Abstract
The International Pediatric Fistula First Initiative was established in 2005 with the aim of addressing the lack of arteriovenous fistula (AVF) use in the pediatric population. Currently, the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) recommends placing permanent hemodialysis access in all patients with end-stage renal disease (ESRD) aged 0–19 who are greater than 20 kg and are not expected to receive kidney transplantation within one year. Thus anyone who is expected to be on dialysis greater than one year and meets the age and size criteria should have a permanent arteriovenous fistula placed.
Although most pediatric patients who initiate renal replacement therapy meet these criteria, nearly 90 % of children start treatment via central venous catheter instead of an AVF. This chapter discusses issues pertinent to pediatric hemodialysis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Background
The International Pediatric Fistula First Initiative (IPFFI) was established in 2005 with the aim of addressing the lack of arteriovenous fistula (AVF) use in the pediatric population [1]. The IPFFI was a collaborative effort with the Midwest Pediatric Nephrology Consortium, whose aim was to increase awareness among providers (nephrologists, surgeons, and dialysis staff) that fistulae are the best access in the pediatric hemodialysis population.
Currently, the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) recommends placing permanent hemodialysis access in all patients with end-stage renal disease (ESRD) aged 0–19 who are greater than 20 kg and are not expected to receive kidney transplantation within one year. Thus anyone who is expected to be on dialysis greater than one year and meets the age and size criteria should have a permanent arteriovenous fistula placed.
Although most pediatric patients who initiate renal replacement therapy meet these criteria, approximately 90 % of children start treatment via central venous catheter instead of an AVF. Furthermore up to 80 % of pediatric patients with central venous catheters (CVC) have a “permanent” catheter in place [2]. Additionally as many as 50 % of the permanent catheters are placed in the subclavian vein as opposed to the internal jugular vein, exacerbating associated central vein stenosis that occurs with prolonged catheter-based hemodialysis [3].
Incidence of ESRD and Trends in Renal Replacement Therapy in the Pediatric Population
According to the United Stated Renal Data System (USRDS) reports, the incidence of ESRD in the pediatric population aged 0–19 years was 1,161 and was up to 1,462 in 2013; while the cummulative prevalence of children with ESRD as of December 31,2013 was 9,921 [4]. This is compared to the incidence of 117,162 adult patients in the 2013. The reported incidence of ESRD in the pediatric population appears to have peaked in 2003 and has been steadily decreasing since that time. Since the initiation of data collection in 1992, the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) reports no significant change in the pattern of incidence of ESRD in pediatric population when looking by age, race, or gender; thus, these rates are anticipated to remain stable [2]. The USRDS reports hemodialysis is the most common index treatment for new-onset ESRD in the pediatric population. Other less common treatments are preemptive kidney transplantation and peritoneal dialysis.
Evaluating trends of index treatments for ESRD, there has been a shift toward patients being treated with hemodialysis initially compared to peritoneal dialysis, presumably because of readily available CVCs. The USRDS data shows that hemodialysis has consistently been the most common form of index treatment for ESRD patients, the majority initiating HD therapy via CVCs. Elaborating on index treatment for the year 2013, 816 (55.8%) of patients diagnosed with ESRD started treatment with hemodialysis, 367 (25.1%) initiated ESRD treatment with peritoneal dialysis, and 267 (18.3%) did so with index transplantation [4]. Compared to adults where index transplantations are rare and most initiate treatment with hemodialysis, there is a wider distribution of index treatment types in the pediatric population. The index treatment for adults, in 2013, was hemodialysis in 88.4% of patients, peritoneal dialysis in 9.0% and only 2.6% of adults initiated ESRD care with index transplantation. As many as 37 % of newly diagnosed children with ESRD undergo transplantation within 1 year of starting ESRD care, and of the 9,921 pediatric patients receiving ESRD care in 2013, 6,739 (67.9%) have undergone a kidney transplantation. It is difficult to explain to the parents that their child needs a permanent AVF when they are likely to proceed to transplantation prior to initiation of dialysis or after a short course of dialysis with a temporary HD catheter.
