Abstract
Chronic cough is a common medical problem which may require the expertise of the bronchoscopist on occasion. There is a myriad of pulmonary and non-pulmonary disorders that are associated with cough which need to be considered for accurate diagnosis. In addition to the common causes, mastery of uncommon reasons for cough is necessary for the specialist. This chapter offers general overview of chronic cough and highlights some of the unusual causes of this symptom which may perplex the clinician.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Chronic Cough: Definition and Etiology
Chronic cough is one of the most common reasons for primary care physician visits and referrals to pulmonologists [1]. Chronic cough, defined as lasting more than 8 weeks, may have diverse and frequently multifactorial etiology (Table 17.1) with significant effect on quality of life. Various pulmonary parenchymal and airway diseases (e.g., interstitial lung disease and bronchiectasis) which present with abnormal chest imaging also have cough as one of the presenting symptoms. In this chapter, we focus on relatively uncommon etiologies of chronic cough related to airway disease which occur in the setting of a normal or near-normal chest X-ray. As such, these conditions are well within the practice realm of the bronchoscopist.
It has been suggested that a systematic approach to chronic cough employing an anatomic diagnostic protocol which includes empirical therapy has an extremely high diagnostic and therapeutic yield [2, 3]. Accordingly, upper airway cough syndrome (postnasal drip), asthma, and reflux disease account for over 80 % of the disorders that lead to chronic cough. In clinical practice, targeted diagnostic evaluation and empirical therapy, without any particular sequence, are used in conjunction with the management of these patients. An optimal cost-effective approach to the management of chronic cough has not been agreed upon. Moreover, recent data from a specialized cough center indicate a different distribution of etiologies for chronic cough, emphasizing the importance of referral bias when considering diagnostic possibilities [4].
The use of invasive testing in the diagnosis of chronic cough is controversial as well. In general, fiberoptic bronchoscopy has low clinical yield in patients with chronic cough [5]. However, clinical judgment is always necessary to determine whether invasive testing should be utilized. For instance, fiberoptic bronchoscopic examination may be indicated to investigate persistent change in the character of cough after antibiotic treatment in a smoker, to exclude endobronchial malignancy.
Physiology of Cough: Cough Reflex Arc, Cough Receptors
Cough is a protective physiologic reflex which facilitates the removal of foreign objects and debris from the airway. In order for an effective cough, an intact respiratory neuromuscular unit and optimal interaction between gas and mucus layers have to be present. Afferent nerve endings are most concentrated in the epithelia of the upper and lower respiratory tracts, but they are also located in the external auditory meatus, tympanic membrane, esophagus, stomach, pericardium, and diaphragm. The afferent limb of the arc is the vagus nerve and its many branches include tracheobronchial, superior laryngeal, Arnold’s nerve, pharyngeal, pleural, and gastric branches. The vagal afferent nerve types involved in the transmission of the impulse are rapidly adapting receptor (RAR), slowly adapting receptor (SAR) which most likely modify the cough reflex by processing mechanical stimuli (lung inflation, pulmonary edema), and C-fibers which respond primarily to chemical changes (pH, carbon dioxide, capsaicin and bradykinin) [6]. Activated C-fibers are also capable of inducing neuropeptide release without the activation of reflex arc and thus may play a role in neurogenic inflammation [7]. The vagal afferent impulse reaches the cough center which is located diffusely in the medulla oblongata. The efferent limb of the cough reflex starts from the cough center and the ventral respiratory group, a column of neurons located ventrolaterally in the medulla. The efferent impulse is conducted by the phrenic nerve and the spinal motor nerves to the inspiratory and expiratory muscles and by the recurrent laryngeal nerve to the larynx and bronchial tree.
The cough reflex is characterized by the generation of high intrathoracic pressures against a closed glottis, followed by forceful expulsion of air and secretions on glottic opening. High-velocity stream of air tears mucus off the airway walls and expel droplets into the air. Mucus clearance is facilitated by the greater depth of mucus but reduced by increasing mucus viscosity and elasticity [8].
Airway-Related Cough
Chronic cough due to primary airway disorders is relatively rare. Most of these conditions have been discussed elsewhere in the text. Table 17.2 provides a list of these.
Upper Airway Cough Syndrome
Upper airway cough syndrome, formerly known as postnasal drip syndrome, remains a poorly defined clinical definition that is largely defined by patient’s symptomatology without specific signs. It is a common cause of chronic cough. Typical patient presents with a sensation of mucus in the oropharynx and persistent need for frequent throat clearing. The condition may be caused by various upper airway inflammatory syndromes that span the spectrum of rhinosinusitis. The etiology may be bacterial, fungal, allergic, vasogenic (vasomotor rhinitis), or medication related (rhinitis medicamentosa). Unfortunately, there are no specific findings that would alert the bronchoscopist to the diagnosis of upper airway cough syndrome [9]. Oropharyngeal mucus and cobblestone changes may be present but are nonspecific. The diagnosis is generally one of exclusion and confirmed with favorable response to antihistamines and decongestants.
