Abstract
It is a common symptom in at least one-third of the patients over the age of 65 years. Benign positional vertigo, vestibular neuronitis and Meniere’s diseases are the commonest causes of vertigo. Other causes include vertebrobasilar insufficiency, migraine, multiple sclerosis and cerebellar neoplasms.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
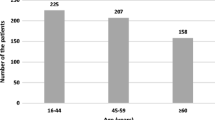
The overall incidence of dizziness, vertigo and imbalance is 5–10% and reaches 40% in patients over the age of 40 years [1]. It is a common symptom in at least one-third of the patients over the age of 65 years [2]. One-year prevalence was 48.3% for vertigo, 39.1% for unsteadiness and 35.6% for dizziness [3]. Vertigo accounts for 52% of all cases [4, 5] and up to 56.4% in the elderly [6]. Overall prevalence in a rural community was 0.17% [7]. The prevalence of vertigo secondary to cardiovascular disease was 0.32%, for neurological disease 0.14% and otologic disease 0.08% in a study of vertigo in an adult rural population [7]. In a study of 187 Chinese patients with vertigo, posterior circulation ischaemia was 59.8% followed by BPPV with 16.04%, and less affected were migraine, Meniere’s disease and vestibular neuronitis, among others [8]. Epidemiological studies indicated that a quarter of the dizziness were central, and the most common central causes were cerebrovascular disease, migraine, multiple sclerosis and tumours of the posterior fossa [9] (Table 1).
Causes of Vertigo
Benign positional vertigo, vestibular neuronitis and Meniere’s diseases are the commonest causes of vertigo. Other causes include vertebrobasilar insufficiency, migraine, multiple sclerosis and cerebellar neoplasms [10].
Benign Positional Paroxysmal Vertigo (BPPV)
BPPV is a common cause of vertigo in the elderly and becomes more frequent as age advances [11] and is most prevalent in those above the age of 50 years [12]. It is most common among peripheral vestibular disorders [13]. About 9% of a group of urban-dwelling elderly were found to have undiagnosed BPPV [14]. It is nearly always a benign condition [15]. BPPV causes nausea, vertigo, light-headedness and imbalance brought about by change in the position of the head [16], for instance, turning over in bed or getting out of bed. Tipping the head backwards as to reach for the upper shelf may precipitate it. Symptoms can be subjective or objective [12].
Degeneration of the vestibular system is the most common cause. Two basic theories of the pathology in BPPV are cupololithiasis and canalithiasis [17]. Other causes are infection, head injury, minor strokes involving the anterior inferior cerebellar artery and medications such as gentamicin [18], but in more than half of the cases, the cause is unknown. Small crystals of calcium carbonate (otoconia), derived from the utricle as the result of damage to the utricle by injury, infection or degeneration because of advancing age, migrate into the canal system.
The history of vertigo or dizziness brought on by lying down or rolling over in bed together with the physical findings and auditory and vestibular tests helps in the diagnosis. The only diagnostic test that confirms the diagnosis of BPPV is Dix-Hallpike manoeuvre [16]. The individual is brought from a sitting position to the supine with the head turned 45° to the side and extended about 20° backwards. A positive response would be after a short latent period; there is a burst of rotating nystagmus. When the individual is brought up to the sitting position, there will be a reversal of the nystagmus. Fatigue of the nystagmus occurs when the procedure is repeated. Electronystagmography (ENG) may be needed to look for the character of the nystagmus induced by this manoeuvre. The vertigo is intermittent and is self-limiting and usually subsides in about 2 months but could last longer. The Epley manoeuvre and the Semont manoeuvre are intended to move the otoconia out of the sensitive part of the ear to less sensitive location with a cure rate of approximately 80% [19]. Positional restriction after canalith reposition manoeuvres for BPPV has been shown to be of no proven benefit [20].
Vestibular Neuronitis
Vestibular neuronitis is a benign disorder characterized by sudden onset of severe vertigo with nausea and vomiting and ataxia [21]. Hearing loss (unilateral) may be present [16]. It is often preceded by a viral illness which may be subclinical and all common viruses have been implicated. The virus selectively affects the inner ear neurosensory structures. Gradual resolution occurs over few days and complete recovery within 3 months. The elderly however could have exacerbations, usually less severe, and the conditions may be recurrent. Treatment is symptomatic with stabilizing measures and vestibular suppressant medication and rehabilitation exercises [22].