The total number of pediatric patients undergoing hemodialysis in 2011 was 3,363 patients or 42 % of all those receiving ESRD treatment. According to the NAPRTCS 2011 data of those 3,363 patients on HD, 78 % were receiving HD via external percutaneous catheters, 0.3 % via external AV shunts, 11.8 % via internal arteriovenous fistula, and 6.7 % via internal AVG. Of the external percutaneous catheters, the majority were placed in the subclavian vein (51.1 %), 43.7 % in the jugular vein, and 4.2 % in the femoral vein. Interestingly, despite the recognized measures and efforts to increase arteriovenous fistula placement, the use of external percutaneous catheters for HD at initiation of therapy has increased from 73 % in 1992 to >90 % of all HD access in 2010. Meanwhile in the same time period, the use of internal arteriovenous fistula for HD at initiation of treatment has decreased significantly from 12 % in 1992 to ~ 1 % in 2010.
Morbidity and Mortality of ESRD in the Pediatric Population
ESRD in the pediatric population, as it does in the adult population, confers an increased morbidity and mortality on those affected compared to the general population. The five-year survival for all pediatric ESRD patients evaluated from 2003 to 2007 was reported as 89 % with the youngest age groups having the lowest overall survival. The one-year survival for ESRD patients aged 0–1 years old is 88.9 %; it increases slightly with age being 95 % for ages 2–5, 97.5 % for ages 6–12, and 98.2 % for those older than 12. The three-year survival for these patients by age group is 75.1 %, 89.6 %, 94.3 %, and 95.4 %, respectively. Finally the five-year survival for those ages are 75 %, 86 %, 90 %, 94 %, respectively. Broken down by modality of treatment, the reported survival is highest for transplant patients which have a five-year survival of 95 %, followed by peritoneal dialysis patients whose 5-year survival is 81 %, and finally 76 % for hemodialysis patients.
The causes of mortality for pediatric ESRD patients are multiple; however, the most commonly cited cause is cardiopulmonary complications, responsible for 21 % of all deaths. Characterized by age, cardiopulmonary disease claims 22.8 % of all deaths in children aged 0–1 years old, 18.3 % for those aged 2–5, 19.1 % of ages 6–12, and 22.1 % of deaths in children 13 or older. The next most common culprits of mortality in pediatric ESRD patients are infections, of which bacterial infections account for 11.1 % of deaths. By age, infectious causes are responsible for 14.6 % of deaths for children 0–1 years old, 9.9 % for those aged 2–5, 5.7 % for those aged 6–12 years old, and 12.9 % of deaths among children aged 13 or older.
Morbidity in ESRD pediatric patients is another serious issue, leaving room for improvement. Pediatric ESRD patients average 1.5 hospitalizations per patient per year. Comparing the two latest USRDS reporting blocks 2002–2006 and 2007–2011, there was an increase in all-cause hospitalizations of 17.2 %. When grouped by mode of renal replacement therapy for the same time block periods, there was an increase in cardiovascular-related hospitalizations by 33.9 % among hemodialysis patients and by 24.5 % among peritoneal dialysis patients, while transplant patients had a decrease in cardiovascular-related hospitalization of 7.8 %. In terms of infectious-related hospitalization, there was a decrease of 4.9 % among hemodialysis patients, while both peritoneal dialysis patients and transplant patients had an increase in infection-related hospitalization by 4.3 % and 25 %, respectively.
Etiology of ESRD on the Pediatric Population
The USRDS compiles a broad table depicting the categories and individual diagnoses responsible for ESRD in children. This data shows little change in the etiologic patterns for ESRD in the latest reporting period compared with previous years. The current reports include data from 2008 to 2012 and compare it to previous reporting period of 2003–2005. The leading group of disorders responsible for ESRD in patients aged 0–19 is cystic/hereditary/congenital disorders accounting for 38.3 % of cases in the current time period (compared to 33.5 % in previous time period). This is followed by glomerular diseases which are responsible for 23 % of ESRD (24.7 % previously) and secondary causes of glomerulonephritis attributed to 11.3 % of patients (11.4 % previously). The most common individual diagnosis causes of ESRD include renal hypoplasia/dysplasia (11.9 %), congenital obstructive uropathies (8.8 %), specifically of the uteropelvic junction (0.7 %), uterovesical junction (0.9 %), focal glomerular sclerosis (12.4 %), and lupus erythematosus (5.7 %).
African American children have a significantly higher percentage of certain nephropathies related to systemic diseases. African American children make up 90 % of all children affected with sickle cell nephropathy. Human immunodeficiency virus (HIV)-related nephropathy patients in the current reporting period are 100 % African American which is an increase from 86.4 % in previous reporting years. Finally among those affected by lupus nephropathy, 59 % are African American (increased from 50.4 % in previous years) (Fig. 24.1).