Cough and Reflux
Gastroesophageal reflux disease (GERD) is generally considered among the most common etiologies of chronic cough. Numerous studies have proposed a correlation between reflux and cough, and it is common clinical practice to initiate a trial of proton pump inhibitors (PPI) in patients that present with chronic cough. Irritation of the laryngeal mucosa is a common otolaryngological finding in patients suspected of suffering from GERD or laryngopharyngeal reflux (LPR). It is well known that GERD/LPR can cause ear, nose, and throat symptoms, secondary to tissue irritation. Most signs of laryngeal irritation have been traditionally attributed to LPR. However, many signs of laryngeal irritation, such as the presence of an interarytenoid bar, pseudosulcus, erythema of the medial wall of the arytenoids, and pharyngeal wall cobblestoning, showed a substantial overlap with normal subjects with no LPR, suggesting a lack of diagnostic specificity [10, 11]. The signs that were found to be more sensitive and specific to LPR include posterior commissure erosion or erythema (Fig. 17.1), vocal fold erythema, edema, and lesions (Figs. 17.2 and 17.3).
Treatment of GERD may result in marked improvement or complete resolution of symptoms in some patients with chronic cough. On the other hand, many patients with documented reflux do not have cough. Moreover, the response to reflux treatment in the management of chronic cough is highly variable [12]. The pathophysiology of reflux as it relates to cough remains elusive. Three main mechanisms have been proposed as possible initiators of cough related to acid exposure [13].
-
(A)
Reflux in the esophagus provokes coughing via an esophago-bronchial reflex that stimulates vagal afferents from the airway and esophagus.
-
(B)
Reflux into the larynx and pharynx may cause chronic laryngeal inflammation, increasing sensitivity of nerve terminals and stimulating cough receptors.
-
(C)
Reflux enters the airway by means of micro-aspiration, leading to chronic inflammation and stimulating airway cough receptors.
There are multiple known triggers for chronic cough including sensitivity to perfumes, chemicals, environmental irritants, changes in temperature, or laryngeal activities that directly stimulate vocal fold mucosa such as talking and laughing. In line with the more recent view on laryngeal neuronal hypersensitivity, GERD-LPR itself is probably not a direct cause of cough, but one additional trigger that stimulates an already hyper-reactive laryngeal—pharyngeal—or upper airway mucosa.
The current recommendations for the management of LPR in patients with signs of laryngeal irritation and chronic cough include initial empiric therapy with twice-daily PPI for two to four months [14]. If the cough responds to therapy, tapering to once-daily therapy and eventually to non-drug treatment such as behavioral and dietary guidelines is advisable.
Swallowing and Cough
An important function of the larynx is to protect the airways, and deficits in the motor or sensory status of the larynx and pharynx, and esophagus can lead aspiration of food, liquids, or secretions into the airways. As alluded to earlier, cough reflex is a brainstem-mediated protective mechanism that helps expectorate material before it enters the airway. Cough that occurs during or immediately after meals may be a sign of swallowing difficulty or dysphagia. The most common symptoms of oropharyngeal dysphagia include (a) aspiration, or entry of food into the airway below the level of the true vocal folds, (b) entry of material into the larynx at some level down to but not below the true vocal folds, (c) residue or food that is left behind in the mouth or pharynx after the swallow, and d) regurgitation of food from the esophagus into the pharynx and nasal cavity. Cough is an important diagnostic sign that can help detect patients at high risk for pneumonia, malnutrition, or dehydration.
Coughing to prevent penetration or aspiration is part of a normal sensory mechanism. It is important to remember that if there is sensory deficit, patients may be “silent aspirators,” where material goes past the true vocal folds into the airway without a proper cough response. Reports show that up to 60 % of in-patients in large hospitals or clinics may aspirate in the absence of a protective cough mechanism. High-risk populations include individuals with Parkinson’s disease, amyotrophic lateral sclerosis, dementia, head and neck cancer, vocal fold paralysis or paresis, stroke, and brain injury.
When patients complain about coughing or choking around mealtimes, they should be referred to an ear, nose, and throat specialist with expertise in swallowing disorders to evaluate the etiology of the cough. It is important to differentiate patients who cough around mealtimes due to acid reflux exposure, or due to a hypersensitive larynx, from those with dysphagia who are at risk for aspiration.