Meniere’s Disease
Meniere’s disease commonly presents in the 40–69 years of age. It is caused by idiopathic endolymphatic hydrops causing swelling of the semicircular ducts and damaging the hair cells. There is fluctuating hearing loss, tinnitus with vertigo and aural fullness and pressure [23]. Vertiginous episodes are paroxysmal lasting minutes to hours and decrease in frequency after multiple attacks only to recur months or years later, eventually with the hearing loss becoming permanent. The first line of treatment is medical which includes a low-salt diet, diuretic (thiazide) [18] and a betahistine, although the efficacies of these treatments have not been proven [24, 25]. Surgical treatment includes labyrinthectomy, vestibular nerve section, endolymphatic sac surgery and chemical ablation using intratympanic gentamicin in patients who have failed medical treatment.
Vertebrobasilar Insufficiency
Abrupt onset with nausea and vomiting and vertigo is the initial symptom in half of the cases. Other symptoms include drop attacks, diplopia, visual hallucinations and visual field defects in conjunction with dysarthria, dysphagia, sensory loss and hemiparesis. It rarely causes isolated vertigo attacks [26]. In impending infarction in the territory of the anterior inferior cerebellar artery, a transient vertigo may be the initial and only complaint. The risk of cerebral infarction following a vertebrobasilar TIA is much less than in the carotid circulation.
Acoustic Neuroma
Acoustic neuroma comprises about 90% of all cerebellopontine angle tumours. It arises from the eight nerves and is retrocochlear in location. The symptoms begin insidiously with mild hearing loss, tinnitus, vague dizziness, disturbance of balance and asymmetric hearing loss. In a small number of patients, the onset is sudden [27]. The cranial nerves, facial and trigeminal (diminished corneal reflex), may be involved by the tumour extending in the cerebellopontine angle, and brain stem compression may occur if untreated. Bilateral acoustic tumours are rare except in patients with neurofibromatosis.
Multiple Sclerosis
Multiple sclerosis is an important cause of central vertigo. Because of the transient nature of these attacks, days to weeks [16], it may be mistaken for one of the self-limiting peripheral causes of vertigo such as vestibular neuronitis [16]. The patients affected are younger than those with benign positional vertigo. The first symptom is often an acute optic neuritis with loss of central vision in one eye, which in most instances resolves. Involvement of the brain stem may produce double vision, dizziness, cerebellar ataxia, dysarthria, dysphagia, numbness of one side of the face and an unsteady gait.
Migraine-Associated Vertigo
This is an atypical form of aura and the dizziness antedates the headache. Individuals with basilar migraine may complain of recurring headaches associated with visual aura followed by vertigo, dysarthria, tinnitus, visual disturbances and unsteadiness in walking [16]. At times, there may be no headache, making the diagnosis difficult. Dietary changes and tricyclic antidepressant generally improve vertiginous migraine headaches [22].
Evaluation
The evaluation of vertigo involves (1) medical history including a drug history, (2) physical examination, (3) laboratory evaluation, (4) vestibular function tests and (5) other diagnostic tests as needed. The medical history is important since the description of each symptom together with the duration and precipitating factors is crucial in establishing the diagnosis. In more than three-quarters of the cases of vertigo, the diagnosis can be made on the history alone. Recurrent vertigo is more suggestive of BPPV, Meniere’s disease or migraine, whereas a single attack lasting for days or more is due either to cerebellar infarction or vestibular neuronitis [26]. Physical examination would include examination of the ear and a neurological examination.
If the patient has true vertigo, the task is one of determining whether it is central or peripheral. Box 1 shows some of the distinguishing characteristics of central and peripheral vertigo [16, 28]. Evidence of brain stem symptoms rules out a peripheral lesion. However, the absence of brain stem symptoms does not exclude a central lesion. Multiple sclerosis and vertebrobasilar insufficiency presenting with isolated vertigo evolve gradually, and the diagnosis may not be apparent at the time of initial presentation. In one study, seven patients had sudden bilateral hearing loss, tinnitus and vertigo, and the initial diagnosis was acute labyrinthitis or Meniere’s disease, until the other brain stem and cerebellar signs appeared [29]. In multiple sclerosis, there are recurrent episodes, with remissions, and in the case of vertebrobasilar insufficiency, prior history of cerebrovascular disease or cardiovascular disease will be helpful in making the distinction. Episodes of vertigo, hearing loss and tinnitus associated with Meniere’s disease can mimic those of acoustic neuroma, and the distinction between them before the appearance of brain stem symptoms can be difficult. The hearing loss with acoustic neuroma however is steadily progressive, whereas it is fluctuating or episodic with Meniere’s disease. Triggering factors and duration of the attacks can help in determining the peripheral causes of the vertigo. In BPPV, the vertigo is with changes in the position of the head and neck, lasts only a few minutes and is recurrent daily. A single severe episode of vertigo after a viral illness is usually due to vestibular neuronitis.