Patient Selection
Despite having the knowledge that fistulae are better than catheters, many parents and/or patients still select catheters over fistulae in the pediatric population. This may be as a result of a multiple issues, preconceived notions, or unintentional provider bias [5]. The selection of access for initiation of treatment depends largely on what information is provided by caregivers but also relies on preconceived notions about ESRD, parent and caregiver biases, and the age and maturity of the child. When evaluated by vascular surgeons, many of these children already have CVCs in place and have initiated hemodialysis. Regardless, there should be a complete discussion of the benefits of AVF over CVCs, and ample time for making an informed decision should be given.
While anecdotally there are many factors that limit placing AVF in children, few studies have been done to study these barriers. A recent publication by Chand and colleagues describes some of these barriers and identifies communication issues between providers as a major issue, in addition to lack of standardized referral practices for CKD patients, lack of standardization as to whom the patients should be referred to, and finally lack of early communication between surgeons and interventional radiologists and dialysis staff (nephrologists, nurse practitioners, dialysis nurses) regarding problematic fistulae [5]. Similarly, few studies have assessed the psychosocial aspects of decision-making in choosing a form of dialysis access in the pediatric population. As one might imagine, for younger patients the decision is up to the parents and caregivers, which may place a huge burden on them. Once a child is able to express desires and dislikes, even without necessarily completely understanding all the options, the decision is often left up to them or at least made with their preference in mind. In our own practice, some of the reasons given a patient might not want a fistula include fear of needles, inability to wear jewelry at the site of an AVF, inability to participate in sports, ugly appearance of fistulae, and desire for the fistula to remain unseen. Parents also voice concerns with fistula placement which include the uncertainty of knowing what is best for their child despite receiving all the data supporting fistulae over catheters and the hope that a more “permanent” solution is approaching and that the “bridge to transplant” could be accomplished with a central venous catheter. In another survey by Brittinger and colleagues, assessing the pediatric patients’ discomfort with cannulation, 39 % of patients reported no discomfort, 39 % had tolerable discomfort, and 22 % reported great discomfort. Interestingly, 95 % of the participants reported they would prefer not to revert to central venous catheter for access [6].
Larger studies are needed to identify barriers to fistula placement, and even further projects are needed to address these barriers and offer solutions. Despite having the knowledge that autogenous access is better than CVCs, many patients and families still select CVCs over AVFs for access. As providers we use CVCs first in 90 % of the pediatric population, and thus both patients and their caregivers may be resistant to change or to undergo another (more invasive) procedure once a central venous catheter is in place. Efforts to educate families at an earlier stage, before initiation of any treatment, should be pursued. A campaign to place AVF in patients months before they start dialysis is ideal; thus, nephrologists and surgeons should communicate frequently and early about these patients such that AVF surgery can be completed in a timely fashion.
Central Venous Catheter Use in the Pediatric Population
Several studies have investigated the reasons for CVC preference among pediatric patients undergoing hemodialysis. Fadrowski and colleagues retrospectively analyzed a cohort of 1,284 patients from 2001 to 2003 [7]. In this cohort, 755 (59 %) had a central venous catheter. The reasons given for choosing a central venous catheter included “small body size” in 142 (18.8 %), having “maturing” AVF/AVG in 53 (7 %) patients, and a “transplant scheduled” in 83 (10.9 %) of patients. Among these 755 patients, 32.2 % did receive a transplant within the year. In another retrospective cohort study published in 2006 by the same group looking at ESRD patients aged 12–18 years old receiving HD for the year 2000, the authors quantify the increased risks attributable to CVCs compared to patients with arteriovenous fistula [8]. The authors included 418 patients, 41 % of whom had an arteriovenous fistula or graft and 58 % had central venous catheter. Data analysis revealed an increased relative risk among central venous catheter patients with regard to all-cause hospitalization (RR 1.84 CI 1.38–2.44), hospitalizations due to infections (RR 4.74 CI 2.02–11.14), and complications of vascular access (RR 2.72 CI 2.00–3.69).