Esophageal adenocarcinoma (EAC) represents one of the most rapidly rising malignancies in the USA. The diagnosis of EAC is usually made in the later stages of the disease, and most patients diagnosed with EAC have incurable disease at the time of detection. The majority of these patients are unaware of the presence of Barrett’s esophagus prior to cancer diagnosis and many do not report typical symptoms of GERD. Several studies have shown that LPR symptoms, in particular chronic refractory cough, may be a predictor for EAC. Moreover, chronic cough has been suggested to be a better predictor of the presence of cancer and Barrett’s esophagus than typical gastroesophageal reflux symptoms such as heartburn. Therefore, endoscopic screening for Barrett’s esophagus and EAC should be considered for patients with refractory chronic cough of unknown etiology [15].
Aberrant Laryngeal Sensitivity and Reactivity
The term Irritable Larynx Syndrome (ILS) was introduced by Morrison and Rammage in 1999, and described as a condition in which a person experiences laryngeal muscle spasms, triggered by a sensory stimulus [16]. The laryngeal muscle spasm can cause episodes of coughing without apparent cause, a sense of a lump in the throat (globus sensation), laryngospasm, hoarseness, and paradoxical vocal fold motion.
ILS was initially thought to be related to altered brain stem control of laryngeal sensory-motor processes. However, in a 2010 update, the authors proposed that ILS is a central sensitivity syndrome where laryngeal and paralaryngeal muscles overreact to normal sensory stimuli [17]. They reported that out of 195 patients with ILS, more than half presented with one or two comorbidities related to central nervous system dysfunction such as irritable bowel syndrome, fibromyalgia, chronic fatigue syndrome, and migraines, concluding that ILS is secondary to central nervous system hypersensitivity.
Laryngeal hypersensitivity is a challenging condition since its constellation of symptoms can defy easy diagnosis and lead to under-recognition or misdiagnosis. Many subspecialties may be the entry point for patients who present with episodes of severe shortness of breath, chronic refractory cough, a prominent sensation of chest and throat constriction, dramatic stridor and hypersensitivity to fumes and strong smells. These can include pulmonary, allergy, otolaryngology, speech-language pathology, gastroenterology, and neurology. Adding to the challenge is the fact that the multidisciplinary involvement has resulted in a lack of unifying terminology. The following terms, all referring to similar conditions, have been used in recent literature: Chronic Refractory Cough, Post-Viral Vagal Neuropathy, Sensory Neuropathic Cough, Cough Hypersensitivity Syndrome, Laryngeal Sensory Neuropathy, Irritable Larynx Syndrome, Airway Hyper-responsiveness, and Cough Reflex Hypersensitivity.
A growing body of literature supports the idea that the aberrant laryngeal activity in these conditions is caused by peripheral sensory and motor neuropathies. All involve sensory dysfunction. There appears to be a complex interaction between peripheral nervous system and central nervous system processes with the evidence of both having excitatory and inhibitory influences.
Recently, Mazzone and colleagues have demonstrated that evoked cough is not only a brainstem-mediated reflex response to irritation of the airways, but it requires active facilitation by cortical regions and is further regulated by distinct higher order inhibitory processes [18]. Recent investigations indicate that there is an inverse relationship between the mechanical and the chemical responses of the airway mucosa to stimuli [19], suggesting that there is hyposensitivity to mechanical stimulation and hypersensitivity to chemical stimulation of the laryngeal airway mucosa.
The mounting evidence that central system sensitization is a relevant mechanism in refractory chronic cough, has led to the use of neuroleptic and psychotropic medications in the treatment of chronic cough and associated conditions. Clinical evidence along with a small cohort of studies recommends the use of the following for treatment of refractory chronic cough that has been non-responsive to more traditional treatment options: (a) Gabapentin, an antiepileptic also used to treat neuropathic pain [20]; (b) Tricyclic antidepressants, also used in chronic pain and fibromyalgia [21, 22]; (c) Selective serotonin re-uptake inhibitors, and combined serotonin and norepinephrine re-uptake inhibitors [23]; and (d) Baclofen, a centrally acting spasmolytic drug [24, 25].
Behavioral therapy is another effective management intervention for chronic cough that persists despite an adequate trial of medical treatments. This therapeutic intervention is conducted by a speech-language pathologist with expertise in treatment of cough. Therapy addresses lifestyle modifications, avoidance of sensory stimuli with treatment of LPR and minimizing exposure to triggers, and voice and breathing exercises in order to reprogram the habituated (laryngeal) motor response [26].