Box 1 Some Characteristics of Peripheral Vertigo and Central Vertigo
Symptoms and signs | Peripheral | Central |
|---|---|---|
Severity | Severe | Less severe |
Nystagmus | Always present | Less often |
Horizontal | Multidirectional | |
Plane, usually | Pure vertical | |
Mixeda | ||
Hearing | Common | Rare |
Tinnitus | May occur | Rare |
Vomiting/nausea | Virtually always | Less frequent |
Present and severe | ||
Neurological | Rare | Common |
Neurological and audiological testing can be helpful in making the distinction. Routine laboratory tests would include a full blood count, sedimentation rate and thyroid function tests, among others. The Dix-Hallpike manoeuvre should be done if the history is suggestive of benign positional vertigo or if the nystagmus is inducible. Vestibular function tests are the Dix-Hallpike manoeuvre, electronystagmography and the rotational chair testing. Audiometry, electronystagmography and brain stem evoked potentials are most useful. The sensitivity of brain stem evoked auditory potentials to detect retrocochlear lesions for acoustic tumours >2 cm is 100% as with MRI [30]. The MRI is used to exclude retrocochlear pathology. To ensure the diagnosis of acoustic neuroma, T1-weighted magnetic resonance imaging with gadolinium (Gd-DTPA) is the gold standard [31], is sensitive and will detect extremely small tumours of 2 mm in size. This technique also identifies other intracranial tumours, meningiomas and demyelinating lesions in the central nervous system. More recently, MR protocols have been used for fast-spin-echo (FSE) imaging [31, 32] for internal auditory canal structures and do not require contrast medium. Three-dimensional fast imaging employing steady-state acquisition (3D-FIESTA) MRI is a sensitive method for the diagnosis of cochlear or retrocochlear lesions and is useful as a screening tool in patients with unilateral ear symptoms [33]. CT scan may be used for inner ear pathology when MRI is not available or when MRI is contraindicated or when tumours more than 1.5 cm in diameter are excluded. Acoustic neuromas are isodense with the brain tissue and intravenous contrast enhancement should be used.
Impact
Dizziness is common in medical practice and is known to impair the health-related quality of life (HR-QoL) [34,35,36]. It affects daily functioning and is associated with functional disability, falls, social isolation and institutionalization [37, 38]. In a study to determine the impact of dizziness and balance disorders in persons >65 years old, balance problems were seen to be associated with unsteadiness, vertigo and faintness and difficulty in walking on uneven surfaces [39]. Approximately in one in five patients, medication triggered the balance problem [39] (Box 2).
Box 2 Key Points: Vertigo
Epidemiological studies indicated that a quarter of the dizziness were central, and the most common central causes were cerebrovascular disease, migraine, multiple sclerosis and tumours of the posterior fossa [9].
BPPV is a common cause of vertigo in the elderly and becomes more frequent as age advances [11].
The only diagnostic test that confirms the diagnosis of BPPV is Dix-Hallpike manoeuvre [16].
In Meniere’s disease, there is fluctuating hearing loss, tinnitus with vertigo and aural fullness and pressure [23].
Vertebrobasilar insufficiency rarely causes isolated vertigo attacks [26].
In a small number of patients with acoustic neuroma, the onset was found to be sudden [27].
Multiple sclerosis is an important cause of central vertigo.
Dietary changes and tricyclic antidepressant generally improve vertiginous migraine headaches [21].
Multiple Choice Questions
-
1.
The following relating to vertigo are correct except:
-
A.
Benign positional paroxysmal vertigo (BPPV) is a common cause of vertigo in the elderly and becomes more frequent as age advances.
-
B.
Meniere’s disease eventually results in permanent deafness.
-
C.