The durability of CVCs, while improved in recent years with smaller profile catheters, still remains inferior to AVF and averages between 4 and 10 months and in some cases is under 1 month. Several groups have published data on the longevity of CVCs and investigated the reasons they fail [9–11]. Central venous catheter durability ranges from 0 to 62 % at 1 year, and failure is attributed to infection (17 %), thrombosis (33 %), extrusion (5.4 %), and kinking (which is more common in smaller catheters). In general, cuffed catheters carry a lower risk of infection and have a longer durability (months) when compared to non-cuffed catheters.
One of the major long-term complications of central venous catheter placement is central venous stenosis. In an attempt to minimize this complication, NKF-KDOQI has delineated management in the event that a central venous catheter is placed in children [12]. The recommendation lists, in order of preference, the right internal jugular vein, right external jugular vein, left internal and external jugular veins, subclavian veins, femoral veins, and finally translumbar and transhepatic access to the IVC.
The prevalence of central venous stenosis associated with a history of subclavian central venous catheter placement is 25–50 % [3, 13–15]. In a recent case report, the author brings to light the fact that central vein stenosis might be grossly underdiagnosed, and as surgeons we likely are only seeing the cases that are significantly stenotic enough to cause symptoms [15]. In this report, however, it is not only hemodialysis-related access which was identified as a risk factor for developing central venous stenosis but rather the use of both tunneled and non-tunneled dialysis catheters, peripherally inserted central catheters (PICC), as well as other CVCs and ports. The length and duration of the catheter and multiple catheters are two factors most closely associated with developing central venous stenosis. A 2012 retrospective review evaluated failure rates of arteriovenous fistulae in adult patients with a history of ipsilateral vs. contralateral catheters [14]. Their results indicate that while maturation times and primary failure rates were similar in both groups, there was a lower cumulative fistula survival at 2 years in patients with ipsilateral catheters compared to contralateral catheters (54 % vs. 74 %). This result is echoed in other publications in the adult population [3, 15, 16]. This phenomenon however has not been demonstrated in the pediatric population. In a study by Wartman and colleagues, catheter history did not affect patency of arteriovenous fistulae after surgery [17]. Thus if a pediatric patient has had a central venous catheter, this does not become a contraindication for ipsilateral arteriovenous fistula creation, although if central venous stenosis is clinically suspected, it should be ruled out as this could confer long-term complications.
Central Venous Catheter Technical Considerations
Central venous catheters may be either non-tunneled or tunneled. These can be placed percutaneously under moderate sedation and local anesthetic; however, tunneled catheters in the pediatric population often require general anesthesia to ensure patient compliance.
Major challenges in establishing central venous access for hemodialysis in children are that there are no evidence-based rules for selection of catheter size and that the pre-curved catheters commercially available for children are limited to larger sizes. Larger catheters offer higher volumes during dialysis, but the size of the child and his or her vessels limits the size of the catheter that can be used. Catheters that are smaller mean that the length of dialysis sessions has to be longer with slower flows. A useful formula that has proved safe in selecting catheter size is [Size (Fr) = Age +/− 2]. Taking the age of the child and converting it to the diameter, in French measurement, with adjustments after physical examination of the child to reduce the size if the patient is small for age or increase size if the child is larger than peers the same age. Pre-curved catheters available for the adult populations make percutaneous and subcutaneous tunneling possible; however, these catheters are largely not available in the smaller sizes for the youngest of pediatric ESRD patients. In these patients placing a tunneled central venous catheter usually means forcing the curve during placement and making one or more counter incisions over the access vessel for accurate and precise placement.
AV Access Use in the Pediatric Population
AVF is the preferred form of access for pediatric patients undergoing hemodialysis as AVFs have superior outcomes when compared to CVCs. In a recent retrospective review, 93 pediatric patients aged 3–19 (mean 14 years old, 70 % male, weight ranged between 12 and 131 kg) undergoing fistula operations were reviewed. In this review, 82 % of the patients were already receiving hemodialysis at the time of surgery for an average time span of 18 months. Most of the patients (78 %) had a history of central venous catheter placement, and 24 % of these patients had multiple catheters placed. The group performed 101 fistula procedures: 43 radiocephalic AVF, 29 brachiocephalic AVF, 20 basilic vein transpositions, and 9 femoral vein transpositions. The primary and secondary patency rates were 83 % and 92 %, respectively, at 2 years and 65 % and 83 %, respectively, at 4 years. Older age was shown to correlate with improved primary patency [17].