Chronic cough and laryngeal hypersensitivity are challenging and difficult to manage conditions because the constellation of symptoms can defy easy diagnosis. The impact that these can have on daily life is substantial. Some patients experience relentless symptoms that can persist for years, even decades, and frequent hospitalizations are not uncommon. Significant disability is seen in some cases, with noticeable impact on quality of life. Chronic cough is currently considered truly a multidisciplinary disease. The degree of cooperation between pulmonary, allergy, ENT, and speech pathology subspecialties is becoming more common in major healthcare facilities, and it can become a part of community practice as well. A “chronic cough clinic” offers the promise of many benefits:
-
Improve the timing of diagnosis.
-
Lower healthcare costs by [1] avoiding duplication of tests and [2] reducing the number of patient visits.
-
Streamline management recommendations.
-
Shorten the time necessary to achieve successful treatment.
-
Improve outcomes.
-
Improve patient satisfaction.
Professionals in subspecialties that commonly see these patients should make an effort to work with their colleagues and develop their own alliances that ultimately result in better patient care.
Obstructive Sleep Apnea
Obstructive sleep apnea is a clinical syndrome that results from an exaggerated propensity of upper airway collapse during sleep which occurs due to a complex interaction between anatomical (narrow, long, collapsible airway) and ventilatory control-related factors.
In a series of carefully documented cases, Birring et al. found obstructive sleep apnea to be the sole reason for chronic cough [27]. These patients experienced diagnostic delays of up to 3 years. The magnitude of the chronic cough symptom overshadowed their obstructive sleep apnea symptoms. Remarkably, within days of starting nasal CPAP, patients experienced significant and objectively documented reduction in their cough.
Chan and colleagues studied 55 patients with obstructive sleep apnea syndrome and no history of lung disease, recent upper respiratory tract infection, or use of ACE inhibitor [28]. 18 of these patients (33 %) had cough and 37 (67 %) did not. The patients with obstructive sleep apnea and cough were more likely to report symptoms of nocturnal heartburn and rhinitis. Presence or severity of cough had no relationship to the respiratory disturbance index.
The pathophysiological relationship between obstructive sleep apnea and cough is open to speculation. However, the two established causes for cough, upper airway inflammation and reflux disease, may explain the association. Repetitive collapse and opening of the airway has been shown to be associated with upper airway inflammation [29–31]. Furthermore, reversal of upper airway and systemic inflammation has been demonstrated after the use of nasal CPAP in patients with obstructive sleep apnea [32]. Obstructive sleep apnea also predisposes to gastroesophageal reflux as a consequence of marked swings in transdiaphragmatic pressure (suction effect) [33].
Patients with obstructive sleep apnea may pose specific challenges to the bronchoscopist. In a series of lung transplant recipients, patients with obstructive sleep apnea had significantly higher rates of procedural hypoxemia due to upper airway collapse [34]. When performing bronchoscopy for the investigation of chronic cough, presence of redundant upper airway, intraprocedural snoring, and hypoxemia may provide clues to the bronchoscopist for the diagnosis of obstructive sleep apnea. In those patients with known obstructive sleep apnea, performing the procedure in the presence of a nasopharyngeal tube [34], or while the patient receives noninvasive positive pressure ventilation [35], can alleviate upper airway obstruction and hypoxemia.
Cough Hypersensitivity Syndrome
In 2005, investigators at the Royal Brompton Hospital cough clinic reported their experience with 100 consecutive patients who were referred to this tertiary care center [4]. These patients were investigated and managed according to the anatomical protocol which involves systematic investigation and empirical treatment of the 3 common conditions which cause cough, i.e., asthma, upper airway cough syndrome, and GERD. The authors determined that the 3 conditions only account for 45 % of the patients. In additional 13 %, miscellaneous etiologies including post-viral cough, ACE inhibitor cough, COPD, bronchiectasis, Bordetella pertussis infection, and yellow nail syndrome were suggested. The remaining 42 % had no diagnosis after exhaustive work-up. These patients were said to have “chronic idiopathic cough” (CIC). Compared to patients with known etiology, patients with CIC had longer duration of the symptom, higher cough sensitivity as measured by capsaicin challenge, a higher incidence of precedent upper respiratory tract infection, and symptoms of sensitive cough reflex (such as coughing while talking, laughing, or eating crumbly foods). Chronic cough hypersensitivity syndrome was suggested as a more descriptive label for the condition since the entity represented a constellation of symptoms and signs associated with objective cough hypersensitivity, not explained by any specific medical condition [36]. It is important to note that cough hypersensitivity does not equate bronchial hyperreactivity.