A transient vertigo may be the only complaint in impending infarction in the territory of the anterior cerebellar artery.
-
D.
Migraine-related vertigo is always accompanied by headache.
-
A.
-
2.
The following are true in relation to the different causes of vertigo except:
-
A.
The only diagnostic test that confirms the diagnosis of benign paroxysmal positional vertigo (BPPV) is Dix-Hallpike manoeuvre.
-
B.
The Epley and the Semont manoeuvres have a cure rate of approximately 80% in patients with BPPV.
-
C.
The MRI is used to exclude retrocochlear pathology.
-
D.
Bilateral acoustic neuromas are common.
-
A.
-
3.
The following symptomatology in relation to causes of vertigo are true except:
-
A.
In BPPV, the vertigo is with changes in the position of the head and neck and lasts for several hours and is not recurrent.
-
B.
A single severe episode of vertigo after a viral illness is usually due to vestibular neuronitis.
-
C.
In Meniere’s disease, the hearing loss is fluctuating and episodic.
-
D.
The hearing loss in acoustic neuroma is steadily progressive.
-
A.
MCQ Answers
1 = D; 2 =D; 3 = A
References
Samy HM. Dizziness vertigo and imbalance. http://e.medicine.medscope.com/article/2149881-overview. Retrieved on 23 October 2013.
Ojala M, Palo J. The aetiology of dizziness and how to examine the dizzy patient. Ann Med. 1991;23(3):225–30.
Bisdorff A, Bosser G, Guegen R, Perrin P. The epidemiology of vertigo, dizziness and unsteadiness and its links to co-morbidities. Front Neurol. 2013;4:29. https://doi.org/10.3389//fneur.2013.00029 9.
Hanley K, Dowd T, Crosindine N. A systematic review of vertigo in primary care. Brit J Clin Pract. 2001;51: 666–71.
Colledge NR, Barr-Hamilton M, Lewis ST, Sellar RJ, Wilson JA. Evaluation of investigation to diagnosis of the cause of dizziness in elderly people in community and controlled study. Br Med J. 1996;313:788–92.
Bird JC, Beynon GJ, Prevost AT, Baguley DM. Analysis of referral patterns for dizziness in the primary care setting. Br J Gen Pract. 1998;48:1828–1832.
Abrol R, Nehru VI, Venkataramana Y. Prevalence and etiology of vertigo in adult rural population. Ind J Otolaryngol Head Neck Surg. 2001;53(1):32–36.
Zhang Y, Chin X, Wang X, Cao L, Dong Z, Zhen J, et al. A clinical epidemiological study of 187 patients with vertigo. Cell Biochem Biophys 2001;59(2):109–12.
Karatas M, Central vertigo and dizziness, epidemiology differential diagnosis and common causes Neurologist 2008;14(6):355–64.
Labuguen RH. Initial evaluation of vertigo. Am Fam Physician. 2006;73(2):244–50.
Froehling DA, Silverstein MD, Mohr DN, Beatty CW, Offord KP, Ballard DJ. Benign positional vertigo: incidence and prognosis in a population-based study in Olmsted County Minnesota. Mayo Clin Proc. 1991; 66:596–601.
Koelliker P, Summers RL, Hawkins B. Benign Positional Paroxysmal vertigo: Diagnosis and treatment in the emergency department-a review of the literature and discussion of carolith repository maneuvers. Ann Emerg Med. 2001;37(4):392–8.
Somefun OA, Giwa OS, Bamgboyi BA, Oke-Igbokwe II, Azeez AA. Vestibular disturbances among adults in a tertiary hospital in Lagos Nigeria. Eur Arch Otorhinolaryngol. 2010;2(10):1515–21.
Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognised benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000;122:630–4.
Baloh RW. Differentiating between peripheral and central causes of vertigo. Otolaryngol Head Neck Surg. 1998;119(1):55–9.
Chan Y. Differential diagnosis of dizziness. Curr Opinion in Otolaryngol Head Neck Surg. 2009;17:200–203.
Neatherlin JS, Egan J. Benign Positional paroxysmal vertigo. J Neurosci Nurs. 1994;26(6):330–5.
Black FO, Pesznecker SC, Homer L, Stallings V. Benign paroxysmal positional nystagmus in hospitalized subjects receiving ototoxic medications. Otol Neurotol. 2004:25(3);353–8
Herdman SJ. Treatment of benign paroxysmal vertigo. Phys Ther. 1990;70:381–388.
