 Epub 2005/02/18.
Fletcher JJ, Bergman K, Feucht EC, Blostein P. Continuous renal replacement therapy for refractory intracranial hypertension. Neurocrit Care. 2009;11(1):101–5 Epub 2009/03/10.
Hwabejire JO, Jin G, Imam AM, Duggan M, Sillesen M, Deperalta D, et al. Pharmacologic modulation of cerebral metabolic derangement and excitotoxicity in a porcine model of traumatic brain injury and hemorrhagic shock. Surgery. 2013;154(2):234–43 Epub 2013/07/31.
Pati S, Khakoo AY, Zhao J, Jimenez F, Gerber MH, Harting M, et al. Human mesenchymal stem cells inhibit vascular permeability by modulating vascular endothelial cadherin/beta-catenin signaling. Stem Cells Dev. 2011;20(1):89–101 Epub 2010/05/08.
Liao GP, Harting MT, Hetz RA, Walker PA, Shah SK, Corkins CJ, et al. Autologous bone marrow mononuclear cells reduce therapeutic intensity for severe traumatic brain injury in children. Pediatr Crit Care Med: J Soc Crit Care Med World Federation Pediatr Intensive Crit Care Soc. 2015;16(3):245–55 Epub 2015/01/13.
Cox CS Jr, Baumgartner JE, Harting MT, Worth LL, Walker PA, Shah SK, et al. Autologous bone marrow mononuclear cell therapy for severe traumatic brain injury in children. Neurosurgery. 2011;68(3):588–600 Epub 2010/12/31.
Saw MM, Chamberlain J, Barr M, Morgan MP, Burnett JR, Ho KM. Differential disruption of blood-brain barrier in severe traumatic brain injury. Neurocrit Care. 2014;20(2):209–16 Epub 2013/11/16.
Ferrada P, Evans D, Wolfe L, Anand RJ, Vanguri P, Mayglothling J, et al. Findings of a randomized controlled trial using limited transthoracic echocardiogram (LTTE) as a hemodynamic monitoring tool in the trauma bay. J Trauma Acute Care Surg. 2014;76(1):31–7; discussion 7–8. Epub 2013/12/26.
Kleindienst A, Brabant G, Morgenthaler NG, Emtmann I, Scheufler N, Buchfelder M. The atrial natriuretic peptide does not serve osmoregulation but predicts outcome following brain injury. Acta Neurochir Suppl. 2012;114:277–81 Epub 2012/04/06.
Davis JW, Davis IC, Bennink LD, Hysell SE, Curtis BV, Kaups KL, et al. Placement of intracranial pressure monitors: are “normal” coagulation parameters necessary? J Trauma. 2004;57(6):1173–7 Epub 2004/12/31.
Rowell SE, Barbosa RR, Lennox TC, Fair KA, Rao AJ, Underwood SJ, et al. Moderate elevations in international normalized ratio should not lead to delays in neurosurgical intervention in patients with traumatic brain injury. J Trauma Acute Care Surg. 2014;77(6):846–50; discussion 51. Epub 2014/11/26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Liao, G.P., Holcomb, J.B. (2017). Trauma Resuscitation and Fluid Considerations in the Polytrauma Patient with CNS Injury. In: Ecklund, J., Moores, L. (eds) Neurotrauma Management for the Severely Injured Polytrauma Patient. Springer, Cham. https://doi.org/10.1007/978-3-319-40208-6_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-40208-6_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40206-2
Online ISBN: 978-3-319-40208-6
eBook Packages: MedicineMedicine (R0)