Diagnosis of chronic cough hypersensitivity syndrome is one of exclusion; however, typical clinical characteristics, i.e., presence of allotussia and hypertussia, long duration, and precedent respiratory infection are helpful to the clinician. Treatment of the condition remains a challenge. Success has been reported with neuroactive agents such as gabapentin [20] and amitriptyline [22, 37]. As alluded to earlier, the relationship of chronic cough hypersensitivity syndrome and other similar entities such as aberrant laryngeal sensitivity remains a topic of discussion and research.
Inflammatory Airway Disease
Eosinophilic Inflammation of the Airway
Chronic cough can be a consequence of a continuum of inflammatory airway disorders associated with eosinophilic infiltration. These encompass the relatively common classic and cough variant asthma and less common and less-known entities of non-asthmatic eosinophilic bronchitis and atopic cough. Since cough is an accompanying and not main symptom of classical asthma, we will focus our discussion to cough variant asthma, non-asthmatic eosinophilic bronchitis, and atopic cough.
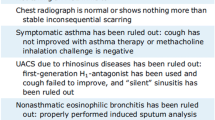
In essence, classical asthma is characterized by intermittent reversible airflow obstruction (bronchial hyperreactivity) and eosinophilic airway inflammation. Symptoms are dominated by the consequence of airflow obstruction, i.e., wheezing and shortness of breath. Eosinophilic inflammation is seen in the smooth muscle layer as well as airway epithelium. Cough variant asthma presents with the sole symptom of cough. There is evidence of bronchial hyperreactivity on challenge testing. Non-asthmatic eosinophilic bronchitis also presents with cough, but there is no evidence of bronchial hyperreactivity on objective testing. Here, eosinophilic inflammation is limited to airway epithelium. Atopic cough is a controversial entity described in Japan, where cough variant asthma is extremely prevalent. The hallmark of atopic cough is response to antihistaminic medications and presence of eosinophilic airway inflammation. Clinical nuances of these disorders are summarized in Table 17.3.
Cough Variant Asthma
Cough variant asthma is a subtype of asthma characterized by cough as the only presenting symptom [38]. It is one of the most common etiologies for chronic cough [1] accounting up to 30-40 % of cases. Atopy and seasonal variation are almost as common as classical asthma albeit lesser in magnitude [39]. Pulmonary function testing is essentially within normal limits. Sine a qua non is the presence of airway hyperreactivity on pulmonary function testing. Cough hypersensitivity as determined by capsaicin challenge is also present and improves after a 2-week course of leukotriene antagonists [40]. Cough variant asthma characteristically responds well to bronchodilators; however, inhaled corticosteroids are frequently necessary for the treatment of persistent cough [41]. Cough variant asthma can progress to classical asthma up to 40 % of the time [42].
Non-asthmatic Eosinophilic Bronchitis
Eosinophilic bronchitis is a pathological entity shared by various clinical conditions. In addition to asthma, rhinitis, COPD, and healthy individuals, patients with GERD may have evidence of eosinophilic bronchitis on pathology. Non-asthmatic eosinophilic bronchitis (eosinophilic bronchitis without asthma) as a cause of chronic cough was first described by Gibson et al. [43]. Patients with the condition presented with sputum eosinophilia (>3 %), normal spirometry without airway hyper-responsiveness, and an excellent response to corticosteroids [44]. Nevertheless, frank asthma (9 %) or fixed airflow obstruction (16 %) can develop over time [45].
Systemic Disorders that Affect the Airways
Connective Tissue Disease
Although cough can occur with various connective tissue disease (scleroderma, lupus, rheumatoid arthritis), this is mostly in the setting of parenchymal pulmonary involvement. In the case of Sjogren’s syndrome however, cough can occur with airway involvement without significant abnormality in the lung tissue.
Sjogren Syndrome
Sjogren syndrome is a systemic inflammatory disorder that chiefly affects the exocrine glands. Diagnosis of Sjogren (primary) syndrome is made by using subjective and objective data for xerostomia and keratoconjunctivitis sicca and one of the criteria for autoimmunity (inflammatory infiltrates detected in minor saliva glands, and/or presence of Ro/La autoantibodies). Positive Schirmer’s test, sialometry, ultrasound, or MRI of the saliva glands may be considered as confirmatory tests.
Sjogren syndrome is associated with multiple interstitial lung diseases such as nonspecific interstitial pneumonia, organizing pneumonia, lymphocytic interstitial pneumonia, follicular bronchiolitis, and granulomatous lung disease [46]. All of these entities may also be associated with chronic cough.