Fyrampas G, Rachovitsas D, Haidich AB, Constantinidis J, Triaridis S, Vital V, et al. Are positional restriction after an Epley maneuver unnecessary? First results of a controlled study and review of literature. Auris Nesus Laryn 2009;36(6):637–43.
Baloh RW. Clinical practice. Vestibular neuritis. NEJM. 2003;348:1027–32.
Swartz R, Longwell P. treatment of vertigo. Am Fam Physician. 2005;71(6):115–22.
Wladislavosky-Waserman P, Facer GW, Mokri B, Kurland LT. Meniere’s disease: a 30 year epidemiologic and clinical study in Rochester, MN 1951–1980. Larynsoscope. 1984; 94:1098.–11-2.
Thirlwall AS, Kundu S. Diuretics for Meniere’s disease. Cochrane Database Syst Rev. 2006;3:CD003599.
James AL, Burton MJ. Betahistine for Meniere’s syndrome. Cochrane Database Syst. Rev. 2001;1: CD001873.
Halmagyi GM. Diagnosis and management of vertigo. Clin Med. 2005;5(2):159–65.
Moffat DA, Bagnley DM, Blumenthal H, Irving RM, Hardy DG. Sudden deafness in vestibular schwannoma. J Laryngol. Otol. 1994;108:116–9.
Eggenberger E, Lovell K. Vertigo and dizziness; Vestibular system disorders-Summary. http://learn.chm.msu.edu/Neuro Ed/neurobiology_disease/content/other sources/vestibular disorders.pdf. retrieved 12 January 2015.
Huang MH, Huang CC, Ryu SJ, Chu N-S. Sudden bilateral hearing impairment in vertebrobasilar occlusive disease. Stroke. 1993;24:132–137.
Maurer J. The role of brain stem evoked potentials in acoustic neuroma screening and diagnosis. Laryngorhinootologie. 2008;87(8):585–96.
Zealley IA, Cooper RC, Clifford KM, Campbell RS, Potterton AJ, Zammit-Maempel I, et al. MRI screening for acoustic neuroma: a comparison of fast spin echo and contrast enhanced imaging in 1233 patients. Br J Radiol. 2000;73(867):242–7.
Soulie D, Cordoliani YS, Vignaud J, Cosnard G. MR imaging of acoustic neuroma with high resolution fast spin echo T2-weighted sequence. Eur J Radiol. 1997; 24(1):61–5.
Oh JH, Chung JH, Min HJ, Cho SH, Park CW, Lee SH. Clinical application of 3D-FIESTA Image in patients with unilateral inner ear symptom. Korean J Audiol. 2013;17(3):111–117.
Weidt S, Bruehl AB, Straumann D, Hegemann SC, Krautstrunk G, Rufer M. Health-related quality of life and emotional distress in patients with dizziness: a cross-sectional approach to disentangle their relationship. BMC Health Serv Res.2014;14:317. https://doi.org/10.1186/1472-6963-14-317.
Hsu LC, Hu HH, Wong WJ, Wang SJ, Luk YO, Chern CM. Quality of life in elderly patients with dizziness: analysis of the Short Form Health Survey in 197 patients. Acta Otolaryngol. 2005;125(1):55–9.
Ten Voorde M, van der Zaag-Loonen HJ, van Leeuwen RB. Dizziness impairs health-related quality of life. Qual LifeRes 2012;21(6):961–6.
Tinettti ME, Williams CS, Gill TM. Dizziness among older adults. A geriatric syndrome. Ann Int Med 2000;132:337–344.
Yardley L, Owen N, Nazareth I, Luxon L. Prevalence and presentation of dizziness in general practice community sample of working age people. Br J gen Pract. 1998;48:1131–1135.
Lin HW, Bhattacharyya N. Balance disorders in the elderly: Epidemiology and functional impact. The Laryngoscope 2012;122(8):1858–61.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this entry
Cite this entry
Nagaratnam, N., Nagaratnam, K., Cheuk, G. (2018). Vertigo/Dizziness in the Elderly. In: Geriatric Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-33434-9_82
Download citation
DOI: https://doi.org/10.1007/978-3-319-33434-9_82
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-33433-2
Online ISBN: 978-3-319-33434-9
eBook Packages: MedicineReference Module Medicine