Many others have published on the feasibility of placing arteriovenous fistulae in pediatric populations with good outcomes. Bagolan and colleagues described their experience placing Cimino fistulae in children and reported a 4-year follow-up with 63.5 % patency and a complication rate of 35 % of which thrombosis was the most common [18]. A retrospective review in a single institution demonstrated that IPFFI is feasible in a pediatric population and also reported on the successful use of the operating microscope in small children [19].
Arteriovenous Fistula Access: Technical Considerations
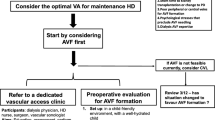
As with central line placement, the NKF-KDOQI publishes guidelines for a structured approach for the placement of AVF access [12]. The recommended order for arteriovenous fistula in the pediatric population is as follows: radiocephalic AVF, followed by brachiocephalic AVF, and lastly basilic vein transposition. The techniques for standard radiocephalic, brachiocephalic, and basic vein transposition AVFs are widely described and discussed in different chapters in this book. When applied to the pediatric populations, there are some additional considerations. As in the adult population, planning of access starts with a complete history including previous central venous access use and a thorough physical exam with a detailed vascular exam and vein mapping on all patients. Vein mapping should then be evaluated by the operating surgeon for suitability of vein size. A size cutoff of 2.0 mm is acceptable in forearm veins, and 2.5 mm cutoff for upper arm veins has been shown to have success rate in maturation [17].
Vein imaging should also be routinely performed intraoperatively once the patient is placed under anesthesia. One of the attributes unique to pediatric vessels is their intense vasospastic response with handling. To reduce this response, tourniquet occlusion can be used for arterial control during fistula construction in lieu of arterial clamping. Additionally, based on surgeon preference an operating microscope might be used; however, loupe magnifications should be the standard of care in all pediatric fistulae. Standard end-to-side anastomosis using a continuous running monofilament suture is recommended in the pediatric population, while interrupted suture placement is not necessary.
Finally, transposition (brachial or femoral) can be performed in either one- or two-stage procedure. Groin fistulae have also been successfully placed in pediatric populations, in the setting of unavailable upper extremities or patient preference as described by Gradman and colleagues. The technique for this is similar to that described in adults [20]. The reported primary patency for the femoral vein transposition was 100 % and 96 % at 1 and 2 years, respectively, and secondary patency reported to be 100 %.
Future Outlook
In order to optimize the care and future of patients with ESRD, we propose to minimize interventions in children as much as possible. This means that all those involved in the care of a child progressing toward ESRD are mindful and plan ahead in order to foresee what the child will need in the future. Early referral to well-trained experts for thorough discussion on types of dialysis and treatment options, in addition to referral to vascular surgeons, is essential. Planning ahead can potentially prevent urgent use of short-lived, morbid, and potentially damaging CVCs. Given the information available to patients over the Internet or from personal acquaintances, one must be mindful of preexisting biases to ensure that each family gets accurate and complete information. As our own experience with obtaining consent has demonstrated, decisions are often made by young teens or children who may not have gathered all of the necessary information to make the best decision. As permanent tunneled catheters may have longer durability and as the time to transplant is shorter compared to that in adults, children who present to a surgeon with a preexisting CVC may potentially avoid a second procedure if transplant comes prior to AVF placement.
If a child must have a central venous catheter because of acute presentation or personal preference, central venous catheter guidelines should be followed: placement in the internal jugular vein is preferred over the subclavian vein, and simultaneous referral to an access surgeon is recommended.
Fistulae in the pediatric population, including in very small children, are both technically feasible and have good long-term outcomes. Taking into consideration certain technical differences in the pediatric population, vascular surgeons can be equipped with the tools needed to be successful in fistula creation. Finally, remembering that diseases in children are psychosocially challenging for all involved, each child and his or her family must be given complete and accurate information, in addition to ample time to process this information, and support in making a decision.
Conclusion
The current state of establishing pediatric hemodialysis access is complex and has yet to become standardized. Both USRDS and NAPRTCS data indicate that a large majority of patients initiate dialysis treatment with CVCs despite published and peer-reviewed data indicating that arteriovenous fistulae are superior to catheters. CVCs are associated with more complications, hospitalizations, and shorter access life span when compared to arteriovenous fistulae. Since the initiation of the IPFFI, there has been little progress in the campaign to create fistulae first in children. A handful of barriers to fistula placement have been identified but remain to be addressed. The USA lags behind the international community in pediatric-arteriovenous fistula placement and use. Given that the majority of the pediatric population will likely outlive at least one transplant and return to dialysis, providers should avoid using CVCs given the long-term complications that can hinder the patient’s access options in the future. CVCs should be reserved for urgent needs or for those who have a transplantation scheduled. Finally, educational material like that used in IPFFI should be widely distributed nationally and not limited to providers but also shared with patients. Each dialysis center should standardize their referral patterns and follow-up practices and, wherever possible, a vascular surgeon or a surgeon with expertise in microvascular anastomoses should be selected.