Chronic cough can also occur in primary Sjogren syndrome, however, without the presence of any interstitial lung disease. In a study by Bellido-Casado [47], 72 % of patients had respiratory symptoms such as cough and dyspnea without any radiological abnormalities. Interestingly, cough was more prevalent among patients with normal sputum inflammatory cell count in this study. In contrast, bronchodilator response or methacholine challenge test positivity was more prevalent among those with abnormal sputum (lymphocytosis). Cough in the absence of airway inflammation suggests that extrapulmonary etiologies for cough may be prevalent among patients with Sjogren syndrome, e.g., reflux disease. Indeed, three quarters of the patients with Sjogren syndrome may report dysphagia and presence of reflux disease has also been demonstrated [48]. Notably, methacholine challenge testing can be positive in up to 60 % of patients with Sjogren syndrome [49].
Inflammatory Bowel Disease
Inflammatory bowel diseases, i.e., Crohn’s disease and ulcerative colitis, are associated with a myriad of pulmonary manifestations. Common embryological origin from the primitive foregut, similar luminal structure, and presence of submucosal lymphoid tissue in both tracts has been proposed as explanation for the pathophysiological link [50]. Lung parenchyma may be involved with pulmonary nodules, organizing pneumonia, nonspecific interstitial pneumonia, and granulomatous inflammation similar to sarcoidosis. The bronchoscopist may encounter large airway involvement manifesting as bronchiectasis, chronic bronchitis, or sometimes life-threatening purulent tracheobronchitis [51]. Severe inflammation in the major airways can lead to inflammatory pseudotumors and frank stenosis of the airway. Inflammatory bowel disease-related airway inflammation responds well to corticosteroids administered systemically or via inhaled therapy. The bronchoscopist should exclude concurrent infection, particularly non-tuberculous Mycobacterium species in these patients [52].
Vasculitis
Vasculitides comprise a group of disorders characterized by immune-mediated inflammation and destruction of blood vessels. Among these, granulomatosis with polyangiitis (GPA) formerly known as Wegener’s granulomatosis and giant cell arteritis (GCA) are the most commonly associated with airway symptoms. GPA involves the central airways commonly and is associated with subglottic and tracheobronchial stenosis. Cough and hemoptysis are common. This disorder has been covered in detail, elsewhere in this text.
Giant cell arteritis is a vasculitic disorder of large- and medium-sized blood vessels characterized by the onset of disease after the age of 50, high sedimentation rate, headache, and vasculitis found on temporal artery biopsy [53]. Respiratory involvement is rare and may take the form of pleural effusion [54], mild interstitial lung disease [55], and in situ pulmonary artery thrombosis [56]. However, a puzzling clinical presentation is with a dry, nagging cough. In fact, dry cough is the most common respiratory manifestation of GCA [57]. It can also be the presenting symptom in approximately 8 % of the patients [57, 58]. Bronchoscopic examination may reveal nonspecific bronchitis [59]. Therefore, the bronchoscopist should be alert to the unusual presentation of this potentially morbid but treatable condition in the elderly patient who presents with a nagging, dry cough and an unexplained inflammatory disease.
References
Irwin RS. Introduction to the diagnosis and management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):25S–7S.
Irwin RS, Corrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis. 1981;123(4 Pt 1):413–7.
Smyrnios NA, Irwin RS, Curley FJ, French CL. From a prospective study of chronic cough: diagnostic and therapeutic aspects in older adults. Arch Intern Med. 1998;158(11):1222–8.
Haque RA, Usmani OS, Barnes PJ. Chronic idiopathic cough: a discrete clinical entity? Chest. 2005;127(5):1710–3.
Barnes TW, Afessa B, Swanson KL, Lim KG. The clinical utility of flexible bronchoscopy in the evaluation of chronic cough. Chest. 2004;126(1):268–72.
Canning BJ. Anatomy and neurophysiology of the cough reflex: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):33S–47S.
Barnes PJ. Neurogenic inflammation in the airways. Respir Physiol. 2001;125(1–2):145–54.
McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):48S–53S.
Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):63S–71S.
Hicks DM, Ours TM, Abelson TI, Vaezi MF, Richter JE. The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers. J Voice. 2002;16(4):564–79.
Milstein CF, Charbel S, Hicks DM, Abelson TI, Richter JE, Vaezi MF. Prevalence of laryngeal irritation signs associated with reflux in asymptomatic volunteers: impact of endoscopic technique (rigid vs. flexible laryngoscope). Laryngoscope. 2005;115(12):2256–61.
Smith JA, Abdulqawi R, Houghton LA. GERD-related cough: pathophysiology and diagnostic approach. Curr Gastroenterol Rep. 2011;13(3):247–56.
Kahrilas PJ, Smith JA, Dicpinigaitis PV. A causal relationship between cough and gastroesophageal reflux disease (GERD) has been established: A Pro/Con debate. Lung. 2014;192(1):39–46.
Barry DW, Vaezi MF. Laryngopharyngeal reflux: More questions than answers. Cleve Clin J Med. 2010;77(5):327–34.
Reavis KM, Morris CD, Gopal DV, Hunter JG, Jobe BA. Laryngopharyngeal reflux symptoms better predict the presence of esophageal adenocarcinoma than typical gastroesophageal reflux symptoms. Ann Surg 2004;239(6):849–56 (discussion 856-8).
Morrison M, Rammage L, Emami AJ. The irritable larynx syndrome. J Voice. 1999;13(3):447–55.
Morrison M, Rammage L. Revue Cannadienne d’orthophonie et d’audiologie. 2010;34–4.
Mazzone SB, Cole LJ, Ando A, Egan GF, Farrell MJ. Investigation of the neural control of cough and cough suppression in humans using functional brain imaging. J Neurosci. 2011;31(8):2948–58.
Phua SY, McGarvey L, Ngu M, Ing A. The differential effect of gastroesophageal reflux disease on mechanostimulation and chemostimulation of the laryngopharynx. Chest. 2010;138(5):1180–5.
Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet. 2012;380(9853):1583–9.
Bastian RW, Vaidya AM, Delsupehe KG. Sensory neuropathic cough: a common and treatable cause of chronic cough. Otolaryngol Head Neck Surg. 2006;135(1):17–21.
Jeyakumar A, Brickman TM, Haben M. Effectiveness of amitriptyline versus cough suppressants in the treatment of chronic cough resulting from postviral vagal neuropathy. Laryngoscope. 2006;116(12):2108–12.
Zylicz Z, Krajnik M. What has dry cough in common with pruritus? Treatment of dry cough with paroxetine. J Pain Symptom Manage. 2004;27(2):180–4.
Xu X, Chen Q, Liang S, Lu H, Qiu Z. Successful resolution of refractory chronic cough induced by gastroesophageal reflux with treatment of baclofen. Cough 2012;8(1):8. doi:10.1186/1745-9974-8-8.
Dicpinigaitis PV, Dobkin JB, Rauf K, Aldrich TK. Inhibition of capsaicin-induced cough by the gamma-aminobutyric acid agonist baclofen. J Clin Pharmacol. 1998;38(4):364–7.
Ryan NM, Vertigan AE, Bone S, Gibson PG. Cough reflex sensitivity improves with speech language pathology management of refractory chronic cough. Cough. 2010;28(6):5.
Birring SS, Ing AJ, Chan K, Cossa G, Matos S, Morgan MD, et al. Obstructive sleep apnoea: a cause of chronic cough. Cough. 2007;2(3):7.
Chan KK, Ing AJ, Laks L, Cossa G, Rogers P, Birring SS. Chronic cough in patients with sleep-disordered breathing. Eur Respir J. 2010;35(2):368–72.
Sekosan M, Zakkar M, Wenig BL, Olopade CO, Rubinstein I. Inflammation in the uvula mucosa of patients with obstructive sleep apnea. Laryngoscope. 1996;106(8):1018–20.
Paulsen FP, Steven P, Tsokos M, Jungmann K, Muller A, Verse T, et al. Upper airway epithelial structural changes in obstructive sleep-disordered breathing. Am J Respir Crit Care Med. 2002;166(4):501–9.
Hatipoglu U, Rubinstein I. Inflammation and obstructive sleep apnea syndrome: how many ways do I look at thee? Chest. 2004;126(1):1–2.
Karamanli H, Ozol D, Ugur KS, Yildirim Z, Armutcu F, Bozkurt B, et al. Influence of CPAP treatment on airway and systemic inflammation in OSAS patients. Sleep Breath. 2012.
Demeter P, Pap A. The relationship between gastroesophageal reflux disease and obstructive sleep apnea. J Gastroenterol. 2004;39(9):815–20.
Chhajed PN, Aboyoun C, Malouf MA, Hopkins PM, Plit M, Grunstein RR, et al. Management of acute hypoxemia during flexible bronchoscopy with insertion of a nasopharyngeal tube in lung transplant recipients. Chest. 2002;121(4):1350–4.
Murgu SD, Pecson J, Colt HG. Bronchoscopy during noninvasive ventilation: indications and technique. Respir Care. 2010;55(5):595–600.