References
Chand DH, Valentini RP. International pediatric fistula first initiative: a call to action. Am J Kidney Dis. 2008;51(6):1016–24.
NAPRTCS North American Pediatric Renal Trials and Collaborative Studies: 2011 Annual Dialysis Report. Available at: https://web.emmes.com/study/ped/annlrept/annlrept.html. 2011.
Lacson Jr E, et al. Balancing fistula first with catheters last. Am J Kidney Dis. 2007;50(3):379–95.
USRDS United States Renal Data System: Pediatric Hemodialysis. Available at: USRDS.org. 2015, Ch 8.
Chand DH, et al. Barriers, biases, and beliefs about arteriovenous fistula placement in children: a survey of the international pediatric fistula first initiative (IPFFI) within the Midwest pediatric nephrology consortium (MWPNC). Hemodial Int. 2015;19(1):100–7.
Brittinger WD, et al. Vascular access for hemodialysis in children. Pediatr Nephrol. 1997;11(1):87–95.
Fadrowski JJ, et al. Patterns of use of vascular catheters for hemodialysis in children in the United States. Am J Kidney Dis. 2009;53(1):91–8.
Fadrowski JJ, et al. Clinical course associated with vascular access type in a national cohort of adolescents who receive hemodialysis: findings from the clinical performance measures and US renal data system projects. Clin J Am Soc Nephrol. 2006;1(5):987–92.
Goldstein SL, Macierowski CT, Jabs K. Hemodialysis catheter survival and complications in children and adolescents. Pediatr Nephrol. 1997;11(1):74–7.
Sharma A, et al. Survival and complications of cuffed catheters in children on chronic hemodialysis. Pediatr Nephrol. 1999;13(3):245–8.
Sheth RD, et al. Successful use of Tesio catheters in pediatric patients receiving chronic hemodialysis. Am J Kidney Dis. 2001;38(3):553–9.
NKF-DOQI National Kidney Foundation-Dialysis Outcomes Quality Initiative. NKF-KDOQI clinical practice guidelines for vascular access. 2006. Am J Kidney Dis. Available at: https://www.kid-ney.org/professionals/guidelines/guidelines_commentaries.
Barrett N, et al. Subclavian stenosis: a major complication of subclavian dialysis catheters. Nephrol Dial Transplant. 1988;3(4):423–5.
Shingarev R, Barker-Finkel J, Allon M. Association of hemodialysis central venous catheter use with ipsilateral arteriovenous vascular access survival. Am J Kidney Dis. 2012;60(6):983–9.
Agarwal AK. Central vein stenosis. Am J Kidney Dis. 2013;61(6):1001–15.
Teruya TH, et al. Symptomatic subclavian vein stenosis and occlusion in hemodialysis patients with transvenous pacemakers. Ann Vasc Surg. 2003;17(5):526–9.
Wartman SM, et al. Outcomes with arteriovenous fistulas in a pediatric population. J Vasc Surg. 2014;60(1):170–4.
Bagolan P, et al. A ten-year experience of Brescia-Cimino arteriovenous fistula in children: technical evolution and refinements. J Vasc Surg. 1998;27(4):640–4.
Chand DH, et al. A vascular access team can increase AV fistula creation in pediatric ESRD patients: a single center experience. Semin Dial. 2009;22(6):679–83.
Gradman WS, et al. Experience with autogenous arteriovenous access for hemodialysis in children and adolescents. Ann Vasc Surg. 2005;19(5):609–12.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Leong, B.V., Wartman, S.M., Rowe, V.L. (2017). Considerations in Pediatric Hemodialysis Access. In: Shalhub, S., Dua, A., Shin, S. (eds) Hemodialysis Access. Springer, Cham. https://doi.org/10.1007/978-3-319-40061-7_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-40061-7_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40059-4
Online ISBN: 978-3-319-40061-7
eBook Packages: MedicineMedicine (R0)