Chung KF. Chronic ‘cough hypersensitivity syndrome’: a more precise label for chronic cough. Pulm Pharmacol Ther. 2011;24(3):267–71.
Greene SM, Simpson CB. Evidence for sensory neuropathy and pharmacologic management. Otolaryngol Clin North Am 2010;43(1):67–72, viii.
Niimi A. Cough and asthma. Curr Respir Med Rev. 2011;7(1):47–54.
Takemura M, Niimi A, Matsumoto H, Ueda T, Yamaguchi M, Matsuoka H, et al. Atopic features of cough variant asthma and classic asthma with wheezing. Clin Exp Allergy. 2007;37(12):1833–9.
Dicpinigaitis PV, Dobkin JB, Reichel J. Antitussive effect of the leukotriene receptor antagonist zafirlukast in subjects with cough-variant asthma. J Asthma. 2002;39(4):291–7.
Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):75S–9S.
Matsumoto H, Niimi A, Takemura M, Ueda T, Tabuena R, Yamaguchi M, et al. Prognosis of cough variant asthma: a retrospective analysis. J Asthma. 2006;43(2):131–5.
Gibson PG, Dolovich J, Denburg J, Ramsdale EH, Hargreave FE. Chronic cough: eosinophilic bronchitis without asthma. Lancet. 1989;1(8651):1346–8.
Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med. 1999;160(2):406–10.
Berry MA, Hargadon B, McKenna S, Shaw D, Green RH, Brightling CE, et al. Observational study of the natural history of eosinophilic bronchitis. Clin Exp Allergy. 2005;35(5):598–601.
Shi JH, Liu HR, Xu WB, Feng RE, Zhang ZH, Tian XL, et al. Pulmonary manifestations of Sjogren’s syndrome. Respiration. 2009;78(4):377–86.
Bellido-Casado J, Plaza V, Diaz C, Geli C, Dominguez J, Margarit G, et al. Bronchial inflammation, respiratory symptoms and lung function in Primary Sjogren’s syndrome. Arch Bronconeumol. 2011;47(7):330–4.
Belafsky PC, Postma GN. The laryngeal and esophageal manifestations of Sjogren’s syndrome. Curr Rheumatol Rep. 2003;5(4):297–303.
La Corte R, Potena A, Bajocchi G, Fabbri L, Trotta F. Increased bronchial responsiveness in primary Sjogren’s syndrome. A sign of tracheobronchial involvement. Clin Exp Rheumatol. 1991;9(2):125–130.
Black H, Mendoza M, Murin S. Thoracic manifestations of inflammatory bowel disease. Chest. 2007;131(2):524–32.
Henry MT, Davidson LA, Cooke NJ. Tracheobronchial involvement with Crohn’s disease. Eur J Gastroenterol Hepatol. 2001;13(12):1495–7.
Storch I, Rosoff L, Katz S. Sarcoidosis and inflammatory bowel disease. J Clin Gastroenterol. 2001;33(4):345.
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990;33(8):1122–8.
Valstar MH, Terpstra WF, de Jong RS. Pericardial and pleural effusion in giant cell arteritis. Am J Med. 2003;114(8):708–9.
Karam GH, Fulmer JD. Giant cell arteritis presenting as interstitial lung disease. Chest. 1982;82(6):781–4.
Andres E, Kaltenbach G, Marcellin L, Imler M. Acute pulmonary embolism related to pulmonary giant cell arteritis. Presse Med. 2004;33(19 Pt 1):1328–9.
Zenone T, Puget M. Dry cough is a frequent manifestation of giant cell arteritis. Rheumatol Int. 2013;33(8):2165–8.
Becourt-Verlomme C, Barouky R, Alexandre C, Gonthier R, Laurent H, Vital Durand D, et al. Inaugural symptoms of Horton’s disease in a series of 260 patients. Rev Med Interne. 2001;22(7):631–7.
Carassou P, Aletti M, Cinquetti G, Banal F, Landais C, Graffin B, et al. Respiratory manifestations of giant cell arteritis: 8 cases and review of the literature. Presse Med. 2010;39(9):e188–96.
Brightling CE. Chronic cough due to nonasthmatic eosinophilic bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1_suppl):116S–21S.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hatipoğlu, U., Milstein, C.F. (2016). Chronic Cough: An Overview for the Bronchoscopist. In: Mehta, A., Jain, P., Gildea, T. (eds) Diseases of the Central Airways. Respiratory Medicine. Humana Press, Cham. https://doi.org/10.1007/978-3-319-29830-6_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-29830-6_17
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-29828-3
Online ISBN: 978-3-319-29830-6
eBook Packages: MedicineMedicine (R0)